PHCY 507 Endocrine Test 1
advertisement
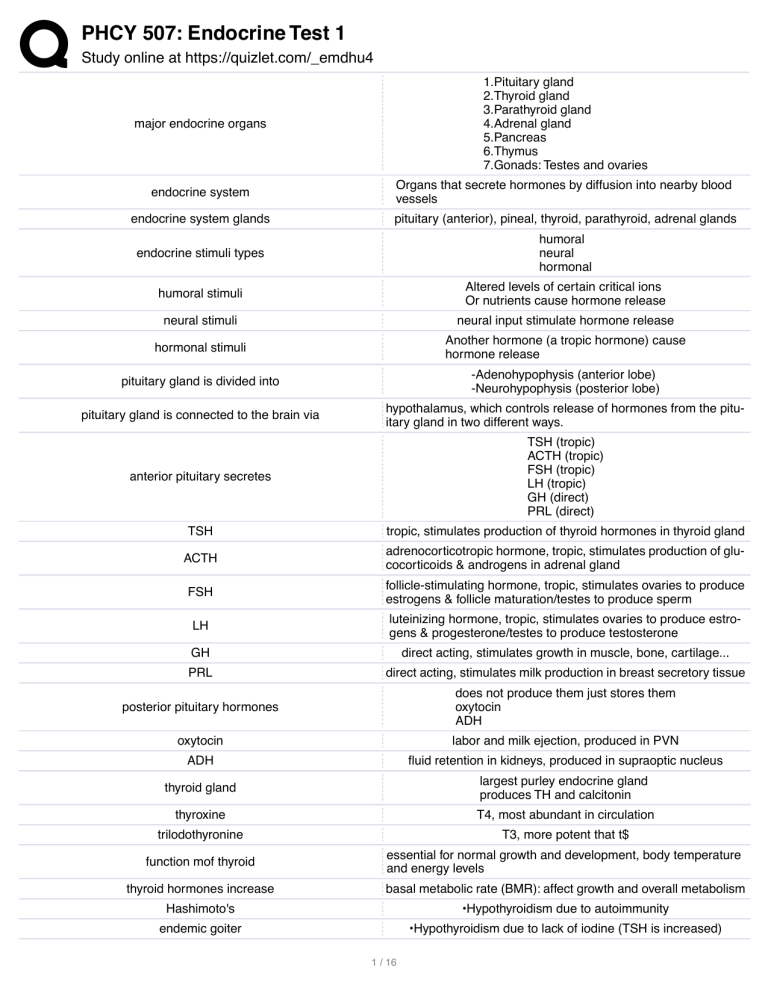
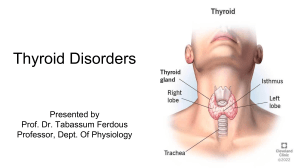
PHCY 507: Endocrine Test 1 Study online at https://quizlet.com/_emdhu4 major endocrine organs 1.Pituitary gland 2.Thyroid gland 3.Parathyroid gland 4.Adrenal gland 5.Pancreas 6.Thymus 7.Gonads: Testes and ovaries endocrine system Organs that secrete hormones by diffusion into nearby blood vessels endocrine system glands pituitary (anterior), pineal, thyroid, parathyroid, adrenal glands endocrine stimuli types humoral neural hormonal humoral stimuli Altered levels of certain critical ions Or nutrients cause hormone release neural stimuli neural input stimulate hormone release hormonal stimuli Another hormone (a tropic hormone) cause hormone release pituitary gland is divided into -Adenohypophysis (anterior lobe) -Neurohypophysis (posterior lobe) pituitary gland is connected to the brain via hypothalamus, which controls release of hormones from the pituitary gland in two different ways. anterior pituitary secretes TSH (tropic) ACTH (tropic) FSH (tropic) LH (tropic) GH (direct) PRL (direct) TSH tropic, stimulates production of thyroid hormones in thyroid gland ACTH adrenocorticotropic hormone, tropic, stimulates production of glucocorticoids & androgens in adrenal gland FSH follicle-stimulating hormone, tropic, stimulates ovaries to produce estrogens & follicle maturation/testes to produce sperm LH luteinizing hormone, tropic, stimulates ovaries to produce estrogens & progesterone/testes to produce testosterone GH direct acting, stimulates growth in muscle, bone, cartilage... PRL direct acting, stimulates milk production in breast secretory tissue posterior pituitary hormones does not produce them just stores them oxytocin ADH oxytocin labor and milk ejection, produced in PVN ADH fluid retention in kidneys, produced in supraoptic nucleus thyroid gland largest purley endocrine gland produces TH and calcitonin thyroxine T4, most abundant in circulation trilodothyronine T3, more potent that t$ function mof thyroid essential for normal growth and development, body temperature and energy levels thyroid hormones increase basal metabolic rate (BMR): affect growth and overall metabolism Hashimoto's •Hypothyroidism due to autoimmunity endemic goiter •Hypothyroidism due to lack of iodine (TSH is increased) 1 / 16 PHCY 507: Endocrine Test 1 Study online at https://quizlet.com/_emdhu4 grave's disease Most common type of hyperthyroidism Immune system makes abnormal antibodies that mimic TSH: oversecretion of TH Sx: nervousness, weight loss, sweating, rapid HR, ... parathyroid glands small pea-like organs that regulate calcium and phosphate balance in blood, bones, and other tissues parathyroid hormone increases blood calcium levels oxyphil cells increase in # as body ages, unknown function adrenal glands adrenal cortex and adrenal medulla adrenal cortex secretes corticosteroids (mineralocorticoids, glucocorticoids, androgens) adrenal medulla -stores & releases epinephrine and norepinephrine (upon sympathetic stimulation) 3 zones of adrenal cortex •Zona glomerulosa: tufts of cells; mineralocorticoids (aldosterone) •Zona fasciculata: cords of cells; glucocorticoids (cortisol) •Zona reticularis: abundant reticular fibers (boundary between medulla and cortex) (dehydroepiandrosterone) glucocorticoids influence function of most cells in the body Part of stress response Modulates immune response stimulate gluconeogenesis and release of insulin net increase of fat deposition in certain areas Cushing's syndrome hyper secretion of glucocorticoid hormones (usually a pituitary tumor) Mineralocorticoids (Aldosterone) Na and fluid retention in kidney ’ ‘ blood volume ’ ‘ BP aldosterone secretion is subject to •ACTH •Angiotensin pancrease exocrine gland: secrete digestive enzyme and endocrine gland: islets secrete hormones endocrine pancrease controls blood glucose homeostasis, secrete glucagon and insulin alpha cells of pancreas secrete glucagon glucagon Signal liver to metabolize glycogen into glucose, and the adipose tissue to metabolize triglycerides into glucose ’ raise blood sugar beta cells of pancrease secrete insulin insulin Signal most body cells to take up glucose from the blood after a meal ’ lower blood sugar delta cells of pancrease secrete somatostatin: Inhibit secretion of insulin and glucagon F (PP) cells of pancreas secrete pancreatic polypeptide: May inhibit exocrine activity of the pancreas thymus •Located in the lower neck and anterior thorax. Superior to heart, within mediastinum •Important immune organ: site of T cell maturation after release from bone marrow, stimulated by thymic hormones (thymopoietin and thymosin) testes •Interior divided into lobules containing seminiferous tubules •FSH & LH from anterior pituitary secrete androgens (testosterone) ovaries •Interior divided into cortex (follicles) and medulla (blood supply) •FSH, LH from anterior pituitary stimulate follicle development ovaries secrete -Estrogen à maintain reproductive organs, secondary sex characteristics -Progesterone à preparation of uterus for pregnancy 2 / 16 PHCY 507: Endocrine Test 1 Study online at https://quizlet.com/_emdhu4 thyroid function •Responsible for the formation and secretion of three thyroid hormones as well as iodine homeostasis within the body three hormones that thyroid produce in the body •Triiodothyronine (T3) •Thyroxine (Tetraiodothyronine) (T4) •Calcitonin calcitonin hormone that regulates circulating levels of calcium 1. hypothalamus releases thyroid-releasing hormone (TRH) 2. Tells the anterior pituitary to synthesize and release TSH Thyroid function controlled by thyroid-releasing hormone and thy3. Tells thyroid to make two iodine-containing hormones: Thyroxine roid-stimulating hormone (TSH) (T4) and Triiodothyronine (T3) 4. Enzymatic reactions lead to incorporation of iodide into active T3 and T4 Thyroid hormone production negatively regulates TRH & TSH release through a negative feedback loop iodine organification •DIT + DIT’ thyroxine (T4) •DIT + MIT ’ triiodothyronine (T3) Thyroxine and T3 in plasma are reversibly bound to protein, primarily thyroxine-binding globulin (TBG) Most thyroid hormone in blood is T4 normal range for total T4 5-12 normal range for total T3 82-180 normal range for free thyroxine 0.8-1.9 normal range for TSH 0.4-4.0 hypothyroidism Defined as the clinical and biochemical syndrome resulting from decreased thyroid hormone production primary hypothyroidism Hashimoto's thyroiditis hashimoto's disease is also called autoimmune thyroiditis Hashimoto disease presentation Patients may present either with goitrous thyroid gland enlargement and mild hypothyroidism or with thyroid gland atrophy and more severe thyroid hormone deficiency. goiter “T3/T4 ’ ‘‘TSH secretion (feedback) ’ trophic stimulation of thyroid Common Signs & Symptoms of Hypothyroid Disease •S leepiness, fatigue, lethargy •L oss of memory •U nusually dry, coarse skin •G oiter •G radual personality changes •I ncrease of weight, or puffiness •S ensitivity to cold •H air loss, sparseness of hair hypothyroidism clinical presentation slowing down of all body functions •In infants and children ’ striking retardation of growth and development, e.g. dwarfism and mental retardation (cretinism) extreme case of hypothyroidism myxedema coma myxedema coma •Early symptoms of myxedema: •Increased sensitivity to cold •Fatigue •Heavier menstruation •Depression •Weight gain •Late symptoms •Slow speech •Decreased taste/smell 3 / 16 PHCY 507: Endocrine Test 1 Study online at https://quizlet.com/_emdhu4 •Puffy extremities •Coma ’ Death Subclinical Hypothyroidism •Increased TSH WITHOUT specific symptoms •Highest incidence in the elderly •Often progresses to diagnosed hypothyroidism highest risk for subclinical hypothyroidism •Initial TSH > 20 mIU/mL •High initial antibody titers Pharmaceutical (Generic) Equivalence •Products with same active ingredient, and identical dosage form, strength, and route of administration bioequivalence Generic equivalents with similar Cmax, Tmax and AUC (80-125% of the standard) Therapeutic Equivalence Pharmaceutical equivalents meeting FDA, USP, and Current Good Manufacturing Practices (Presumed similar E/S profiles) drugs with a narrow therapeutic index extended phentyoin, digoxin, lithium carbonate, conjugated estrogens, carbamazepine, warfarin, levothyroxine •95% of hypothyroid patients are hyperlipidemic Correlation of Serum TSH and Cholesterol in Hypothyroid Patients •Correction of hypothyroidism normalizes cholesterol in majority of patients hyperthyroidism Defined as a syndrome with EXCESS thyroid hormone production Causes of Hyperthyroidism •Graves' Disease •Toxic Uninodular Goiter •Multinodular Goiter •Jod-Basedow •Factitious •Drugs •Thyroiditis •Tumor graves disease An autoimmune syndrome that usually includes: •Hyperthyroidism •Diffuse thyroid enlargement •Exophthalmos •Pretibial myxedema (less common) •Thyroid acropachy graves disease patho 1. Antibodies bind to and stimulate TSH-R 2. Stimulate growth and biosynthetic activity of the thyroid cell 3. Excessive amounts of thyroid hormone synthesis Toxic Uninodular Goiter •Discrete thyroid mass whose function is independent of pituitary and TSH control. Arises from gain-of-function somatic mutations of the TSH receptor, the Gs± prote multinodular goiter •Follicles with autonomous function coexist with normal or even nonfunctioning follicles •Diffuse hyperplasia caused by goitrogenic stimuli, leading to mutations and clonal expansion of benign neoplasms Common Signs & Symptoms of Hyperthyroid Disease •Flushed, Moist Skin •Thinning of hair •Proptosis, lid lag •Pretibial myxedema •Palmar erythema •Brisk DTR's •Goiter Tremor •Weakness, fatigue •Nervousness •Muscle aches •Weight Loss •Heat Intolerance 4 / 16 PHCY 507: Endocrine Test 1 Study online at https://quizlet.com/_emdhu4 •Palpitations •Amenorrhea •Diarrhea Hyperthyroidism Clinical Presentation Excess levels of thyroid hormone •Symptoms include high temperature, high metabolic rate, excessive alertness, etc. •Resembles sympathetic nervous system overactivity (esp. on CV system) extreme case of hyperthyroidism thyroid storm Acute exacerbation of all symptoms: •Agitation, alertness, confusion, rapid heart rate, increased systole, shaking, sweating •Can develop CHF and Pulmonary edema ’ death treatment of hyperthyroidism surgery radioactive iodine drug therapy Clinical and laboratory evaluations should be performed for thyroid hormone •~6-week intervals at initiation and dose adjustments •Annually once a euthyroid state is established under replacement of thyroid hormone risks •Continued hypothyroid state •Hyperlipidemia •Decreased heart rate and ventricular contractility •Increased peripheral resistance and diastolic pressure •Memory loss •Fatigue Depression over replacement of thyroid hormone risk •Induced hyperthyroid state •Increased heart rate and myocardial contractility •For cardiac patients, increased risk of angina and myocardial infarction •Reduced bone density (osteoporosis) thyroid hormone in pregnancy •Treat even mildly elevated TSH •Increase T4 replacement by 30% with 1st detection of pregnancy •Monitor TSH and adjust dose accordingly •Routine screening suggested Inappropriate Uses of THR Therapy •Obesity •Chronic Fatigue •Short Stature •Infertility Parathyroid Glands •Small endocrine glands located on the back of the thyroid in variable locations •Responsible for production and secretion of parathyroid hormone in response to a low blood calcium Parathyroid Hormone (PTH) •The most important endocrine regulator of calcium and phosphorus concentration in extracellular fluid •Secreted from the parathyroid glands Major targets: bone and kidney synthetic TH drugs •Levothyroxine: T4 - preparation of choice •Liothyronine: T3 •Liotrix: Levothyroxine + Liothyronine (4:1) TH drugs boxed warning DO NOT use to treat obesity if levels are normal (not effective/detrimental). levothyroxine •Synthetic version of endogenous T4 (thyroxine) levothyroxine MOA activation of all receptors for T4, converted to T3 and activates T3-R •Preparation of choice for thyroid replacement and suppression therapy levothyroxine 5 / 16 PHCY 507: Endocrine Test 1 Study online at https://quizlet.com/_emdhu4 levothyroxine AE hyperthyroid-related due to therapeutic overdosing (‘HR, palpitations, sweating, weight loss, arrhythmias, irritability) Liothyronine T3, cytomel liothyronine cons shorter half life expensive liothyronine pros 3-4x more potent than levothyroxine liothyronine AE hyperthyroidism with OD liothyronine CI patients with cardiac disease liotrix •Levothyroxine + Liothyronine (4:1) •Tablet •No advantage over levothyroxine alone •Available, but almost never indicated (cost) dessiccated USP thyroid armour thyroid •Animal origin (porcine) •~100 mg of desiccated thyroid = 100 mcg levothyroxine + 37.5 mcg of liothyronine •NOT recommended •protein antigenicity •variable potency and stability •difficulty in lab monitoring If a woman with hypothyroidism becomes pregnant, her dose of levothyroxine will need to be: increased Antithyroid drug therapy 1.Thioamides 2.Iodides 3.Anion Inhibitors adjunctive therapy for hyperthyroidism Adrenoreceptor-blocking agents radioactive iodine •Preferred for most patients over 21 (easy, effective, cheap, painless). •Antithyroid therapy prior to administration. •80% develop hypothyroidism afterwards. thioamides MOA 1.Prevent hormone synthesis by inhibiting thyroid peroxidase and interfering with the incorporation of iodine into tyrosyl residues of thyroglobulin 2.Block coupling of MIT and DIT 3.PTU also partially inhibits peripheral deiodination of T4 à T3 methimazole •Drug of choice for Graves' disease , 10x more potent than PTU propylthiouracil •Class prototype, but Black box warning for severe liver injury & acute liver failure ’ only used if: •Cannot tolerate methimazole, and radioactive iodine/surgery are not appropriate •Thyroid storm First trimester pregnancy thioamides adverse events •Nausea, GI upset, skin rash (4-6%), +/- fever. Other rare reactions (vasculitis, lupus-like reactions) •Propylthiouracil: black box warning for severe liver damage Methimazole AE most severe (very rare) event is agranulocytosis = potentially fatal, rapidly reversible with D/C of drug and CSFs propylthiouracil black box warning severe liver damage Iodides MOA •Excessive iodide in thyroid temporarily inhibits iodide organification and hormone release •Decrease size and vascularity of hyperplastic thyroid gland iodides AE •Rare & mostly reversible: rash, swollen salivary glands and risk of mucous membrane ulcerations, conjunctivitis, rhinorrhea, metallic 6 / 16 PHCY 507: Endocrine Test 1 Study online at https://quizlet.com/_emdhu4 taste, bleeding disorder •GI upset (take with food to decrease ) Anion Inhibitors MOA Competitively block iodide uptake through NIS Anion Inhibitors thiocyanate, no longer used Adrenoreceptor Blockers Symptomatic therapy, no effect on the thyroid itself Adrenoreceptor Blockers drugs B-blockers: metoprolol, propranolol, atenolol adrenoreceptor blockers CI •Decompensated HF •If non-cardioselective selective, care must be taken in asthmatics and with COPD! Radioactive Iodine (131I) •Oral administration (solution/capsule) •Rapidly absorbed, concentrated in the thyroid, incorporated into colloid of follicles without endangering other tissues Radioactive Iodine (131I) MOA •emits beta-rays with effective t1/2 = 5-8 days. Within weeks, thyroid parenchyma is destroyed with epithelial swelling and necrosis, edema, leukocyte infiltration. •Patients should be euthyroid before RAI (antithyroid drugs first) Radioactive Iodine (131I) advantages ease of administration, efficacy, low expense, painless Radioactive Iodine (131I) CI pregnant women or nursing mothers (fetal thyroid will concentrate the isotope) levothyroxine med chem T4 widely used prohormone antacids and cations reduce absorption t3/t4 mixture armour thyroid liothyronine med chem T3 hormone bypasses bodys control of metabolism shorter half life than T4 propylthiouracil med chem inhibit thyroid peroxidase prevent formation of T3 and T4 use gloves when handeling methimazole med chem inhibit thyroid peroxidase prevent formation of T3 and T4 use gloves when handeling cincacalcet med chem Increases sensitivity of calcium-sensing receptor of parathyroid gland Lowers parathyroid hormone and serum levels of calcium etelcalcetide med chem Allosteric activator of the calcium-sensing receptor of the parathyroid gland somatostatin •Growth hormone inhibiting hormone ØInhibits the release of growth hormone ØInhibits the release of thyroid stimulating hormone •Produced by pancreas •Peptide hormone (pre-hormone) Half-life is 2-3 minutes octreotide med chem cyclic peptide (prevent metabolism) inhibits growth hormone secretion lanreotide med chem cyclic peptide (prevent metabolism) inhibits growth hormone secretion pasireotide med chem cyclic peptide (prevent metabolism) inhibits growth hormone secretion 40 fold more potent than octreotide two necessary parts of clinical guidelines systematic review and set of recommendations rigorously conducted systematic reviews should use meta-analysis 7 / 16 PHCY 507: Endocrine Test 1 Study online at https://quizlet.com/_emdhu4 PRISMA outlines the minimum set of items required for a systemic review or meta analysis systematic reviews contain a focused questions a methods section with defined inclusion and exclusion criterai and predefined literature search strategy key questions in study should define the following type of population type of exposure/intervention comparator of interest outcome of interest GRADE assessment evaluating the strength of evidence for each major outcome and for each comparison made hypothyroidism treatment for pt 15-50 year old treatment levothyroxine 50-100, FU in 6 weeks hypothyroidism treatment for pt >50 or heart disease levothyroxine 25-50 mg, FU in 6 weeks liothyroxine half life short, require multiple daily dosing liothyroxine greater risk of cardiac toxicity liothyroxine indication treatment of myxedema coma •NOT recommended for routine replacement therapy •Best used for the short-term suppression of TSH liothyroxine CI •Uncorrected adrenal cortical insufficiency •Untreated thyrotoxicosis liothyroxine AE •Cardiac dysrhythmia •Myocardial infarction •Tachycardia Hyperthyroidism liothyroxine DI •Oral anticoagulants and vasopressors liotrix components •Combination therapy of T3 and T4 •Physiologic ratio of 4:1 •1 grain (65mg) equivalent to approximately 60 ¼ g of T4 Preparation of choice for thyroid replacement and suppression therapy levothyroxine levothyroxine CI acute myocardial infarction, thyrotoxicosis, uncorrected adrenal insufficiency levothyroxine administration on empty stomach for best absorption Six populations of thyroid hormone replacement patients especially at risk with inconsistent T4 dosing: •Pregnant women •Infants •Thyroid cancer patients •Patients with preexisting cardiac disease •Older persons •Patients with preexisting skeletal disease treating hypothyroidism in pregnancy •Treat even mildly elevated TSH •Monitor TSH monthly and adjust dose accordingly goal TSH in pregnancy goal 0.1-3.0 mIU/L treating hypothyroidism in thyroid cancer •Goal: inhibit TSH secretion (0.1-0.2 mIU/mL), which will inhibit growth of thyroid cells, without causing overt HTR •Post thyroidectomy use higher T4 doses treating thyroid issues in patients with preexisting cardiac disease Start low (12.5 mcg) and go slow (12.5-mcg increments every 6-8 weeks). treating thyroid issues in patients with osteopenia/osteoporosis watch for over-replacement treating thyroid issues in older patients •Start low (12.5 mcg) and go slow (12.5-mcg increments every 6-8 weeks). •Cholestyramine •Colestipol •Aluminum Antacids 8 / 16 PHCY 507: Endocrine Test 1 Study online at https://quizlet.com/_emdhu4 drugs the decrease absorption of thyroid hormone •Ferrous Sulfate •Sucralfate •Raloxifene •Di- and Tri-valent Cations drugs that increase metabolism of thyroid hormone •Traditional anti-epileptic drugs (PB, PHT, CBM) •Rifampin subclinical hypothyroidism •Increased TSH without specific symptoms •Highest incidence in the elderly highest risk patients for subclinical hypothyroidism •Initial TSH > 20 mIU/mL •High initial antibody titers myxedema coma treatment •Treat underlying disorder •IV Glucocorticoids (HC 100 mg ) •High-dose IV levothyroxine or triiodothyronine •CV/Respiratory support •Treatment of hypothermia, hypoglycemia, hyponatremia hyperthyroidism In young patients/small glands/mild disease treatment antithyroid drug therapy thioamides anion inhibitors iodines hyperthyroidism treatment in most patients over 21 radioactive iodine thioamides Methimazole Propylthiouracil methimazole in treatment of hyperthyroidism Drug of choice in adults & children 10x more potent than PTU patient should report fever, sore throat, and flu like symptoms t1/2 = 6 h propylthiouracil in treatment of hyperthyroidism Indicated only in: •First trimester pregnancy •Thyroid storm •Adverse reaction to methimazole potassium iodine brand names •SSKI (38 mg/drop) - better palatability •Lugol's Solution (6 mg/drop) •Thyro-Block (potassium iodide 130 mg) potassium iodine MOA •Block thyroid hormone release •Inhibit organification •Inhibit peripheral T4 conversion •Decrease gland size/vascularity iodines advantages •Prompt effectiveness, useful for thyroid storm •Effective adjunct for surgery iodines disadvantages •Can't use alone •May delay onset of thioamide therapy or delay treatment with radioactive iodine (‘intraglandular stores of iodine) •CI's: pregnancy; pts with nodular goiter or adenomas; prior to RAI •Allergic reactions "Escape phenomenon" iodines AEs •Rare & mostly reversible: rash, swollen salivary glands and risk of mucous membrane ulcerations, conjunctivitis, rhinorrhea, metallic taste, bleeding disorder •May induce hyperthyroidism in susceptible patients (make it worse) adrenoreceptor blockers in hyperthyroidism Provide symptomatic improvement, with no change in the etiology of the disease treatment of choice for hyperthyroidism in pregnancy Low-dose PTU (MMI in 2nd and 3rd trimester) Maintain FT4 in high-normal range 9 / 16 PHCY 507: Endocrine Test 1 Study online at https://quizlet.com/_emdhu4 treatment of choice for toxic nodular goiter RAI therapy Surgery Avoid Iodides! treatment of choice for thyroiditis Usually self-limited Inflammatory in nature Treat symptomatically with NSAID (or steroid) and BB as needed Look for subsequent transient hypothyroidism neonatal thyrotoxicosis treatment of choice Treat with thioamides and/or beta blockers treatment of choice for iodine induced HTR disease Due to excessive iodine ingestion (Jod-Basedow) Discontinue source of iodine Usually self-limited treatment of choice for thyrotoxicosis factitia Due to excessive thyroid hormone administration Discontinue or decrease dose of thyroid hormone treatment of choice for pituitary adenoma Rare cause of HTR Requires neurosurgical resection treatment of choice for subclinical hyperthyroidism > 65 years old Concerns of CVD (angina, arrhythmias) Concerns of Osteoporosis Concerns of symptomatic HTR treatment of choice for thyroid storm Supportive Therapy Fluids, Fever, Nutrition Treat precipitating event High dose PTU Iodide Therapy Beta blocker Therapy IV Glucocorticoids adrenocorticosteroids glucocorticoids mineralcorticoids androgen, estrogen, and progesterone glucocorticoids function intermediary metabolism and immune function, cortisol mineralcorticoids function salt retaining activity aldosterone cortisol is also know as hydrocortisone cortisol function •Regulates intermediary metabolism (intracellular conversion of nutrients to cellular components), CV function, growth, immunity •Tightly regulated synthesis and secretion, tight negative feedback loop cortisol responds to physio/psychological stress to maintain homeostasis (stress can override negative feedback control) cortisol MOA Glucocorticoid receptor agonist Regulates gene transcription cortisol physiologic effects •Extensive - influence the function of most cells in the body, generally via direct intracellular actions •Important permissive effects: Deficiency of physiological levels of cortisol attenuates physiological response to other hormones (e.g. catecholamines) cortisol metabolic effects •Stimulate gluconeogenesis •Increase serum glucose levels à release of insulin. • •Stimulate hormone-sensitive lipase and thus lipolysis •However, insulin à lipogenesis too much cortisol can lead to decreased muscle mass, skin thinning and osteoporosis cortisol anti-inflammatory and immune suppressing effects Dramatic decrease in inflammation modulation of leukocyte function, suppressing inflammatory cytokines and chemokines 10 / 16 PHCY 507: Endocrine Test 1 Study online at https://quizlet.com/_emdhu4 cortisol effects in CNS •Too low à apathy, depression, irritability, and even psychosis •Too much à behavioral disturbances like insomnia and euphoria followed later by depression cortisol effect in GI tract •Large amounts associated with peptic ulcers aldosterone secretion in subject to •Angiotensin II •ACTH aldosterone MOA Gene transcription upon binding to mineralocorticoid receptor aldosterone effects •Renal reabsorption of sodium & potassium excretion in the kidney •Reabsorption of sodium in sweat, salivary glands, GI mucosa, across cell membranes aldosterone AE •Increased plasma volume •Hypertension •Hypokalemia •Metabolic alkalosis disease with too much cortisol cushings syndrome disease with too much aldosterone hyperaldosteronism disease with too little cortisol and aldosteron adrenal insufficiency (Addison's disease) cushing's syndrome Constellation of clinical features that result from chronic exposure to excess glucocorticoids of any etiology (hypercortisolism) ACTH-producing pituitary adenoma ("Cushing disease") cushing's syndrome treatment •Surgical removal of tumor is the treatment of choice, but not always effective •Adjuvant therapy with pharmacological inhibitors: •Inhibitors of ACTH secretion •Inhibitors of adrenal steroidogenesis •Inhibitors of glucocorticoid receptors primary aldosteronism excess production of aldosterone by the adrenal zona glomerulosa, most common cause of mineralcorticoid excess hyperaldosteronism can cause resistent hypertension peripheral edema severe hypokalemia metabolic alkalosis Aldosterone excess may cause direct damage to the myocardium and the kidney glomeruli Patients with primary aldosteronism (AKA Conn's syndrome) show increased rates of osteoporosis, type 2 diabetes, and cognitive dysfunction hyperaldosteronism treatment •surgery •Pharmacological treatment for not surgical candidates: MR antagonists Primary adrenal insufficiency Addison's disease, structural or functional lesions of the adrenal cortex (autoimmune) Secondary adrenal insufficiency structural or functional lesions of the anterior pituitary or hypothalamus Addison's disease symptoms •weakness, fatigue, weight loss, hyperpigmentation, inability to maintain blood glucose level while fasting. hypotension, circulatory shock and death Addison's disease treatment DAILY glucocorticoid (hydrocortisone) and mineralocorticoid (fludrocortisone) replacement, increased during periods of stress acute adrenal crisis •Life-threatening, emergency presentation •Requires large doses of GCs (parenteral hydrocortisone), fluid and electrolyte correction, and tx of underlying cause •Characterized by GI symptoms (N/V, abdominal pain), dehydration, hyponatremia, hyperkalemia, hypoglycemia, weakness, lethargy, and hypotension. •Usually associated with disorders of the adrenal rather than the 11 / 16 PHCY 507: Endocrine Test 1 Study online at https://quizlet.com/_emdhu4 pituitary or hypothalamus and sometimes follows abrupt withdrawal of GCs used at high doses or for prolonged periods. synthetic corticosteroids MOA GR agonists, mimicking cortisol short acting glucocorticoids DOA <12 h hydrocortisone cortisone intermediate acting glucocorticoids DoA = 12-36h prednisone prednisolone methylprednisolone triamcinolone long acting glucocorticoids DOA: 1.5 - >2 days highest potency more anti-inflammatory action betamethasone dexamethasone hydrocortisone •Equally efficacious anti-inflammatory and salt-retaining properties •Used in wide array of applications, including dermatological (topical), ulcerative colitis, hemorrhoids, Addison's disease (chronic and acute presentations), general immune suppression •PO, IM, IV, SC cortisone •Prodrug of hydrocortisone •No topical activity, but equi-active at anti-inflammation and salt-retention •PO intermediate acting glucocorticoids are used for Used to treat skin conditions (psoriasis, eczema - topical), immune disorders (arthritis, ulcerative colitis, lupus - oral), asthma prevention (inhaled), keloids (injectable) predinsone prodrug of prednisolone, hepatic activation, only PO betamethasone is used for skin (eczema, psoriasis), fetal lung development (crosses placenta) dexamethasone use •Anti-inflammatory - RA, bronchospasm/asthma, idiopathic thrombocytopenia purpura, allergic rhinitis, anaphylaxis, bacterial meningitis where bacterial "clean-up" can be problematic; •Oncological - anti-emetic and decreases post-surgical inflammation (ie. brain tumor removal), also directly toxic to some "liquid" tumors; •Fetal lung development agents of choice for adrenal insufficiency •hydrocortisone or cortisone acetate BID (mimic morning cortisol) •prednisolone (once daily, or alternate-day is appropriate response.) •Might also need mineralocorticoid replacement glucocorticoids in non-adrenal disorders •Mostly used for their ability to suppress inflammatory & immune responses (where host response is the problem). •Assess Risk / benefit •Immune response might be important to control pathological problem •Might also cause irreparable damage •Only symptomatic. Not specific or curative Best medium- to intermediate-acting glucocorticoids. If possible, alternate day therapy non-adrenal disorders that use glucocorticoids allergic reactions hematologic disorders systemic inflammation inflammatory condition of bones and joints nausea and vomiting 12 / 16 PHCY 507: Endocrine Test 1 Study online at https://quizlet.com/_emdhu4 organ transplants skin diseases dexamethasone suppression test blood analysis for cortisol levels after administration of synthetic glucocorticoid, used to detect cushing's syndrome short period of corticosteroids (<2 weeks) AE •Insomnia, behavioral changes, acute peptic ulcers (acute pancreatitis with high doses, rare but serious) long term use of corticosteroids metabolic AE •100 mg/day for >2 weeks à iatrogenic Cushing's syndrome •rounding puffy face (moon face), fat deposition and redistribution, hair growth, acne, insomnia and increased appetite •Increased glucose production and diabetes •Weight gain, visceral fat added, myopathy, muscle wasting, thinning skin and osteoporosis, impaired wound healing long term use of corticosteroids AE kids --> growth arrest hypertension: sodium and fluid retention glucocorticoid withdrawal adrenal suppression flare up of underlying disease Steroidogenesis inhibitors drugs Metyrapone Ketoconazole Etomidate adenolytic drugs mitotane glucocorticoid receptor antagonist Mifepristone Neuromodulators of ACTH Release pasireotide and cabergoline metyrapone MOA Inhibits 11²-hydroxylase ’ blocks cortisol and aldosterone production (not androgens) metyrapone AE significant androgenic AE (hirsutism, acne, etc) ’ not ideal for women... but safest choice during pregnancy. •BP and electrolyte abnormalities. metyrapone DDI inducer of CYP3A4 ketoconazole •Antifungal agent •At higher doses, non-selective & potent inhibitor of adrenal and gonadal steroid synthesis. •MOA: inhibition of multiple enzymes (including 11²-hydroxylase and 17±hydroxylase) ketoconazole AE •Antiandrogenic activity (gynecomastia and hypogonadism in men). •Hepatotoxic (CI in hepatic disease), reversible elevation of hepatic transaminases in 10% pts •GI upset, dermatologic reactions. ketoconazole DDI strong inhibitor of CYP3A4 etomidate MOA inhibits 11²-hydroxylase, aldosterone synthase •For acute hypercortisolemia requiring emergency tx or in preparation for surgery (IV only) mitotane effect on adrenal cortex Cytotoxic effects to the adrenal cortex mitotane use •non-operable adrenal carcinoma •Cushing's only off-label (compassionate basis only) mitotane AE •GI upset, nausea, diarrhea (up to 80% pts) Lethargy, somnolence, CNS disturbances mifepristone MOA Binds GR with high affinity ’ stabilization of the hsp-GR complex; blocks cortisol binding via competition; and changes the interaction with co-regulators (no effect on steroid synthesis). mifepristone use Treatment Cushing's syndrome (hyperglycemia) in inoperable patients with ectopic ACTH secretion or adrenal carcinoma who didn't respond to other therapies 13 / 16 PHCY 507: Endocrine Test 1 Study online at https://quizlet.com/_emdhu4 mifepristone AE Hypokalemia, nausea, fatigue, headache, peripheral edema, dizziness, endometrial hyperplasia mifepristone CI pregnancy and severe hepatic impairment Pasireotide (Signifor) •Somatostatin analog: agonizes somatostatin receptors ’ inhibit ACTH secretion ’ “cortisol secretion. cabergoline •D2-receptor agonist •Sustained response in only 30-40% pts aldosterone effect in body Na+ and fluid retention in kidney ’ ‘ blood volume ’ ‘ BP fludrocortisone •Aldosterone receptor agonist •CA: adrenal insufficiency associated with mineralocorticoid deficiency to modulate salt retention •250-fold more salt-retention than cortisol Mineralocorticoid Antagonists Spironolactone Eplerenone Steroids that compete with aldosterone for its receptor Mineralocorticoid Antagonists clinical applications •Aldosteronism •Excessive aldosterone production, usually by adrenal adenoma or another tumor. •Diuresis (HTN, HF) The two classes of steroids are corticosteroids and sex hormones topical corticosteroids med chem •Usually highly potent agents •Display many halogens to enhance potency and/or block metabolism 1st line for management of cushings surgical resection of ACTH of cortisol producing tumors 2nd line for management of cushings oPituitary irradiation oMedical therapy oRepeat transphenoidal surgery or bilateral adrenalectomy ketoconazole response seen after several weks ketoconazole benefits cholesterol and blood pressure levoketoconazole new agent recently approved in January 2022 for Cushing's syndrome; has led to sustained improvements of urinary free cortisol in 31% of 94 patients after 6 months of treatment; ADE: QT prolongation and ALT increase (SONICS Trial: http://bit.ly/2lbLBFJ) metyrapone response •Response seen within hours (short t ½ à requires multiple doses/day) osilodrostat •Oral cortisol synthesis inhibitor (inhibits 11²-hydroxylase ~ metyrapone) •Dose 2-7 mg twice daily •Has longer t½ and is more potent against 11²-hydroxylase > metyrapone (twice daily dosing vs QID for metyrapone) •ADE: GI, fatigue, headache, edema, adrenal insufficiency etomidate •Only comes as an injection •Monitor serum cortisol mifepristone FDA approval FDA approved for patients who have T2DM or glucose intolerance and who are not eligible for or who have had poor response to surgery mifepristone has ___________ due to anti-progestin activity and risk of early termination abortive effects mitodane response time •Takes weeks to months (~6 months) for beneficial effects to be seen pasireotide FDA approval Only approved for adults with Cushing whom pituitary surgery is not an option pasireotide AE diarrhea, nausea, QTc prolongation 14 / 16 PHCY 507: Endocrine Test 1 Study online at https://quizlet.com/_emdhu4 vaccinations for Cushing's syndrome Flu, Shingrix, Prevnar cortisol-dependent comorbidities psychiatric disorders, DM, HTN, hypokalemia, infections, DLD, osteoporosis, poor physical fitness goals of therapy for primary hyperaldosteronism normalize aldosterone levels normalize serum potassium and reduce BP 1st line treatment of primary hyperaldosteronism unilateral adrenalectomy 2nd line treatment of primary hyperaldosteronism medical therapy: MR antagonists spironolactone CI •Addison's disease (hyperkalemia), hyperkalemia (>5.5 mEq/L), anuria, CrCl <30 mL/min, co-administration with other potassium-sparing diuretics or potassium supplements (eplerenone, amiloride) Preferred drug during pregnancy, preferred for children due to little anti-androgen effects for hyperaldosteronism eplerenone Monitoring for Primary Hyperaldosteronism education titrate medical therapy every 4-8 weeks goals of therapy for Addison's •Limit morbidity and mortality and return the patient to a normal functional state •Ensure patients are aware of treatment complications, expected outcomes and consequences of missed doses •Educate patient on long-term steroid therapy and emergency procedures for adrenal crisis pharmacotherapy for Addison's glucocorticoids and mineralocorticoids glucocorticoids replaces cortisol hydrocortisone and cortisone dose adjustment by weight or BSA glucocorticoid better for nonadherence but not for pregnant patients prednisolone glucocorticoids CI live vaccines, serious systemic infections (fungal infections) glucocorticoids ADE •HPA suppression •Psychiatric disturbances Worsen other conditions pharmacotherapy monitoring for glucocorticoids •Measurement of plasma ACTH is not recommended •Monitor replacement and adjust treatment based on clinical assessment of s/s •signs of glucocortiocid insufficiency and excess signs of glucocorticoid insufficiency nausea, poor appetite, weight loss, lethargy, hyperpigmentation (Addison's) signs of glucocorticoid excess weight gain, insomnia, peripheral edema fludrocortisone ADE edema hypokalemia mineralcorticoid pharmacotherapy monitoring •Monitor based off clinical assessment of s/s •Avoid licorice and grapefruit juice à potentiate effects •Monitor for HTN steroids taper is necessary when taking steroid for >14 days ACTH test for monitoring steroid discontinuation •Ideally, would want to check HPA integrity using ACTH test or a serum cortisol (@ 8:00 AM) •A normal morning serum cortisol (>20µg/dL) or normal ACTH test indicates therapy may be discontinued If cortisol is <3µg/dL, axis is suppressed and continued replacement is required; suppression can persist for up to a year in some patients addisonian crisis •Acute adrenal insufficiency mainly from HPA axis suppression = endocrine emergency (fatal!) •Occurs with abrupt withdrawal of chronic glucocorticoid use or 15 / 16 PHCY 507: Endocrine Test 1 Study online at https://quizlet.com/_emdhu4 lack dose adjustments during stressful situations (surgery, infection, trauma) signs and symptoms of addisonian crisis •weakness, myalgias, malaise, vomiting, fever, hypotension and shock treatment of addisonian crisis •immediate parenteral injection of 100 mg hydrocortisone + fluid resuscitation, then 200 mg Q24 hrs (continuous infusion or split). After the initial 24 hrs, may taper dose gradually and resume normal oral dosing once patient is stable. addisonian crisis prevention •add 5-10 mg hydrocortisone to normal daily regimen before strenuous activities or double dose during times of severe physical stress (illness) management of addisons •Educate about stress dosing for intercurrent illnesses and/or provide injectable emergency steroids •Offer a medical alert tag indicating adrenal insufficiency/ glucocorticoid replacement are essential •Annual visits to an endocrinologist 16 / 16