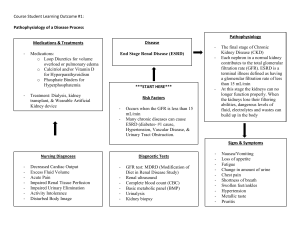
Case 3 A 53-year-old woman with endometriosis comes to the physician because of bilateral flank pain and decreased urine output for 1-week. She has not had any fevers, chills, or dysuria. Physical examination shows several surgical scars on her abdomen. Laboratory studies show a serum creatinine concentration of 3.5 mg/dL. A CT scan of the abdomen shows numerous intra-abdominal adhesions, as well as dilatation of the renal pelvis and proximal ureters bilaterally. An increase in which of following is the most likely underlying mechanism of this patient's renal dysfunction? This patient has bilateral hydronephrosis secondary to post-surgical adhesions. Hydrostatic pressure in the tubules In this patient, bilateral occlusion of the urinary system due to post-surgical adhesions increases intraluminal ureteral pressure, which leads to increased hydrostatic pressure in the renal tubules and Bowman capsule. Because the glomerular hydrostatic pressure is unable to overcome this increase in the tubular hydrostatic pressure there is a reduction in the net glomerular filtration rate (GFR), as manifested by this patient's elevated serum creatinine. Sustained elevation of intratubular pressure can cause compression of surrounding renal blood vessels, which ultimately can lead to ischemic tubular atrophy, thinning of the renal cortex and medulla, and irreversible loss of renal function. Osmotic pressure in the glomeruli Increased osmotic pressure in the glomerular capillaries would oppose the net flow of water across the capillary walls, leading to a decrease in GFR. However, osmotic pressure in the glomeruli is driven by osmotically-active solute concentration, which remains unchanged in hydronephrosis. Therefore, this cannot be the primary mechanism of renal dysfunction in hydronephrosis. Hydrostatic pressure in the efferent arteriole Hydrostatic pressure in the efferent arteriole is primarily driven by the muscle tone of the efferent arterioles (which is predominantly regulated by RAAS). Vasoconstriction of the efferent arterioles reduces the renal plasma flow but increases the glomerular filtration rate and filtration fraction by increasing glomerular hydrostatic pressure. In this patient, however, elevated serum creatinine concentration suggests renal dysfunction with a reduced glomerular filtration rate. Osmotic pressure in the afferent arteriole An increase in osmotic pressure in the afferent arteriole would cause a decrease in the net flow of water across the capillary walls into the afferent arteriole. Based on the Starling equation, an increase in the osmotic pressure in the afferent arteriole would lead to a net decrease in GFR. However, this is not the mechanism behind the decrease in GFR seen with hydronephrosis, in which the solute concentration of the blood remains unchanged. Osmotic pressure in the tubules Osmotic pressure in the tubules is regulated by osmotically active solutes such as sodium and urea. Increased osmotic drive towards the inside of tubules can be observed after the administration of osmotically-active substances (e.g., mannitol). Hydronephrosis can lead to changes in the ability of the tubules to secrete and absorb solutes, but this is not the primary mechanism for the renal dysfunction seen with hydronephrosis.