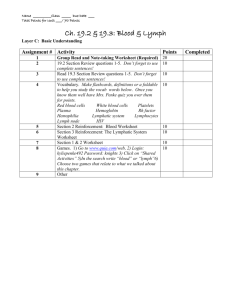
CVS Lecture 4:
THE VASCULAR FUNCTIONS
DYNAMICS OF CIRCULATION
Lecture contents:
Arterial Circulation
Cardiovascular/intravascular loop
Venous circulation
Microcirculation ~ Trans vascular loop
Lymphatic circulation ~ Lymphatic loop
By: Wondimu DH
direshaile@gmail.com
Department of Medical Physiology, SoMP, UR
1
2024
Arterial
2
1. Elastic Arteries
Windkessel vessels – aorta and major branches
Two properties
Distensibility: compliance (accommodative/systole, P~ 80 → 120 mmHg).
Elastic recoil: subsidiary pump( pulsatile to a steady continuous flow/diastole)
WINDKESSEL EFFECT
a second pump.
Reduces the energy expenditure of heart.
determinant for venous return
Cc: age-related degenerative changes (systolic HTN)
Atherosclerosis in small blood vessels (essential HTN)
3
2. Muscular Arteries
Distributing channels to the organs (eg. radial, facial …)
Relatively large lumen to minimize resistance.
3. Arterioles
Stopcocks (valves) of circulation ~ A narrow, thicker wall/vascular tone/ major
determinant of TPR (~75%) and pressure transmitted to capillaries and veins.
Conversion of pulsatile flow from the
heart to a steady continuous flow
↑Vasomotor/sympathetic innervations.
Also: local and hormonal control.
Autoregulation (metabolic &
myogenic) ~ Renal, brain,
skeletal muscle, mesentery
4
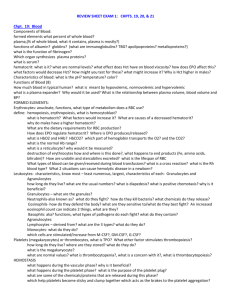
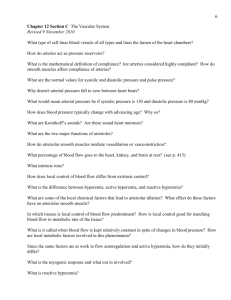
Systemic Arterial Blood Pressure
Decreases throughout the system
Pressure caused by blood on the wall of
the blood vessels
Normal: Ps: 90 – 140 mm Hg (120)
Pulse pressure
Pd: 60 – 90 mm Hg (80)
Pp: Ps – Pd ~ 40
MAP = Pd + 1/3(Ps - Pd) ~
Determinants: [ABP = CO x TPR]
1. Cardiac output
2. Peripheral vascular resistance
3. Blood volume
5
CO = HR x SV
SV ~ EDV
Regulation of Arterial Blood Pressure
Short term and Intermediate-term
regulation is the function of peripheral
◦ Heart activities
◦ Resistance
◦ Capacitance and
◦ Fluid volume shift
Long-term regulation is the function of
blood volume
oExcretion of water and electrolytes
ECF Blood volume
Circulatory filling pressure
VR CO ABP
6
Variations in ABP: causes
oAge: ABP rises as age increases
oSex: After the age of 50, F > M by 5 mm Hg
oTime of the day: ↓morning, ↑evening
oBody wt: ABP higher by 10-15 mm Hg in obese
oGravity:
oExercise: increases ABP by 40 – 50 mm Hg
oEmotion: increases ABP by 10 – 30 mm Hg
oDeep sleep: decreases ABP by 20 mm Hg
oThermal stress: decreases ABP
7
Method of Measurement of ABP
8
Venous
9
Veins are thin walled vessels
with relatively large lumen.
larger cross-sectional area than
do the arteries.
Veins have paired semilunar,
bicuspid valves to restrict
backflow in lower extremities:
CC: varicose veins
10
Functions of veins
1. Blood reservoirs: ~ 60–70%
Distensibility and collapsibility
Highly compliant: spleen, liver, large
abdominal veins, venous plexus below
the skin.
2. Conduits
Systemic return to RA and the
pulmonary veins from the lungs to LA.
Capacitance vessel
3. Maintenance of cardiac output (VR)
Venoconstriction during blood loss.
11
Venous Pressure and Flow
low-resistance and low-pressure system
Is the pressure in the RA and thoracic vena
cava (RAP = jugular venous P.).
Responsible for cardiac filling.
o
Central venous pressure
(CVP)
The higher, the less VR
CVP = 0 - 4 mm Hg [Abn:-3 to 30 mmHg]
Assess hypovolaemia and transfusion
o
Raised in right-sided failure
The pressure in the venules ~10 mmHg.
In the great veins, near the heart, venous
pressure drops ~ <5 mmHg
Peripheral venous pressure
VR
…..favores VR
12
Mean Systemic Filling Pressure (MSFP)
Mean Circulatory Pressure (MCP)
Measured at all points in the whole circulatory
system if the heart were stopped suddenly.
The pressure nearest to the tissues (~ 7 mm Hg).
RAP at which venous return is zero.
MCP
Vascular function curve intersects the X-axis
(i.e.,VR is zero and RAP is at its highest value)
MCP
It is affected by: Blood volume & venous/
vascular capacity/compliance
Venous return curve: Vascular function13curve
Venous Return (VR)
It is the volume of blood
returned to the RA per min.
VR or Vascular function curve
Graph drawn from RAP and venous return
~ CO when averaged over
time as CVS is a closed loop.
VR = MSFP – RAP
--------------Resistance to VR (RVR)
VR = MAP-RAP/TPR (If RAP = 7; VR goes to 0)
o MSFP = 7, RAP = 0; RVR=1.7 mmHg/L of blood flow; VR-5 L/min
~ 5 L/min at rest & about 35L/min in well trained athletes during exercise
Venous return back to the heart is driven by a pressure gradient
[The lower the RAP, the higher the pressure gradient the greater the VR].
14
…VFC shifts to the right
10VENOUS
RETURN
(L/min)
MCP
5-
…VFC shifts to the left
Blood Volume
or
Venodilation
Blood Volume
or
Venoconstriction
MCP
0-
-4
0
+4
RAP (mmHg)
+8
TPR
Vasoconstriction
15
Combining Cardiac Function/CO curve and
Vascular Function/VR curve
Intersect at a single value of RAP.
CO equals VR (steady state operating point of the system).
o satisfies both CO and VR relationships.
A shift of the vascular function curve to the right…increase in MSFP.
Steady state or operating point
16
Factors affecting VR
1. Mean Systemic Filling Pressure (MSFP)
• It is the driving force for VR.
• MCFP = equilibration pressure where arterial BP = venous BP
2. Right Atrial Pressure(RAP)
• Mean pressure in the right atrium = central venous pressure (SVC and IVC, CVP) =2
mmHg
• RAPVR
3. Resistance to venous return (RVR)
• Resistance blood meets(1mmHg/L/min) during its flow from arterial side to RA.
VR
=
MSFP – RAP
-----------------RVR
17
4. Blood volume:
At constant venous capacity, as the blood volume → the MCP → VR.
5. Vascular compliance ~ blood that veins can accommodate.
The overall compliance of the vascular system is determined by venous tone.
At a constant blood volume, as venous compliance → MCP ↓→ ↓ VR.
o As the venous capacity ↓ → VR.
Arteriolar vasoconstriction → ↓ VR because blood flow into the
microcirculation.
18
6. Sympathetic activity:
Sympathetic stimulation of venous smooth muscle:
→ venoconstriction → → ↓ venous capacity → modest MCP → VR.
cardiac pumping power & arteriolar dilatation RVR VR
Capillary dilatation vascular capacity, MSFP VR
7. Skeletal muscle pump:
Skeletal muscle contraction → external venous
compression → ↓ venous capacity, MSFP → VR.
Also counter the effects of gravity on VR.
8. Venous valves:
Permit blood to move forward towards the heart but
prevent it from moving back toward the tissues.
Play a role in counteracting the gravitational effects.
Skeletal muscle pump is ineffective when the venous valves are incompetent.
Eg. varicose veins; increased capillary filtration leads to swelling (edema)
with trophic skin changes and ulceration (venous ulcers).
19
9. Effect of gravity on venous return
Venous volume and pressure become very high in the feet and
lower limbs when standing (decreases thoracic venous blood
volume and therefore CVP).
RV filling pressure (preload) stroke volume.
Pulmonary venous return LV preload LV sv.
CO and MAP.
Standing motionless for some time pooling of
blood in lower extremities MSFP VR CO
hypotension brain ischaemia syncope
20
Effect of hydrostatic pressure of blood on arterial and venous pressure in an upright position.
21
10. Respiratory activity
(respiratory pump; thoracic pump):
The increased rate and depth of ventilation.
Forceful inspiration causes -ve intrathoracic
pressure that expand the lungs.
The decrease in intrathoracic pressure acts
as an external force on the venae cava and
the right atrium, causing them to distend
(transmural pressure changes).
As more blood is drawn into the thoracic
vena cava from the abdomen, more blood
enters the right atrium.
Question: What is the effect of Valsalva maneuver on
venous return?
22
The
Capillary
23
The Capillary or microcirculation
Functions:
Exchange of materials between the
blood and tissues.
Drain waste from tissues to blood.
Maintain arterial blood pressure by
altering total peripheral vascular
resistance and diastolic cardiac filling.
Involved in temperature regulation.
24
Parts of microcirculation
Microscopic (d ~ 100 μm): small
arterioles, meta-arterioles, pre-cap
sphinictor, capillaries, Post-cap
venules and arteriovenous shunts.
25
Capillary bed: Arterioles
Resistance blood vessels restrict flow to
capillaries or allow greater flow.
~ diameter: 5 – 100 μm.
Have a thick continuous smooth muscle
layer and endothelial lining.
Have pre-capillary sphincters
When open → nutritional flow.
[Resting: 20% open in skeletal M.]
When closed → non-nutritional flow
or shunt flow.
26
Capillary bed: Metarterioles and A-V shunt
Metarterioles
Discontinuous smooth muscle layer.
Give rise to capillaries (d~ 10-20 μm)
Linked to venules and/or capillaries.
They have pre-capillary sphincters/gate.
A-V shunt (AV anastomosis/thoroughfare):
direct connection between arteriole & venule.
Allows bypass of capillaries if precapillary
sphincters are closed (sympathetic innerv.)
flow is 100% non-nutritional (skin of
fingers, toes and earlobes/thermoregulation).
.... bronchial veins,
thebesian veins, pleural
veins, enters the left
ventricle directly.
Postcapillary Venules: with VSM, most permeable part/affected by local
factors and histamine. Are blood reservoirs/buffer volume changes.
27
Capillary bed: Capillaries and Venules
Capillaries
Structure:
Small blood vessels [ ~ 0.5-1 μm long, d ≈ 0.01 mm]
With no SMCs.
A single endothelial cell thick (rapid diffusion ~ < 2 ms)
Density ~ tissue’s metabolic activity
in skeletal muscle, heart, brain, liver and kidney.
in skin and cartilage.
Functions:
Sites of exchange between blood and tissues. The arterial
system delivers blood to > l billion capillaries throughout
the body [Total capillary surface area=1000 m2].
Venules: Constriction of venules increased capillary pressure
Capillaries diameters are not uniform. Eg. deformation of RBCs as they28 pass.
Regulation of flow in capillary beds
(Neural and Metabolic)
Arterioles and met-arterioles: mainly controlled by sympathetic vasoconstriction.
Flow through capillaries is controlled by pre-capillary sphincters.
This is affected by local metabolic state of tissue – auto-regulation.
During the “fight or flight” response, flow to non-essential organs
(kidney, skin, etc) is clamped off → increased flow to skeletal muscle.
Metabolic waste products act as vasodilators.
Vasomotion: intermittent flow via capillary intermittent contraction of metaarterioles and precapillary sphincters, in response to changing needs.
spontaneous, rhythmic, smooth muscle contractions result either from
pacemaker currents or from slow waves of depolarization.
29
Types of body capillaries
1~μm
Muscle, lung, and
adipose tissue,
Blood-Brain-Barrier,
Blood-Retinal-Barrier
wide pores
d~ 20–100 nm
Allow bulk fluid and even
large substances to pass but
not plasma proteins.
Renal glomeruli, intestinal
villi, and endocrine glands.
Cilliary process of the eye
Choroid plexus
Sinusoid
d~600–3000 nm
Not closed by BM
Large irregular lumens
allow large molecules
(e.g., proteins) to pass
Liver, spleen, bone
marrow, lymphoid tissue,
some endocrine glands.
30
Microcirculation and Thermoregulation
The cutaneous circulation
Capillaries are arranged perpendicular to surface.
Has low density of capillaries.
Venous plexus ~ heat transfer to the skin.
Arteriovenous anastomosis: opens/closes in
response to changes in temp.
If core or surface temp high →
↓sympathetic outflow to skin →
opening of the arteriovenous anastomoses →
↑ flow in venous plexus and capillaries
(radiation/loss).
31
Transcapillary exchange
The interstitium also contains two major types of solid structures: collagen
fiber and proteoglycan filaments (~ tissue gel with most ISF).
Little ISF (<1%) forms the free fluid.
Fluid can pass through the tissue gel very slowly but diffusion can occur
through it as rapidly as in free fluid.
Gases, nutrients and waste products diffuse through the tissue gel very freely.
Mechanisms of exchange:
Diffusion (across PM &/or clefts; Fick’s law; concentration gradient)
J = P (CB – CT) {p: no charge, small, water soluble sub. – eg. gases, AAs, glucose}
Transcytosis (vesicular transport/larger & non-lipid soluble substances).
Ultrafiltration (Bulk transport/according to pressure gradient).
32
Transcytosis (vesicular transport)
An active process by which large
molecules can be transported
Very slow and contributes very
little to total capillary exchange.
Includes
in-pocketing
(endocytosis)
out-pocketing (exocytosis).
e.g. Peptide hormones.
33
Ultrafiltration: Starling’s Forces
Net fluid flux = K (filtration forces – reabsorption forces).
K [(Pc + πIF) – (πc + PIF)].
K is determined by:
Blood viscosity.
Wall thickness.
Surface area.
Permeability of capillary
20ml fluid/min
18ml fluid/min
~ 2ml/min
K is high in liver and kidneys, while it
is low in the blood-brain barrier.
Normally the amount filtered slightly exceeds the amount reabsorbed and is eventually
returned to the circulation via the lymphatics
34
Hydrostatic capillary pressure (Pi)
~ −2 mmHg in subcutaneous tissue
but is positive in the liver and
kidneys, and as high as +6 mmHg in
the brain.
Oncotic pressure (πc)
Mainly related to plasma proteins
and solute concentration.
Oncotic pressure (πi)
Mainly related to plasma proteins.
↑Pc → ↑filtration; can lead to edema.
Glomerular /filtering capillary: 50–60 mmHg
Hydrostatic interstitial pressure (Pc)
depends on ABP, Pre- and postcapillary resistance and Venous
pressure (most important).
Intestine and the pulmonary circulation absorptive capillaries: 8-10 mm Hg.
35
Note: The amount of blood passing through pulmonary circulation is the same as through
systemic one despite pressure difference (17 vs. 7 mmHg) .
36
Capillary fluid shift (Intermediate Level Regulation of ABP)
This mechanism corrects a change in blood volume by shifting fluid b/n plasma
and interstitial fluid.
↑Blood volume
↑ABP
↑Filtration out of capillaries (blood moved
to ISF)→↓ABP )
↓Blood volume
↓ABP
↓Capillary pressure
↓Filtration of fluid
37
Lymphatic
38
Where does the excess fluid of 2-3 L/day go?
• Net filtration – net absorption = net outflow
• collected by lymph vessels (2-3 L fluid and 120 g protein/day)
When ISF increases as filtration exceeds the rate of capillary reabsorption plus
lymphatic flow, it can lead to tissue swelling (i.e., edema).
39
LYMPHATIC DRAINAGE SYSTEM
Lymphatic vessels: lymphatic capillaries
Blind sacs collecting excess tissue fluid.
Simple squamous epithelium with large gaps, no tight J., no basement M.
Cells overlap to form one-way valves within lumen.
They possess fine filaments which anchor them to the connective tissue
When contracts, can pull on the endothelial cells, allowing protein, large particles or
cells to enter lymph system.
40
Lymphatics: originate as lymph capillaries that unite to form larger vessels
- resemble veins but with thinner walls, less muscle, less connective tissue, and more valves.
- They connect to lymph nodes at various intervals.
Lymphatic trunks: formed by the union of lymphatics. They carry lymph to lymphatic ducts.
Lymphatic ducts: empty into large veins (right and left subclavian veins) just before they join the
superior vena cava.
Thoracic duct - drains lower body & left head, left arm, part of chest (open into junction of left
subclavian vein and internal jugular vein)
Right lymph duct - drains right head, neck, right arm & part of chest (opens into right subclavian v)
Major driving force: Pif →↑fluid in lymphatics→ stretch-mediated contraction propel lymph
(safety factor)
41
Mechanism of Lymph Circulation
Lymph moves along pressure gradient ( ~ 2-4 liters/day).
Valves keep unidirectional lymph flow to the heart.
The mechanisms that may contribute to pressure gradient are:
– Skeletal muscle pump.
– Inspiration (-ve intrathoracic pressure but increases abdominal cavity).
– Pulsation of neighboring elastic arteries.
– contraction of smooth muscle in walls of larger lymphatic vessels and ducts
(intrinsic lymphatic pump).
– Suction effect of high-velocity blood flow in the veins in which the lymphatics
terminate also promotes lymph flow.
– An increase in the interstitial fluid pressure increases the lymph flow
– Increase in capillary surface area by capillary distension and permeability
– Increase in functional activity of the tissue
42
Composition of Lymph
Protein (regional variation, 6g/100ml in liver): < plasma ~ = ISF (~ 2 g/100ml)
[Arteriolar end: 100-200g/day; Venular end: 5g/day; Lymph:95 to 195 g/day]
Lipids: route of absorption of fat
cholesterol and phospholipid (lipoproteins)
neutral fat (chylomicrons, chyle)
Electrolytes: ~ plasma
Cells:
Mainly lymphocytes of all sizes and maturity
rare monocytes / macrophages
granulocytes following infection
43
Function of Lymph flow
1.
2.
3.
4.
Return lost protein to the vascular system (~ 200g/d)
Drain excess plasma filtrate from ISF space (maintain its gel state).
Carry absorbed nutrients (e.g. fat-chlyomicrons) from GI tract.
Acts a transport mechanism to remove red blood cells that have lost
into the tissues as a result of haemorrhage.
5. Supplies nutrients & oxygen to those parts where blood cannot reach.
6. Filter system (defense function) at lymph nodes
lymph nodes with sinuses with tissue macrophages (phagocytosis)
No true lymphatic vessels in superficial portions of skin, CNS, endomysium of
muscle, & bones = eg. functional lymphatic system in CNS
44
Edema
Is an abnormal increase in the interstitial fluid volume.
Hydrostatic edema
Exudate
Permeability edema
Lymphatic Filariasis
(Elephantiasis)
45
Clinical significance of capillary fluid dynamics
In blood loss:
Vasoconstriction of arterioles decrease capillary hydrostatic pressure.
Hence osmotic pressure of plasma proteins favours absorption of
interstitial fluid blood volume.
In congestive heart failure:
Venous pressure rises build-up of blood in capillaries capillary
hydrostatic pressure filtration oedema.
In hypoproteinaemia (e.g., starvation, liver disease):
Plasma protein loss of fluid from capillaries oedema.
In inflammation:
Gaps between the endothelial cells increase because of the inflammatory
mediators movement of proteins into the interstitium oedema.
46