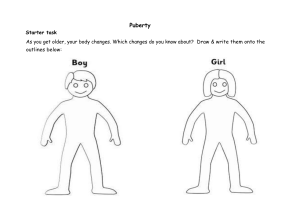
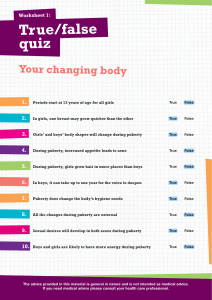
NORMAL PUBERTY AND DISORDER OF PUBERTY By Phyo Wai Aung (Wednesday/8.9.2021) Puberty Puberty is a vital process in the development of all individuals – the series of hormonal changes during puberty results in the physical development of sexually mature adults.In addition to sexual maturity ,children also go through other physical and emotional changes such as hair growth , voice changes and acne. Hormonal control of puberty Hypothalamic-pituitary-gonadal axis Normal physiolgy -hypothalamic-pituitary-gonadal axis is active for the first few months of life -is dormant until about 8 -9 yrs of age -About 1 -3 yrs before puberty is clinically evident ,LH levels become detectable during sleep -LH is pulsatile in nature -this pulsatile nature results in the increse in the size of the gonads and maturation and secrection of sex hormones Development Puberty typically begins Grils → 8 -13 yrs Boys → 9– 14 yrs Pubery in girls -the most notable and reliable first sign of puberty in girls is breast development -Breast development (thelarche) typically occurs between 10 to 11 yrs old followed by the appearance of pubic hair (pubarche) 6-12mon later → -Menarche follows shortly after thelarche about 2- 2.5 yr later, but may be as long as 6 yrs. -Peak height velocity occurs early (at breast stages II-III, typically between 11 and 12 yrs of age) in girls and always precedes menarche In males , -Growth of testes ( ≥ 4ml in volume or 2.5cm in longest diameter ) and thinning of the scortum are the first signs of puberty(11-12 yr) -these are followed by pigmentation of the scrotum and growth of the penis and by pubrache -axillary hair → occurs in midpuberty -growth → maximal at genital stages IV-V -In males,the growth spurt occurs approximate – 2 yrs later than in females and growth may continue beyond 18 yrs of age Clinical staging of puberty Boys -Genitalia(penis) development stages Stage G2 Stage G1 Stage G1 Stage G2 Preadolescent. Tests,scortum and penis are about same size and shape as in early childhood Scortum slightly enlarged , with reddening of the skin and changes in the texture.little or no enlargement of the penis at this stage. Stage G3 Stage G4 Penis slightly enlarged, at first mainly in length.Scortum further enlarged than in stage G2 Penis further enlarged,with growth in breath and development of glans.Further enlargement of scortum and darkening of scortal skin Stage G3 Stage G4 Stage G5 Stage G5 Genitalia adult in size and shape Prader orchidometer 1-2 ml are prepubertal 3-4 ml mark the beginning of puberty 8-10ml are associated with the beginning of height acceleration in mid-pubertal boys, usually at stage G3 12- 15 ml coincide with the maximum growth velocity, usually at stage G4 20ml (usually at stage G5) signifies that most boys have passed the peak of their growth spurt and are beginning to fuse their epiphyses on account of higher levels of testosterone secrection. Parder Orchidometer Pubic hair stages for boys and girls Stage PH1: Preadolescent. The vellus over the pubes is not further developed than that over the abdominal wall, i.e.no pubic hair. Stage PH2: Sparse growth of long,slightly pigmented downy hair, straight or slightly curled, chiefly at the base of the penis or along labia Stage PH3: Considerably darker, coarser and more curled.The hair spreads sparsely over the junction of the pubes Stage PH4: Hair now adult in type,but area covered is still considerably smaller than in adults.No spread to medial surface of thighs. Stage PH5: Adult in quantity and type with distribution of the horizonal (or classically ’feminine’)pattern.Spread to medial surface of thighs , but not up the linea alba Stage PH6: Spread upward along the linea alba(the typical male escutcheon) Girls Development Breast Stage B1: Preadolescent:elevation of papilla only Stage B2: Breast bud stage:elevation of breast and papilla as small mound.Areolar diameter enlarged over stage B1 Stage B3: Breast and areola both enlarged and elevated more than in stage B2, but with no separation of their contours. Stage B4 The areola and papilla form a secondary mound projecting above the contour of the breast Stage B5 Mautre stage: papilla only projects, with the areola recessed to the general contour of the breast Timing of puberty In almost all children the pattern of progress through puberty is constant but the timing of attainment of each stage can be considerably variable. Onset of puberty G2 in boys –mean age of 12 yrs Onset of puberty B2 in girls –mean age of 11 yrs Mean age at menarche – 13yrs PATHOPHYSIOLOGY Precocious Puberty Precocious puberty is defined by the onset of secondary sexual characters before the age of 8 yrs in girls and 9 yrs in boys. Classified 1.Central (gonadrotropin dependent,or ture ) precocious puberty -early activation of the hypothalmus-pituitary-gonadal axis -5 to 10 fold more often in girls than in boys -always isosexual -usually sporadic in female -90% of girls – idiopathic -almost always pathological in males Peripheral (gonadrotropin independent,or precocious pseudopuberty) Peripheral precocious puberty, also known as precocious pseudo puberty, is gonadotropin-independent and occurs due to excess production of sex hormones either from the gonads, the adrenal glands, ectopic or exogenous sources. In peripheral precociouspuberty, some of the secondary sex characteristics appear, but there is no activation of the normal hypothalamic-pituitary-gonadal interplay. In this group, the sex characteristics may be isosexual or heterosexual Peripheral precocious puberty ↓ induce Maturation of hypothalmus- pituitary- gonadal axis ↓ trigger Onset of central puberty (Mix type of precocious puberty) bone age reaches the pubertal range (10.5-12.5 yr) Laboratory Findings (liquid chromatography/tandem mass spectrometry) -Assays for sex hormones -sensitive and specific -serum estradiol concentration – low or undetectable in early phase of sexual precocity in girls -serum testrosterone levels - usually detectable (early monring blood sample) Immunoflurometric and chemiluminescent assays ( LH ) -highly sensitive -LH concentrations – undetectable in prepubertal children (radom blood sample ) - detectable in 50 -75% of girls & - higher percentage of boys with central sexual precocity (measurement of LH in serial blood samples obtained during sleep > diagnostic power than measurement in a single random sample ) GnRH stimulation test -also called (leuprolide stimulation test ) -helpful diagnostic tool In boys -pubertal LH response (LH peak >5IU/L) , -predominance of LH over FSH . Early in the course of Precocious puberty In girls Noctural LH secrection and LH response to GnRH or GnRH agonist -may be quite low at breast stages II to early III (LH peak, < 5IU/L) -LH:FSH ratio → remain low until mid-advance puberty Pubertal estradiol levels → (>50 pg/mL) 20 to 24hr after stimulation with leuprolide Osseous maturation -variably advanced -often more than 2-3 SD Pelvic U/S- girls → reveals progressive enlargement of of the ovaries -enalrgement of the fundus -whole uterus to pubertal size MRI -physiology enlargement of pituitary gland – seen in normal puberty -reveal CNS pathology -MRI scan recommend- all children with central precicous puberty Conditions causing precocious puberty Central(gonadotropin dependent,True precocious puberty) Idiopathic Organic brain lesions Hypothalamic hamartoma Brain tumors,hydrocephalus,severe head truma,myelomeningocele Hypothyroidism, prolonged and untreated COMBINED PERIPHERAL AND CENTRAL Treated congenital adrenal hyperplasia McCune-Albright syndrome, late Familial male precicous puberty,late PERIPHERAL(GONADOTROPIN INDEPENDENT,PRECOCIOUS PSEUDOPUBERTY) Girls - Contined Isosexual(Feminizing) conditions McCune-Albright syndrome Autonomous ovarian cysts Ovarian tumors Granulosa-theca cell tumor associated with Olier disease Teratoma, chorionepithelioma SCTAT associated with Peutz-Jeghers syndrome Feminizing adrenocortical tumor Exgenous estrogens Heterosexual (musculinizing) conditions Congenital adrenal hyperplasia Adrenal tumors Ovarian tumors Glucocorticoid receptor defect Exogenous androgens ContinuedBoys Isosexual (masculinizing) conditions Congenital adrenal hyperplasia Adrenocortical tumor Leydig cell tumor Familial male precocious puberty isolated Associated with pseudohypoparathyroidism hCG-secrecting tumors Central nervous system Hepatoblastoma Mediastinal tumor associated with Klinefelter syndrome Teratoma Glucocorticoid receptor defect Exogenous androgen ContiunedHeterosexual (feminizing ) conditions Feminizing adrenalcotical tumor SCTAT associated with Peutz-Jeghers syndrome Exogenous estrogens IMCOMPLETE (PARTIAL) PRECOCIOUS PUBERTY Premature thelarche Premature adrenarche Premature menarche Hypothalmus Harmartoma -most common brain lesion – cause central precocious puberty -congenital malformation consists of ectopically located neural tissue -produce transforming growth factor alpha → activate GnRH pulse generator CF - Central precocious puberty - epilepsy with gelastic seizures → complex seizure -hypothalmic symptoms(such as diabetes insipidus , adipsia, hyperthermia -visual signs (protosis , decreased visual acuity , visual field defects ) -sexual precocity- isosexual -growth hormone deficiency occour MRI -small pedunculated mass attached to the tuber cinereum or the floor of third ventricle sessile mass Hypothalamic hamartoma measuring 1.3cm×0.8cm×1cm at the floor of the third ventricle, affecting the tuber cinereum, and between the mamillary bodies (A) T1 sagittal view and (B) T2 coronal view. Precocious puberty following Irradiation of the brain Etiology - CNS-irradiation in prepubertal children with leukemia or brain tumors can lead to precocious puberty -in high doses to delayed puberty. The underlying mechanisms of these disorders are unknown. -The GnRH-pulse generator is very radiosensitive -Radiation induced - precocious puberty -damage to inhibitory GABAergic neurons leading to desinhibition and premature activation of GnRH neurons -Radiation therapy, generally for leukemia or intracranial tumors → risk of precocious puberty ↑ -low dose (18 – 24 Gy) → hastens the onset of puberty in grils -High dose radiation (25-47Gy) → trigger precicous sexual development in boht sexes -associated with growth hormone deficiency -rapid advacne bone age (+) -impaired adult height potential Syndrome of Precocious puberty and hypothyroidism (untreated) -onset of puberty usually delay until epiphyseal maturation reaches 12-13 yr of age In girls -breast enlargement , menstral bleeding -U/s-reveal large ,multicystic ovaries Boys -testiucualr enlargement associated with modest or no penile enlargement -no pubic hair in both sexes Investigatons -TSH level ↑ (> 500umol /L ) → specificity spillover induce FSH-like effect→ causing precicous puberty -prolactin and estradiol → mildly elevated serum FSH is low and LH is undetectable, the precocious puberty associated with hypothyroidism behaves as an incomplete form of gonadotropin-dependent puberty Chronic Gonadotropin-secreting Tumors -secrection of hCG → stimulates LH receptors in the Leydig cells -testicles minimally enlarged -FSH / LH - low -these tumor induce puberty in boys but not in grils Hepatic tumors -isosexual precocious pubety in boys -plasmas levels of hCG and 𝛼-fetoprotein – usually marked elevated McCune-Albright syndrome (polycystic fibrous dysplasia) -endocrine dysfunction , hyperpigmentation, skeletal fibrous dysplasia -missense mutation Endrocrine Precocious puberty Multiple hormonal hyperactivity may be seen (eg.ovary, thyroid , adrenal glands , pituitary) Bone Polyostotic fibrous dysplasia(visible as radiolucent areas on X-ray) Patchy hyperpigmentation and café-au-lait patches (of very irregular outline) Skin Central Precocious puberty > Peripheral Pseudopuberty -Precocious puberty → predominantly in girls -average age → about 3 yrs -vaginal bleeding → 4 months of age -secondary sex characterstics → as early as 6 mo -suppressed level of LH and FSH (+) -there is no response to GnRH stimulation (leuprolide) -estradiol levels – normal to markedly elevated ( > 900pg/ml) -recurrent ovarian cysts (+) -functional ovarian cysts – often disappear -ovarian torsion may occour In girls -mense – more regular -fertility - documented In boys -precocious puberty - less common -testicular enlargement – fairly symmteric • Tx given • -letrozole • -tamoxifen • -spironolactone • -flutamide • -bicalutamide • -GnrH analogs Extra-gonadal manifestations Hyperthyroidism -male and female equal -present with mutinodular goitre -↑T3 and suppressed TSH levels Continued Cushing syndrome -bilateral adrenocortical hyperplasia → sexual precocity Increase secrection of growth hormone – gignatism or acromegaly -equal sex -serum growth hormone ↑ , prolacitn ↑ (50% associated with pituitary tumor Familial Male Gonadotropin - Independent Precocious puberty (Testotoxicosis) - Autosomal dominant - mutation of the luteinizing hormone receptor (LHCGR) gene, - puberty appear -2 -3 yrs of age - acclerated growth , early development of secondary sex charactersitc and reduce adult height Testes -slightly enlarged -Leydig cell maturation (+) , marked hyperplasia - Serum Testosterone level – marked elevated - LH level → prepubertal , pulsatile secrection of LH is absent - LH does not respond to GnrH agonist - Osseous maturation – markedly advanced Adrenal cortical tumors -Virilizing tumors > Feminizing or non secreting tumors CF -androgen hypersecrection → pseudoprecocious puberty , tall stature ,growth accleraton , precocious pubic hair , axillary hair In boys – growth of penis↑, prepubertal size testes In girls –clitoromegaly and labial enlargement -15-40% of adrenal cortical tumors have Cushing syndrome Tx -surgical removal Prognosis - often poor Mediastinal tumor associated with Klinefelter syndrome -mediastinal germ cell tumor – produce HCG so precicoucus puberty (+) Leydig cell tumors (GIPP) -asymmteric enlargement of the testes -more common in adult -10% - malignant -onset – 5 - 9 yrs old -Gyneocomastia -plasma level of testosterone – marked elevlated -FSH and LH suppressed Tx -surgical removal -resistant to chemoTx Testicular adrenal rests -mimic Leydig cell tumors -Usually bilateral - Assciated with indequate controlled congenital adrenal hyperplasia -salt losing (+) during adolescence or yong adult life Ovarian tumors - Most are benign - Present before 8yrs of age → signs of puberty - Synthesize estrongens , afew → androgens - Common estrogen producing ovarian tumor causig precocious puberty is – granulosa cell tumor - Isosexual precocious sexual development (+) associated with Benign ovarian cysts (estrogenic lesion of the ovary ) Juvenile Granulosa cell tumor -estrogenic menifestation -1-10% of all ovarin tumors -is benign -associated with multiple enchondromas (Olier disease) -associated with multiple subcutaneous hemangiomas (Maffuci syndrome) CF -observed in newborns -manifest with sexual precocity at 2yrs of age -mean age is 7.5yr -always unilateral -breast enlarged (premature thelarche) Continued-external genitals – resemble a normal girl at puberty -uterus – enlarged -white vaginal d/c followedby irregular of cyclic menstration -not ovulation -present with abdominal pain or swelling -pubic hair absent Investigation -U/s , CT -plasma estradiol levels → markedly elevated -FSH and LH suppressed -not respond to GnrH analog stimulation -(antimullerian hormone,inhibin B, 𝛼 fetoprotein)↑ -osseous maturation – moderate advanced Type IA pseudohypothyroidism with precocious puberty -temperature sensitive mutation of Gs protein -normal body temperature (37’C) Gs is degeraded result in PHP -in the cool temperature (33’C) →Gs mutation (+) ↓ Result in activation of LH receptor ↓ Precocious puberty Glucocorticoid receptor defect -point mutation or microdelection -↑ circulating corticotropin and cortisol -increase androgen synthesis CF (hypertension and hypokalaemic alkalosis) In girls, -hyperandrogenism can result in acne, hirsutism, menstrual irregularities, oligoanovulation, In boys, -infertility -precocious puberty Premature thelarche -usually in girls aged between 1 and 3 yrs -isolated breast development (never more than stage 3) -unilateral or asymmteric -NO other signs of puberty -Normal growth velocity for age -Normal bone age -Prepuberal gonadotrophin levels -Progress to puberty at normal age -benign condition -may be first sign of true precocious puberty -may be exogenous exposure to estorgen Investigation - ↑serum level of FSH ( GnrH stimulatin test) - ↓serum level of LH and estradiol - U/S –ovaries – normal in size - few small cysts (< 9mm) Premature Adrenarche isolated pubic hair (or any other androgen effects-body odor,acne, or axillary hair ) before 8 yrs of age in girls and before 9yrs of age in boys Continued- -premature pubarche -incrase high velocity -the timing of true puberty onset – generally unaffected -girls > males -no involvement of the gonads development -no involvement of breast development and testicular enlargement Gynecomastia prepubertal gynecomastia -may be unilateral -can cause discomfort -usually benign, self –limiting and idiopathic pubertal girls –d/t estrogen level androgen insensitivity syndromes - < 50 % of normal boys during early to mid-puberty (estrogen levels > androgens ) spontaneous resolve within 12-18 months -Klinefelter syndrome -estrogen producing andrenal and testicular tumors -Drugs – digoxin,methyldopa,ketoconazole and cannabis amphetamine abuse Delayed Puberty Girls Faliure of onset of any signs of puberty by 13 yrs Boys Faliure of onset of any signs of puberty by 14 yrs Causes of delayed puberty Constitutional delay of growth and puberty Hypothalamic or pituitary disorders -Hypogonadrotropic hypogonadism -Idiopathic -Pituitary tumors -Post-central irradiation -Post-intracranial surgery -Post-chemotherapy -Anorexia nervosa Systemic disease Kallman syndrome Gonadal dysgenesis Turner syndrome Hypothyroidism Constitutional Growth delay -one of the variant of normal growth -Length and weight measurements of affected children are normal at birth -growth is normal for the 1st -12 month of life -High is lower percentile during childhood -puberdal growth spurt is delayed Continued- -Detailed questioning about family h/o (history of short stature in childhood , delay puberty ) -bone age – normal in range Investigation -IGF-1 level ↓ for chronological age -GH response to provocative testing - lower than in children Hypogonadotropic hypogonadism (primary) Congenital -Follicle –stimulating hormone (FSH) and LH resistance -Mutation in steriod synthetic pathways -Gonadal dysgenesis -Klinefelter syndrome -Noonan syndrome -Cystic fibrosis Acquired -Cryptorchidism -Vanishing testes -chemotherapy -Radiation -Infection (mump) -Infraction (testicular torsion) -Trauma Secondary hypogonadotropic hypogonadism Congenital -Kallmann syndrome -Prader-Willi,Bardet-Biedl,LaurenceMoon-Biedl,Alstrom -Isolated HH at pituitary level -septooptic dysplasia -Idiopathic Acquired -Anorexia nervosa -Drug use -Malnutrition -Chronic illness -Hyperprolactinemia -pituitary tumors -pituitary infraction -infiltrative disorders(Histocytosis) -Hemosiderosis, hemochromatosis -Radiation Congenital Anorchia or testicular Regression Syndrome -sporadic -external genitalia - developed normally -cryptorchidism (+) -micropenis -testosterone level low ( < 10 ng/dL) -FSH and LH – marked elevated -HCG stimulation test – failed -serum level of AMH – undetectable or low Chemotherapy and Radiation-induced hypogonadism -germ cell damage ( eg cyclophosphamide) -infertility -azoospermia Radiation damage -dose dependent -Temporary oligospermia -permanent azoospermia Sertoli Cell-Only Syndrome (germ cell aplasia or Del Castillo syndrome) -sporadic and idiopathic -small testes -azoopermia -normal testosterone production -infertility Other causes of testicular hypofunction Testes atropy -manipulation of the testes during surgical procedures for correction of cryptorchidism , bilateral torsion of testes Acute orchitis -common in pubertal or adult males with mumps -subfertility -13% of cases -testosterone secrection – normal Testicular Dysgenesis syndrome -develops in intrauterine life from genetic as well as environmental factors -increased risk – cryptorchidism,hypospadias,hypofertility and testicular cancer CF -primary hypogonadism -testes and penis – abnormally small -secondary sexcharacterstics – fail to develop -Facial, pubic , axillary hair – scant or absent -epiphyses close later than normal (delay bone age ) -propotions of body – eunuchoid -us/Ls ratio < 0.9 Noonan syndrome -Puberty delayd -adult height is achieved by the end of the 2nd decade and usually reaches the lower limit of normal Klinefelter syndrome -Puberty delay -normal or nearly normal virilization -gynecomastia -spermatogenic arrest -azoospermia and infertility XX males -1:20,000 newborn males -male phenotype, small testes, small phallus and no evidence of ovarin or mullerian duct tissue -undescended testes and hypospadias -infertility -hypergonadrotropic hypogonadism Isolated Gonadotropin Deficiency -defect the GnRH synthesis in the pituitary -isolated gonadotropin deficiency (+) -other pituitary hormone levels are normal Kallmann syndrome -the most common form of HH -AR, X-linked , autosomal dominant -delections of the Xp22.3 -associated with anosmia or hyposmia -synkinesia , hearing loss,midfacial defects and renal agenesis -Cleft lip and palate , hypertelorism XX Gonadal dysgenesis -pure gonadal dysgenesis or pure ovarian dysgenesis -external genitals are normal -gorwth is normal -at pubertal age → sexual maturation fails to take place, plasma Gonadotropin level elevated , delay epiphyseal fusion may result in eunuchoid -Pelvic U/s – streak ovaries Mullerian agenesis or mayer-Rokitansky-Kuster-Hauser syndrome -mutation in WNT4 gene -gonadal dysgenesis -absence of mullerian – derived structures -unilateral agnesis -clinical signs of androgen excess -primary amenorrhoea -lack of breast development Tx -estrogen replacement Tx 45X/46,XY Gonadal dysgenesis -called mixed gonadal dysgenesis -short stature -90% has – normal male phenotype -some have female phenotype – (somatic signs of Turner Syndrome ) -frank ambiguity of the genitals in infancy Autoimmune ovarian faliure (type I autoimmune polyendocrinopathy-addison d/s, hypoparthyrodism, candidiasis) -60% of children older than 13 yrs of age Affect girls -may not develop sexually -secondary amenorrhoea (premature ovarian faliure) -ovaries –lymphocytic infiltration -circulating steroid cell Ab and autoAb to 21-Hydroxylase (+) Other ovarian defects Galactosemia -result in ovarian damage -FSH and LH ↑ Denys-Drash syndrome -gonadal dysgenesis -affect kidney and genitilia Ataxia-telangiectasia -ovarian hypoplasia -elevated gonadotropin -Gonadoblastomas -Dysgerminomas – occoured Congenital Adrenal Hypoplasia -X linked recessive pattern -mainly affect the male -Adrenal insufficiency -Hypogonadotropic hypogonadism -under developed reproductive tissues, undescended testicles, delayed puberty, and an inability to father children Turner Syndrome -short stature -ovarian insufficiency -lymphedema , webbed neck -shield chest ,cubitus valgus , short 4th metacarpal -hypoplastic nails ,renal abnormalies -left sided heart d/s(coarctation of aorta,bicuspid mitral valve) Red Flags Related to puberty -Pubertal changes in African-American girls beginning before age 6 yr (excluding isolated thelarche from birth to 2 yr of age) -Pubertal changes in white girls beginning before age 7 yr (excluding -isolated thelarche from birth to 2 yr of age) -Pubertal changes in all boys beginning before 9 yr of age -Absence of pubertal changes in girls by 13 yr of age -Absence of pubertal changes in boys by 14 yr of age -Neurologic signs and symptoms (headaches, visual disturbances) -Vaginal bleeding before breast development -Significantly asymmetric gonadal size in either sex (boys, by clinical examination; girls, by pelvic ultrasonography) -Testicular underdevelopment -Girls with advancing breast development but no androgen signs -Galactorrhea -pelvic mass SEXUAL DIFFERENTIATION DISORDERS-AMBIGUOUS GENITALIA -Virilization of a female (Female pseudohermaphrodite, 46 XX) -Undervirilization of a male (male pseudohermaphrodite, 46 XY) -True hermaphrodite (both ovarian and testicular tissue present) Causes Female pseudohermaphrodite (virilized) (46XX-DSD + ovaries) Fetal CAH 21-hydroxylase deficiency 11𝛽 –hydroxylase deficiency 3𝛽 –Hydroxysteroid dehydrogenase II deficiency Cytochrome P450 oxidoreductase (POR) Aromatase (P450arom or CYP19 ) deficiency Glucocorticoid receptor gene mutation Maternal. Virilizing tumors (adrenal , ovarian ) Virilizing drugs Male pseudohermaphrodite (undervirilized) (46 XY + testes) Defect in testes differentiation Denys-Drash syndrome , WAGR syndrome ,Delection of 11p13 Campomelic syndrome , SOX9 mutation , XY pure gonadal dysgenesis Mutation in SRY gene , Gonadal dysgenesis/agenesis Defect in testicular hormones CAH-3𝛽 -hydroxysteroid dehydrogenase deficiency ,Leydig cell aplasia Mutation in LH receptor ,lipoid adrenal hyperplasia 17-Hydroxylase/17-20-lyse deficiency Persistent mullerian duct syndrome Defect in androgen activity 5𝛼 –reductase deficiency Androgen insensitivity syndrome Smith-Lemli-Optiz syndrome True hermaphrodite (ovarian + testicular tissue ) 46 XX 46 XY Mosaic karyotypes,eg .46 XX/XY (chimera) , XO/XY Congenital Adrenal Hyperplasia -Autosomal recessive -mutations in the CYP21B gene located on chromosome 6) -various defects in the enzymes involved in the adrenal synthetic pathways. 21-hydroxylase deficiency The most common casue CF -Virilization of a female baby (cliteromegaly .etc) -Adrenal crisis may occur in first 1-2 weeks of life ( Classic form) -saltlosing ,progressive weight loss (through 2 weeks of age), anorexia, vomiting, dehydration -may present late with precocious puberty , advance bone age , tall stature in childhood (eventual short stature ) -Hypertension ,Hirsutism and skin pigmentation -precocious adrenarche ,menstral irregularity , infertility Hormones -ACTH ↑ -Aldosterone↓ -Testosterone↑ -Cortisol↓ -Androstenedione↑ Investigations -Plasma 17 –OH-progesterone↑ , plasma renin ↑ -Urine steriod profile –urine pregnanetriol ↑ -Serum electrolytes Na ↓ , K↑ , glucose ↓ -Karyotype -Pelvic USS(looking for female organs in a virilized female) Other variants 11𝜷 –hydroxylase deficiency -non salt losing , Na↑ , K↓ , BP↑ -Virilization -Diagnosis: 11-deoxycortisol ↑ 3𝜷 hydroxysteriod dehydrogenase deficiency -Salt –losing , Na ↓, K ↑ -virilization of girls , incomplete virilization of boys Diagnosis : elevated pregnenolone, DHEA,17-OH -pregnenolone Aromatase Deficiency -in genotypic females -46XX DSD -hypergonadotropic hypogonadism -enlargement of clitoris -posterior labial fusion at birth -large ovarian cysts (+) -elevated level of Gondotropins and androgens -low estrogen levels Campomelic syndrome -short-limbed dysplasia -usually lethal in early infancy -46 XY patients- exhibit female phenotype -some 46 XY - ambignous genitals -gonads – ovaries but histologically – both ovaries and testes WAGR Syndrome -delection of 1 copy of chromosome 11p13 -Wilm tumor -aniridia -genitourinary malformations -46 XY males (ranging from cryptorchidism to severe deficiency of virilization) -Gonadoblastoma -unexplain obesity XY pure Gonadal Dysgenesis(Swyer syndrome) -normal stature with female phenotype -at pubertal age – breast development and menarche fail to occour -hypergonadotropic primary amenorrhoea -mutation of SRY gene( X-linked dominant ) Leydig cell Aplasia -have female phenotype -mild virilization -no secondary changes at puberty -pubic hair may be normal -plasma testosterone level low , not response to hCG -LH -elevated Lipoid Adrenal Hyperplasia -Phenotype – Female -accumulaton of cholesterol and cholesterol ester -All serum steroid levels – low or undectable -corticotropin and plasma level renin level – quite elevated -acute adrenal crisis Persistent Mullerian Duct syndrome -Cryptorchidism -Testicular function – normal Ovotesticular DSD -both ovarin and testicular t/s (+) -ambiguous genitalia -usually sporadic (a) Prader stages. Prader 1: female external genitalia; Prader 5: male external genitalia. (b) Female newborn with 21OHD. It would be easy make a male sex assignment in an initial assessment (Prader 5). Algorithm for the diagnosis of a newborn with suspected CAH. Algorithm for the diagnosis of a child or adolescent with suspected 21OHD. Thank You