General Data
Name: P. L
DOB: 12/9/1963
Race: Fijian of Indian Descent
Religion: Hindu
Sex: Female
Address: Wairabetia, Lautoka
NHN: 320028681
DOA: 11/4/22 (Lautoka Hospital)
DOD: 17/04/22
Informant: Patient’s Daughter
Chief complaint:
Admitting 59 years old Fijian of Indian Descent female with known case of Diabetes Mellitus
II and Hypertension presented to Emergency Department with chief complains of:
Fever
Right upper abdominal and epigastric pain
Generalized body weakness
x 3/7
Vomiting
History of Presenting Illness
According to the patient’s daughter, she was well until 3 days ago prior to admission, the
patient ate a lot of bananas after which she started having generalized abdominal pain that
was radiating to the chest and she describes it as like “gastric pain”. Along with abdominal
pain, the patient also had 3 episodes of vomiting which was bilious and yellowish in color
and one episode of loose bowel motion with no associated blood. Three days prior to
consult, on 8th April, 2022, at around 7pm, she presented to the Emergency Department for
her above symptoms whereby her bloods, scan and chest x-ray was done and she was given
2 doses of morphine and amlodipine. Her blood pressure upon presentation to ED was
200/116. The patient was then reviewed by the surgical team and she was being ruled out
for gastritis. The following day upon presentation to ED, on 9th April, 2022, at around 8am,
she was discharged on Tramadol and Omeprazole. After she was discharged for home, the
daughter explains that the patient was only feeling sleepy and kept complaining about the
abdominal pain, however, she was able to get off the bed and use the washroom without
any assistance or support. On Sunday, 10th April, 2022, she still had abdominal pain and
other symptoms, however, on Monday, 11th April, 2022, she started feeling weak and could
not get off the bed and started having urinary incontinence together with chills and rigors,
at around 5pm. Her vitals at home were T – 389 HR- 97
to the Emergency Department.
BP – 140/97, hence, presented
Review of Systems:
(+) weakness (+) fatigue (+) fever (-) anorexia
(-) chest pain (-) SOB (-) orthopnea (-) PND (-) cough (-) hemoptysis (-) swelling of
ankles (-) palpitations (-) cyanosis
(+) nausea (+) vomiting x2 episodes (-) heart burn (-) difficulty in swallowing
(+) abdominal pain (-) abdominal distension (-) hematemesis (-) melena
(-) Jaundice (+) loose bowel motion x1 episode
(-) frequency (-) urgency (-) dysuria (-) hesitancy (-) polyuria (-) back pain (-)
incontinence
(-) discharge (-) unusual bleeding
(-) headache (-) blurred vision (-) black outs or loss of consciousness (-) muscle weakness
(-) tremors (-) abnormal sensations
(-) muscle, bone or joint pain (-) deformities (-) abnormal gait
Past medical History
•
•
•
•
The patient was diagnosed with type 2 Diabetes Mellitus 15 years ago and was on
medications: Metformin 1g PO BD and Glipizide 15mg PO BD
She was compliant to her medications; however, she was not compliant to her
diabetic diet.
She was diagnosed with Hypertension before she was diagnosed with Diabetes and
was prescribed medications: Enalapril 10mg PO BD, Aspirin 100mg PO OD and
Simvastatin 20mg PO Nocte
She also has a history of partial hysterectomy for uterine prolapse that was done in
2010 and appendectomy that was done when she was in class 5
Drug History:
She is on:
•
•
•
•
•
Metformin 1g PO BD
Glipizide 15mg PO BD
Enalapril 1omg PO BD
Aspirin 100mg PO OD
Simvastatin 2omg Po Nocte
Nil allergies known
Family History
•
•
According to the daughter, the patient’s father had uncontrolled Diabetes Mellitus
and Hypertension and had died due to Stroke
She has 4 siblings: three brothers and one sister out of which one brother and sister
has Diabetes Mellitus.
Social History
•
•
The patient lives with her daughter, son, daughter in law and 2 grandchildren
She does not smoke or drinks grog or alcohol
Patient’s Physical Examination findings upon admission, after being stabilized in the
Emergency department
On examination:
The patient was lying supine on bed in recumbent position, hooked to cardiac monitor, on
4L oxygen via Hudson mask, oriented to time, place and person
Vitals:
T- 373
BP- 131/65
Physical Examination
HEENT:
(-) Conjunctival Pallor
(-) Icteric Sclera
(-) Xanthelasma
(-) Central Cyanosis
P- 106
RR- 19
SPO2- 100%
CBG- 20.6
(+) Dry oral mucosa
(-) JVP elevation
Chest:
(-) scars
(+) Apex beat at 5th Intercostal Space Midclavicular
Line
(-) heaves (-) thrills
(+) Tachycardiac (Regular)
(+) clear lung fields
(-) murmurs appreciated
Abdomen:
right upper quadrant – Mild tenderness upon deep palpation
(+) surgical scar
(-) striae
Left upper quadrant – Severe tenderness upon deep palpation
(-) rebound
(-) guarding
(-) renal angle tenderness
Extremities:
(-) scars
(-) edema
(+) Warm
(+) Bounding pulses (Tachycardiac)
CR < 2secs
Patient’s vitals upon Presenting to Emergency Department:
P – 150
BP – 135/68
T – 394 R/R – 32 SPO2: 96% CBG: 30.4
The patient was assessed at 6.50pm as:
Clinical Sepsis
o R/O Cholecystitis and Gallbladder Stones
o R/O Diabetic Ketoacidosis vs Hyperosmolar Hyperglycemia State
Emergency Department Plans:
•
•
•
•
•
•
•
•
•
•
•
•
Resuscitate on bed
2 IV cannula
Bloods: FBC/ UECr/ LFTs/ Amylase/ VBG
Follow up blood culture – sent on 8th April, 2022
IV Fluid 1L bolus
Medications:
o Ampicillin 2g IV stat
o Gentamicin 320mg IV stat
o Paracetamol 1g PO stat
o Soluble insulin 1o units subcutaneous stat
Insert IDC
Send MSU
Ultrasound Abdo/Pelvis
Chase old folder from 8th April, 2022
ECG and Chest X-ray
Patient and the daughter explained and updated
At 8pm, the patient was reassessed by the Emergency Department MO:
After evaluating the results and the status of the patient, the patient was assessed as
Diabetic Ketoacidosis:
Plans were:
IVF 1L Normal saline bolus
1L Normal saline Q1H
1L Normal saline Q2H
1L Normal saline Q4H
Commence on insulin infusion
Chase UECr
For Medical Admission
Investigation Results:
WBC: 13110 (high)
Na: 129 (low)
Hb: 11 (low threshold)
K: 4.4 (normal)
MCV: 75.3 (low threshold)
Cl: 95 (normal)
Platelet: 239000 (normal)
Amylase: 36 (normal)
Urea: 10.1 (high)
Urine Ketones: +3
ABG: Compensated Respiratory Alkalosis
pH: 7.446 (normal)
(7.35-7.45)
pCO2: 30.9 (low)
(35-45)
pO2: 57.0 (low)
(80-100)
cHCO3 21.3 (Normal)
(20.0-30.0)
ECG Findings:
•
•
•
•
•
Rate: 126 bpm
Normal Sinus Rhythm and Regular
Normal Axis Deviation
Sinus Tachycardia
Non specific ST changes in leads V2 and V3
Assessment after Stabilizing the patient in ED:
•
•
•
•
•
•
•
Diabetic Ketoacidosis
Clinical sepsis?? Foci
o R/o intraabdominal
o R/O Liver Abscess
o ?? UTI
o ?? Pneumonia
Mild Microcytic Anemia
Diabetes Mellitus
Hypertension
History of Partial Hysterectomy (uterine prolapse)
Renal impairment
Admission Plans:
•
•
•
•
•
•
•
•
•
•
•
•
•
Admit to Women’s Medical Ward
Insert IDC and monitor urine input/output and record please
FBC/ VBG/ UECr/ Minerals noted
Follow up Blood Culture done on 8th April, 2022 from ED
Medications:
o Cloxacillin 2g IV Q6H
o Chloramphenicol 1g IV Q6H
o Paracetamol 1g PO Q6H prn
o Insulin infusion as per DKA protocol
o Aspirin 100mh PO OD
o Enalapril 10mg PO BD
IV Fluids normal saline at 166mls/ hour in 20mmols KCL in each bag
For Abdo/ Pelvis/ Renal scan
Send Sputum Gram stain/ AFB/ MSU
For chest x-ray
UECr tomorrow morning \
Monitor vital signs and respiratory status: If patient is desaturating, put the patient
on O2
Dietician to see: Commence DM diet
Patient and daughter updated
Ward Reviews:
This patient was Dr Narayan’s case and was handled by him and the Team.
The patient was Soaped and reviewed every day by Dr Narayan’s Team
Results of the tests rendered by Dr Narayans’s Team:
Abdomen/ Pelvis Ultrasound:
•
•
•
•
•
•
•
•
•
Left Renal meas was 15.9 x 7.8cm
Multiple cystic structures seen within. Largest in upper pole measuring 4.5cm in AP
diameter
Right Renal meas 20.4 x 9.2cm. multiple cystic structures seen within
Largest in lower pole meas 8cm in AP diameter
Gallbladder meas 11.7cm in length – irregular echogenic content seen on posterior
wall, meas 1-2cm in thickness. Gallbladder sludge – GB wall thickness = 7mm
CBD meas 8mm AP diameter
Pericystic collection seen
Gaseous bowel contents ++
No ascites
Chest Ultrasound:
Ultrasound of the right chest showed anechoic fluid meas 11.8 x 8.7 x 4.9cm – 52mls.
No loculations.
Left chest had minimal pleural effusion
Chest X- ray: In AP supine
Subsegmental Atelectasis seen in both lower zones
Upper lung fields were clear
Heart size was not enlarged.
The patient was then assessed as:
Likely Cholelithiasis
Resolving cholecystitis
Right lower zone pneumonia
Plans was to:
Continue medical management
Refer accordingly
To consider cholecystectomy and discuss the diagnosis and plans with the patient
The patient was reviewed on 17th April, 2022, Day 6 of Admission
Vitals were stable and CBG was 11.2
Patient was assessed as stable and discharged on:
•
•
•
•
•
•
•
•
Chloramphenicol 500mg PO Q6H x 2/7
Aspirin 100mg PO OD
Enalapril 10mg PO BD
Metoprolol 25mg PO OD
Omeprazole 20mg PO BD
Metformin 500mg PO TDS
Mebendazole 100mg PO BD x 3/7
FeSO4 200mg PO TDS
Patient was booked for SOPD clinic on 21st April, 2022 with FBC/ UECr/ RBS on arrival
Inform surgical team to review upon discharge
Daughter at bedside was updated
The patient was reviewed by Surgical Team upon discharge:
Plans were:
•
•
If the patient does not want surgical intervention, then no need to review for now
Can present to the health center and if symptoms appear again, she can be referred
for surgery.
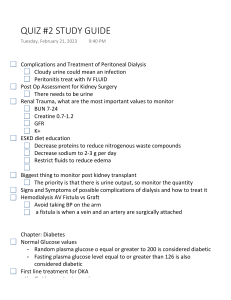
Learning Objective:
In this case, I was able to learn about:
•
•
•
•
Diabetic Ketoacidosis: Its causes, pathophysiology, investigations and its appropriate
treatment.
Difference between DKA and HHS
Why patient developed respiratory Alkalosis
DKA protocol according to Fiji Guidelines
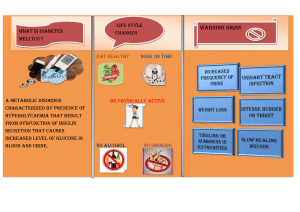
Diabetic Ketoacidosis
•
•
•
Diabetic ketoacidosis (DKA) is an acute, major, life-threatening complication of
diabetes. DKA mainly occurs in patients with type 1 diabetes, but it is not uncommon
in some patients with type 2 diabetes
DKA is a state of absolute or relative insulin deficiency aggravated by ensuing
hyperglycemia, dehydration, and acidosis-producing derangements in intermediary
metabolism. The most common causes are underlying infection, disruption of insulin
treatment, and new onset of diabetes.
DKA is defined clinically as an acute state of severe uncontrolled diabetes associated
with ketoacidosis that requires emergency treatment with insulin and intravenous
fluids
Epidemiology
• Despite advancements in self-care of patients with diabetes, DKA accounts for 14%
of all hospital admissions of patients with diabetes and 16% of all diabetes-related
fatalities.
•
Almost 50% of diabetes-related admissions in young persons are related to DKA.
•
DKA frequently is observed during the diagnosis of type 1 diabetes and often
indicates this diagnosis.
DKA occurs primarily in patients with type 1 diabetes. The incidence is roughly 2
episodes per 100 patient years of diabetes, with about 3% of patients with type 1
diabetes initially presenting with DKA. It can occur in patients with type 2 diabetes as
well; this is less common
•
•
The incidence of DKA is higher in whites because of the higher incidence of type 1
diabetes in this racial group. The incidence of DKA is slightly greater in females than
in males for reasons that are unclear. Recurrent DKA frequently is seen in young
women with type 1 diabetes and is caused mostly by the omission of insulin
treatment.
•
Among persons with type 1 diabetes, DKA is much more common in young children
and adolescents than it is in adults. DKA tends to occur in individuals younger than
19 years, but it may occur in patients with diabetes at any age.
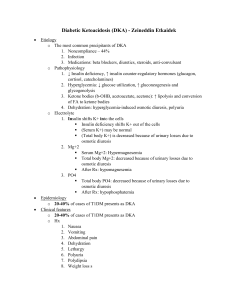
Etiology
The most common scenarios for diabetic ketoacidosis (DKA) are underlying or concomitant
infection (40%), missed or disrupted insulin treatments (25%), and newly diagnosed,
previously unknown diabetes (15%).
Other associated causes make up roughly 20% in the various scenarios.
Causes of DKA in type 1 diabetes mellitus include the following:
• In 25% of patients, DKA is present at diagnosis of type 1 diabetes due to acute insulin
deficiency (occurs in 25% of patients)
o Poor compliance with insulin through the omission of insulin injections, due
to lack of patient/guardian education or as a result of psychological stress,
particularly in adolescents
• Missed, omitted or forgotten insulin doses due to illness, vomiting or excess alcohol
intake
• Bacterial infection and intercurrent illness (eg, urinary tract
• infection [UTI])
• Klebsiella pneumoniae (the leading cause of bacterial infections precipitating DKA)
• Medical, surgical, or emotional stress
• Brittle diabetes
• Idiopathic (no identifiable cause)
• Insulin infusion catheter blockage
• Mechanical failure of the insulin infusion pump
Causes of DKA in type 2 diabetes mellitus include the following:
• Intercurrent illness (eg, myocardial infarction, pneumonia, prostatitis, UTI)
• Medication (eg, corticosteroids, pentamidine, clozapine)
Pathophysiology
• Diabetic ketoacidosis (DKA) is a complex disordered metabolic state characterized by
hyperglycemia, ketoacidosis, and ketonuria. DKA usually occurs as a consequence of
absolute or relative insulin deficiency that is accompanied by an increase in counterregulatory hormones (ie, glucagon, cortisol, growth hormone, epinephrine).
•
This type of hormonal imbalance enhances hepatic gluconeogenesis, glycogenolysis,
and lipolysis. Hepatic gluconeogenesis, glycogenolysis secondary to insulin
deficiency, and counter-regulatory hormone excess result in severe hyperglycemia,
while lipolysis increases serum free fatty acids.
•
Hepatic metabolism of free fatty acids as an alternative energy source (ie,
ketogenesis) results in accumulation of acidic intermediate and end metabolites (ie,
ketones, ketoacids).
•
Ketone bodies have generally included acetone, beta-hydroxybutyrate, and
acetoacetate. It should be noted, however, that only acetone is a true ketone, while
acetoacetic acid is true ketoacid and beta-hydroxybutyrate is a hydroxy acid.
•
Meanwhile, increased proteolysis and decreased protein synthesis as result of insulin
deficiency add more gluconeogenic substrates to the gluconeogenesis process. In
addition, the decreased glucose uptake by peripheral tissues due to insulin
deficiency and increased counter regulatory hormones increases hyperglycemia.
•
Ketone bodies are produced from acetyl coenzyme A mainly in the mitochondria
within hepatocytes when carbohydrate utilization is impaired because of relative or
absolute insulin deficiency, such that energy must be obtained from fatty acid
metabolism. High levels of acetyl coenzyme A present in the cell inhibit the pyruvate
dehydrogenase complex, but pyruvate carboxylase is activated. Thus, the
oxaloacetate generated enters gluconeogenesis rather than the citric acid cycle, as
the latter is also inhibited by the elevated level of nicotinamide adenine dinucleotide
(NADH) resulting from excessive beta-oxidation of fatty acids, another consequence
of insulin resistance/insulin deficiency. The excess acetyl coenzyme A is therefore
rerouted to ketogenesis.
•
Progressive rise of blood concentration of these acidic organic substances initially
leads to a state of ketonemia, although extracellular and intracellular body buffers
can limit ketonemia in its early stages, as reflected by a normal arterial pH associated
with a base deficit and a mild anion gap.
•
When the accumulated ketones exceed the body's capacity to extract them, they
overflow into urine (ie, ketonuria). If the situation is not treated promptly, a greater
accumulation of organic acids leads to frank clinical metabolic acidosis (ie,
ketoacidosis), with a significant drop in pH and bicarbonate [4] serum levels.
Respiratory compensation for this acidotic condition results in Kussmaul respirations,
ie, rapid, shallow breathing (sigh breathing) that, as the acidosis grows more severe,
becomes slower, deeper, and labored (air hunger).
•
Ketones/ketoacids/hydroxy acids, in particular, beta-hydroxybutyrate, induce nausea
and vomiting that consequently aggravate fluid and electrolyte loss already existing
in DKA. Moreover, acetone produces the fruity breath odor that is characteristic of
ketotic patients.
•
Glucosuria leads to osmotic diuresis, dehydration and hyperosmolarity.
•
Severe dehydration, if not properly compensated, may lead to impaired renal
function.
•
Hyperglycemia, osmotic diuresis, serum hyperosmolarity, and metabolic acidosis
result in severe electrolyte disturbances. The most characteristic disturbance is total
body potassium loss. This loss is not mirrored in serum potassium levels, which may
be low, within the reference range, or even high.
•
Potassium loss is caused by a shift of potassium from the intracellular to the
extracellular space in an exchange with hydrogen ions that accumulate
extracellularly in acidosis. Much of the shifted extracellular potassium is lost in urine
because of osmotic diuresis.
Patients with initial hypokalemia are considered to have severe and serious total
body potassium depletion. High serum osmolarity also drives water from
intracellular to extracellular space, causing dilutional hyponatremia. Sodium also is
lost in the urine during the osmotic diuresis.
The combined effects of serum hyperosmolarity, dehydration, and acidosis result in
increased osmolarity in brain cells that clinically manifests as an alteration in the
level of consciousness.
•
•
•
Many of the underlying pathophysiologic disturbances in DKA are directly
measurable by the clinician and need to be monitored throughout the course of
treatment. Close attention to clinical laboratory data allows for tracking of the
underlying acidosis and hyperglycemia, as well as prevention of common potentially
lethal complications such as hypoglycemia, hyponatremia, and hypokalemia.
Clinical Presentation
History
Insidious increased thirst (ie, polydipsia) and urination (ie, polyuria) are the most common
early symptoms of diabetic ketoacidosis (DKA).
Malaise, generalized weakness, and fatigability also can present as symptoms of DKA.
Nausea and vomiting usually occur and may be associated with diffuse abdominal pain,
decreased appetite, and anorexia. A history of rapid weight loss is a symptom in patients
who are newly diagnosed with type 1 diabetes.
Patients may present with a history of failure to comply with insulin therapy or missed
insulin injections due to vomiting or psychological reasons. Decreased perspiration is
another possible symptom of DKA.
Altered consciousness in the form of mild disorientation or confusion can occur. Although
frank coma is uncommon, it may occur when the condition is neglected or if dehydration or
acidosis is severe.
Among the symptoms of DKA associated with possible intercurrent infection are fever,
dysuria, coughing, malaise, chills, chest pain, shortness of breath, and arthralgia. Acute
chest pain or palpitation may occur in association with myocardial infarction. Painless
infarction is not uncommon in patients with diabetes and should always be suspected in
elderly patients.
Physical Examination
General signs of diabetic ketoacidosis (DKA) may include the following:
• Ill appearance
• Dry skin
• Labored respiration
• Dry mucous membranes
• Decreased skin turgor
• Decreased reflexes
• Characteristic acetone (ketotic) breath odor
Effects on vital signs that are related to DKA may include the following:
• Tachycardia
• Hypotension
• Tachypnea
• Hypothermia
• Fever, if infection is present
Specific signs of DKA may include the following:
• Confusion
• Coma
• Abdominal tenderness
The physical examination should also include detection of the signs of possible intercurrent
illnesses such as myocardial infarction, urinary tract infection, pneumonia, and perinephric
abscess. Search for signs of infection is mandatory in all cases.
Signs and Symptoms of Hyperglycemia, Acidosis, and Dehydration
Symptoms of hyperglycemia associated with diabetic ketoacidosis may include thirst,
polyuria, polydipsia, and nocturia.
Signs of acidosis may include rapid, shallow breathing (sigh breathing) that, as the acidosis
grows more severe, becomes slower, deeper, and labored (air hunger), as well as abdominal
tenderness and disturbance of consciousness. Although these signs are not usual in all cases
of diabetic ketoacidosis (DKA), their presence signifies a severe form of DKA. The breath has
a fruity smell.
Signs of dehydration include a weak and rapid pulse, dry tongue and skin, hypotension, and
increased capillary refill time.
Emphasizing that no direct correlation exists between the degree of acidosis,
hyperglycemia, and the disturbances in the level of consciousness is important.
Complications Associated with DKA
Includes sepsis and diffuse ischemic processes. Other associated complications include the
following:
• CVT
• Myocardial infarction
• DVT
• Acute gastric dilatation
• Erosive gastritis
• Late hypoglycemia
• Respiratory distress
• Infection (most commonly, urinary tract infections)
• Hypophosphatemia
• Mucormycosis
• Cerebrovascular accident
Diagnosis
The diagnosis of DKA is defined by the presence of
• Diabetes: Hyperglycaemia (blood glucose > 11 mmol/L)
• Ketosis: Ketonuria* and/or ketonaemia
• Acidosis: Metabolic acidosis (pH < 7.3, Bicarbonate < 15 mmol/L)
Ketonuria – measurement of urine ketones confirms ketosis but should not be used to judge
the severity of ketonaemia.
The severity of DKA is categorized by the degree of acidosis (ISPAD definition):
• Mild: pH 7.2 - 7.3 and/or bicarbonate 10 - 15 mmol/L
• Moderate: pH 7.1 - 7.2 and/or bicarbonate 5 - 10 mmol/L
• Severe: pH < 7.1 and/or bicarbonate < 5 mmol/L
Urine Ketone Levels
Trace
+1
+2
+3
+4
Serum Ketone Levels
0.05 g/dl
0.15 g/dl
0.4 g/dl
0.8 g/dl
1.6 g/dl
Laboratory studies for diabetic ketoacidosis (DKA) should be scheduled as follows:
• Blood tests for glucose every 1-2 h until patient is stable, then every 4-6 h
• Serum electrolyte determinations every 1-2 h until patient is stable, then every 4-6 h
• Initial blood urea nitrogen (BUN)
• Initial arterial blood gas (ABG) measurements, followed with bicarbonate as
necessary
Repeat laboratory tests are critical, including potassium, glucose, electrolytes, and, if
necessary, phosphorus. Initial workup should include aggressive volume, glucose, and
electrolyte management.
It is important to be aware that high serum glucose levels may lead to dilutional
hyponatremia; high triglyceride levels may lead to factitious low glucose levels; and high
levels of ketone bodies may lead to factitious elevation of creatinine levels.
Plasma Glucose Study
• The blood sugar level for patients with DKA usually exceeds 250 mg/dL. The clinician
can perform a fingerstick blood glucose test while waiting for the plasma glucose
level.
Urine Dipstick Testing
• For patients with DKA, the urine dipstick test is highly positive for glucose and
ketones.
Ketones
• In patients with DKA, serum ketones are present.
• Diagnosis of ketonuria requires adequate renal function.
Arterial Blood Gases
• In patients with DKA frequently show typical manifestations of metabolic acidosis,
low bicarbonate, and low pH (less than 7.3).
• When monitoring the response to treatment, the 2011 JBDS guideline recommends
the use of venous blood rather than arterial blood in blood gas analyzers, except
where respiratory problems preclude using arterial blood.
Serum Electrolyte Panel
• Serum potassium levels initially are high or within the reference range in patients
with DKA. This is due to the extracellular shift of potassium in exchange of hydrogen,
which is accumulated in acidosis, in spite of severely depleted total body potassium.
This needs to be checked frequently, as values drop very rapidly with treatment. An
ECG may be used to assess the cardiac effects of extremes in potassium levels.
• The serum sodium level usually is low in affected patients. The osmotic effect of
hyperglycemia moves extravascular water to the intravascular space.
Bicarbonate
• Use bicarbonate levels in conjunction with the anion gap to assess the degree of
acidosis that is present.
Anion Gap
• In patients with diabetic ketoacidosis, the anion gap is elevated ([Na + K] - [Cl +
HCO3] greater than 10 mEq/L in mild cases and greater than 12 mEq/L in moderate
and severe cases).
CBC
•
Even in the absence of infection, the CBC shows an increased white blood cell (WBC)
count in patients with diabetic ketoacidosis. High WBC counts (greater than 15 X
109/L) or marked left shift may suggest underlying infection.
Renal Function Studies
• BUN frequently is increased in patients with diabetic ketoacidosis.
Osmolarity
• Plasma osmolarity usually is increased (greater than 290 mOsm/L) in patients with
diabetic ketoacidosis. Urine osmolarity also is increased in affected patients.
• Patients with diabetic ketoacidosis who are in a coma typically have osmolalities
greater than 330 mOsm/kg H2 O. If the osmolality is less than this in a patient who is
comatose, search for another cause of obtundation.
Cultures
• Urine and blood culture findings help to identify any possible infecting organisms in
patients with diabetic ketoacidosis.
Amylase
• Hyperamylasemia may be seen in patients with diabetic ketoacidosis, even in the
absence of pancreatitis.
Phosphate, Calcium, and Magnesium
• If the patient is at risk for hypophosphatemia (eg, poor nutritional status, chronic
alcoholism), then the serum phosphorous level should be determined.
Chest X-ray
• Chest radiography should be used to rule out pulmonary infection such as
pneumonia.
Electrocardiography
• DKA may be precipitated by a cardiac event, and the physiological disturbances of
DKA may cause cardiac complications. An ECG should be performed every 6 hours
during the first day, unless the patient is monitored. An ECG may reveal signs of
acute myocardial infarction that could be painless in patients with diabetes,
particularly in those with autonomic neuropathy.
• An ECG is also a rapid way to assess significant hypokalemia or hyperkalemia. T-wave
changes may produce the first warning sign of disturbed serum potassium levels.
Low T wave and apparent U wave always signify hypokalemia, while peaked T wave
is observed in hyperkalemia.
Treatment and Management According to Fiji Guidelines
Initial Evaluation: Assess
•
•
•
•
Airway, Breathing and Circulation (ABC ) status
Mental status
Possible precipitating events (e.g. Infection, myocardial infarction, stroke, trauma or
drug non- compliance)
Volume status
Baseline investigations:
•
•
•
•
•
•
Serum glucose
Urea, electrolytes and creatinine
Arterial blood gas and calculation of anionic gap: ( Na + K) – (CI + HCO3)
Full blood count with differential
Urine dipstick ketones (*measurement of serum ketones is not available)
Electrocardiogram
*Additional testing (cultures of urine, sputum and blood, serum amylase, and chest x-ray)
should be performed on a case-by case basis*
Management:
IV fluids
•
•
If patient is in shock, give sodium chloride 0.9% boluses till MAP improves to
>65mmHg
If not in shock and in patients without heart or renal failure:
o Normal saline 0.9% infusion at 15 to 20 ml/kg body weight per hour during
the first 2 hours
If the corrected Na* is low or normal infuse NS at 4 to 14 ml/kg /hour.
If the corrected Na* is elevated then give half isotonic saline (or D5W or DS in
our setting) at 4 to 14 mls/kg/hour
*Corrected Na = measured Na + (change in serum glucose - 2.3)
Common fluid regimen:
•
•
•
•
1st litre over 30mins
2nd litre over 1hr
3rd litre over 2hrs
4th litre over 4hrs
Further infusion rate depends on urine output and clinical assessment
Once CBG reaches 14 mmol/L, change IV fluid to D5% (D10% preferred); use D-Saline if
D5%/D10% not available
If initial CBG is between 11.1 and 14mmol/L please continue fluid resuscitation with 0.9%
saline while running a concurrent D10%side drip and insulin infusion.
*Discuss with medical registrar or consultant if any uncertainties.
Insulin
Give Soluble Insulin IV bolus of 0.1unit/kg then start insulin infusion at 0.1unit/kg/hour
•
•
If IV access is not available, give short acting insulin(soluble insulin) IMI at
8units/kg/hour
If the serum glucose does not fall by 3-4 mmol/L from the initial value in first hour,
repeat I.V. bolus dose and double insulin infusion rate until a steady glucose decline
is achieved.
*Please refer to the insulin infusion chart below*
Bicarbonate
•
•
Generally, NOT recommended but can be given if pH is less than 6.9 despite fluid and
insulin therapy
Dose: 1mmol/kg of NaHCO3 diluted with 0.9% normal saline over 1hr via infusion
Switching to subcutaneous insulin
•
•
•
•
•
serum glucose < 11.1 mmol/
anionic gap < 12
serum bicarbonate > 18
venous pH >7.3
patient is mentally alert and able to tolerate oral feeds
NOTE: there should be a 2 hour overlap of I.V and subcutaneous insulin therapy
Insulin Infusion Guidelines
Preparation
Add 100 units of soluble insulin (1 ml) in 100 ml of normal saline in a chamber to give a
concentration of 1 unit / ml. Insulin infusion should be run via a dedicated line and it should
not be co-infused with any other I.V fluids.
Monitoring
•
•
Test capillary blood glucose {CBG} every one hour until three consecutive readings
are within the target range (CBG: 6 – 10mmol/L), and then test CBG every 2 hourly,
while patient on infusion. Once CBG is between 11-17mmol/L, call medical registrar
to change fluid therapy in DKA and HHS if this is not ordered in the fluid balance
chart.
Record each CBG reading and infusion rate accurately in a specified chart
Stability:
Re-constituted insulin infusion solution should be used within 24 hours of preparation. On
replacement, the fresh insulin infusion can be more potent and result in an unexpected fall
in blood glucose for the same infusion rate.
Hypoglycemia (BSL< 3.5 mmol/L) Treatment
•
•
•
•
•
If asymptomatic, repeat blood sugar level
Cease Insulin Infusion
Give 25-50 mls of 50% glucose I.V
Call Medical Intern
Recheck BSL in 15 minutes
o If BSL < 5 repeat 25-50 mls of 50 % glucose
o If BSL > 7.9 recommence insulin after discussing with medical registrar
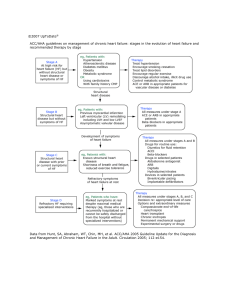
Hyperosmolar, Hyperglycemic State
This is a relatively uncommon event usually occurring as a dramatic presenting feature or as
a complication of type2 diabetes. It presents with a history of thirst, polyuria and
progressive impairment of consciousness commonly in a patient who is 60 years or older. It
differs from DKA in those patients with hyperosmolar, hyperglycaemic state do not develop
ketoacidosis. Investigations reveal very high blood glucose, usually higher than 30mmol/L,
the serum sodium is often elevated and the calculated serum osmolality >320mOsm/l
Management
The treatment is similar to that in DKA Intravenous isotonic saline, low dose intravenous
insulin (46u/hour by infusion) and careful attention to serum potassium concentrations are
the central strategies.
Careful monitoring is required as in DKA. On recovery, the patient may not need long term
insulin therapy. After an initial period of stabilization with insulin, most patients with type2
diabetes who present in a hyperosmolar, hyperglycaemic state can be controlled with oral
hypoglycaemic drugs combined with diet.
Distinguished from DKA by:
• Marked Hyperglycemia (Blood Glucose > 33.3 mmol/L)
• Minimal Acidosis (Venous pH > 7.25, or Arterial pH > 7.30 and serum HCO3 > 15)
• Absent to Mild Ketosis
• Marked elevation in serum osmolality (> 320 mOsm/L)
*More common in Diabetes Mellitus Type 2
Why patient develops respiratory Alkalosis in DKA in this case?
Detection of primary respiratory alkalosis in a patient with DKA has great importance
because it often provides a clue for the presence of sepsis which is the underlying cause of
DKA in many instances.
Therefore, the patient developing respiratory alkalosis is a clue for us indicating that the
patient is most likely having sepsis