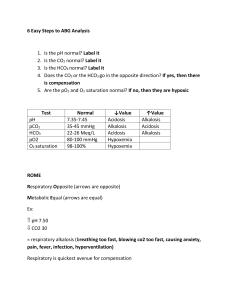
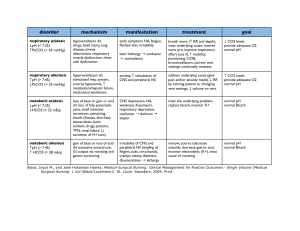
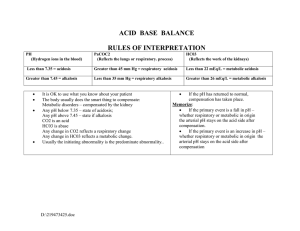
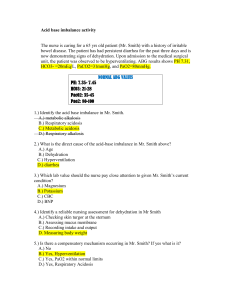
BLOOD GAS ANALYS : VENOUS AND ARTERIAL - Importance of O2 evaluation: adequate tissue oxygenation necessary for correct organ function When delivery ↓ consumption will also ↓ → switch to anaerobic metabolism w/ lactate production → late sign - O2 delivery (ml/min) = CO x arterial blood content (CaO2=1.34 x SaO2 x Hb) → insight on lung, heart, Hb ↓ O2 delivery will comes about only if compensatory mechanisms are not enough (delivery at baseline is x4 of actual need) - Arterial blood gas analysis = what is going on inside the cells - Venous blood gas analysis = O2 delivery vs consumption ARTERIAL BLOOD GAS BLOOD GAS ANALYSIS → info about: acid/base balance, gas exchange (oxygenation=PaO2, ventilation=PaCO2) - Used to: assess presence and severity of respiratory failure, monitor pts on ventilator, assess metabolic dysfunction - Normal values: pH : 7,35-7,45 → the value does not directly correlate with the severity of the situation: it depends on how fast the change occur and how much the pts is able to sustain it PaO2 : 80-100 mmHg (109-0.4xage) → hypoxemia < 80 mmHg, hypoxic respiratory failure < 60 mmHg PaCO2: 35-45 mmHg → hypercapnia > 50 mmHg HCO3: 24-26 mEq/L BE : +/- 2 mmol/L = amount of acid that would be need to buffer blood to a normal pH Lattato: < 1,5 mmol/L Na : 135-150 mEq/L K: 3,5-5 mEq/L Ca: 8,5-10,5 mEq/L Cl: 95-105 mEq/L - Step by step evaluation: 1) Is the BGA actually arterial? - Is SaO2 and PaO2 too low is probably venous - Consider parameters that can alter values: temperature, cell count (O2 consumption, analyze w/in 10 min) , air bubbles (↑PaO2) 2) Oxygenation → PaO2, PaO2/FiO2 ⇒ respiratory failure? Compare with PaCO2 to define type - Type 1 (lung failure): hypoxia + normo/hypocapnia - Type 2 (pump failure): hypoxia + hypercapnia 3) pH analysis ⇒ normal, alkalosis, acidosis ? 4) PaCO2 analysis + HCO3 ⇒ respiratory vs metabolic ? - PaCO2 is altered in the opposite direction of pH = respiratory → Mnemonic ROME = Respiratory Opposite, Metabolic Equal - HCO3 is altered in the same direction of pH = metabolic 5) Acute vs chronic + simple vs mixed condition (estimated compensation not satified) Respiratory acidosis For every 10 CO2 ↑ Respiratory alkalosis For every 10 CO2 ↓ Metabolic acidosis Metabolic alkalosis For every 1 HCO3 ↓ For every 1 HCO3 ↑ Acute Chronic Acute Chronic 6) If metabolic acidosis calculate AG to define etiology - ↑ AG : Acidosis due to ↑ metabolic acids w/ ↓ HCO3 in attempt to buffer - Normal AG: Acidosis due to loss of HCO3 (renal or extrarenal) w/ ↑ Cl Expected compensation 1 HCO3 ↑ 3 HCO3 ↑ 2 HCO3 ↓ 4 HCO3 ↓ 1 CO2 ↓ 0.5 CO2 ↑ Parameters and their meaning GAS EXCHANGE PARAMETERS - PaCO2: ventilation = volume of air transported btw alveoli and external air in 1 min Depends on : respiratory CNS centers, muscles, diaphragm Is the main trigger for ventilation: low PaCO2 → ↓RR by inhibit muscle function. In chronic hypercapnic pts PaCO2 is no longer used as stimulus bc loose sensitivity , PaO2 is instead used (hypoxic drive) → oxygen supplementation might suppress respiratory drive ! - Arterial blood O2 content = (0.0031 x PaO2) + (1,34 x [Hb] x SaO2) Distribution of O2 inside blood: 1% free (represented by PaO2) + 99% bound to Hb (carrying capacity) PaO2 = driving force for O2-Hb binding → affinity expressed by oxygen-Hb dissociation curve Factors ↓ affinity (O2 released in tissues) : acidosis (effetto Bohr) , ↑ T°, ↑ DPG, ↑ PaCO2 Factors ↑ affinity (O2 remains in the blood) : alkalsosi, ↓ T°, ↓ DPG, ↓ PaCO2 steep for values of PaO2 < 60 mmHg (SaO2 < 90%) → PaO2 unable to sustain Hb saturation for correct tissue oxygenation [Hb] = carrying capacity: how much O2 can be carried SaO2 = used carrying capacity =% of O2 binding sites on Hb carrying O2 (Hb saturation) - Oxygen delivery formula = cardiac output x arterial O2 content - SaO2 : O2 arterial transport - PaO2 : lung gas exchange Depends on: pts age, alveolar ventilation, V/Q, FiO2 (FiO2-PaO2≥10mmHg; FiO2 room air=21 %) - Horowitz index = PaO2 / FiO2 (n.v ≥ 300) → if < 300: gas exchange alteration Considered alone is more informative than PaO2 ACID BASE BALANCE PARAMETERS - Acids (H+) Come from metabolic activity in the form of CO2 and metabolic acids Excretion by : respiration (CO2, regulated by RR), renal metabolism (H+ excretion, HCO3 reabsorption) Detrimental effect of acidosis on protein structure - Maintenance of electrolyte neutrality : Expressed by Anion Gap = difference btw positive charged electrolytes and negatively charged electrolytes that can be measured in lab = unmeasured anions AG = (Na+K) – (Cl + HCO3) = 12±4 (or 10±2 if K not counted) + charged: Na+ exchanged with H or K → H and K increase and decrease together - charged: Cl- and HCO3- balance each other by exchanging → one rise while the other fall Must be corrected with albumin: AG ↑ by 2.5 mEq/L for every 1 g/dL ↓ in serum albumin ↓ AG = wasting of ions (diarrhea, vomiting, renal tubule acidosis) ↑ AG = metabolic alterations (sepsis, liver disease, intoxication) Main alterations and causes: - Simple / Primary acid-base disorder = single process of alkalosis / acidosis due to change in PCO2 or HCO3 - Compensation = normal respiratory or kidney response to pH change - Mixed acid-base disorder = ≥1 acid-base disorder together • Acidosis - CP : ↑ RR (Kausmall respiration as compensation mechanism), fatique, lethargy, coma - Respiratory acidosis: alveolar hypoventilation due to : pulmonary edema, BPCO, airways obstruction, thoracic trauma, neuromuscular disease, opioid overdose, coma, compensation of metabolic alkalosis - Metabolic acidosis ↑ AG : Acidosis due to ↑ metabolic acids w/ ↓ HCO3 in attempt to buffer : lactic acid (shock, sepsis), diabetic ketoacidosis, alcholic acidosis, renal insufficiency, salycilate, uremia Confirm lactic acidosis: lactate ≥ 50% of BE Low or Normal AG: Acidosis due to loss of HCO3 (renal or extrarenal) w/ ↑ Cl : tubular renal acidosis, diarrhea, physiological solution infusion (high Cl), post hypocapnia, spironolactone, aacetazolamide • Alkalosis - CP: ↓ RR (compensatory bradypnea), shallow breathing, vertigo, confusion, irritable state Respiratory alkalosis: hyperventilation due to initial phase of pulmonary embolism (n.b unresponsive to O2 delivery, check right ventricle dilation at eco cardio),panic attack, fever, pregnancy, hypoxia, high altitude Metabolic alkalosis: loss of acid gastric secretion (vomit, NG tube), dehydration, loss of H+ (loop diuretics loosing K+), antacid intoxication, Cushing, primary aldosteronism, diarrhea with loss of Cl-, hypocalcemia, cirrhosis, HCO3 reabsorption, HCO3 exogenous VENOUS BGA - Represent scvO2 = central venous oxygen saturation Measured by central venous catheter = tip lies in superior vena cava close to the right atrium (access is variable: subclavian, internal jugular, femoral) Other indications beside VBGA: drug infusion, unavailable peripheral venous access, dialysis, need for a long-term venous access Represent how much of the delivered arterial blood O2 has been unutilized by cells → ScvO2 = O2 delivery / O2 consumption ⇒ you don’t know the absolute values but only if O2 delivery is enough Is a flow-weighted representation (higher flow=more represented) of blood with different O2 saturations from different vascular beds all mixing inside the inferior vena cava → is a marker of general oxygenation state, not informative for the single organ → an ischemia of a low flow organ can be completely masked if high flow organs are not affected → check for specific organ signs of hypoperfusion - Difference btw venous and arterial blood: lower pH, higher PCO2, lower pO2, lower SaO2, comparable amount: Hb, glucose, lactate, electrolytes - When a venous BGA is enough (easier to perform, so if you can avoid an arterial one is better): Define levels of : Hb, glucose, lactate, electrolytes Rule out respiratory acidosis Rule out hypercapnia Rule out respiratory failure - When a venous BGA is NOT enough Evaluation of arterial oxygenation (PaO2, SaO2) → pulse oximetry might be enough, arterial BGA is not always required (oxy-Hb dissociation curve=relation btw PaO2 and SaO2 → if SaO2 is 100% you can rule out hypoxemia) cvSaO2 values : - Lactate is a late sign as it comes about only in the emergency range, so look out for intermediate values of abnormalities - < 50% : easier interpretation, check for: ↓ Delivery (DO2) Lung (hypoxemia) : pulse oximetry (SaO2) → if 100% you can rule out a respiratory problem Hb (anemia) measure it via venous BGA Heart (low tissue perfusion) : if lung and Hb is normal, conclude is an heart problem by exclusion ↑ Consumption (VO2) : fever, pain, shivering, respiratory effort, muscle activity, agitation - Normal / > 85% (no cellular extraction) → cannot rule out localized tissue hypoxia, check for hypoperfusion signs (altered mental status, hyperlactatemia, mottled skin, oliguria, hypotension, tachycardia) Summary for bedside assessement