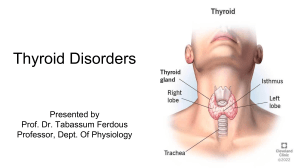
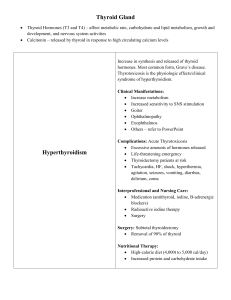
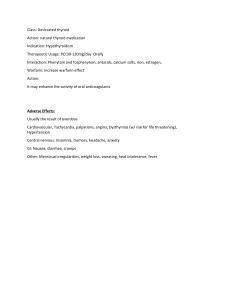
Ch 31: Thyroid and antithyroid drugs Thyroid function: • Thyroid gland lies across the larynx in front of the thyroid cartilage. • Responsible for secretion of thyroxine (T4), triiodothyronine (T3) and calcitonin which are essential for proper regulation of metabolism • Parathyroid glands are made up of encapsulated cells responsible for maintain adequate calcium levels in the ECF • T4 and T3 are produced through the coupling of iodine and the amino acid tyrosine o Iodide is obtained in diet (we need 1 mg/week) o In the blood stream iodide is converted to iodine • Iodine is combined with tyrosine to make diiodotyrosine, when two of these molecules combine thyroxine (T4) is formed • When coupling of one diiodotyrosine and one monoiodotyrosine combine if makes triiodothyronine (T3) • Both T3 and T4 are stored in follicles in thyroid gland in a complex with thyroglobulin • When the thyroid is signaled the thyroglobulin-thyroid hormone complex is broken down to release T3 and T4 into circulation o This process is triggered by thyroid-stimulating hormone (TSH) also called thyrotropin o Released from the anterior pituitary gland when T3 and T4 blood levels are low • Thyroid hormones are responsible for: o regulating basal metabolic rate o lipid and carb metabolism o essential for normal growth and development o control thermoregulatory center in brain Patho of hypothyroidism: • 3 types of hypothyroidism • Primary: o Stems from abnormality in the thyroid gland itself o Occurs when thyroid gland can’t perform one of the functions o Most common • Secondary: o Begins at the level of pituitary gland and results from decreased TSH secretion (which is needed to signal T3 and T4) • Tertiary: o Caused by reduced level of thyrotropin-releasing hormone from the hypothalamus o This causes reduced TSH and reduced thyroid hormone levels • s/s of hypothyroidism: o cold intolerance, unintentional weight gain, depression, dry brittle hair/nails, fatigue • hyposecretion of thyroid hormone during youth may lead to cretinism (low metabolic rate, retarded growth and sexual development, possible mental delays) • hyposecretion as an adult may cause myxedema (condition manifested by decreased metabolic rate, loss of mental and physical stamina, weight gain, hair loss, firm edema, yellow dullness of skin) • some forms of hypothyroidism may result in formation of goiter that results from overstimulation of elevated levels of TSH because there is little or no thyroid hormone • amiodarone is a common drug that can cause hypo and hyperthyroidism Patho of hyperthyroidism: • excessive secretion of thyroid hormones • disease known to cause hyperthyroidism include Graves’ disease (most common cause) and Plummer’s disease (toxic nodular disease) (least common cause) • thyroid storm is a severe and potentially life-threatening exacerbation of symptoms normally induced by stress or infection • results in overall increase in metabolism • s/s: diarrhea, flushing, increased appetite, muscle weakness, fatigue, palpitations, irritability, nervousness, sleep disorders, heat intolerance, altered menstrual flow Thyroid replacement drugs • monitoring of serum TSH and free thyroid hormone levels is required to determine the appropriate dose • MOA: o Work in the same manner as endogenous thyroid hormones • • • • o Work to induce changes in the metabolic rate (includes rate of protein, carb, and lipid metabolism) and also to increase O2 consumption, body temp, blood volume and overall cellular growth and differentiation o These drugs also stimulate the CV system by increasing the number of myocardial beta adrenergic receptor to increase the sensitivity of heart to catecholamines and increase CO o These hormones also increase renal blood glow and GFR (diuretic effect) Indications: o Given to replace what the thyroid gland itself cannot produce to achieve normal levels (euthyroid) o Fiagnosis of suspected hyperthyroidism o Prevention/ treatment of various types of goiters o Used in replacement hormonal therapy for pt who had surgical removal of thyroid or thyroid destroyed by radioactive iodine (cancer tx) o During pregnancy: hypo is treated with dose adjustments Q4weeks to maintain TSH level at lower end of normal (hypo may reduce fetal growth) Contraindications: o Drug allergy o Recent MI o Adrenal insufficiency o Hyperthyroidism Adverse effects: o Usually result of OD o Most significant: cardiac dysrhythmia w/ risk of fatal irregularities o Other affects: tachycardia, angina, hypertension, insomnia, tremors, HA, anxiety, menstrual irregularities, weight loss, heat intolerance Interactions: o Enhance activity of oral anticoagulants o Cholestyramine binds to thyroid hormone in GI tract (can reduce absorption of both drugs) o Food can reduce absorption of levothyroxine (take on empty stomach and in the AM) o Phenytoin, fosphenytoin, antacids, calcium salts, iron, estrogen: can all reduce levothyroxine effects o Levothyroxine + warfarin: increase warfarin effects • Drug profile o Levothyroxine § Pregnancy category A § Chemically pure (meaning its effects are more predictable) § Long half life: only admin once a day § Taken PO in AM 30-60 minutes prior to food § Dosed in mcg (question if higher than 200 mcg) Antithyroid drugs • Aimed to treat the underlying cause • Beta blockers are used to treat the symptoms • MOA: o Act by inhibiting the incorporation of iodine molecultes into the amino acid tyrosine ( a process required to make the prescursors of T3 and T4) o These drugs impede the formation of thyroid hormone o PTU inhibits the conversion of T4 and T3 in the peripheral circulation o Primarily limited to the thyroid gland • Indications o Hyperthyroidism o Prevent thyroid hormone surge after radioactive iodine therapy o Long term admin of these drugs in Graves’ disease may induce spontaneous remission o Surgical resection of thyroid often used in pt who are intolerant to med and pregnant women (when drugs and radioactive iodine are CI) • Contraindications o Drugs allergy o Pregnancy (PTU can only be used in first trimester) • Adverse effects o Liver and bone marrow toxicity o HA, vertigo, N/V/D, smoky urine, decreased urine output, myalgia, increased BUN and Serum creat levels, enlarged thyroid gland, nephritis • Interactions o Bone marrow suppressants can cause additive leukopenic effects o Anticoagulants can have increased effects • Drug profile o Propylthiouracil § Pregnancy category D except for 1st trimester § 2 weeks for symptoms to improve § Po 50 mg Nursing process • Assessment o VS o T3, T4, TSH levels prior to and during therapy o Past medical history o Cardiac history (dysrhythmias) o Drug interactions o Antithyroid drugs § Assess for precipitating causes of thyroid storm (stress or infection) • Implementation o Give at same time every day o Take in the morning (30-60 min before breakfast) o Avoid otc preparations with iodine, antacids, vitamins, iron or calcium containing meds w/in 4 hour time frame o Avoid salt containing foods o DC thyroid medication 4 weeks before undergoing radioactive iodine isotope studies o Teach to report fever, sore throat, bleeding, skin eruptions (liver toxicity) o Watch for s/s of hypothyroidism (unexplained weight loss, loss of mental/physical stamina, hair loss, firm edema, yellow skin) • Evaluation o Thyroid replacement drugs effectiveness can be seen in the disappearance of hypothyroid symptoms § Improved energy levels, mental and physical stamina o Clues on inadequate dose: return of symptoms o Antithyroid drugs effectiveness include return to normal status § Watch for leukopenia and s/s of hyperthyroidism