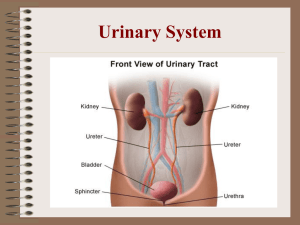
Krutikov E.S., Polskaya L.V., Tsvetkov V.A., Chernuha S.N., Fedoseeva C.M. PROPEDEUTICS TO INTERNAL MEDICINE Simferopol 2019 Chapter 6. URINARY SYSTEM FUNCTIONAL ANATOMY AND PHYSIOLOGY Adult kidneys are bean-like shape 11-14 cm in length, 150-160 g of mass, and are located retroperitoneally on either side of the aorta and inferior vena cava. The right kidney is usually a few centimeters lower. The kidneys are covered by dense fibrous capsule. Two layers are distinguished: cortical and medullar. Cortex in a form of renal column divides medulla in pyramids. Apex of each renal pyramid forms renal papilla that opens into renal calyces, which are joined in renal pelvis that continues by ureter. The functional units of the kidney are nephrons. Each kidney contains approximately 1 million nephrons. There is a rich blood supply (20-25% of cardiac output). Each nephrons is intimately associated with a glomerulus. The blood courses through the glomerulus, fluid and many dissolved materials filter out of the capillaries (120 ml/min, 170 l/day) and into the nephrons lumen. The ultrafiltrate is further modified by selective absorption and secretion as it passes through the nephrons and then finally into the collecting tubule. The urine formation thus depends essentially on glomerular and tubular filtration (Fig. 6.1). Fig. 6.1 – The nephron The ureter is a muscular tube, about 25 cm long, which joins with urinary bladder. The urinary bladder is a muscular storage bag, which empties through the urethra. The main kidney functions are: 1. Excretory. Kidneys carry out the excretion of the: a. end products of catabolism (urea, uric acid, creatinine); b. excess substances absorbed in the intestines: water, organic acids, vitamins, hormones, etc.; c. xenobiotics - foreign substances (drugs, nicotine). 2. Homeostatic. Kidneys regulate: a. water homeostasis; b. salt homeostasis; c. acid-base state. 3. Metabolic: a. the participation of the kidneys in carbohydrate, protein, fat metabolism; b. the synthesis in the kidneys of some biologically active substances: renin, the active form of vitamin D3, erythropoietin, prostaglandins, kinins. Kidney diseases may be primary, such as: Glomerulonephritis (acute or chronic) Pyelonephritis (acute or chronic) Congenital anomalies of the kidneys and urinary tract Urolithiasis Kidney amyloidosis Kidney tuberculosis Kidney tumors Secondary kidney diseases appear due to their damage in diabetes mellitus, hypertension, systemic connective tissue diseases, gout, etc. MAJOR MANIFESTATION OF KIDNEY DISEASES. The main complaints of the patient with kidney disease: Pain in the lumbar region Deranged urination - dysuria Oedema Headache Fever Pain in the lumbar region can be unilateral or bilateral. Unilateral pain can be in pyelonephritis, urolithiasis, tumor, renal infarction. Bilateral pain can be in pyelonephritis, glomerulonephritis, heart decompensation - "congestive kidney". Acute pain is characteristic of inflammatory diseases of the kidneys (pyelonephritis) associated with stretching the capsule and the pelvis. Often, acute pain associated with impaired passage of urine, characteristic of the urolithiasis, compression of the urinary tract by the tumor. Acute pain is also characteristic of renal infarction (renal artery thrombosis). Very strong attack of pain radiating along the ureter and into the genitals is called renal colic. Dull, aching pain can be in: chronic pyelonephritis, acute and chronic glomerulonephritis, nephroptosis (aching pain, disappearing in a horizontal position), paranephritis, heart failure (congestive kidney) It is necessary to clarify how the pain is provoked (by shaking up, drinking heavily, urinating), and the pain is relieved. Dysuria is disordered urination. Diuresis - secretion of the urine during a certain period of time (hour, day, night, etc.). Diuresis is called positive when the patient excretes more urine than he took fluids. It can be due to resolution of oedema after administration of diuretics. Negative diuresis is called when urine is less excreted than fluids taken. It can be due to retention of liquid in the body (oedema), excess excretion of liquid through the skin (heavy sweating), repeated vomiting, and diarrhea. Polyuria is increase in the daily amount of urine more than 2 l / day (diuresis of a healthy person is 1-2 l / day). Polyuria is observed under physiological conditions with plentiful fluid intake, while taking diuretics. Pathological polyuria is observed in diabetes mellitus, the initial stages of chronic renal failure, in the stage of recovery after acute renal failure. Oliguria is reducing the amount of urine, less than 500 ml / day. Oliguria can happen of renal origin (acute nephritis, acute necrosis of the kidneys in case of poisoning by poisons, final stages of chronic renal failure) and of extrarenal origin (when limited intake liquid, in a dry and hot environment, severe vomiting, diarrhea, severe heart failure). Anuria is absence of urine excretion or when the urine excretion is less than 50 ml / day. Renal anuria (secretory) can be associated with acute renal failure (acute glomerulonephritis, acute toxic damage to the kidneys (renal necrosis in case of poisoning with sublimate lead, etc.) or final stages of chronic renal failure. Excretory anuria may be due to obstruction of the ureters by a calculus or proliferation of a malignant tumor. Extrarenal anuria may be result of shock, massive blood loss, and severe heart failure. Ishuria is a condition where the patient cannot empty the urinary bladder. It happens when the urethra is obstructed (adenoma, calculus, tumor) or if the spinal cord is damaged. Pollakiuria is a frequent urination, more than 10 times a day. Causes: cystitis, prostatic hyperplasia, uterus enlargement during pregnancy, in the initial stage of chronic renal failure. Ollakiuria is rare micturition that not always associated with oliguria. The commonest causes of ollakiuria are limited fluid intake, eating of much salted food, excessive sweating in hot climate or fever, and neuroreflex disorders. Stranguria is difficult, painful urination. It can be in cystitis. Nocturia is a condition in which the night diuresis persistently prevails over the day diuresis. It is observed of the patients in the initial stages of chronic renal failure (against the background of polyuria), with heart failure (against the background of Oliguria). Oedema usually appears on the face at locations of soft tissue, and then on the lower limbs, in the abdominal and pleural cavities. Renal oedema increases in the morning after sleep and decreases in the evening. More intensive oedema develops of the patients with nephrotic syndrome (glomerulonephritis, amyloidosis), with acute renal failure and final stage of the chronic renal failure (СRF). With increasing blood pressure, the patient complains of: headache; vertigo; tinnitus; reduced vision; palpitation; pain in the heart. Complaints of weakness, fatigue, malaise, poor sleep, decreased work capacity, skin itching, unpleasant breath, loss of appetite, nausea, impaired stool, etc., occur in intoxication due to the accumulation in the body of metabolic products in renal failure. Fever can indicate infectious inflammatory kidneys affection (pyelonephritis, paranephritis, renal abscess). When collecting the anamnesis vitae, you should find out the presence of: Previous infectious processes (tonsillitis, scarlet fever, influenza, hepatitis). Habitual intoxications (alcohol, narcotic), taking medicines (NSAIDs, barbiturates, etc.) Industrial intoxication, casual intake of poisons (mercury, lead, bismuth). Strong hypothermia, stress. Presence of tuberculosis infection. The presence of chronic purulent infections foci: osteomyelitis, bronchiectasis, which can cause kidney amyloidosis. Kidney disease in close relatives. Pregnancy anamnesis in women (toxicosis during pregnancy can cause nephropathy of pregnant women, followed by the development of CRF). INSPECTION On inspection, the patient is assessed for general condition, consciousness, position of the patient, facial expression, and skin condition. Be sure to inspect the lumbar region. The general condition and consciousness of the patient change with the progression of renal failure. The position of the patient may be passive with renal coma. Forced posture occurs with paranephritis - inflammation of the pararenal tissue (the patient lies on the affected side with flexed leg) and with renal colic (the patient is restless and tossing in bed). The patient's face has a typical expression (facies nephritica) in glomerulonephritis, renal amyloidosis, nephrotic syndrome. It is pale, puffy with swollen eyelids, with narrowed eye slits. Pale skin, often detected in kidney diseases, is caused by anemia and spasm of skin arterioles. With the progression of renal insufficiency, the skin becomes dry, covered with urea crystals, traces of scratches are visible as a result of severe itching. You can see the cramps and feel smell the ammonia from the mouth and skin of the patient (factor uremicus). Protrusion and hyperemia in the lumbar region can be detected in paranephritis. In considerable kidney tumor protrusion of the abdominal wall or loin on the corresponding side can be detected. PALPATION The palpation of kidneys can be carried out in the various position of the patient: supine, standing, sitting, on the side etc. In most cases, the kidneys are palpated in supine position. The patient lies on the back with the extended legs; the arms are placed on the chest, the abdominal muscles are weakened. The right kidney is first palpated. A palm of a palpating right hand is put longitudinally on the right part of abdomen outside from the edge of rectus muscle so that close and slightly bent fingertips was slightly below of the costal arch. The palm of the left hand with close and straightened fingers is placed horizontally under the right loin between ribs and wing of the ileac bone (Fig. 6.1). Fig. 6.1 – Palpation of the kidney The right hand is smoothly dipped in the abdominal cavity during expiration. Simultaneously with right hand, the left hand makes pressure on the loin, trying to approach a back abdominal wall in a direction of a palpating right hand. In a considerable nephroptosis a lower pole or all kidneys is palpated. In other cases the patient is asked to make the deep inspiration by abdomen. The kidney, being displaced downwards, reaches fingers of the right hand and passes under them. For palpation of a left kidney the right palm is put on left flank of the abdomen, and the left hand is carried out further of the backbone and placed under the left part of loin. The palpation is carried out similarly above described. The kidneys can be palpated in standing position. The patient slightly inclines the trunk forwards. The doctor sits on the chair before the patient. The technique is similar above described. According to gravity low in vertical position the kidney are displaced downwards, that allows to reveal better their lowering, however palpation is complicated because of poor weakening of abdominal muscles. In norm the kidney, as a rule, are not palpated, except for cases of sharp emaciation and flabby abdominal wall that more often happens for the women. A lower pole of a right kidney, which in norm is located lower then left one, can be palpated in asthenic patients. The kidneys become palpated in nephroptosis, pathological mobility and in increase of organ in 1,5-2 times. If the kidneys are palpated their form, sizes, consistence, character of the surface, mobility and presence of morbidity must be determined. Lowered kidney is spherical bean-like form, with a smooth surface, elastic consistence, painless, its length is about 12 cm; transverse size is about 6 cm. The increase sizes one of kidneys more often can be in hydronephrosis and tumor process. In cancer the surface of the kidney is tuberous, consistence is increased density, and the mobility is limited. In patents with hydronephrosis kidneys are soft consistence with smooth surface. The synchronous increase of both kidneys more often can be in polycystic kidney disease. In this case kidneys are soft-elastic consistence with rough surface. Nephroptosis can be uni- and bilateral. Three degrees of nephroptosis are distinguished. In first degree 1/3-1/2 lower part of kidney can be palpated on the height of inspiration, during expiration it slips upwards and can not be kept by hand. In second degree full kidney is palpated, it can be kept by hand and its physical properties can be determined. In third degree of nephroptosis the kidney freely moves in different directions and even for a backbone to the opposite side (" wandering" kidney). The palpated kidney must be differentiated from adjacent organs: liver, gallbladder, spleen, and colon. First of all, the kidney is characteristic the bean likes form and dense consistence. The characteristic painful points can be determined in the projection of kidneys and ureter. The deep palpation is carried out by index or middle finger in symmetric points. Kidneys points are divided on front and back. Front point is situated immediately under costal arch near the anterior edge of the X rib. Back point is situated in the point of crossing of the lower edge of the XII rib and external edge m. latissimus dorsi. The front points are palpated in supine position of the patient, back points are palpated in sitting position. Ureter points are divided on upper and lower. Upper point is situated on external edge of rectus muscle on the level of navel. Lower point is situated in the point of crossing of the iliac line with external edge of rectus muscle. The morbidity of points on palpation indicates pathological process, more often inflammatory origin. PERCUSSION Tapping method (modified Pasternatsky symptom) is used in clinical practice. The doctor stands behind the patient put his left palm upright on the loin in the area of the XII rib and make short, abrupt strokes with increasing force by the edge of right palm (Fig. 6.2). Fig. 6.2 – Modified Pasternatsky symptom In norm this symptom is negative. If patient feels pain in the loin depending of its intensity symptom is weakly or distinctly positive. It is typical for the patients with urolithiasis, pyelonephritis, and paranephritis. However it is not specific. The appearance of sensitivity or pain in the kidneys area after tapping with subsequent short-term appearance or increase erythrocytes in urine is called positive Pasternatsky symptom. EXAMINATION OF THE URINARY BLADDER Palpation The empty urinary bladder is not palpated. The full urinary bladder is palpated in suprapubic area as an oval diverticulum with a smooth intense — elastic surface, moderately painful. After evacuation of the urine the diverticulum disappears. Reasons of ischuria (delay of urine) can be due to paresis of the urinary bladder muscles; obstruction of the urethra by a stone, tumor, enlarged prostate; in compression by the adjacent enlarged organs and tissues. In malignant affection of the urinary bladder the dense tumor is sometimes palpated (Fig. 6.3А). Percussion Percussion is used for definition position of the upper border of the urinary bladder. The percussion is carried out along l. mediana from the navel downwards. The finger-plessimeter is placed horizontally. The overfilled urinary bladder gives dull sound (Fig. 6.3В). Fig. 6.3 – Examination of the urinary bladder INVESTIGATION OF KIDNEY DISEASE Laboratory methods examination URINALYSIS (UA; routine UA) is an important routine screening test that gives information about the status of the renal and urinary tracts and the total body system. The test involves collection of a random sample of at least 100-200 ml of urine. A first-voided morning specimen is preferred. Female patients should be instructed to clean external genitals before voiding, because the specimen should be free of vaginal discharge and feces. The specimen is sent to the laboratory or refrigerated if it must be kept longer than 1 hour. If left standing at room temperature for 5 hours, the specimen will not be suitable for culture; erythrocytes will decompose and casts will disintegrate. Nurses can obtain immediate information on ketones, pH, protein, glucose, and blood by using a Multistix reagent strip. The three principal constituents of urine are water, urea, and electrolytes, namely, sodium and chloride. In addition to many other substances found in the urine are all indications of possible disease. Routine urinalysis includes physical, chemical and microscopic examinations. Physical examination includes the following information: Volume. The amount of urine, both total daily volume and volume of each voiding, depends on a number of factors: fluid intake, fluid losses from other routes, fever, environmental temperature, age, ingestion of a high-protein diet (which produces more urine), or diuretic drugs. This index is not significant because urinalysis is examination only one voiding. The amount per voiding normally depends on the person's bladder capacity. Color. The color of normal urine depends on its concentration and varies from straw-yellow to the color of amber. The color of urine darkens on standing because of the oxidation of urobilinogen to urobilin. It begins in 30 minutes. When there is bleeding in the upper urinary tract, the urine may be dark red or smoky. Bleeding in the lower urinary tract produces red urine. Visible change of color due to presence of large quantity of erythrocytes is called macrohematuria. Dark yellow urine may indicate the presence of urobilin or bilirubin, which can be in some liver diseases. Milky white urine may be caused by pus or by fat globules released in the kidney as a result of nephrosis or severe trauma. Foods that may turn the urine red are rhubarb, beets, blackberries, and red food dyes. Bright yellow urine comes from ingesting large amounts of carotene (carrots or sweet potatoes). Many medications cause color changes in the urine. Transparency. Urine is usually transparent when freshly voided. It turns cloudy on standing. Cloudiness in freshly voided urine indicates the presence of bacteria, inflammation within the urinary tract, sperm or prostatic fluid. Odor. Normal, freshly voided urine is aromatic. Concentrated urine usually smells stronger than dilute urine. When urine stands, it may develop an ammonia smell due to bacterial action. Certain foods, such as asparagus, cause characteristic odor changes. Inflammatory reactions also alter the normal odor to ammonia smell (cystitis, pyelonephritis). Heavily infected urine has a particularly unpleasant fetid odor. A sweet (fruit) odor may indicate the presence of ketone bodies or acetone. It is found with diabetes mellitus, starvation, or dehydration. Other changes occur with medications, such as paraldehyde, vitamins, and antibiotics. Specific Gravity. The specific gravity of the urine varies from 1.001 to 1.040. Urinometer is used for measuring specific gravity. It gives information on the concentration of substances dissolved in it (urea, uric acid, salts) and characterizes the concentrating and diluting capacity of the kidneys. Specific gravity depends not only on the amount of particles dissolved but mainly on their molecular weight. Specific gravity of the morning portion is not important for diagnostics because it depends on many factors. If kidney function is normal, specific gravity indicates fluid status. High specific gravity in the absence of kidney failure usually indicates dehydration (after taken meat food, excessive perspiration), whereas low specific gravity under normal circumstances reflects overhydration (after vegetable meal, increased fluid intake, salt-restricted diet). In average the specific gravity morning portion is varied from 1015-1025. Specific gravity is altered by severe kidney disease and by intravenous contrast media used during x-ray procedures. Specific gravity is increased by radiopaque contrast media, albumin, dextran, and in dehydration, chronic heart failure, and liver failure. Unusually high values for specific gravity, for example, above 1.030, suggests the presence of large amount of solid constituents in the urine, such as glucose in a diabetic patient. Low specific gravity indicates dilute urine and may occur with diabetes insipidus, acute tubular necrosis, released edema and alimentary dystrophia. Chemical Analysis of Urine: Reaction of the Urine. The kidneys are important for maintaining acid-base equilibrium in the body. The kidneys are capable of removing the ions of hydrogen and hydrocarbonate from the blood and this is a mechanism by which pH of blood is maintained constant. Measure urine pH by using a dipstick, which is a multiple reagent strip treated with chemicals. Dip the dipstick into a fresh urine specimen and compare the color change with a standardized color on the bottle after waiting the specified amount of time. The mean pH value of the urine in healthy subjects with normal nutrition is abount 5,0-7,0. The value of pH depends from the character of nutrition and can be changed by the action of some medicinal preparations. A diet high in meats, eggs, cheese, whole grains, plums, prunes, and cranberries (including prune juice and cranberry juice) may decrease the pH, producing acid urine. A diet high in vegetables, citrus fruits, and milk may increase the pH, producing alkaline urine. Also the urine pH may be intentionally altered to inhibit bacterial growth or urinary stone development or to facilitate the therapeutic activity of certain medications. For example, acid urine should be maintained in the treatment of urinary tract infections and persistent bacteriuria and in the management of some urinary calculi. Conversely, alkaline urine should be maintained when streptomycin, neomycin, and kanamycin are used in the treatment of urinary tract infections. Acidity of urine can increase in diabetes mellitus, renal insufficiency, tuberculosis of the kidneys, metabolic or respiratory acidosis, pyrexia, starvation. Alkaline pH occurs with diarrhea and vomiting, chronic urinary tracts infections due to bacterial-ammoniacal fermentation, metabolic or respiratory alkalosis. Protein. Testing the urine for protein is based on its coagulation in the presence of acid. Normal urine does not practically contain protein. The small quantity of plasma proteins that is present in the urine, cannot be determined by qualitative tests used in practical medicine. The appearance of protein in the urine is called proteinuria. It can be of renal and extra renal origin. Functional renal proteinuria is connected with the permeability of membranes in the renal filter in the presence of strong stimulation, slowing of the blood flow in the glomeruli, in intoxications. The urine will contain albumin after a cold bath, excessive exercise (effort), a high-protein diet or a lordotic posture in children (orthostatic), emotional stress. In cases with extrarenal proteinuria proteins enter in the urine from the urinary and sex ducts. Extrarenal proteinuria is not exceed 1 g/L usually. Organic renal proteinuria occurs in kidney affections due to increased permeability of glomeruli which are underlined by vascular inflammation or structural disorganization of the basal membrane. Glomerular permeability is upset by the "molecular sieve" mechanism, low-molecular proteins are lost in the first instance (albuminuria), as the process progresses, high-molecular proteins are also lost. Renal proteinuria occurs with glomerulonephritis, preeclampsia in pregnant woman, or multiple myeloma, amyloidosis, and renal abscesses. Congestive proteinuria may be indicative of decompensated heart failure, abdomen cavity tumors. Toxic proteinuria may be after overdosage some medications (aspirin, analgetic). Neurogenic proteinuria occurs with cranium trauma, and hemorrhage of the brain, myocardial infarction, renal colic. Proteinuria can be moderate, when protein loss is not exceed 1 g/twenty-four hours, average, when protein loss is from 1 to 3 g/twenty-four hours, and considerable, when protein loss more than 3 g/twenty-four hours. Glucose. Testing the urine for glucose can be done by using reagent strips. The urine of a healthy person contains very small quantity of glucose, which cannot be detected by common qualitative tests. Glucose in the urine (glycosuria) can be both physiological and pathological. In the presence of normal renal function, glycosuria occurs when concentration of sugar in the blood 8 -10 mmol/L. Physiological glycosuria can be observed in persons whose diet is rich in carbohydrates (alimentary glycosuria), following emotional stress, and administration of some medicines (caffeine, corticosteroids). Less frequent is renal glycosuria associated with disturbed resorption of glucose in the tubules in normal amount of sugar in the blood (in renal diabetes, chronic nephritis, nephrotic syndrome). Pathological glycosuria occurs most frequently in diabetes mellitus, less frequently in thyrotoxicosis, in Itsenko-Cushing syndrome, in liver cirrhosis. Ketone. The presence of ketone bodies in the urine is called ketonuria. The urine of a healthy person contains very small quantity of ketone bodies, which cannot be detected by common qualitative tests. Ketonuria can be detected due to abnormal fat metabolism. Ketone may be indicative of poorly controlled diabetes, dehydration, starvation, long-standing gastro-intestinal disorders, postoperatively, or excessive ingestion of aspirin. Bilirubin. Normal urine is practically free from bilirubin. Bilirubinuria occurs in hepatic and subhepatic jaundice at which the concentration of bound bilirubin in the blood increases (more than 34 mkmol/L). Urobilin. Urobilinoids are urobilin and stercobilin. Excretion of large amount of urobilinoids in the urine is called urobilinuria which occurs in diseases of the liver, hemolytic anemia and enteritis. Microscopic examination of urine sediment is made for qualitative and quantitative appraisal of the main urine elements. Epithelium Cells. Cells of squamous, transitional and renal epithelium can be revealed. Squamous epithelium enters the urine from the external genitalia and the urethra, their diagnostic importance is low. Large amount of squamous epithelium in female can be indicative of bad clearing of the external genitalia or some gynecological diseases. Large amount of squalors epithelium in male occurs with inflammation of the urethra. Cells of transitional epithelium line the mucosa of the urinary tract. The presence of large amount of transitional epithelium in the urine indicates inflammatory process in the pelves or the bladder. The presence of renal epithelium in the urine is a specific sign of acute and chronic affections of the kidneys, and also of fever, toxicosis, and infectious diseases. Leucocytes in the urine of a healthy person are usually neutrophils and their amount is insignificant and less than 6-8 in the microscope's vision field. Increased quantity of leucocytes in the urine (leukocyturia) indicates inflammation in the kidneys or urinary tract (urethritis, prostatitis, cystitis, and pyelonephritis). Erythrocytes can be altered and unaltered. The urine of a healthy person is free from erythrocytes or can have single erythrocytes in preparation. The presence of erythrocytes in the urine is called hematuria. Hematuria that can be established only by microscopy is called microhematuria, while hematuria revealed by macroscopy is called macrohematuria. Physiological microhematuria can be found in physical overstrain of the sportsman. Erythrocytes may be liberated either from the kidneys (glomerulonephritis, tumor of the kidney) or from the urinary tract (stones in the pelves, urinary bladder or; tuberculosis or malignant new growths of the urinary bladder or ureters). In the presence of glomerular hematuria the urine usually contains much protein. Protein-erythrocytic dissociation (hematuria with insignificant proteinuria) usually suggests hematuria associated with pathology of the urinary tract. Non-glomerular hematuria can have intermittent character. Casts (cylinders) are proteinous or cells formation of tubular origin, they have cylindrical configuration and variable size. In normal urine the casts are absent. Hyaline casts are found in acute and chronic glomerulonephritis, nephrotic syndrome and also in physiological transient albuminuria. They can be found in the urine of practically healthy people when the pH of the urine decreases sharply along with increasing specific gravity of the urine, which is characteristic of dehydration. Presence of granular casts indicates dystrophic processes in the tubules. Waxy casts are characteristic of chronic diseases of the kidneys. "Non-organized sediment" of the urine consists of salts that precipitate as crystals and amorphous substances. Their character depends on the colloidal composition of the urine, its pH and other properties. Acid urine contains uric acid, urates, and oxalates. Alkaline urine contains ammonium urate, calcium carbonate, phosphates. The sediment is diagnostically insignificant. Phosphate and calcium oxalate crystals occur with hyperparathyroidism or malabsorption. Urate crystals occur with serum acid levels (gout). Bacteriological Examination of Urine. The urine culture remains a standard procedure for diagnosing urinary tract infections. A test of the antimicrobial sensitivity of identified organisms is usually ordered. Newer methods help identify positive specimens more accurately and rapidly. The patient is told that the detection of the urinary tract infection and that proper collection is necessary for useful results. The nurse ensures that patient has a sterile container, is aware that only the outside of the container is to be touched, and that the container should be held in such a way that it does not contact legs, genitalia, or clothing. The patient is instructed in proper cleansing techniques. Specimens for urine culture may also be collected through catheterization or directly from an indwelling catheter. The first voided morning specimen is preferred because bacterial counts are highest at this time. A colony count of less than 50,000 bacterial units/ml of urine is not significant, and a count of 50,000 to 100,000 is inconclusive. A count of 100,000 is considered a positive culture and is indicative of pyelonephritis if accompanied by fever and flank pain. A positive culture that is accompanied by dysuria, frequency and urgency is indicative of cystitis. A positive culture that is not accompanied by symptoms may indicate contamination of the specimen during collection or chronic low-grade pyelonephritis. The presence of more than two organisms or of vaginal or skin organisms is suggestive of contamination. Urinary syndrome in glomerulonephritis is characterized by the presence in the urine of protein, red blood cells, and cylinders (casts). Urinary syndrome in pyelonephritis is characterized by the presence of leukocytes, bacteria, and minor proteinuria in the urine. Urinary syndrome in renal colic is characterized by the presence in the urine of fresh erythrocytes (macrohematuria) and large amount of salts, there may be leukocyturia and slight proteinuria. URINE TEST FOR ALBUMINURIA is prescribed for patients with high blood pressure, diabetes mellitus, and kidney diseases to clarify the presence of proteinuria as a more accurate and highly sensitive diagnostic method. NECHIPORENKO'S METHOD is used to count erythrocytes, leucocytes and casts in 1 ml of urine for differential diagnosis between pyelonephritis and glomerulonephritis. The main advantage of this method is that an average sample of urine is taken for analysis and the presence of pus from the sex organs is excluded thus. In norm: erythrocytes count is to 1 x 106/L ; leucocytes count is to 4 x 106/L; hyaline casts count is to 0,25 x 106/L . The amount of leucocytes increases in pyelonephritis; the amount of erythrocytes and casts increases in glomerulonephritis. ZIMNITSKY'S TESTS assess the concentration and excreted functions of the kidney by specific gravity and amount of the excreted urine. The main advantage of this method is that the renal function is tested without interfering with the normal life of the patient. The patient collects his urine at 3-hour intervals (8 portions during 24 hours). He begins to collect the urine from 9 o'clock in the morning and finishes at 6 o'clock in the morning the next day. Excreted Function. The volume of each portion of the urine determined. It is necessary to compare daily diuresis with amount of taken liquid. The normal daily amount of urine (daily diuresis) excreted by an adult varies from 1000 to 2000 ml. A normal individual should eliminate about 7580% of the taken liquid during a day. The daily amount of urine below 75% of taken liquid is observed in patient with edema (negative diuresis). The amount of urine, both total daily volume and volume of each voiding, depends on a number of factors: fluid intake, fluid losses from other routes, fever, environmental temperature, age (a child excretes proportionately more than an adult), ingestion of a high-protein diet (which produces more urine), or diuretic drugs. The daily amount of urine over 2000 ml (polyuria) is observed in person who takes much liquid (physiologically or in diabetes mellitus), during resolution of edema after taken diuretics, in early stage of chronic pyelonephritis, renal failure. The daily amount of urine below 500 ml (oliguria) may be of patient with kidney diseases (renal insufficiency) and extrarenal diseases (vomitus, diarrhea, limited intake of liquid, after hemorrhage, heart failure, pyrexia). The volumes of daily and night urine are compared and a conclusion is derived concerning daily (the first 4 portions) and nocturnal (the next 4 portions) diuresis. Normally the daily diuresis exceeds the nocturnal one in 2-3 times. Nocturnal diuresis (nocturia) prevails in renal insufficiency. Oliguria accompanied with nocturia is typical for heart failure. Volumes of urine portions can be varied from 50 to 250 ml, but it not be able lesser than 100 ml between small and big portions. Equal amount urine in all portions is called isuria and indicates renal failure. Concentrative Function. Fluctuations in specific gravity of the urine during the course of the day and its maximum value are determined thus. Normally specific gravity of urine is from 1.005 to 1.028 and the difference between small and maximum value can't be lesser then 10. If renal insufficiency is pronounced, decreased specific gravity becomes permanent (hyposthenuria). If the renal function is upset significantly, the specific gravity of the urine in all portion is 1.009-1.011, which corresponds to the specific gravity of the primary urine or blood plasma (isosthenuria). In diabetes mellitus the specific gravity is more than 1.028 (hypersthenuria). The main criterion for assessing renal function is the glomerular filtration rate, which is calculated by the clearance method (Reberg test) and the calculation method (according to the formula), the results of which can be slightly different for the same patient. REHBERG'S TEST is used to determine the functional renal condition depending of the glomerular filtration rate (GFR) and the percentage of reabsorbed water. Renal insufficiency arises in cases where the mass of the active parenchyma is 20% and lower of normal weight. If a substance that is filtered in the glomeruli but is not reabsorbed or liberated in the tubules is used for the assessment of renal function, the clearance of this substance is actually equal to glomerular filtration. Using this phenomenon, Reberg proposed a test for studying the amount of filtration by endogenic or exogenic creatinine. If one assumes that creatinine content of plasma and glomerular filtrate is the same, it is possible to determine the degree of concentration of the glomerular filtrate as it passes the tubules. Blood is taken from the vein of the patient on a fasting stomach and creatinine concentration is determined. Urine is collected during 2 hours. Diuresis is measured thoroughly and creatinine content is determined. Next, using the formula of the amount of glomerular filtration and reabsorbtion percentage are calculated. In healthy individuals the GFR is 65-125 ml/min. The percentage of reabsorbed water is 98-99%. As renal failure develops, glomerular filtration decreases gradually to attain as 5 ml/min. Tubular reabsorbtion changes less markedly to decrease in cases of pronounced insufficiency to 80-60%. The prognostic value of the method increases if it is used in follow-up studies. Persistent decrease in glomerular filtration to 40-50 ml/min during 18-24 months following acute glomerulonephritis suggests the conversion of the acute process into the chronic disease. GFR is often calculated by the formula CKD=EPI based on the result of blood creatinine. To determine the functional renal condition it is possible to examine concentration of urea, and creatinine in blood. In norm: concentration of urea is 3,33-8,32 mmol/L creatinine - 53-106,1 mkmol/L. In renal failure their amounts increase. Instrumental methods ULTRASOUND is quick and noninvasive technique for renal imaging. It can show renal position and size, dilatation of the collecting system, distinguish tumours and cysts, and show other abdominal, pelvic and retroperitoneal pathology. In addition, it can image the prostate and bladder. Ultrasonographic density of the renal cortex is increased and corticomedullary differentiation lost in chronic renal disease. Doppler techniques are used to show blood flow and its characteristics in extrarenal and larger intrarenal vessels. INTRAVENOUS UROGRAPHY has been largely replaced by ultrasound for routine renal imaging; this technique provides excellent definition of the collecting system and ureters, and remains superior to ultrasound for examining renal papillae, stones and urothelial malignancy. The disadvantages of this technique are the need for an injection, time requirement, dependence on adequate renal function, and risk of allergic reaction. RENAL ARTERIOGRAPHY AND VENOGRAPHY is used to investigate suspected renal artery stenosis or haemorrhage. COMPUTED TOMOGRAPHY (CT) is particularly useful for characterizing mass lesions within the kidney, or combinations of cysts with other pathology. It gives clearer definition of the retroperitoneal anatomy and, unlike ultrasound, is added by increased amounts of fat. MAGNETIC RESONANCE IMAGING (MRI) offers excellent resolution and distinction between different tissues. Magnetic resonance angiography can produce good images of main renal vessels. These techniques are likely to develop further and find and important role in non invasive screening for renal artery stenosis. RADIONUCLIDE STUDIES require the injection of gamma ray-emitting radiopharmaceuticals which are taken up and excreted by the kidney, a process which can be monitored by an external gamma camera. In this way, the function of individual kidneys can be assessed. RENAL BIOPSY is used to establish the nature and extend of renal disease in order to judge the prognosis and need for treatment. It has definite indications, contraindications and complications. The procedure is performed with ultrasound guidance to ensure accurate needle placement into a renal pole. RENAL SYNDROMES Urinary syndrome Urinary Syndrome is characterized only by changes in the general analysis of urine. This is the most common syndrome that occurs with kidney and urinary tract damage. It may be the only manifestation of kidney disease. First of all, you need to pay attention to proteinuria, hematuria and an increase in the number of white blood cells. Proteinuria, often asymptomatic, requires careful examination of the patient. It is most often associated with increased filtration of plasma proteins through the basement membrane of the renal glomeruli (glomerular proteinuria). Proteinuria can be associated with the inability of the proximal convoluted tubules to reabsorb plasma low-molecular-weight proteins that have been filtered by normal (unchanged) glomeruli (tubular proteinuria). Persistent proteinuria is observed in most primary kidney diseases, in some systemic diseases, renal amyloidosis, diabetic nephropathy, and "congestive kidney." Transient (episodic) proteinuria is subdivided into orthostatic, febrile, and effort proteinuria. Hematuria is the presence of red blood cells in the urine more than 2-3 cells in men and 6-8 cells in women. It has been suggested that erythrocytes in the urine appear due to damage to the interstitial tissue of the kidney, or due to necrotic inflammation of the renal arterioles. Renal colic Renal Colic is one of the most severe and painful types of pain, which occurs as a result of a violation of the passage of urine through the urinary tract. The most common causes of renal colic are: obstruction of the ureter with a stone (nephrolithiasis) or a clot of pus, mucus (pyelonephritis); occlusion of the ureter with necrotic tissue in tuberculosis and kidney cancer; occlusion of the ureter with tissue, blood clots in case of kidney injury; occlusion of the ureter by the tumor with prostate adenoma. Clinical signs. The pain occurs acutely, suddenly, has a constant and cramping character, it is localized in the lumbar region or hypochondrium. Pain irradiate along the ureter to the ileac and inguinal region, to the genitals (Fig. 6.4). In men, pain radiates to the head of the penis and may be accompanied by frequent and painful urination. Renal colic may be accompanied by nausea and vomiting, not bringing relief, as well as flatulence, the development of intestinal paresis. The patient has fever, tachycardia and an increase of blood pressure. Fig. 6.4 – Localization and irradiation of pain (renal colic) The intensity of the pain, especially in the first hours, forces the patient to change the position of the body, any of which, as a rule, does not bring him relief. The patient tosses in the bed, sometimes tilts his trunk, keeping his palm on the lower back from the side of pain. As the stone moves, the intensity of the pain may decrease. With the localization of the stone in the pre-bladder ureter, there may be false urge to defecate and frequent urination. Physical examination of the patient noted severe pain on palpation of the kidney and along the ureter on the affected side. In the blood test revealed a moderate increase in the number of leukocytes to 10-12x109 /L with a shift to the left leukocyte formula, accelerated ESR. In the urine - "fresh" red blood cells. Hematuria is the most common symptom of renal colic. NB urinalysis may be normal in the absence of urine from the blocked kidney and its receipt from the unaffected opposite kidney. Nephrotic syndrome Nephrotic Syndrome is symptom complex developing in: glomerulonephritis; diabetes mellitus; kidney amyloidosis; multiple myeloma; kidney tumors; pregnant nephropathy. The main clinical manifestations are: pronounced edema; proteinuria more than 3,0 - 3,5 g/day; hypoalbuminemia; hyperlipidemia. Massive proteinuria causes hypooncotic edema with sodium and water retention, hyperaldosteronism, increased renin and catecholamine activity, as well as hyperlipidemia, impaired homeostasis (hypercoagulation, loss of microelements, etc.). With the development of nephrotic syndrome, patients complain of edema, oliguria, general weakness. Edemas, primarily on the face, can later spread to the lower extremities, and ascites, hydropericardium, and hydrothorax often develop. Severe dyspnea occurs in patients with hydrothorax and hydropericardium. In the blood - hypoproteinemia and hyperlipidemia. Hypoproteinemia (hypoalbuminemia less than 30 g / l) is a direct consequence of proteinuria. The albumin level is lower, the more its excretion in the urine. Triglycerides and cholesterol are increased (the liver increases the production of lipoproteins in response to a decrease in plasma oncotic pressure). In the urine: the relative density of urine is increased to 1030 - 1040, proteinuria more than 3.5 g/day., hyaline, granular, waxy casts. Glomerular filtration may be normal or even increased. Renal hypertension syndrome Renal Hypertension Syndrome often develops with glomerulonephritis, congenital kidneys anomalies, kidney tumors, polycystic kidney disease, pyelonephritis, nephropathy of pregnant women. Arterial hypertension in kidney disease is caused by the following main mechanisms: Delayed sodium and water. Activation of the renin-angiotensin-aldosterone system. Activation of the sympatho-adrenal system. Reduced production of vessel-dilating hormones (prostaglandin and kallikrein-kinin systems). and substances Complaints of: headache, dizziness, weakness, fatigue, nausea, decreased visual acuity, flickering of spots, circles and "flies" before the eyes, tinnitus, pain in the heart, heart failure, shortness of breath. Hypertensive syndrome is characterized by a significant increase in diastolic pressure, severe retinopathy (with foci of hemorrhage, edema of the optic disc, sharp decrease in vision up to complete blindness), hypertensive encephapathy and heart failure. Changes in the cardiovascular system are characteristic of hypertensive syndrome: displacement of the left heart border; diffused, high, resistant apex beat; hard pulse; accent II sound on the aorta Renal eclampsia syndrome. Eclampsis (lat) - flash, convulsions. In pathogenesis, the main importance is given to the increase of intracranial pressure, cerebral angiospasm due to increased blood pressure, and brain edema. It often occurs in nephrotic syndrome and uncontrolled (malignant) hypertension in severe glomerulonephritis, nephropathy of pregnant women. Clinical manifestations: The first signs of eclampsia are flaccidity, drowsiness, apathy, headaches, dizziness, nausea, vomiting. Then there are disorders of the central nervous system such as, aphasia (short-term speech loss), amaurosis (short-term loss of vision due to retinal and optic nerve damage), paresis of the limbs. In severe cases, the patient loses consciousness, clonic convulsions occur. Provocative factors are a disturbance of the water-salt regime, which causes the progression of edema and a sharp increase of the blood pressure. Death can occur as a result of the brain edema. Renal failure Renal Failure is used primarily to denote failure of the excretory function of the kidneys, leading to retention of nitrogenous waste products of metabolism. Various other aspects of renal function may fail at the same time, including the regulation of fluid and electrolyte status and the endocrine kidney function. The most fundamental categorization is renal failure is into acute or chronic renal failure. ACUTE RENAL FAILURE (ARF) or acute kidney damage is a sudden development of renal dysfunction with delayed elimination of nitrogenous metabolism products and disorder of water, electrolyte and acid-base balance, i.e. rapidly occurring disorders primarily renal excretory function. There are three variants for the ARF: prerenal occurs in disturbance of blood flow to the kidneys, renal is characterized by impaired renal function at the level of parenchyma, postrenal occurs in urinary obstruction (Tab.22). Table 22 Etiology ARF. Variant ARF Prerenal Renal Reasons Shock kidney: trauma, loss of a large amount of fluid, massive tissue breakdown, hemolysis, bacteremic shock, cardiogenic shock. Toxic kidney (action of nephrotoxic substances: salts of heavy metals, carbon tetrachloride, methyl alcohol, poisonous mushrooms, drugs, alcohol), acute infectious-toxic kidney (direct or indirect effect of infectious factors), vascular obstruction (systemic vasculitis, malignant arterial Postrenal hypertension, necrotizing papillitis). Acute urinary tract obstruction: urolithiasis, tubular blockade with urates. Clinical manifestation. During acute renal failure, it is common to distinguish four stages: initial, oligo-anuric (azotemic), diuresis recovery (polyuric), complete recovery of renal function (not always). The initial (latent) stage has no characteristic manifestations. The clinic of the basic disease that caused the acute renal failure prevails (shock, acute poisoning, etc.). The oligo-anuric stage begins with a sharp decrease in diuresis of less than 500 ml per day up to anuria. Symptoms of uremia increase: severe weakness, loss of appetite, thirst; nausea, vomiting, headache, dizziness; fever. On inspection: patient is adynamic; skin becomes dry, desquamates; hemorrhagic rashes can occur on the skin, and subcutaneous hemorrhages are frequent; yellow sclera is also possible. On examination of the respiratory system: dyspnoea due to accumulation of fluid in the pleural cavity; in serious condition, Kussmaul's breath develops. On examination of the cardiovascular system: tachycardia, rhythm disturbances, (associated with hyperkalemia); displacement of the heart borders; dull heart sounds, systolic murmur at the heart apex, sometimes pericardial friction murmur; arterial hypertension. On examination of the gastro-intestinal tract: severe tongue and mouth dryness; the tongue is covered with white or brown coating, stomatitis often develops; gastrointestinal bleeding is observed in 10% of patients as a result of erosions and ulcers of the mucous membranes. Later, with the progression of the ARF, depression of consciousness develops, reflexes decrease, convulsions appear, and death is possible. Laboratory examination: blood analysis: anemia persists during all periods of ARF, leukocytosis is characteristic of the oligoanuric period; the content of residual nitrogen, creatinine, urea, potassium, phosphates in the blood increases; urinanalysis: specific gravity is decreased from the beginning of ARF. The protein content and urinary sediment depend on the cause of ARF. With a favorable outcome of the disease polyuric stage appears. The severity of azotemia is gradually reduced, homeostasis is restored, and clinical improvement observed. Complete recovery of renal function (concentrating mechanism and tubular reabsorption) can last for 12 months, but not always. CHRONIC RENAL FAILURE (CRF) is a symptom complex that is the outcome of any nephrological disease caused by an irreversible deterioration in renal function as a result of the death of the nephrons and their replacement with connective tissue. Initially, it is manifest only as a biochemical abnormality. Eventually, loss of the excretory, metabolic and endocrine functions of the kidney leads to the development of the clinical symptoms and signs of renal failure, which are referred to as uremia. Uremia is a pathological condition caused by a delay in the body of nitrogenous slags, acidosis, electrolyte, water and osmotic imbalance. Three conditional groups of factors can lead to CRF (Tab. 23). Table 23 Etiology CRF. Variant ARF Prerenal Renal Postrenal Reasons Renal artery stenosis Thrombosis of the vena cava inferior Chronic glomerulonephritis Chronic pyelonephritis Diabetes mellitus Polycystic kidney disease, etc. Prolonged urinary tract obstruction Clinical manifestations. Initially, it is manifest only as a biochemical abnormality. Typical signs of beginning CRF are polyuria and nocturia. Further, as the glomerular filtration rate (GFR) decreases, general symptoms appear: weakness, drowsiness, fatigue, apathy (uremic encephalopathy). The characteristic signs of СRF are anemia and arterial hypertension (possibly malignant). Anemia is usually correlates to the severity of CRF. Several mechanisms are implicated, including: relative deficiency of erythropoietin; diminished erythropoiesis due to the toxic effects of uraemia on marrow precursor cells; reduced red cell survival; increased blood loss due to capillary fragility and poor platelet function; reduced dietary intake and absorption of iron and other haematinics. For severe СRF, oliguria is characteristic. As a result of increasing intoxication, various organs are affected. Neurological symptoms increase up to the development of uremic coma, muscle cramps appears. Frequent signs of uremia: dyspeptic syndrome: nausea, vomiting, loss of appetite, diarrhea; increased bleeding; renal myopathy, osteodystrophy and osteomalacia as a result of calcium, phosphorus, vitamin D metabolic disorders, secondary hyperparathyroidism; severe cardiac abnormalities (arrhythmia, fibrinous pericarditis, heart failure) due to hyperkalemia and the toxic effect of creatinine and urea; dry and exudative (often hemorrhagic, with an increased concentration of creatinine in the pleural fluid) pleurisy; cellular and humoral immunity are impaired, with increased susceptibility to infection. Infections are the second most common cause of death in dialysis patients, after cardiovascular disease. On inspection: dry, pale skin with traces of scratching, due to excruciating itching; petechial rash, hematoma, edema; dry, brown tongue; muscle twitching, the smell of urine (ammonia) is felt from the mouth and skin of the patient. The key laboratory indicator for CRF is glomerular filtration rate. In the terminal stage of CRF, drug treatment is ineffective. Hemodialysis or kidney transplantation is necessary to prolong the life of the patient. Chronic Kidney Disease (CKD) Since 2006, the term Chronic Kidney Disease (CKD) has been adopted. CKD is a disease based on the death of a portion of the nephrons; in the remaining nephrons, compensatory structural and functional changes develop that lead to a decrease in the functional reserve of the kidneys. The diagnosis of "Chronic kidney disease" implies the inevitable further progression of the pathological process and is intended to attract the attention of a doctor in the early stages of its development. The presence of CKD should be established based on the following criteria: 1. The presence of any clinical markers of kidney damage confirmed twice with an interval of at least 3 months. Markers of Renal Damage: albuminuria ≥ 30 mg / 24 hours change in urinary sediment (hematuria, cylindruria) tubular dysfunction histological changes renal structural changes during imaging studies a history of kidney transplantation. 2. Any markers of irreversible structural changes in the kidneys detected once (biopsy or visualization). 3. A decrease in GFR < 60 ml / min / 1.73 m2 for 3 or more months, regardless of the presence or absence of other signs of kidney damage. Chronic kidney disease is divided into 5 stages by the level of GFR (Tab. 24). Stage 1 2 3a 3b 4 5 Table 24 Chronic kidney disease stages GFR ml/min Characteristic 90 and more high or optimal 60-89 slightly reduced 45-59 moderately reduced 30-44 significantly reduced 15-29 sharply reduced < 15 terminal renal failure The period of relative compensation for CKD can last several years. CKD should be suspected by a doctor if the patient has the following signs for more than 3 months: anemia of unknown origin, low specific gravity of urine (in several analyzes!), proteinuria, polyuria and nocturia, decreased GFR, arterial hypertension. RENAL DISEASES. Chronic pyelonephritis Chronic pyelonephritis is chronic inflammatory process, nonspecific bacterial etiology with predominant localization in the intersticium, obligatory affection of the calyx-pelvis system and further spreading pathological process оn the tubules and blood vessels. Clinically it is characterized by pain in the lumbar region, fever, dysuria, then edema, and arterial hypertension. Chronic glomerulonephritis Chronic glomerulonephritis is bilateral immuno-inflammatory process with predominant affection glomeruli and intersticium tubules and blood vessels involvement in the pathological process. Clinically it is characterized by edema-nephrotic and hypertensive syndromes. Amyloidosis Amyloidosis is a systemic disease, which is based on complex changes in metabolic processes, characterized by the deposition of a protein-polysaccharide complex (amyloid) in the tissues. Amyloidosis primarily affects the kidneys, as well as the heart and nervous system. Clinically it is characterized by edema-nephrotic syndrome. Urolithiasis Urolithiasis (nephrolithiasis) is a disease characterized by the formation of concrements in the urinary tract, which are formed from the urine constituents as a result of: - metabolic disorders associated with tubulopathies (oxalaturia, phosphaturia), hyperparathyroidism, and uric acid metabolism (urates); disturbance of urodynamics with stagnant urine. Clinically it is characterized by renal colic syndrome.