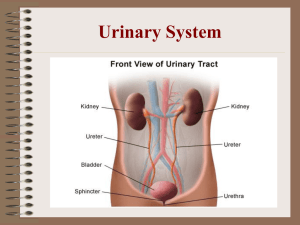
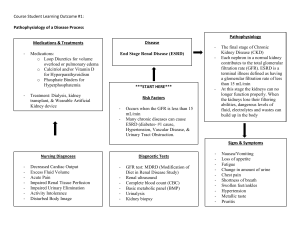
KIDNEY STUDY GUIDE Kidney Structure - Cortex – contains part of the nephrones - Medulla - Nephrons – where filtration takes place - Renal blood supply The Nephron – you do not make nephrons as you get older. All are made as baby. Those who get less and less nephrons as they age can end up having kidney disorders - Vascular components – blood flow goes into the kidney o Glomerulus – capillary network (blood vessels) § Has slits to help with filtration o Peritubular Capillaries - Tubular components: o Proximal Convoluted Tubule o Loop of Henle – where Na and H2O concentration occurs o Distal Convoluted Tubule o Collecting tubule Function of the Nephron Our capillaries Has very high pressure Whatever the body needs at the time the tubules absorb it GFR – glomerulus filtration rate - estimates how well kidneys are functioning - Rate of filtration – how much fluid is moving through the glomerulus - Normal 125mL/min Major Functions of the Kidneys - Waste Removal – unneeded fluids, biproducts of metabolism that we don’t need - BP Regulation & Fluid Volume - Hormone Function – MUST KNOW: How different things the kidney excretes can affect you hormone o RAAS system for regulation of blood pressure o Erythropoietin – kidneys produces a substance that helps with the production of red blood cells o Activation of IgG in reference to the kidney Waste removal: Urine - Clear, yellow-colored fluid produced by the kidneys - ~ 95% water & 5% dissolved solids - Contains metabolic wastes & few or NO plasma proteins, blood cells, or glucose molecules - Normally urine SHOULD not have any blood, protein or sugar Urine Formation Urine Formation - Involves: o Glomerular filtration § This capillary filters the blood into the bowman’s capsule and it will begin to move in the nephron. § Happens first through hydrostatic pressure (comes from the blood pressure) § Osmotic pressure (how much albumin/protein is in the blood that can cause a gradient) o Tubular reabsorption – everything that comes into your kidney § Reabsorption of electrolytes and nutrients that the body needs this to maintain consistency of an internal environment. § If the body needs to reabsorb an acid or base they can do that through here o Tubular secretion – everything that comes out your kidney § You loose a lot of volume, water, Na, k, and molecules. - The kidneys filter about 120-150 quarts of blood to produce about 1 to 2 quarts of urine, composed of wastes and extra fluid. Hydrogen ions are being excreted throughout the ENTIRE nephron - If you are loosing part of that, then that can affect your acid base balance Tubular Reabsorption - 99% Water reabsorbed back into the blood stream from nephron after it goes through the glomerulus - Active & Passive Transport o Glucose should be completely reabsorbed. It shouldn’t be passing through the urine. Glucose hitches a ride on sodium - Proximal Tubule Tubular Secretion - Extract materials from peritubular capillaries & vasa recta (blood vessels/capillaries around the nephron => urine - Eliminates undesirable amounts: urea & uric acid, excess K+ o Some urea is send back into the bloodstream - Controls blood pH Kidney & Urinary System Function Regulation Intrinsic - in the kidney itself - Kidneys can control function locally (intrinsic): Autoregulation of renal blood flow (RBF) - These intrinsic mechanisms maintain filtrate production so that the body can maintain fluid, electrolyte, and acid-base balance and remove wastes and toxins from the body. Extrinsic – related to outside the kidney - Ex. shock and trauma increase kidney function – you have les bp, and less perfusion o Urine output can drop to zero under these conditions - Control mechanisms that originate outside of the kidney; CNS and the Endocrine system (hormones – Angiotensin 2, ADH can produce vasoconstriction; dopamine, hydroxide, prostaglandin can vasodilate) o Certain drugs can be very toxic to the kidney – NSAIDS (ibuprofen, relieve) § Inhibits prostaglandin synthesis in the kidney, which causes reduction in renal blood flow and GFR § Patients who have kidney disease SHOULD NOT TAKE NSAIDS - CNS and hormones control systemic blood pressure by increasing or decreasing GFR to change systemic blood pressure by changing the fluid lost from the body. RAAS System – kidneys uses this to regulate bp. - Certain drugs target these areas – doctors will use it to treat high bp Hypothalamic Pituitary-Adrenal Axis - Starts in the brain Osmolarity and Volume – In selective reabsorption, sodium, amino acids and glucose are reabsorbed from the filtrate back into the blood - Homeostasis is achieved by using Na and H2O to maintain fluid volume o Increase Na and H20 can increase fluid volume and activation of ADH. Electrolytes The Kidneys and Diuretics – medications that will increase urine output. - They work on all sections of the nephrons - Keep watch of electrolytes such as potassium imbalances Regulation of Acid Base Balance - pH-means potential [power] of hydrogen Regulates the composition of pH of body fluids through reabsorption, elimination or conservation § H2O, H2O and Na+, K+, H+, Cl-, HCO3 o The kidneys will respond when there is an acid base imbalance by giving more bicarbonate to increase the pH in the body § Bicarb is filtered out and reabsorbed § H+ ions is lost in the urine All parts of the nephron secreted H+ o When the kidneys don’t function properly, you are living in a state of acidosis o - Regulation of Blood Pressure - Cardiovascular center (brain controlled) ↑or↓ bp by rapidly adjusting co/blood vessel diameter using: o The central nervous system § SNS – fight or flight – increases HR and vasoconstricts § P SNS – rest and digest – decreases HR, vasodialation o Baroreceptors – Nerve endings at the carotid aortic arch § They are bp sensors and very sensitive - The kidneys release hormones and other things for a longer-more sustained control of bp, how? o The renin-angiotensin- aldosterone system (raas) § Controls blood volume (bp) § And constriction of blood vessels (bp) by releasing hormones We will be focused on number the second one!! Secretion The kidneys secrete… - Erythropoietin (EPO) – a substance that kidneys will produce o EPO stimulates bone marrow to enable the production of red blood cells for the body § Able to synthesize this and give it to patients with this dysfunction - Enzymes o 25-dihydroxyvitamin D3 helps to convert inactive vitamin D to active vitamin D for calcium metabolism § Treats calcium imbalance in the bones - Renin o Converts angiotensinogen into angiotensin I § Part of the RAAS system to help produce aldosterone - Prostaglandins o Lipids that help regulate renal hemodynamics by controlling Na+ & H2O and help in regulating the renin-angiotensin system Excretion/Elimination They act as a filtration system Excretion - The kidneys play a major role in getting rid of: - Waste products - Foreign substances (poisons/toxins/etc.) - Pharmacokinetic elimination – medications and drugs Elimination - After the kidneys make the urine, it is then stored and carried out of the body by way of the Urinary System: o ureters o bladder – you’re able to consciously decide when to urinate o urethra – last section to cary urine Test of Renal Function Need to know if when something is elevated whether that is good or bad - Blood urea nitrogen (BUN) – ­ = issue with kidney - Creatinine – ­ = a very good indication of kidney disease - Creatinine Clearance – lab and urine test to compare and see how much creatinine the kidney if filtering out - GFR – Glomerulus Filtration Rate – used to stage kidney diseases (how bad they are) - Urine Specific Gravity – how concentrated the urine is o Important because, you need to know if the kidneys are filtering properly § Too concentrated urine – need of hydration § No concentration (clear urine) – sign of kidney dysfunction, DI (DIabetis Insipidus), drinking a lot of water - Urinanlysis Blood Urea Nitrate (BUN) - End product of protein metabolism from the liver - Blood levels regulated by the kidneys - 8 - 20 mg/dL is a normal level. o BUN higher than 20 mg/dL can affect renal impairment Causes of Elevated Serum BUN Levels - Dehydration - Urinary tract obstruction - Congestive heart failure - Recent heart attack - Certain medications - Shock - High protein diet – eating a lot of protein would leave a lot of bicarb in the bloodstream Serum Creatinine (SCr) - A chemical compound left over from energy-producing processes in your muscles (creatinine) - Normal range 0.7-1.5 depending on gender and build – should be low o Normal serum creatinine – you can rule out kidney disease o Elevated serum creatinine – most likely renal disease o Healthy kidneys filter creatinine out of the blood o Creatinine exits your body as a waste product in urine o Tells us about the function of kidneys - Causes of Elevated Serum Creatinine Levels o Kidney failure o Kidney infection o Glomerulonephritis – inflammation of kidney structures that filter blood o o Kidney stones – these can block the urinary tract Temporary elevations – causes can be multiple Glomerular Filtration Rate (GFR) – this is a blood test - GFR= total volume of ultrafiltrate formed by the collective kidney nephrons per minute - Approximately 125 mL/min of filtrate is formed each minute o Lower means glomerular isn’t functioning like it should - Regulated by: hydrostatic and osmotic pressure in the glomerular capillaries vs. Bowmans capsule - GFR is the best indicator of renal function! < 60 indicates kidney disease (it can be a very early stage) - This decreases with age due to loosing nephrons as you age Urine Testing Urine Specific Gravity - Measures concentration of solutes in the urine o Density of urine/ density of water - Measures the ratio of urine density compared with water density - Provides information on the kidney’s ability to concentrate urine - Normal=1.005-1.020 g/mL o ­ = dehydration o ¯ = well hydration or kidneys are not functioning very well - Tells you how well your kidney can concentrate Urinalysis (UA) - UAs are used to detect and assess a wide range of disorders, including: o UTIs o Kidney disease – shouldn’t be protein in the urine § That means there is damage in th e kidney where protein is able to fit through the small slits o Diabetes – shouldn’t be any glucose in the urine - UAs examine: o Appearance – urine should be light yellow, it shouldn’t be clear, amber, yellow, red or brown § Bilirubin makes the urine very dark – a sign of liver problems/disease o Concentration – helps indicate blood or protein in the urine o Content of urine – it can show bacteria and white blood cells § Sign that your body is trying to fight off an infection Urine output (UOP) and things in the urine – when examining things about the urine we must also look at this - Normal urine output (UOP) o 0.5 to 1.5 cc/kg/hour at least every 6 hours (at least 30cc/hour or 800-2L per day) - Excessive UOP o Frequency - frequent voiding more than every 3 hrs o Polyuria - 1 volume of urine voided - Poor UOP - o Anuria - means "without" urine o Oliguria - decreased UOP < 0.5 mL/kg/hour (less than 400mL in a day) Things that we can have in the Urine o Bacteria (bacteriuria) – would be a UTI o Protein (Proteinuria) – would be kidney disease or someone who is a risk factor for kidney disease o Blood (Hematuria) – can be from infection or a kidney stone o Sugar (glycosuria) – glucose gets filtered into the nephron initially, however it will end up going back to the bloodstream § If you already have a high blood sugar concentration in your blood you would pee out the excess glucose Disorders of Renal Function Types of Renal Function Disorders - Congenital and Inherited – can be born with them - Obstructive Disorders – something that is blocking the urine outflow or pressing something pressing o Ex. kidney stones - Urinary Tract Infections – major complication in pts in hospital - Disorders of Glomerular Function - Tubulointerstitial Disorders - Malignant Tumors Congenital or Inherited - Most common – Horseshoe Kidney o Where kidneys are fused at the base o Typically asymptomatic – you don’t have to treat or do anything to it - Inherited Cystic Kidney Disease o Polycystic Kidney Disease – Group of kidney disorders involving multiple cysts o First asymptomatic, then slow progression to kidney disease o Diagnosed with ultrasound or CT o Treatment = Supportive § Educate patient on lifestyle to changes to make sure they do not enter end stage renal failure • Ex. making sure they are not taking medications that can harm the kidneys • Making sure they are drinking enough water • Avoiding UTI’s Obstructive Disorders – something is obstructing - Anything that could potentially blocking the way of urine to go out o Examples – § A tumor § A stone (most common) – can form because of a obstructive disorder; urine is stagnant so it leads to formation of stones § A fibroid – scar tissue § A pregnancy § Scriptures – where there’s a tightening (scar tissue can form a scripture) - It can occur at any level of the urinary tract and at any age Causes damage by: - Stasis of urine, leading to infection or stone formation - Progressive dilation of renal collecting ducts and tubular structures, causing destruction and scarring o Tubes inside the kidneys are stretched and they are being scarred and destroyed o Once the nephron dies, you can’t restore it Hydronephrosis – swelling of the kidneys due to backflow of urine - “Urine-filled dilation of the renal pelvis and calices associated with progressive atrophy of the kidney because of obstruction of urine outflow” - Treatment – treat the cause! - Urine is backing up and goes to the kidney causing dilation. Dilation causes weakened walls making them more susceptible to damage such as sheering. - Expected to be seen in UTI’s - If you have on only one side it can go a while without being detected. Renal Calculi – Kidney stones - Most common cause of upper urinary tract obstruction! o Stone is hanging out in the urine pelvis, it moves to the ureter (this can be really painful because it is a tight spot) causing a blockage - 4 Types – the only way to know what type of stone you have is to filter it (MUST STRAIN IT – you wouldn’t know how to treat or prevent that kidney stone unless you strain it and see what it is) o Calcium (most common) – oxalate or phosphate § Pt may have high calcium levels due to parathyroid issues (hyperparathyroidism), not getting enough exercise or because of renal disease § There is oxalate in the blood. This oxalate binds with the calcium in the kidney and forms a stone o Magnesium ammonia phosphate – struvite § Only form with high urine pH o Uric acid – rare cause § Seen in obese patients, low pH (different types of stones form in different pH: when you find out what your stone is, you can either increase or decrease the urine pH) o Cystine - Clinical manifestations o PAIN! Renal Colic – a sudden severe pain whenever the hearing duct is stretched or when something is moving in there § People can have back pain, pain in the upper quadrants, on the sides of the body and radiate to the groin § Comes on suddenly, severely pain § You may be sweaty, throwing up or pale/clamy o Urinalysis may show blood, crystals, bacteria, will show pH § Blood – the stones are pretty sharp and can cause bleeding § Bacteria – usually the magnesium stones § pH – know if it is low or high o o Most will show on Xray CT- recommended with colic Renal Calculi – Requires 3 things to form: - Supersaturated urine – for it to be supersaturated your intravascular volume (dehydration) is low so your kidneys are allowing more water to be reabsorbed into the nephrons o There is not going to be a lot of water in the urine o REVIEW: Would the specific gravity be high or low if it were supersaturated? Answer: It would be high… greater than 1.03 High specific gravity = supersaturation o Supersaturated urine increases the risk of kidney stones - A nidus (something in the middle of the stone) or nucleus that facilitates crystal aggregation (small cluster of crystals such as calcium oxalate) o There is some substance that is sticky § Ex. bacteria that want stuff to stick to it § Ex. oxalate from the blood binds with calcium from the supersaturated urine - Lack of natural stone inhibitors (magnesium and citrate -ONLY NEED TO KNOW that this is a stone inhibitor) o Your body is aware that this is happening, so it is releasing inhibitors to stop it Renal Calculi – only way for it to come out is to pee it out or have surgery - Treatment- usually supportive – provide heating pads, promote drinking water so they can void, pain medication (sometimes need narcotics) o Pain, UTI treatment, try to change urine pH (ex. cranberry juice can make urine more acidic) o Most stones <5 mm pass spontaneously o Strain urine** o May need stone removal if large stone Urinary Tract Infections - Inflammation of the bladder and/or the kidneys caused by bacteria that moves up the urethra into the bladder o If you did a urine sample you may see some bacteria and blood o You can treat it with antibiotics, but it may not get better § Still at risk for stones and it takes antibiotics a long time to treat stones o Much more common in women – vaginal opening is close to anus opening - Acute Pyelonephritis is a bacterial infection causing inflammation of the kidneys o Very dangers… bacteria traveled all the way up to the kidney OR it came in through the blood stream which is rare o One of the most common diseases of the kidney o Occurs as a complication of an ascending UTI which spreads from the bladder to the kidneys and their collecting systems § Bacteria usually comes in through the urethra o +Bacteria in the urine- Usually gram-negative (commonly E.coli) § It is good to practice good hygiene • tell girls to wipe front to back o Referred pain-flank pain - What causes a Urinary Tract Infection (UTI)? o bacteria infect any part of the urinary tract (kidneys, ureters, bladder and urethra) o UTIs most often affect the bladder. - An uncomplicated UTI (cystitis – bladder infection) o is an infection in the lower urinary tract, the bladder and urethra. § Usually can treat it with antibiotics and it will go away - A complicated UTI (pyelonephritis – kidney infection) o is when the infection extends beyond the bladder and toward the kidneys-more serious. o Seen in pregnancy, after menopause, and when there are other issues, such as kidney stones o Pyelonephritis (kidney infection) Catheter-Associated Urinary Tract Infections - Urinary catheter- most common cause of nosocomial (hospital caused infection) UTI. Why?? o Make sure you’re installing catheter with sterile technique and clean with aseptic technique o The longer the catheter stays in, the more bacteria grows around it. The bacteria can travel up the vagina and enter the urethra o It’s good to change out change out catheters and limit its use o The catheter bypasses our body’s normal protective mechanism (washing out) – you’re not able to wash out by peeing. UTI Risk factors - Not washing up after sexual intercourse - Medications such as oral contraceptives - Pregnancy - Diabetes – bacteria loves sugar. If you have sugar in your urine it will attract bacteria o Bacteria also loves certain type of yeast Symptoms of a UTI - Frequent urination - Dysuria – burning/painful urination - Cloudy looking urine - Pain in pelvic area - Blood in urine - Strong smelling urine Review: What type of results do you think you would see on a urine analysis for a UTI? Answer: Bacteria and nitrates Disorders of Glomerular Function - Glomerulonephritis- Inflammatory process involving the glomerular structures o Glomerular capillaries nd - 2 leading cause of death is kidney failure worldwide – most common in the US is HTN and diabetes - Types: o Immunologic – your immune system is attacking itself § Forms immune complexes that get clogged up o Nonimmunologic (Metabolic, hemodynamic, and toxic) § Substances make complications of diabetes and other diseases o Hereditary Glomerular Disorders – an umbrella term to describe damage to the glomeruli (acute/chronic) - Primary glomerular disease – only causes damage in that area in the kidneys, not in the whole body o Disease process that causes damage within the kidneys but only to the kidneys (nonsystemic) o Cause usually idiopathic but likely an auto-immune mediated process - Secondary glomerular disease o Damage to the glomeruli caused by a systemic disease (diabetes, lupus, sickle cell) more common - **Regardless of the type, if glomerular disease goes untreated it will become chronic and may lead to end stage renal failure Chronic Glomerulonephritis - Causes o Repeated acute glomerulonephritis episodes (chronic injury to the tubules) o Hypertension nephrosclerosis – hardening of the arteries to the kidneys (disease) o Hyperlipidemia – high cholesterol o Secondary glomerular disease; Lupus, DM, Goodpasture syndrome (rare/autoimmune disorder-antigens attacks kidneys [and lungs]) - Pathophysiology o Glomeruli injury-shrinks the kidneys § The kidneys atrophy down o Bands of scar tissue build up-kidneys become rough and irregular (fibroids) o Renal arteries can become thickened o Poor renal function=↑BUN/SCr, ↓ UOP - Starts as AKI and Progression often leads to CKD and… o Hyperkalemia o Metabolic acidosis o Anemia o Hypoalbuminemia o Hyperphosphatemia and hypocalcemia Glomerular Disorders - Nephritic syndromes o Caused by acute glomerular inflammation o DECREASE in glomerular permeability, hematuria, decreased GFR, fluid retention, and nitrogenous waste accumulation o Can be caused by post infectious GN (certain strains of staph group A- think untreated strep throat) - Nephrotic syndromes o INCREASE in glomerular permeability, massive loss of protein in urine peeing out all the protein (proteinuria >3.5 g/day), hypoalbuminemia, generalized edema, and hyperlipidemia (cholesterol >300) § REVIEW: What do you think happens when you loose all your proteins in your urine? - Answer: The osmotic pressure is way less so the water is seeping out of the capillaries. You don’t have enough water to hold it in, causing edema. o Not a specific glomerular disease, but a constellation of clinical findings r/t o You would see edema Rapidly progressing glomerulonephritis o Severe glomerular injury without specific cause – possibly immune? Chronic glomerulonephritis o Small kidneys with sclerosed glomeruli o Develops insidiously and slowly progresses to CKD Tubulointerstitial Disorders - Part of the nephrons that contain the tubules is involved - Affect the tubules and the surrounding area of the kidneys - Can be acute or chronic - Include: o Acute Tubular Necrosis (ATN) § Tubules are damaged from lack of oxygen/blood flow, and can cause kidney failure • Can be caused by anything that decreases blood flow to the kidney (heart attack, shock) o Renal Tubular Acidosis (RTA) § Defects in reabsorption of bicarbonate ions or excretion of hydrogen ions- the kidneys cannot balance acid-base levels effectively • Can be hereditary or acquired • Treatment – giving them alkaline therapy since they are acidic - Acute and chronic Pyelonephritis – interstitial disorders - Effects of drugs and toxins Acute Kidney Injury (AKI) and Chronic Kidney Disease (CKD) Also known as Acute renal disease - Prerenal – lack of perfusion, decreased circulation causes decreased blood pressure to the kidneys o ** prerenal cause can turn into an intrarenal problem, § If you have a prolonged lack of circulation, blood flow to the kidney– eventually the kidneys is not going to have the needed blood flow to function properly] o THINK HEART ISSUE o Causes § Severe volume depletion § Hypotension § Sepsis § Shock § Massive loss of blood § Over diuresis (volume depletion) § Heart failure § Cirrhosis § Bilateral renal stenosis § Nephrosclerosis – hardening and narrowing of the renal arteries • Leads to slow, progressive kidney disease • Causes: ◦ long-standing, poorly controlled hypertension ◦ DM can also cause this (called diabetic nephropathy) • Symptoms: ◦ Asymptomatic early in disease course ◦ Uncontrolled HTN from the AKI ◦ Uremia Renal artery stenosis (RAS)- a narrowing of the renal arteries • Result of atherosclerosis-hardening of the arteries due to gradual plaque buildup • Causes: ◦ Same as heart disease and atherosclerosis: DM, HTN, morbid obesity, smoking, ◦ Can lead to clot formation (d/t narrowed blood vessels) ◦ After AKI-can cause further HTN as well Intrarenal – a direct injury to the kidneys o Its not that the heart is not pumping the blood o It is the glomerulus is not functioning properly o INSIDE THE KIDNEY ITSELF o Common causes § Acute tubular necrosis § Prolonged renal ischemia § Nephrotoxic drugs § Intratubular obstruction § Acute glomerulonephritis § Acute pyelonephritis Postrenal – obstruction o Common causes § BPH or prostate cancer § Cervical cancer § Retroperitoneal disorders § Pelvic mass § Bladder masses § Neurogenic bladder § Kidney stones § - - Phases of AKI - Onset o Initial insult to cause the AKI o Where the tubule injury occurred o Examples - When that stone first got there, the time when you fell into heart failure and first fell into AKI - Oliguria (decrease in unrine output) o ↑serum concentration of substances normally excreted by kidneys and decrease in urine output - Diuresis – o Gradual ↑ in UOP & stabilization of lab values. Uremic symptoms may still be present along with hyperkalemia o Kidneys are starting to put out urine now (heal) and labs are looking a little better - Recovery – o Tubular edema resolves and renal function improves, normalization of fluid and electrolytes o GFR is almost at its normal range Outcomes of Kidney Injury Sign, Symptoms & Clinical Manifestations - Decreased Output - Fluid Retention - Drowsiness – all the toxins cause neuro changes - SOB – from retention of all that fluid - Fatigue - Confusion - Chest Pain - Lab changes? Whenever you’re assessing your patient with kidney disease, you want to listen to their lungs. Not being able to eliminate will cause fluid retention and fluid can back up into the lungs - Can hear crackles Also assess for edema in: - Legs/ankle/feet - Scrotum REVIEW: In renal failure think about acid base. Patients in renal failure are acidotic because they lost a lot of hydrogen ions, and they can’t regulate the balance. What might you notice about the respiratory system in these patients if they are trying to compensate? Answer: Carbon dioxide is an acid. The body is acidic, so the patient is hyperventilating trying to blow off all that acid. They will become Respiratory Alkalosis. Clinical Manifestations of Kidney Disease - ↓GFR ↑BUN ↑ SCr - Sodium & Water Retention – GFR has decreased and they are retaining water - Hyperkalemia – body is not able to excrete K - Calcium & Phosphorus Imbalances – kidney is working hard to get rid of phosphorus. When you have a high phosphorous, you’ll have a low calcium - Renal Osteodystrophy – you have a low calcium so your parathyroid gland is going to push out more parathyroid hormone, more of the calium is going to be reuptake from your bones cause them to thin and break - pH imbalances – KIDNEY DISEASE IS ACIDOTIC - Anemia & Poisons – erythropoietin is not being excreted causing low blood counts - Azotemia and Uremia – certain toxins can be in the bloodstream, causing itchinesss Sodium & Water Retention - Kidneys lose ability to concentration or dilute urine - Retaining sodium & water o Increased risk for edema, HF, and HTN o Activation of RAAS and aldosterone secretion can increase BP - Losing sodium & water o Develop hypotension & hypovolemia o Exacerbated by vomiting and diarrhea Hyperkalemia – potassium levels increase (check EKG’s for cardiac arrythmias) Calcium & Phosphorus Imbalances: (C+ and PO4 are usually found together) - Poor Vitamin D levels/absorption o Impaired ability for the parathyroid hormones to active vitamin D and thus they are at a loss o Vitamin D is activiated in the kidney - Hypocalcemia o Causes calcium to leave bone and changes in bone structure and calcification in vessels o Can have bone problems - Hyperphosphatemia o Decreased renal function makes it hard for kidneys to excrete phosphorous thus it builds up. o High phosphorous - Renal Osteodystrophy o Due to Ca and P imbalance, bone disease also develops o Ca+ gets removed from the bones to “compensate” Imbalances in pH, Anemia, Poisons - Bicarbonate (HCO3-) o The body cannot get rid of enough acid through the urine, so CKD patients live in a constant state of acidosis o Long term: bone and muscle loss, hyperglycemia, worsened CKD, death - Anemia o CKD -↓ erythropoietin (EPO) production, thus shortening the life span of the RBCs (ANEMIA) - Ammonia build up o Ammonia-a nitrogen waste compound that is normally excreted in the urine. o BUT…..Renal patients lose the of ability to excrete nitrogen so Ammonia (NH3-) builds up in the blood Azotemia (more of clinical symptoms) and Uremia (more of findings – in the bloodstream) – both mean excess waste in the blood - Can occur in prerenal, intra-renal, or post renal failure Chronic Kidney Disease and End-Stage Kidney Disease - The first stage you don’t have any symptoms, just lab findings that looks questionable o You’re having decreased renal function - End stage renal failure – you don’t have function in your kidneys o You have to do either kidney transplant or dialysis to filter out your blood Most Common Causes of Kidney Disorders - Uncontrolled HTN- (modifiable risk factor) o Cuts off normal blood supply to the kidneys o Can cause Nephrosclerosis-hardening of the renal arteries - Uncontrolled Diabetes AKA-Diabetic nephropathy (modifiable risk factor) o Develops over years o High glucose levels cause narrowing of the blood vessels/damages the glomeruli o Kidneys can’t handle all the glucose – it releases in the urine - Heart Disease/Atherosclerosis (modifiable risk factor) o Can decrease blood flow to the kidneys o Build up plaque in the renal arteries (Renal Artery stenosis) - Obesity (modifiable risk factor) o Puts people at risk for HTN, DM, heart disease, etc. - Smoking (modifiable risk factor) o Increases risk for developing heart disease-decreasing blood flow to the kidneys o Also increases the risk of ALL cancers (Kidney cancers in this case) - Family history o Non-modifiable risk factor…. REVIEW: Why does my patients with diabetes need urine testing every year for microalbumin? Answer: Microalbumin is a urine test that will show small particles of protein that won’t be detected on a dip stick. It shows they are at risk of kidney disease. GFR Decreases With The Progression Of CKD, but Serum Creatinine And BUN Increase REVIEW: Which one is more specific to kidney disease? Answer: Serum Creatinine Clinical Manifestations of CKD - Accumulation of nitrogenous wastes – they are going to feel sick and be itchy - Alterations in water, electrolyte, and acid–base balance - Mineral and skeletal disorders (Calcium and phosphorus metabolism) - Anemia Management of Chronic kidney disease (CKD) Treatment of CKD - Conservative – risk factor reducrion o Measures to prevent or delay loss of remaining renal function o Assist the body in compensating for the existing impairment o Vitamin D supplementation (increase Ca+ absorption) o BP control, Glucose control, diet changes, modifiable risk factor reduction o Avoid nephrotoxic medications § NSAID § Chemotherapy agens § Certain antibiotics - Renal Replacement Therapy o Indicated for advanced uremia and when serious electrolyte problems present o Dialysis or Kidney transplantation Renal Replacement Therapy Principles of Dialysis - Diffusion o toxins/waste removed by diffusion-movement of molecules from an area of high concentration to low concentration - Osmosis o excess fluid is removed using osmosis-net movement of solvent molecules through semipermeable membrane from area of low solute concentration to area of high solute concentration - Ultrafiltration o fluid moves from area of high pressure to area of lower pressure and helps to manage fluids and electrolytes - Anticoagulant agents o often used to prevent clotting of the circuits - “Cleansed” is returned to the patient Hemodialysis – filtration of the blood - Indications o Short term use in acutely ill patients until kidney function resumes (AKI) o Long term use in patients with advanced CKD/ESRD - Timing o 3 days a week (M/W/F or T/R/S) o 3–5-hour sessions - Purpose o Extract toxic nitrogenous substances o Remove excess fluid - ** Patients on long term dialysis DO NOT MAKE URINE (or very little) Continuous Renal Replacement Tx - Indicated for hemodynamically unstable patients with: o Fluid overload due to oliguric kidney disease o Life threatening electrolyte imbalance o Drug overdose o Major burns with compromised renal function o Clotting of the hemofilter can occur o Hemodynamically unstable patients-Hypotensive episodes during regular HD Peritoneal Dialysis (PD) – not as effective as hemodialysis - To remove toxins and waste products through the peritoneum - The peritoneum acts as semipermeable membrane - Dialysate is infused by gravity into peritoneal cavity for specific time - After dwell time, fluid drains by gravity into drainage bag