DKA & HHS: Diabetic Ketoacidosis & Hyperosmolar Hyperglycemic State
advertisement

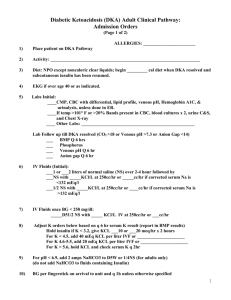
DKA & HHS Dr. Imad Abu Khader By: Fida Ayed DKA & HHS • Diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS) are endocrine emergencies occurring in diabetes patients. • Both conditions require prompt, adequate treatment to avoid mortality. In patients with known diabetes mellitus, both conditions are most commonly triggered by noncompliance with diabetes treatment or infection. • Nevertheless, any condition that induces severe insulin resistance and elevated counterregulatory hormones may trigger DKA or HHS, including severe trauma, myocardial infarction, and stroke. • DKA and HHS may be the presenting syndrome of previously unknown or new onset diabetes. Hyperglycemic Emergencies 1 DKA . 2 HHS 3 EDKA 4 Ketosis-Prone Diabetes (KPD 5 • MIXED HHS & DKA : Over 30% of patients have features of both DKA and HHS with most recent evidence confirming that about one out of four patients will have both conditions at the time of presentation with hyperglycemic crisis. Patients presenting with this phenotype have shown to have a worse prognosis and have a higher risk of mortality (8%). ) Epidemiology: 1.In contrast to popular belief, DKA is more common in adults than in children. 2.more than 40% of patients with DKA are older than 40 years, and more than 20% are older than 55 years 3.Up to 25–40% cases of T1D present as DKA at first diagnosis 4.According to a survey in USA, more than two-thirds of children presenting with HHS have T1D. These are mostly obese T1D and adolescent T2D. 5.It is estimated that out of all DKA cases, around 34% occur in T2D Epidemiology: in Palestine; 1.In 2016, in the annual PMoH report, the newly reported DM cases in primary diabetes clinics in West Bank were 5,148 cases 2.Data on T1DM in Palestine is very limited. No data is available for T2DM in children 3.In a recent modeling for diabetes projections, diabetes prevalence (for those aged 25years or more) is predicted to reach 21.5% in 2030, representing apredicted increase of 35% from 2000 to 2030. 4.The estimated number of patients withdiabetes is thus expected to reach 444,000 in 2030. 5.Prevalence in men increased from 9.1% to 16.9% and in women from 10.2% to 13.6%. mortality 1.DM is considered the fourth leading cause of death in Palestine. 2.In contrast to DKA, the mortality rate in HHS is considerably higher. It is 15% for HHS compared to 2–5% for DKA (Umpierrez et al. 2002). The possible explanations for this higher mortality rate for HHS are older age and presence of co-morbid conditions, the insidious time course of HHS, with more severe dehydration and secondary organ damage, may also contribute to the higher mortality risk. 3.DKA is the leading cause of mortality among children and young adults with T1D, accounting for ~50% of all deaths in diabetic patients younger than 24 years of age. In the United States, the overall inpatient DKA mortality is <1% , but a higher rate is reported among elderly patients with life-threatening illnesses. 4.mortality rates for those over 65–75 years reaching 20–40%. The cause of death in patients with DKA rarely results from the metabolic complications of hyperglycemia or metabolic acidosis but relates to the underlying medical illness (i.e., trauma, infection). 5.Over 30% of patients have features of both DKA and HHS. Patients presenting with this phenotype have shown to have a worse prognosis and have a higher risk of mortality (8%) compared to those with isolated hyperglycemic crises (3% for isolated DKA and 5% for isolated HHS). pathophysiology Setting up Morph HHS DKA 1 • Symptoms of hyperglycemia including polyuria, polydipsia, and weight loss are usually present for several days prior to the development of DKA 1 • Present 2 • weakness, nausea, vomiting, and abdominal pain 2 • Usually no abdominal pain 3 • Physical examination reveals signs of dehydration, including loss of skin turgor, dry mucous membranes, tachycardia, and hypotension 3 • Present 4 • Acetone on breath and labored Kussmaul respiration 4 • Not present 5 • Mental status can vary from full alertness to profound lethargy 5 • decrease LOC • Focal neurologic deficits and seizures may also occur in HHS precipitating factors 1.Infection is the most common precipitating factor for DKA, occurring in 30–50% of cases. 2.cerebrovascular accident, alcohol abuse, pancreatitis, pulmonary embolism, myocardial infarction, and trauma. Drugs that affect carbohydrate metabolism such as corticosteroids, thiazides, and sympathomimetic agents may also precipitate the development of DKA 3.Lack of insulin treatment adherence is reported as a major precipitating cause for DKA in urban black and medically indigent patients 4.use of sodium glucose co-transporter 2 (SGLT2) inhibitors has been associated with DKA in patients with T1D and T2D Key Diagnostic Criteria ( DKA) D K A HYPERGLYCEMIA KETOSIS ACIDEMIA blood glucose greater than 250 mg/dL (hydroxybutyrate and acetoacetic acid greater than 3 mmol) • pH lower than 7.3, serum bicarbonate lower than 15 mEq/L • elevated anion gap The key diagnostic feature is the elevation in circulating total blood ketone concentration. Key Diagnostic Criteria ( HHS) 1 2 HYPERGLYCEMIA HYPEROSMOLARITY severe hyperglycemia (.540–600 mg/ dL [30– 33.3 mmol/L] and often .1000 mg/dL hyperosmolarity (serum osmolality .320 mmol/kg) absence of significantly elevated ketone concentrations and metabolic acidosis. Other Laboratory Abnormalities DKA and HHS - AKI : patients may have secondary organ damage because of volume depletion, including acute kidney injury. Acute kidney injury is usually more pronounced in HHS patients, because of a more protracted time course before admission and more severe volume depletion. - CULTURES: cultures of urine, sputum, and blood .Infection (most commonly pneumonia and urinary tract infection) is a common precipitating event. Thus, cultures should be obtained if there are suggestive clinical findings. Recognize that infection may exist in the absence of fever in these patients. - ELECTROLYTES: Although patients have a potassium and phosphate deficit, admission serum potassium and phosphate are often normal or elevated as a result of insulin deficiency, hypertonicity, and acidemia - LIPIDS: Severe hyperlipidemia caused by lipolysis may lead to pseudohyponatremia and pseudonormoglycemia in DKA. LIPIDS • Patients with DKA or HHS may present with marked hyperlipidemia and lactescent serum. • Lipolysis in DKA, and to a lesser extent in HHS, is due to insulin deficiency, combined with elevated levels of lipolytic hormones (catecholamines, growth hormone, corticotropin [ACTH], and glucagon). • Lipolysis releases glycerol and free fatty acids into the circulation. High levels of serum fatty acids cause insulin resistance at both the peripheral and the hepatic level, and they serve as the substrate for ketoacid generation in hepatocyte mitochondria. • Insulin is the most potent anti-lipolytic hormone. KETONEMIA •Assessment of ketonemia can be performed by the nitroprusside reaction, which provides a semiquantitative estimation of acetoacetate and acetone levels, or by direct measurement of betahydroxybutyrate, the main ketoacid in DKA. •Accumulation of ketoacids results in an increased anion gap metabolic acidosis. •The anion gap is calculated by subtracting the sum of chloride and bicarbonate from the sodium concentration [Na-(Cl + HCO3)]. The normal anion gap is 12 ± 2 mEq/L •Not all patients who present with ketoacidosis have DKA. •Patients with chronic ethanol abuse with a recent binge culminating in vomiting and acute starvation may develop alcoholic ketoacidosis (AKA). •The key difference between AKA and DKA is the concentration of blood glucose. DKA is characterized by severe hyperglycemia; the presence of ketoacidosis without hyperglycemia in an alcoholic patient suggests AKA. • In addition, some patients with decreased food intake lower than 500 calories/day may present with starvation ketosis. The diagnosis of starvation ketosis is suggested by a history of poor intake and the fact that it rarely presents with a serum bicarbonate concentration less than 18 mEq/L OTHER LABS •Leukocytosis is present in most patients with DKA; however, a leukocyte count greater than 25,000 mm3 or the presence of greater than 10% neutrophil bands is seldom seen in the absence of bacterial infection. •The admission serum sodium is usually low because of the osmotic fux of water from the intracellular to the extracellular space in the presence of hyperglycemia. •An increase in serum sodium concentration in the presence of hyperglycemia indicates a rather profound degree of water loss. •The admission serum potassium concentration is usually elevated in patients with DKA. These high levels occur because of a shift of potassium from the intracellular to the extracellular space due to acidemia, insulin deficiency, and hypertonicity. Typical laboratory characteristics of DKA and HHS Fluid therapy • DKA and HHS patients have profound volume depletion, with an approximate water deficit of 100 mL/kg and 100–200 mL/kg body weight, respectively, requiring aggressive fuid resuscitation to restore intravascular volume and renal perfusion. • Isotonic saline (0.9% NaCl) is infused at a rate of 500–1000 mL/h during the first 2 h, but larger volume may be required in patients with hypovolemic shock to restore normal blood pressure and tissue perfusion. • After intravascular volume depletion has been corrected, the rate of normal saline infusion should be reduced to 250 mL/h or changed to 0.45% saline depending upon the serum sodium concentration. • when blood glucose falls below 200–250 mg/dL in DKA or 250–300 mg/dL in HHS, dextrose 5% should be added to the intravenous fluid to allow continued insulin treatment to suppress ketogenesis while avoiding hypoglycemia. Cont. •The free water defcit can be estimated, based on corrected serum sodium concentration, using the following equation: water defcit = (0.6)(body weight in kilograms) × (1 − [corrected sodium/140]). •The goal is to replace half the estimated water defcit over a period of 12–24 h. •An important aspect of fuid management in patients with DKA is to replace the volume of urinary losses. Failure to adjust fuid replacement for urinary losses may delay the correction of electrolytes and water deficit. MONITORING: Capillary blood glucose testing should be determined during treatment every 1–2 h at the bedside using a glucose oxidase reagent strip; and blood should be drawn every 4 h for determination of serum electrolytes, glucose, blood urea nitrogen, creatinine, magnesium, phosphorus, and pH until resolution of ketoacidosis. Typical total body deficits of water and electrolytes in diabetic ketoacidosis and hyperosmolar hyperglycemic state* Insulin therapy •The American Diabetes Association recommends an initial intravenous bolus of regular insulin of 0.1 units/kg of body weight, followed by a continuous infusion of regular insulin at a dose of 0.1 units/kg per hour until blood glucose levels reach 250 mg/dL. •Once glucose is lower than 250 mg/dL, dextrose should be added to intravenous fuids, and the insulin infusion rate is reduced to 0.05 units/kg per hour. •Thereafter, the rate of insulin administration should be adjusted to maintain glucose levels at approximately 150– 200 mg/dL and continued until ketoacidosis is resolved. •The goal is to lower blood glucose by 50–100 mg/dL per hour. •Resolution of hyperglycemia takes about 4–6 h, but resolution of ketoacidosis takes longer (~10–14 h); thus, dextrose is needed to allow insulin infusion and the prevention of hypoglycemia •Most cases of DKA are treated with intravenous insulin. In mild cases, subcutaneous insulin may be considered as an alternative Because these patients are generally not admitted to an intensive care unit. •An initial bolus of insulin is not needed, because fluid resuscitation by itself will reduce blood glucose, as described earlier. potassium •Measure potassium and other electrolytes every 2–4 hours. •An estimated total body potassium deficit of ~3–5 mEq/kg of body weight has been reported in adult patients with DKA; however, most patients present with normal or high serum potassium. •With initiation of insulin and fluid therapy, the extracellular potassium concentration invariable falls. •Insulin therapy and correction of acidosis decrease serum potassium levels by stimulating cellular potassium uptake in peripheral tissues. •Therefore, all patients require intravenous potassium to prevent hypokalemia. •The American Diabetes Association recommends the administration of intravenous potassium chloride (20– 30 mEq/L) as soon as the serum potassium concentration is below 5.5 mEq/L. •The treatment goal is to maintain serum potassium levels within the normal range of 4–5 mEq/L. •A presentation with severe hypokalemia may be aggravated during insulin administration, which can induce life threatening arrhythmias and respiratory muscle weakness. Thus, if the initial serum potassium is equal or lower than 3.0 mEq/L, potassium replacement should be given for 1–2 h at a rate of 10– 20 mEq per hour, before insulin infusion is started. carbonate • bicarbonate treatment increases the risk of hypokalemia and may paradoxically worsen intracellular acidosis. • Despite the lack of evidence, most experts in the feld recommend that in patients with severe metabolic acidosis (pH < 6.9–7.0), 44.6 mEq of sodium bicarbonate should be added to a liter of hypotonic saline until pH rises to at least 7.0. In patients with arterial pH > 7.0, no bicarbonate therapy is necessary. anticoagulant As DKA and HHS are procoagulant states, patients are at risk for venous thrombosis. Therefore prophylactic administration of low molecular-weight heparin is indicated. Transition to Subcutaneous Insulin Resolution of DKA has been defined as blood glucose concentrations below 200 mg/dL , plus two of the following: pH .7.3, bicarbonate 15 mmol/L, and/or anion gap 12 mmol/L. Resolution of HHS has been defined as normal serum osmolality and regained mental status. •The half-life of insulin is <10 min; thus, abrupt cessation of the insulin may result in rebound hyperglycemia, ketogenesis, and recurrent metabolic acidosis. •Subcutaneous insulin should be given at least 2 h before discontinuing the intravenous insulin infusion. complication: 1.Hypokalemia 2.hypoglycemia, 3.hyperchloremic metabolic acidosis 4.cerebral edema: This condition most often occurs in DKA episodes in children, with a prevalence of 0.3%–1%. In adults and patients with HHS, the condition is very rare. Once cerebral edema develops, mortality rates are high (20%–40%), and survivors are at risk for long-term sequelae. Clinical symptoms include new or worsening headache, gradually decreased consciousness, irritability, and seizures. When cerebral edema is suspected, prompt treatment with mannitol (0.5– 1.0 g/kg) has been recommended before computed tomography is obtained. Traditionally, development of cerebral edema has been attributed to rapid normalization of hyperosmolarity by fluid therapy and blood glucose lowering. Therefore, gradual correction of hyperglycemia and fluid deficits has been recommended, especially in critically ill children. Useful formulas for the evaluation of DKA Summary References: • Muneer, M., & Akbar, I. (2021). Acute Metabolic Emergencies in Diabetes: DKA, HHS and EDKA. Advances in experimental medicine and biology, 1307, 85–114. https://doi.org/10.1007/5584_2020_545 • Emilie V. Rosager, Amalia Lærke K. Heltø, Cathrine U. Fox Maule, Lennart Friis-Hansen, Janne Petersen, Finn E. Nielsen, Steen B. Haugaard, Rasmus Gregersen; Incidence and Characteristics of the Hyperosmolar Hyperglycemic State: A Danish Cohort Study. Diabetes Care 2023; dc230988. https://doi.org/10.2337/dc23-0988 • Moazzami, B., Zabala, Z.E., Umpierrez, G.E. (2023). Hyperglycemic Crises: Diabetic Ketoacidosis. In: Rodriguez-Saldana, J. (eds) The Diabetes Textbook. Springer, Cham. https://doi.org/10.1007/978-3-031-25519-9_44 • Mustafa OG, Haq M, Dashora U, Castro E, Dhatariya KK, the Joint British Diabetes Societies (JBDS) for Inpatient Care Group. Management of Hyperosmolar Hyperglycaemic State (HHS) in Adults: An updated guideline from the Joint British Diabetes Societies (JBDS) for Inpatient Care Group. Diabet Med. 2023; 40:e15005. doi:10.1111/dme.15005 • Vincent, J.-L., Moore, F. A., Bellomo, R., & Marini, J. J. (2024). text book of CRITICAL CARE (8th ed.). Elsevier. • Dhatariya KK; The Joint British Diabetes Societies for Inpatient Care. The management of diabetic ketoacidosis in adults—An updated guideline from the Joint British Diabetes Society for Inpatient Care. Diabet Med. 2022; 39:e14788. doi:10.1111/dme.14788