Uploaded by
Francesca Bianca Joy Gañalongo
Vascular System: Function, Assessment, and Disorders
advertisement

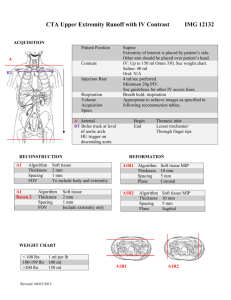
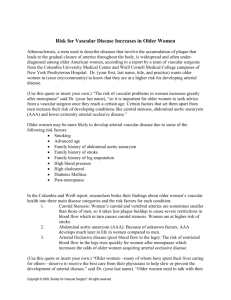
consists of two interdependent systems 1. right side of the heart - pumps blood through the lungs to the pulmonary circulation 2. left side of the heart - pumps blood to all other body tissues through the systemic circulation Vascular system Function of the Vascular System 1. Circulatory Needs of Tissues 2. Blood Flow arterial pressure - approximately 100 mm Hg venous pressure - approximately 40 mm Hg 3. Capillary Filtration and Reabsorption - Fluid exchange across the capillary wall is continuous Function of the Vascular System 4. Blood pressure 5. Hemodynamic Resistance - the most important factor that determines resistance in the vascular system is the vessel radius. Small changes in vessel radius lead to large changes in resistance. 6. Peripheral Vascular Regulating Mechanisms - an integrated and coordinated regulatory system is necessary so that blood flow to individual tissues is maintained in proportion to it’s needs consists of; 1.central nervous system influences 2. circulating hormones and chemical 3. independent activity of the arterial wall itself Assessment of the Vascular System Health History Rubor – a–reddish – blue Cyanosis a bluish tint of the Pallor – reduction in blood Inspection of the Skin discolorationof the extremities skin 9.Edema may be– 2apparent bilaterally - flow Maybe observed 2 sec. min especially when 1. Cool and pale extremities after-or Occurs when amount of - dependent position theunilaterally extremity is placed in the extremities is elevated oxygenated hgb contained in appear after 2. Pallor position 10.dependent Gangrenous changes the blood arterial is reduced - Severe peripheral damage 3. Rubor prolonged, severe ischemia 4. loss of hair 5. brittle nails 6. dry or scaling skin 7. Atrophy 8. Ulcerations Nursing Implications 1.Patients with impaired renal function scheduled for MDCT may require preprocedural treatment to prevent contrast-induced nephropathy - e.g. oral or IV hydration 6 to 12 hours preprocedure or administration of sodium bicarbonate - alkalinizes urine and protects against free radical damage. 2. nurse should monitor the patient’s urinary output postprocedurally, which should be at least 0.5 mL/kg/h. Contrast-induced acute kidney injury may occur within 48 to 96 hours postprocedure 3. known iodine or shellfish allergies may need premedication with steroids and histamine blockers. 6. Angiography - used to confirm the diagnosis of occlusive arterial disease when surgery or other interventions are considered - It involves injecting a radiopaque contrast agent directly into the arterial system to visualize the vessels. The location of a vascular obstruction or an aneurysm (abnormal dilation of a blood vessel) and the collateral circulation can be demonstrated. 7. Magnetic Resonance Angiography (MRA) - is performed with a standard magnetic resonance imaging (MRI) scanner and special software programmed to isolate the blood vessels. 8. Contrast Phlebography (Venography) - contrast phlebography involves injecting a radiopaque contrast agent into the venous system. If a thrombus exists, the x-ray image reveals an unfilled segment of vein in an otherwise completely filled vein. - Injection of the contrast agent may cause brief but painful inflammation of the vein. . Atherosclerosis - direct result - indirect results stenosis of the lumen obstruction by thrombosis malnutrition Aneurysm Ulceration fibrosis of the organs that Rupture the sclerotic artery supplied with blood Reduction in blood supply - severe and permanent (cells) ischemic necrosis fibrous tissue ( requires much less blood flow) Atherosclerotic lesions are of two types: Stages of Atherosclerosis Modifiable risk factors Nonmodifiable factors risk Medical Management A. Surgical Management 1 B. Radiologic Interventions 1. Angioplasty or Percutaneous transluminal angioplasty (PTA) - a balloon-tipped catheter is maneuvered across the area of stenosis B. Radiologic Interventions Atherectomy - reduces the plaque build-up within an artery using a cutting device or laser Complications: hematoma formation embolus dissection (separation of the intima) of the vessel acute arterial occlusion bleeding C. Improving Peripheral Arterial Circulation positioning: - below the level of the heart D. Promoting Vasodilation and Preventing Vascular Compression - To increase blood flow to the extremities Nursing interventions: 1. applications of warmth 2. avoid exposure to cold temperatures 3. adequate clothing and warm temperatures 4. if chilling, a warm bath or drink is helpful. A hot water bottle or heating pad may be applied to abdomen 5. stop smoking 6. avoid stress 7. restrict use of constrictive clothing and accessories such as tight socks or shoelaces 8. Avoid Crossing the legs for more than 15 minutes at a time because it compresses vessels in the legs. E. Relieving Pain F. Maintaining tissue integrity Promoting Home, Community-Based, and Transitional Care Peripheral Arterial Occlusive Disease - Arterial insufficiency of the extremities occurs most often in men and is a common cause of disability. - The legs are most frequently affected - The age of onset and the severity are influenced by the type and number of atherosclerotic risk factors Peripheral Arterial Occlusive Disease Clinical Manifestations 1. intermittent claudication - hallmark symptom 2. decreased ability to walk the same distance as before or may notice increased pain with ambulation 3. rest pain - persistent, aching, or boring; it may be so excruciating that it is unrelieved by opioids and can be disabling. Peripheral Arterial Occlusive Disease Assessment and Diagnostic Findings 1.sensation of coldness or numbness in the extremities 2.intermittent claudication 3.extremity is cool and pale when elevated 4.ruddy and cyanotic when placed in a dependent position 5. Skin and nail changes - hickened and opaque 6. Ulcerations 7.gangrene 8. muscle atrophy 9.Peripheral pulses may be diminished or absent 10.Unequal pulses between extremities 11.skin may be shiny, atrophic, and dry, with sparse hair growth Upper Extremity Arterial Occlusive Disease - occur less frequently in the upper extremities (arms) than in the legs - causes less severe symptoms because the collateral circulation is significantly better in the arms. - The arms also have less muscle mass and are not subjected to the workload of the legs. Upper Extremity Arterial Occlusive Disease Clinical Manifestations 1.arm fatigue and pain with exercise (forearm claudication) 2. inability to hold or grasp objects (e.g., combing hair, placing objects on shelves above the head) 3. occasionally difficulty driving 4.“subclavian steal” syndrome - characterized by reverse flow in the vertebral and basilar arteries to provide blood flow to the arm. This syndrome may cause vertebrobasilar (cerebral) symptoms like vertigo, ataxia, syncope, or bilateral visual changes Upper Extremity Arterial Occlusive Disease Assessment 1.coolness and pallor of the affected extremity 2. decreased capillary refill 3. a difference in arm blood pressures of more than 20 mm Hg Diagnostic Findings 1. upper and forearm blood pressure determinations 2. duplex ultrasonography. 3. Transcranial Doppler evaluation. 4. arteriogram Upper Extremity Arterial Occlusive Disease Medical Management 1. PTA with possible stent or stent graft placement focal lesion - short 2. surgical bypass - If the lesion involves the subclavian artery with documented siphoning of blood flow from the intracranial circulation Upper Extremity Arterial Occlusive Disease Nursing Management 1.bilateral comparison of upper arm blood pressures (obtained by stethoscope and Doppler), 2.radial, ulnar, and brachial pulses 3.motor and sensory function 4. temperature 5. color changes 6.capillary refill every 2 hours Upper Extremity Arterial Occlusive Disease Nursing Management Post surgery or endovascular procedure: 1. Keep arm elevated or at heart level (fingers at highest level) 2. Monitor pulses 3. Blood pressure 4. Motor and sensory function 5. Temperature 6. Capillary refill and color Aortoiliac Disease Medical Management Nursing Management Preprocedural or preoperative assessment includes: a.evaluating the brachial, radial, ulnar, femoral, posterior tibial, and dorsalis pedis pulses to establish a baseline for follow-up after arterial lines are placed and postoperatively b. educate about the procedure and anticipated plan of care Nursing Management Postoperative care: - is a localized sac or dilation formed at a weak point in the wall of the artery - It may be classified by its shape or form. - most common: - Saccular - fusiform Characteristics of arterial aneurysm. A. Normal artery. B. —actually a pulsating hematoma. The clot and connective tissue are outside the arterial wall. C. . One, two, or all three layers of the artery may be involved. D. —symmetric, spindle-shaped expansion of entire circumference E. —a bulbous protrusion of one side of the arterial . F. — this usually is a hematoma that splits the layers of the arterial wall. Caused by: atherosclerosis (70%) - occur most frequently in men between the ages of 50 and 70 years - - estimated to affect 10 of every 100,000 older adults - thoracic area is the most common site for a dissecting aneurysm - Thoracic aortic emergencies are associated with high morbidity and mortality rates Clinical Manifestations - Some patients are asymptomatic - In most cases, pain is the most prominent symptom - pain is usually constant and boring but may occur only when the person is supine - dyspnea, cough, hoarseness, stridor, weak or complete loss of voice, dysphagia Assessment and Diagnostic Findings 1. superficial veins of the chest, neck, or arms become dilated 2. edematous areas on the chest wall and cyanosis are often evident 3. chest x-ray 4. computed tomography angiography (CTA) 5. MRA 6. echocardiography (TEE) Medical Management - Treatment is based on whether the aneurysm is symptomatic, is expanding in size, is caused by an iatrogenic injury, contains a dissection, and involves branch vessels. - General measures such as controlling blood pressure and correcting risk factors are helpful Pharmacological: 1. beta blockers S - have been the mainstay of medical treatment for aortic aneurysms 2. angiotensin receptor blockers (ARBs) - also retard aortic dilatation Surgical: endovascular graft - most common cause is atherosclerosis - affects men 2 to 6 times more often than women - 2 to 3 times more common in Caucasian versus black men - Often occur below the renal arteries (infrarenal aneurysms) - If untreated, the eventual outcome may be rupture and death. Pathophysiology - All aneurysms involve a damaged media layer of the vessel - caused by congenital weakness, trauma, or disease Risk factors - genetic predisposition - tobacco use - hypertension Clinical Manifestations 1. Patients complain that they can feel their heart beating in their abdomen when lying down 2. they may say that they feel an abdominal mass or abdominal throbbing 3. Severe back or abdominal pain (persistent or intermittent) – sign of impending rupture 4. Low back pain 5. Indications of a rupturing abdominal aortic aneurysm includes: - constant, intense back pain - falling blood pressure Assessment and Diagnostic Findings 1. 2. 3. 4. pulsatile mass in the middle and upper abdomen palpable during routine physical examination A systolic bruit may be heard over the mass Duplex ultrasonography or CTA is used to determin the size, length, and location of the aneurysm. Pharmacologic Therapy 1.Antihypertensive agents Diuretics beta blockers ACE inhibitors ARBs - calcium channel blockers Endovascular and Surgical Management 1. open surgical repair of the aneurysm - involves subclavian artery, renal artery, femoral artery or (most frequently) popliteal artey Assessment and Diagnostic findings 1. aneurysm produces a pulsating mass and disturbs peripheral circulation distal to it 2. Pain and swelling develop because of pressure on adjacent nerves and vein 3. duplex ultrasonography or CTA - to determine the size, length, and extent of the aneurysm. Arteriography may be performed to evaluate the level of proximal Occasionally, in an aorta diseased by arteriosclerosis, a tear develops in the intima or the media degenerates, resulting in a dissection Pathophysiology: - refer to ink Medical Management - medical or surgical treatment of a dissecting aorta depends o the type of dissection present Nursing Management - the same nursing care as a patient with an aortic aneurysm requiring intervention - Acute vascular occlusion may be caused by an embolus or acute thrombosis. - may result from iatrogenic injury, which can occur during insertion of invasive catheters such as those used for: 1. Arteriography 2. PTA or stent placement 3. intra-aortic balloon pump 4. as a result of IV drug abuse - Other causes include trauma from a fracture, crush injury, and penetrating wounds Pathophysiology - Arterial emboli arise most commonly from thrombi that develop in the chambers of the heart as a result of atrial fibrillation, myocardial infarction, infective endocarditis, or chronic heart failure - These thrombi become detached and are carried from the left side of the heart into the arterial system - lodge in and obstruct an artery Medical Management 1. Surgery - embolectomy 2. Heparin therapy - initial IV bolus of 60 U/kg body weight, followed by a continuous infusion of 12 U/kg/h 3. Intra-arterial thrombolytic (e.g., tissue plasminogen activator [alteplase (Activase, t-PA) Nursing Management 1. affected part is kept at room temperature 2. protect affected leg from trauma 3. patient is admitted to a critical care unit for continuous monitoring 4. Vital signs are taken initially every 15 minutes and then at progressively longer intervals if the patient’s status remains stable. 5. Closely monitored for bleeding. 6. The nurse minimizes the number of punctures for inserting IV lines and obtaining blood samples 7. Apply pressure at least twice as long as usual - Raynaud phenomenon is a form of intermittent arteriolar vasoconstriction that results in coldness, pain, and pallor of the fingertips or toes. 2 forms of this disorder: 1. Primary or idiopathic Raynaud’s (Raynaud disease) - occurs in the absence of an underlying disease 2. SecondaryRaynaud’s (Raynaud syndrome) - occurs in association with an underlying disease, usually a connective tissue disorder a. systemic lupus erythematosus b. rheumatoid arthritis c. scleroderma; Clinical Manifestations 1.pallor 2.skin becomes bluish (cyanotic) 3.hyperemia due to vasodilation 4.rubor - produced when oxygenated blood returns to the digits after the vasospasm stop The characteristic sequence of color change of Raynaud phenomenon is described as white, blue, and red. 5. numbness, tingling and burning pain – can occur as color changes Medical Management - Avoiding the particular stimuli (e.g., cold, tobacco) that provoke vasoconstriction is a primary factor in controlling Raynaud phenomenon - 1. Calcium channel blockers - nifedipine [Procardia], amlodipine [Norvasc) - 2. Sympathectomy - interrupting the sympathetic nerves by removing the sympathetic ganglia - 3. Avoidance of exposure to cold and trauma