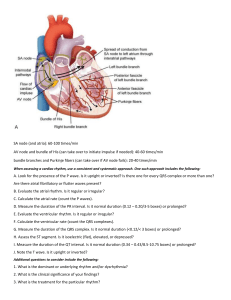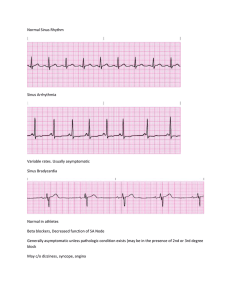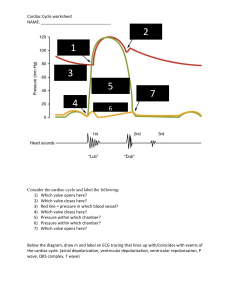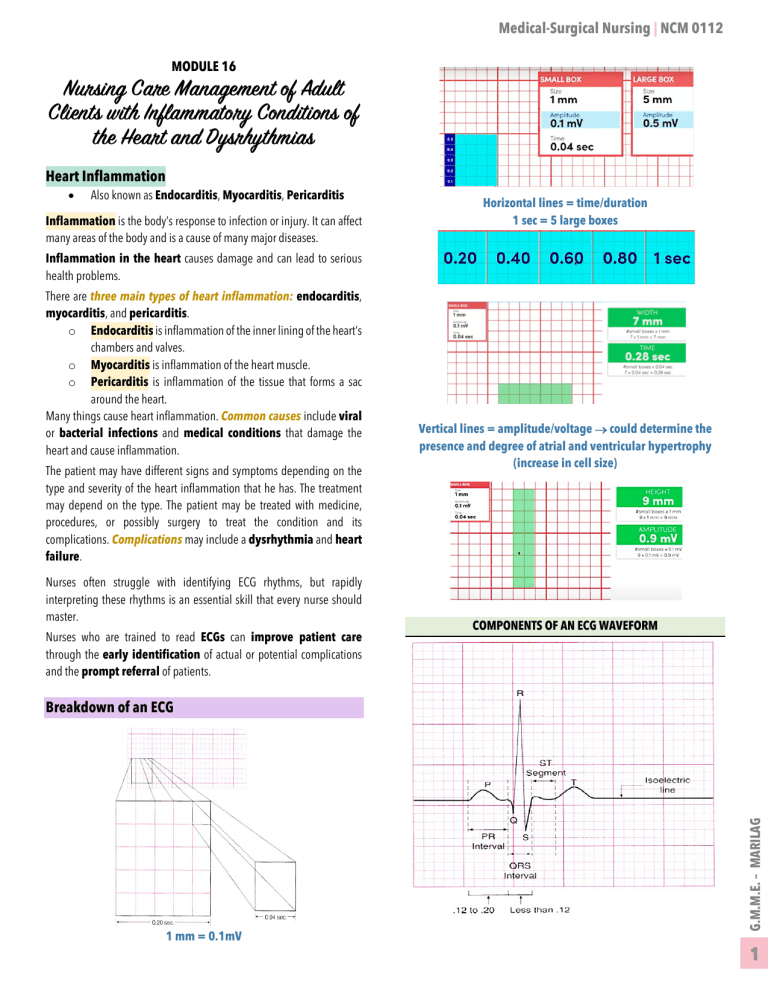
Medical-Surgical Nursing | NCM 0112 MODULE 16 Nursing Care Management of Adult Clients with Inflammatory Conditions of the Heart and Dysrhythmias Heart Inflammation • Also known as Endocarditis, Myocarditis, Pericarditis Inflammation is the body’s response to infection or injury. It can affect many areas of the body and is a cause of many major diseases. Horizontal lines = time/duration 1 sec = 5 large boxes Inflammation in the heart causes damage and can lead to serious health problems. There are three main types of heart inflammation: endocarditis, myocarditis, and pericarditis. o Endocarditis is inflammation of the inner lining of the heart’s chambers and valves. o Myocarditis is inflammation of the heart muscle. o Pericarditis is inflammation of the tissue that forms a sac around the heart. Many things cause heart inflammation. Common causes include viral or bacterial infections and medical conditions that damage the heart and cause inflammation. The patient may have different signs and symptoms depending on the type and severity of the heart inflammation that he has. The treatment may depend on the type. The patient may be treated with medicine, procedures, or possibly surgery to treat the condition and its complications. Complications may include a dysrhythmia and heart failure. Nurses often struggle with identifying ECG rhythms, but rapidly interpreting these rhythms is an essential skill that every nurse should master. Nurses who are trained to read ECGs can improve patient care through the early identification of actual or potential complications and the prompt referral of patients. Vertical lines = amplitude/voltage ® could determine the presence and degree of atrial and ventricular hypertrophy (increase in cell size) COMPONENTS OF AN ECG WAVEFORM 1 mm = 0.1mV G.M.M.E. – MARILAG Breakdown of an ECG Medical-Surgical Nursing | NCM 0112 PR Interval (PRI) • • • • Time at which impulse travels from the SA node to the atria and downward to the ventricles = conduction delay in the AV node Normally 0.12-0.20 seconds Measured from beginning of P wave to the end of the R segment Measured from beginning of P wave and beginning of QRS (P WAVE + PR SEGMENT) hyPeRkalemia = prolonged PR interval QRS Complex • • • • There is no distinctly visible wave that shows atrial repolarization in the ECG, yet it occurs during ventricular depolarization (QRS complex). Because the wave of atrial repolarization is relatively small in amplitude (i.e., has low voltage), it is masked by the much larger ventricular-generated QRS complex. • Ventricular depolarization 0.04 to 0.11 seconds R wave = 25mm in V5, V6 = ventricles Generally tall R waves are a sign of left ventricular hypertrophy (R wave greater than 25mm in V5, V6 = precordial leads) note however that, in order to be confident about the diagnosis of left ventricular hypertrophy, there should also be inversion of the T wave in these leads Tall wave is common in young, thin people and athletes P Wave Atrial depolarization Approximately 0.11 seconds in length <2.5 mm in height ST Segment • Time period between depolarization and repolarization of ventricles • Measured from end of QRS complex to beginning of T wave • Normally isoelectric (baseline) = negative and positive forces are equally balanced Notched (w/ division) = 1 atrium is larger than the other IF INCREASED: enlarged atria or forceful contraction of the atria G.M.M.E. – MARILAG • • • Medical-Surgical Nursing | NCM 0112 • Elevation or depression of the ST segment indicates an abnormality in the onset of recovery of the ventricular muscle usually because of an injury INTERPRETATION OF THE ECG ST segment elevation (chair-like image) = MI Long lead II is usually checked (from RA to LL), the same with the heart conduction T Wave • • • • • • • Ventricular repolarization Normally upright and 1/3 of height of the QRS complex Any condition that interferes with atrial repo may cause the T wave to invert HKTG = Potassium imbalances ­Potassium = ­T wave Usually rounded Flat or inverted: hypokalemia or myocardial ischemia Tall peaked: hyperkalemia Hyper-acute: MI Artifacts • Abnormal waves and spikes in an ECG that result from sources other than the electrical activity of the heart • Interfere and distort components • Make evaluation difficult or impossible *Check patient’s status ® check the machine (pads/wires may not be properly connected/attached) QT Interval • Measured from beginning of QRS to end of T wave • QT interval varies with heart rate, gender, and age • Normally less than 0.40 seconds U Wave • Sometimes follows a T wave • Appears to represent repolarization of the Purkinje fibers • Usually in the same direction as T wave Presence of U wave = hypUkalemia (hypokalemia) • • • ALTERNATING CURRENT INTERFERENCE: Extrinsic electric sources due to io improper grounding of the electrical equipment CHAOTIC TRACING: Poor contact with skin, dried electrode paste or jelly = using water-based jelly WANDERING BASELINE: due to anxiety, pain, restlessness, heavy breathing = check patient’s status G.M.M.E. – MARILAG Prolonged QT interval = hypocalcemia Chvostek’s sign & Trousseau’s sign Medical-Surgical Nursing | NCM 0112 4. Measure PR Interval = N: 0.12-0.20 secs 5. Measure QRS Duration = N: 0.04-0.11 secs; 25mm in height 6. Measure QT Interval = N: <0.40 secs 7. Examine ST Segment deviation = N: isoelectric (elevation or depression means abnormality in the onset of recovery of the ventricular muscle) 8. Examine T Wave = N: upright, 1/3 of the QRS complex, rounded 2. Determine the heart rate a. 6-Second Strip Method i. Have a six second strip (30 large boxes), count the QRS complexes (ventricular rhythm) and multiple by 10. ii. Have a six second strip (30 large boxes), count the P waves (atrial rhythm) and multiple by 10. NORMAL: atrial rate = ventricular rate iii. For accuracy, timing should begin on the P wave or QRS complex b. (shortcut method) Count the number of small boxes within an R-R interval and divide 1500 by that number or count the number of large boxes between within an R-R interval and divide 300 by the number. = for regular rhythms only c. The Box Method i. Find a QRS complex that lands on a heavy line. ii. Place the following values on succeeding heavy lines. (300-150-100-75-60-50-43-37-35-30) iii. If the next QRS complex falls on a heavy line, assign the appropriate rate for it. 3. Examine the P wave a. P wave should precede every QRS b. All P waves should appear the same § § § § § § § § Heart rate = YES Rhythm/regularity = YES Impulse conduction time intervals = YES Abnormal conduction pathways = YES Pumping action = NO Cardiac output = NO Blood pressure = NO Cardiac muscle hypertrophy = YES Which of the following is true regarding normal sinus rhythm? a. It has an inherent heartbeat of 40-60 beats per minutes (60-100) b. it is a result of electrical impulse initiated by the AV node (SA) c. it is best characterized by the presence of ectopic beats (none) d. P-R interval is 0.12-0.20 seconds Normal Sinus Rhythm (NSR) • • • • • Ventricular and atrial rate: 60-100 bpm (SA node firing rate) = initiated by SA node (primary pacemaker) Heart rhythm: regular QRS shape and duration: usually normal but may be regularly abnormal P wave: normal and consistent shape (has normal intervals with no aberrant or ectopic beats P:QRS ratio: 1:1 G.M.M.E. – MARILAG 1. Determine the heart rhythm 5 large boxes = 1 sec strip (6 secs = 30 large boxes) a. Regular or irregular? b. Measure ventricular rhythm by measuring the interval between R-to-R waves c. Measure atrial rhythm by measuring the P-to-P waves. d. If measurement is the same or varies less than 0.12 seconds, it is regular. e. For accuracy, timing should begin on the P wave or the QRS complex and exactly at 30 large blocks later = 6 second rhythm strip INFORMATION OBTAINABLE FROM ECG RHYTHM STRIP ANALYSIS Medical-Surgical Nursing | NCM 0112 Dysrhythmias also known as arrhythmias Problem: abnormal heart rhythm Priority nursing diagnosis: decreased cardiac output ® decreasing cerebral and vascular perfusion SUMMARY OF ANTIDYSRHYTHMIC MEDICATIONS Class Na Channel Blockers IA Action Moderate depression of depolarization, prolongs repolarization Drugs Treats and prevents atrial and ventricular dysrhythmias Quinidine Procainamide IB Depolarization – electrical stimulation Repolarization – electrical relaxation Minimal depression of depolarization, repolarization IC Treats ventricular dysrhythmias Marked depression of depolarization, little effect on repolarization shortens Treats atrial and ventricular dysrhythmias Indirectly blocks calcium channel II Beta blockers III K Channel Blockers IV Ca Channel Blockers Blocks the ability of the catecholamines to cause dysrhythmias Treats atrial and ventricular dysrhythmias (-) Inotropic – strength of cardiac contractility (-) Dromotropic – conduction of cardiac impulses (-) Chronotropic – heart rate (slows) Prolongs repolarization Treats and prevents atrial and ventricular dysrhythmias especially in patients with ventricular dysfunction Slows SA node cells and AV node cell conduction by direct blockage of L-type voltage gated calcium channel Treats atrial dysrhythmias Flecainide Propafenone • • Acebutolol Esmolol Metoprolol Propranolol Atrial Dysrhythmia DISTURBANCES IN CONDUCTION Blockage on the conduction pathway RE-ENTRY OF IMPULSE Occurs when cardiac tissue is depolarized multiple times by the same impulse Normal electric signal: SA ® AV ® His Purkinje system ® dies out Propagating impulse fails to die and persists to re-excite the heart after the refractory period has ended (usually ventricular dysrhythmias) 1. Sinus arrest 2. Sinus exit All characteristics are the same as those of NSR, except the rate >100/min Usually ASYMPTOMATIC Occurs when abnormal electrical signals interfere with signals coming from SA node ® can prevent heart from filling properly and reduces overall blood flow out of the heart Verapamil Diltiazem Felodipine Nicardipine CATEGORIES aka. RHYTHMICITY – ability of the cardiac pacemaker cells to initiate an electric impulse spontaneously & repetitively 1. Sinus Tachycardia 2. Sinus Bradycardia 3. Sinus Dysrhythmia 4. Premature Atrial Contractions 5. Atrial Flutter 6. Atrial Fibrillation 1. Premature Ventricular Contractions 2. Ventricular Tachycardia 3. Torsade’s de Pointes 4. Ventricular Fibrillation Amiodarone Ibutilide hyperkalemia = Class III (K Channel Blockers) hypercalcemia = Class IV (Ca Channel Blockers) Dysrhythmia 1. Supraventricular Tachycardia DISTURBANCES IN AUTOMATICITY Sinus Tachycardia • But, if it is already isolated case, such as knowledge regarding the electrolyte imbalance, give specifics Alteration in the normal heart rate produced by various pacemaker Ventricular Dysrhythmia Lidocaine For an UNKNOWN ETIOLOGY of a dysrhythmia, the safest initial management that’ll be given is a CLASS II (BETA-BLOCKERS) DISTURBANCES IN AUTOMATICITY Atrioventricular Junctional Dysrhythmia 1. First Degree AV Block 2. Second Degree AV Block 3. Third Degree AV Block 4. Bundle Branch Block 1. Ventricular Asystole Paroxysmal Atrial Tachycardia Etiology: o Increased SNS = increased heart rate / Decreased PNS stimulation = decreased VAGAL stimulation o Increased BMR = tachycardia, Stimulants = release of epi/norepinephrine ® increasing HR, Compensatory increased SNS = d/t hypovolemia, Hypercalcemia = Ca is essential in automaticity and plays a vital role in cardiac contraction ® increased cardiac contractility Management: o Bed Rest = to reduce metabolic demands o Oxygen Therapy = to supply the myocardium with oxygen adequately o Determine the cause (hypercalcemia = treat with Ca channel blocker meds) o Vagal Maneuvers Carotid sinus massage – firm pressure applies over carotid sinus ® stimulate vagal response Valsalva maneuver — usually performed by a practitioner or nurse specialist G.M.M.E. – MARILAG • • • 1. Premature Junctional Contractions 2. Paroxysmal Junctional Tachycardia Medical-Surgical Nursing | NCM 0112 o o Sinus Bradycardia • • • All characteristics are the same as those of NSR, except the rate <60/min This may be normal for some individuals = ATHLETES (have greater than normal stroke volume) CO = SV x HR = Athletes: CO = ­SV x ¯HR (compensates) o o o Premature Atrial Contraction (PAC) • • • Etiology: o Increased PNS / Decreased SNS stimulation. o Valsalva, Drugs (Digitalis, Class II, Class IV Antidysrhythmic agents), Inferior MI = problem with conduction, presence of abnormality in the lower chambers of heart, Decreased BMR, Hyperkalemia = HyperK reduces myocardial excitability, with depression of both pacemaking and conducting tissues Drugs: BB/Class II – negative dromo & chrono effect CCB/Class IV – slow HR Digitalis – lengthens PR interval Management: o Determine the cause o Oxygen = to supply myocardium with adequate O2 o Atropine = prevents vagal effects on SA and AV nodes ® enhancing conduction on AV node and increasing HR (WOF tachycardia) o Dopamine Dobutamine Isoproterenol ADRENERGIC AGONISTS/SYMPATHOMIMETIC DRUGS – mimic the effects of transmitter substances of the SNS ® increasing HR PACEMAKER – Provides electrical stimulation and maintains the heart rate when the client’s intrinsic pacemaker fails to provide a perfusion rhythm o Transcutaneous pacing – temporary noninvasive; delivered through the skin o Permanent pacemaker: pulse generator is internal and surgically implanted in a subcutaneous pocket under the clavicle or abdominal wall *when the intrinsic pacemaker fails to produce a perfusion rhythm ® will initiate the electrical signal ECG reveals a premature P wave (abnormal) that differs in morphology from the sinus P wave P wave = atrial depolarization; sinus P wave = initiated by SA node (normal) Early beats arising from ectopic atrial foci interrupting the normal rhythm = does not originate from the pacemaker (SA node) irritable cell in the atria causes EXTRA HEARTBEAT Etiology: o VHD, CAD, HF = abnormalities in the heart o Stress, Fatigue, Smoking = releases the stress hormones: epi/norepinephrine, catecholamines Management: o No treatment if the client remains ASYMPTOMATIC o May lead to ATRIAL FIBRILLATION ® WOF for signs o Avoid stimulants that could further cause of epi/norepinephrine o Digitalis/Class II/ Class IV = PACs are often seen with SINUS TACHYCARDIA Atrial flutter • • • • Arises from a single irritable focus in the atria Atrial rhythm: regular Ventricular rhythm: usually regular but may be irregular because of a change in the AV conduction ATRIAL RHYTHM: P-P interval VENTRICULAR RHYTHM: R-R interval Atrial rate (250-400) > ventricular rate (75-150) G.M.M.E. – MARILAG o ü Record an ECG strip before, during and after the procedure to observe the change in rhythm (procedure can slow the HR) ü Have a defibrillator and resuscitative equipment available (emergency) Cardiac glycosides (Digoxin, Digitoxin) (+) Inotropic – strength of cardiac contractility (-) Dromotropic – conduction of cardiac impulses (-) Chronotropic – heart rate Antidysrhythmic agents (rarely used; to decrease HR quickly) o Class II (to slow HR) o Class IV (hypercalcemia) Eliminate stimulants = etiology (epinephrine, norepinephrine) Medical-Surgical Nursing | NCM 0112 • • • The AV node cannot conduct all the atrial impulses that bombard it, therefore ventricular rate is always slower than the atrial rate P wave: saw-toothed pattern (referred to as F waves; bigger) P:QRS ratio: 2:1; 3:1; 4:1 Can also be reentry of impulses; impulses travel in circular course in atria N: SA node ® AV node ® His purkinje system What happens: SA node ® AV node ® His purkinje system ® SA node (or d/t irritable focus firing electrical impulse) Etiology: o CAD, MVD, Pericarditis Management: o Cardioversion – direct current cardioversion 25-100 J o Classes IA, II, III, IV o Ibutilide (IV) or Amiodarone (III) short-acting antidysrhythmic, 60-90% converts A. flutter to NSR Atrial Fibrillation • • • • • Atrial and ventricular rhythm: irregular Atrial rate (300-600) > ventricular rate (120-200) in untreated Afib Erratic or no identifiable P wave: small, irregular baseline undulations that vary in shape and size called smaller f waves No effective pumping of blood into the ventricles, only quivers ® blood pooling in the atria ® can lead to stroke or other heart-related complications P:QRS ratio: Many:1 Etiology: o CAD, MVD, Pericarditis – Mechanical and electrical disorganization of the atria without effective atrial contraction – Impulses have chaotic, random pathways in atria (Ectopic foci in atria) ® quivers (d/t ineffective pumping) Complications: o Angina d/t ineffective pumping of the atria ® impaired cardiac output = decreased oxygenation of the cardiac muscle tissues (chest pain) o Heart Failure d/t ineffective pumping of the atria o Shock = ¯ circulating blood volume o Embolism = blood pooling/stasis in the atria ® clot/thrombus ® embolus ® pulmonary embolism ® cerebral blood vessel (CVA) Management: o Initial tx goal is to reduce thromboembolism; and convert rhythm to sinus rhythm o Oxygen = to provide adequate O2 to myocardium o Classes I, II, IV (Class II – most effective tx in promoting adequate rate control) o Digoxin = positive inotropic, negative dromo & chrono effect o Anticoagulants o Low molecular weight heparin o Warfarin o Aspirin – antiplatelet o Cardioversion DISTURBANCES IN CONDUCTIVITY • • • Usual causes of conduction problems: Ischemia, injury or infarct Myocardial cells cannot conduct impulse properly Heart block occurs when the conduction signal passes weakly from the atria to the ventricles, or completely fails to transmit First degree AV block • • ECG reveals a regular rhythm, P wave followed by a QRS complex but with prolonged P-R interval (N: 0.12-20 secs) Atria impulses are conducted through the AV node into the ventricles at a rate slower than normal G.M.M.E. – MARILAG • Medical-Surgical Nursing | NCM 0112 Etiology: o Right atrial enlargement or atrial septal defect PR = atrial depolarization and conduction delay at AV node If there is problem in RA ® problem in conduction of impulses since SA node is located in RA Atrial septum = AV node location o Idiopathic Degenerative Diseases of the Conduction system (progressive deterioration) o Digitalis = lengthens PR interval Management: o Observe patient condition and monitor ECG changes for progression to other types of disturbances in conductivity o Discontinue digitalis therapy Second degree AV block • • • Some initial impulses fall to conduct to the ventricles Some impulses are conducted and others are blocked Resulting in intermittently dropped QRS complex *Expect that there will be missing QRS complexes in a rhythm strip A. Mobitz Type I • • • Wenckebach phenomenon PR Interval becomes longer with each succeeding QRS complex until there is a P wave not followed by a QRS (with warning) = there’s dropping of QRS complexes Abnormally long refractory period at the AV node Etiology: o Ischemia, Digitalis toxicity, Anterior wall MI Management: o Close ECG monitoring o Withhold cardiac depressants (Beta-blockers, Ca channel blockers, digitalis) o Atropine – blocks vagal effects on SA and AV nodes ® enhancing conduction on the AV node and increasing HR (WOF bradycardia) o Isoproterenol – cardiac stimulant = speeds the rate of impulse conduction o Pacemaker – can be temporary or permanent = fires electrical signals when the intrinsic pacemaker fails to transmit one Third degree AV block (AV dissociation) • • • • • • Complete Heart Block – the atria and the ventricles work independently of each other, most severe The atria are regularly paced by the SA node The ventricles are regularly paced by a ventricular ectopic pacemaker ECG shows a regular P-P interval, regular R-R interval, normal appearing P wave, absence of a consistent P-R interval *works independently (atria & ventricles) P-P interval normal and constant QRS complexes normal, rate constant but below normal, 2055/min Etiology: o Similar to first-degree AV block except that this is caused by a block in the AV node = located in the atrial septum (RA) Management: o Not required as long as the ventricular rate is adequate for perfusion o Assessed for progression to a higher degree of block • ECG shows normal P waves that are followed by normal QRS complex at regular intervals until a QRS complex is dropped (no warning) = sudden drop of QRS complexes G.M.M.E. – MARILAG B. Mobitz Type II Medical-Surgical Nursing | NCM 0112 Etiology: o Anterior wall MI, Cardiac surgery, Myocarditis, Drug toxicity (Beta-blockers, Ca-channel blockers, Digitalis), Cardiomyopathy Complications: o Heart Failure – ineffective pumping of the chambers of the heart (AV dissociation) o Asystole – may happen if an ectopic focus in the ventricles does not initiate a heartbeat/impulse BECAUSE IN 3RD DEG AV BLOCK: atria = paced by the SA node ventricles = paced by the ECTOPIC FOCUS ® No pumping ® No CO Premature Ventricular Contraction (PVC) • • • ECG reveals a premature QRS complex with a bizarre morphology with T wave polarity opposite to the normal QRS complex *most concern: fall on a T wave *initiated by an irritable focus in the ventricle An impulse that starts in a ventricle (should start from the SA node at RA) and is conducted through the ventricles before the next normal sinus impulse Time interval between normal R peaks is a multiple of R-R interval Management: o Atropine – blocks vagal effects on SA and AV nodes ® enhancing conduction on the AV node and increasing HR (WOF bradycardia) o Dopamine – improve perfusion to other organs = ­ cardiac output o Epinephrine – restores cardiac rhythm when there is asystole o Pacemaker = if natural pacemaker fails to initiate an impulse, an artificial pacemaker can be placed (temporary or permanent) to initiate an impulse o If Asystole: CPR ® Pacemaker when revived Types: 1. 2. 3. 4. • • NORMALLY: Impulse is initiated by the SA node (natural pacemaker) ® AV node ® His Purkinje system ® propagating impulse will die RE-ENTRY OF IMPULSES: propagating impulse fails to die and persists to re-excite the heart after refractory period has ended Etiology and Risk Factors: o Enhanced automaticity or reentry phenomenon o CAD, Heart Failure, Hypocalcemia, Hypokalemia, Caffeine, Nicotine, TCA, Hypermetabolic states *increased irritability of the ventricles Management: o No Treatment if isolated / asymptomatic o Determine the cause o Evaluate electrolytes – particularly K levels (K has a role in normal depolarization & repolarization) o Oxygen Therapy – adequate O2 to myocardium o Class I, Class II and Class III Antidysrhythmic Agents G.M.M.E. – MARILAG RE-ENTRY OF IMPULSES Bigeminy – PVC every other beat Trigeminy – PVC every third beat Quadrigeminy – PVC every fourth beat R on T phenomenon – if there would be an extra beat in ventricular relaxation ® a vulnerable period that may precipitate V fib = fatal dysrhythmia R = PVC T = ventricular relaxation Medical-Surgical Nursing | NCM 0112 • • • ECG shows absent P waves, absent P-R interval wide and bizarre QRS complex ventricular rate between 100 to 200 Characterized by 3 or more PVCs Life-threatening dysrhythmia Ventricular Fibrillation • • • • Etiology: o Significant Cardiac Diseases o CAD, AMI with hypoxia and acidosis, Cardiomyopathy, MVP, HF o REPETITIVE firing of an irritable ectopic focus Complications: o Cerebral and Myocardial ischemia – problem in the pumping of ventricles o Ventricular Fibrillation Management: STABLE CLIENT WITH VTachs o Oxygen therapy – adequate O2 to myocardium o Antidysrhythmic (Class I and Class III) Na channel blockers & K channel blockers o Magnesium Sulfate *Intracoronary administration of MgS04 ® suppress sinoatrial automaticity and ventricular contraction UNSTABLE CLIENT WITH VTachs o Same o Cardioversion = synchronized cardioversion o Cough CPR – instruct and coach the patient to cough forcefully every one to three seconds during the initial seconds of a sudden arrhythmia *Vigorous rhythmic coughing could produce arterial pulses and can convert V. tach to sinus rhythm PULSELESS VTachs o Defibrillation o CPR ECG shows fibrillatory wave patterns with no identifiable P waves, QRS complex T waves Characterized by extremely rapid, erratic impulse formation and conduction always that causes ineffective quivering of the ventricles Characterized by an absence of audible heartbeat, a palpable pulse and respirations Ineffective pumping of ventricles ® Primary cause of SCD (sudden cardiac death) Etiology: o Severe myocardial (vulnerable period) o Untreated VTach damage, R-on-T Phenomenon Management: o Vfib is rapidly fatal if not successfully terminated within 3-5 minutes o CPR = no palpable pulse o Defibrillation up to 3x as needed o Epinephrine, vasopressin or both – administered after the 2nd rhythm check o Antidysrhythmic medications Class I (lidocaine) Class III (amiodarone) – administered after the 3rd rhythm check o Magnesium sulfate *Intracoronary administration of MgS04 ® suppress sinoatrial automaticity and ventricular contraction G.M.M.E. – MARILAG Ventricular Tachycardia Medical-Surgical Nursing | NCM 0112 Ventricular Asystole • State of cardiac standstill V.Fib ® SCD Problem with the conduction of impulses ® asystole NR during defibrillation and cardioversion: o Stop the oxygen – to avoid hazard of fire o Be sure that no one is touching the bed or the client when delivering the shock “1 I’m clear, 2 You’re clear, 3 All clear” Position of Paddles: o 1st paddle on 3rd ICS, right of sternum o 2nd paddle on 5th ICS, left MAL (sternum) Etiology and Risk Factors: Primary o Sinus node block-arrest o Complete Heart Block NURSING MANAGEMENT: (GENERAL) Signs and Symptoms: No ventricular depolarization ® no cardiac output: o Fainting o Loss of consciousness – d/t ¯ cerebral perfusion o Seizure episode – hypoxia ® seizure (hyperexcitable neural network) o Apnea – cessation of breathing o Death – eventually occurs in all dying patients Medical Management: o CPR = no respiration o Epinephrine o Vasopressin = after 2nd rhythm check o Transcutaneous pacing = for electrical impulse to be initiated by pacer DEFIBRILLATION CARDIOVERSION Unsynchronized mode No markers Emergency Patient in cardiac arrest Patient has no pulse (pulseless VT or VFib) No need to premedicate (sedative) The electrical voltage required is usually greater than what is required in cardioversion ® may cause more myocardial damage Synchronized mode – timed Markers with R wave Patient not arrested Patient has pulse (atrial flutter, atrial fib, SVT) Premedicate as needed Elective – Anticoagulation for a few weeks before cardioversion = thromboembolism Check for digitalis toxicity because it may predispose client to ventricular dysrhythmias during cardioversion Significance of all dysrhythmias: their effect on cardiac output ® cerebral & vascular perfusion Decreased Cardiac Output Change in the LOC, Chest Discomfort, Hypotension, Shortness of breath, Respiratory Distress, Pulmonary Congestion, Crackles, Rapid, slow or weak pulse, Dizziness, Syncope, Fatigue, Restlessness o Assess VS o Monitor I&O o Restrict fluid as ordered o Elevate the head of the bed o Provide physical, emotional and mental rest o Administer prescribed medications to reduce cardiac workload Activity Intolerance r/t ineffective cardiac contraction/ imbalance between O2 supply and demand o Monitor VS before, during and after exercise o Encourage adequate rest o Encourage self-care o Increase activity levels gradually o Assist with ADL as needed o Formulate a schedule with alternating rest and activities Anxiety related to fear of the unknown Deficient knowledge about dysrhythmia and its treatment AV BLOCK FAMILY STORY P wave = wife; QRS complex = husband; Pacer = counselor § The wife (P wave) waits at home for the husband (QRS). The husband (QRS) comes home on time every night. = NSR § The wife (P wave) is waiting at home. The husband (QRS) comes home late every night, but he always comes home and it’s at the same time every night. = FIRST-DEGREE AV BLOCK § The wife (P wave) is waiting at home. The husband (QRS) comes home later and later every night until one night he doesn’t come at all. = MOBITZ 1 § The wife (P wave) is no longer waiting at home. She and her husband (QRS) are now both on separate schedules and have no relationship and they are no longer talking. Each spouse has a regular, individual schedule.e = THIRD-DEGREE AV BLOCK G.M.M.E. – MARILAG Secondary o Severe Hypoxia o Pre-existing acidosis *outside of the heart’s electrical system that result in failure to generate depolarization