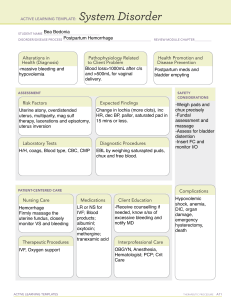
High Risk Pregnancy Care of a Woman with Postpartum Complications Chari V. Rivo NUPC 110 2nd Semester 20232024 Postpartal • Puerperium Period • Women are very susceptible to postpartum complications like hemorrhage, infections, thrombophlebitis which can result to personal injury, impaired fertility or even death Assessment • Elevated temperature • Relaxed uterus • Feeling of extreme sadness or unreality • Pallor • Thready, rapid, weak pulse • Pain and swelling • Decreased blood pressure • Uterine hemorrhage • Abdominal pain • Pain of symphysis pubis on walking • Perineal pain • Lochia with foul odor • Pain and tenderness in calf or leg Nursing Diagnosis • Deficient fluid volume r/t blood • Social isolation r/t precautions loss necessary to protect infant and others from infection • Ineffective breastfeeding r/t transmission development of mastitis • Risk for impaired parenting r/t • Ineffective peripheral tissue perfusion r/t interference with postpartum depression circulation secondary to • Risk for injury to self and development of newborn r/t postpartal thrombophlebitis (blood clot) psychosis • Risk for infection r/t • Acute pain r/t a collection of microorganism invasion of blood in traumatized tissue episiotomy, surgical incision (hematoma) secondary to birth site, or migration of trauma Outcome Identification and Planning • Provide measures that will restore the woman most quickly to health • Promote contact among her, her child, and her primary support person • Promote mother-infant attachment Implementation Interventions should include instruction for both self-care and child care. Outcome Evaluation • Lochia is free of foul odor. • Fundus remains firm and midline with progressive descent. • Patient maintains a urinary output greater than 30 ml/hr. • Lochia discharge amount is 6 in. or less on a perineal pad in 1 hour. • Patient maintains vital signs and oxygen saturation within defined normal limits. • Patient identifies signs and symptoms that should be reported. • Patient demonstrates attachment behaviors with infant Postpartum Hemorrhages • Bleeding is a major threat during pregnancy, labor and postpartum period • (Hge) One of the primary causes of maternal mortality assoc. with childbearing • (hge) defined as 500 ml or more following birth (Normal Delivery) • Blood loss of 1000 ml in CS • Four main reasons: four T’s • • • • Tone Trauma Tissue thrombin Uterine Atony Postpartum Hemorrhage • Relaxation of the uterus; most frequent cause of postpartum hemorrhage • Conditions increase the risk for• postpartal • Multiplethat gestation High parityHge: • • • • • • • • • Polyhydramnios Large baby Presence of uterine myomas Operative birth Rapid birth Placenta previa Placenta accreta Abruptio placenta Labor induction/augmentation (oxytocin) • • • • • • • • • Advanced maternal age Previous uterine surgery Prolonged and difficult labor Chorioamnionitis or endometritis Anemia History of PP Hge Prolonged use og Mg So4 or other tocolytics Fetal death DIC Uterine Atony Postpartum Hemorrhage • THERAPEUTIC MANAGEMENT: • Fundal massage • Administration of oxytocin as prescribed (bolus r dilute) • Administration of carboprost, prostaglandin F2a derivative, methergine as second possibilities (IM) • Prostaglandin E1 analogue may also be given rectally • PG may cause diarrhea and nausea – antiemetics may be given • These oxytoxics may cause high blood pressure – Uterine Atony Postpartum Hemorrhage • THERAPEUTIC MANAGEMENT: • Other Measures: • Elevate the woman’s lower extremities to improve circulation to essential organs. • Offer a bedpan or assist the woman to the bathroom at least every 4 hours to be certain her bladder is emptying because a full bladder predisposes a woman to uterine atony. To reduce the possibility of bladder pressure, insertion of a urinary catheter may be prescribed. Uterine Atony Postpartum Hemorrhage • THERAPEUTIC MANAGEMENT: • Other Measures: • Administer oxygen by face mask at a rate of about 10 to 12 L/min if the woman is experiencing respiratory distress from decreasing blood volume. Position her supine (flat) to allow adequate blood flow to her brain and kidneys. • Obtain vital signs frequently and assess them for trends such as a continually decreasing blood pressure with a continuously rising pulse Lacerations Postpartum Hemorrhage • Tears of the birth canal – may occur in the cervix, vagina, or perineum • Large lacerations w/c may cause infection or Hge can occur with: • Difficult or precipitate birth • In primigravidas • Birth of a large infant (<9 lb) • Use of forceps or vacuum extraction Lacerations Postpartum Hemorrhage • CERVICAL LACERATIONS • Usually found on the sides of the cervix, near the branches of the uterine artery • Blood loss may come from torn artery • Management: • Repair/suture • Maintain a calm environment and assure mother of NBs condition • Regional anesthesia if laceration is extensive or difficult to repair • Explain the procedure to the patient Lacerations Postpartum Hemorrhage • VAGINAL LACERATIONS • Easier to locate than cervical lacerations, but difficult to repair due to friable vaginal tissue • Management: • Balloon tamponade • Vaginal packing to maintain pressure on the suture line • Record time of placement and be certain to remove it 24-48 hr after or before discharge • IFC as vaginal packing may cause pressure on the urethra Lacerations Postpartum Hemorrhage • CERVICAL LACERATIONS • Usually found on the sides of the cervix, near the branches of the uterine artery • Blood loss may come from torn artery • Management: • Repair/suture • Maintain a calm environment and assure mother of NBs condition • Regional anesthesia if laceration is extensive or difficult to repair • Explain the procedure to the patient Lacerations Postpartum Hemorrhage • PERINEAL LACERATIONS • Occurs more during lithotomy than supine position • 4 classifications: • First degree laceration • Second degree laceration • Third degree laceration • Fourth degree laceration Lacerations Postpartum Hemorrhage • PERINEAL LACERATIONS CLASSIFICATIO DESCRIPTION N First degree Vaginal mucous membrane and skin of the perineum to the fourchette Second degree Vagina, perineal skin, fascia, levator ani muscle, and perineal body Third degree Entire perineum, extending to reach the external sphincter of the rectum Fourth degree Entire perineum, rectal sphincter, and some of the Lacerations Postpartum Hemorrhage • PERINEAL LACERATIONS • Management: • Suturing • Document degree of laceration • High fluid diet and stool softeners in the first week • No enema or rectal suppository for 3rd and 4th degree Retained Placental Fragments Postpartum Hemorrhage • Uterine bleeding occurs due to fragments that keeps the uterus from contracting fully • Usually happens with succenturiate placenta and placenta accreta Retained Placental Fragments Postpartum Hemorrhage • Assessment: • large fragments may cause immediate bleeding • Small fragments –bleeding may occur in PP day 6-10 • Uterus is not fully contracted • Management: • Removal of fragments –D&C • Methotrexate if fragment cannot be removed • Advise woman to observe color of lochia and report unusual change (serosa to alba to rubra) • Balloon occlusion • hysterectomy Uterine Inversion Postpartum Hemorrhage • A prolapse of the fundus of the uterus through the cervix that the uterus turns inside out • may occur if traction is applied to the umbilical cord to remove the placenta or if pressure is applied to the uterine fundus when the uterus is not contracted • Total Inversion – uterus protrudes in the vaginaä Uterine Inversion Postpartum Hemorrhage • Assessment: • Large amount of blood suddenly gushes from the vagina • Fundus is not palpable in the abdomen • Woman may show signs of blood loss • Hypotension • Dizziness, paleness, diaphoresis • Exsanguination may occur within 10 minutes Uterine Inversion Postpartum Hemorrhage • Assessment: • NEVER ATTEMPT TO: • Replace an inversion as it could increase bleeding • Remove placenta as it would create a larger surface for bleeding • Continue oxytocin as it makes the uterus more tense and difficult to replace Disseminated Intravascular Coagulation Postpartum Hemorrhage • Deficiency in clotting ability caused by vascular injury • Fibrinogen level falls to below effective limits • Presence of extreme bleeding and so many PLT and fibrin that rush to site (bleeding) that that there is not enough left in the rest of the body • Associated with premature separation of the placenta, missed miscarriage, or fetal Disseminated Intravascular Coagulation Postpartum Hemorrhage • Assessment: • Easy bruising or bleeding from IV site • Lab: PLT, prothrombin, thrombin time, fibrinogen Disseminated Intravascular Coagulation Postpartum Hemorrhage • Management: • To stop the process of DIC, stop the underlying insult • in pregnancy, birthing of the fetus and placental delivery is part of the solution • Heparin to halt clotting cascade (IV then SQ) • Blood/platelet/FFP/Cryoprecipitate transfusion after heparin treatment Disseminated Intravascular Coagulation Postpartum Hemorrhage • Evaluation; • Coagulation studies • Check if anoxia has occurred, part. In renal and brain cells • Fetal and NB assessment – evaluate efficiency of placental circulation Subinvolution Postpartum Hemorrhage • Incomplete return of the uterus to its prepregnant size and shape • May result from small retained placental fragment, mild endometritis or uterine myoma • Assessment: • At 4-6 week PP, uterus is still enlarged and soft Subinvolution Postpartum Hemorrhage • Management: • Methylergonovine, 0.2 mg q 6 (oral) • Tender uterus – endometritis • Oral antibiotics • Educate about normal process/lochia • May result to anemia and lack or energy from chronic blood loss • Seek early care Perineal Hematomas Postpartum Hemorrhage • Collection of blood in the subcutaneous layer of tissue • May occur after rapid spontaneous birth and in women with perineal varicosities • Usually represent only minor bleeding Subinvolution Postpartum Hemorrhage • Assessment: • Severe pain in the perineal area • Feeling of pressure between her legs • Intact skin but with area of purplish discoloration and swelling • Can be 2cm to 8cm in diameter • If tissue is drawn taut, it palpates as a firm globe and feels tender Perineal Hematoma Postpartum Hemorrhage • Management: • Report presence of hematoma • Estimated size • Degree of woman’s discomfort • Mild analgesic • Ice pack in a towel to prevent further bleeding • Usually resolves in 3-4 days • If size increases, incision and ligation of vessel may be done Perineal Hematoma Postpartum Hemorrhage • Management: • If episiotomy incision line is opened to drain a hematoma, it should be left open and packed with gauze to be removed in 24 to 48 hours Puerperal Infections • Infection of the reproductive tract in the postpartum period • Also a major cause of maternal mortality • May progress into peritonitis and septicemia • Causes: Grp. B strep, staphylococci, E. coli Puerperal Infections • Risk Factors: • Rupture of the membranes more than 24 hours before birth • Retained placental fragments within the uterus • Postpartal hemorrhage • Preexisting anemia • Prolonged and difficult labor, particularly with instrument births • Internal fetal heart monitoring electrode • Uterus explored after birth for a retained placenta or abnormal bleeding site Endometritis • Infection of the endometrium • Usually associated with chorioamnionitis and CS • Can lead to tubal scarring - infertility • Assessment: Puerperal Infections • • • • • • Fever (3rd or 4th day) Chills Loss of appetite General malaise Uterus not well contracted and painful to touch Dark brown and foul odor lochia Endometritis Puerperal Infections • UTZ to check for placental fragments • Management: • • • • • • • Vaginal fluid culture Antibiotics: as determined by culture Oxytoxic agents for uterine contraction Increase fluid intake Analgesics Walking for lochia drainage Use gloves when helping woman to change pads or linen; handwashing • Educate woman about S/S of endometritis upon discharge Infection of the Perineum Puerperal •Infections An episiotomy, suture line or laceration can be a portal of entry for bacterial invasion (usually local) • Assessment: • Pain, heat, feeling of pressure • With or w/o fever • Inflammation of the suture line, stitches may have sloughed away and purulent drainage may be present Infection of the Perineum Puerperal • Management: Infections • Systemic or topical antibiotic • • • • • • • Analgesic Open sutures to allow drainage Sitz bath, moist warm compress Hubbard tank Tx – to hasten drainage and cleanse the area Change perineal pads frequently Wiping from front to back after urinating or bowel movement Avoid placing the infant on the bottom bed sheet of the woman’s bed • Encourage ambulation Peritonitis Puerperal Infections • infection of the peritoneal cavity, usually an extension of endometritis • one of the gravest complications of childbearing and is a major cause of death from puerperal infection • Assessment • rigid abdomen, abdominal pain, high fever, rapid pulse, vomiting, and the appearance of being acutely ill Peritonitis Puerperal Infections • Management: • Paralytic ileus – blockage of inflamed intestines • NGT insertion • IV or TPN • Analgesics • IV antibiotics • Can cause infertility due to scarring Thrombophlebitis • inflammation with the formation of blood clots • Phlebitis – inflammation of the lining of a vessel • Classified as: • SVD – superficial vein disease • DVT – deep vein thrombosis Thrombophlebitis • Tends to occur during PP because; • A woman’s fibrinogen level is still elevated from pregnancy, leading to increased blood clotting. • Dilatation of lower extremity veins is still present as a result of pressure of the fetal head during pregnancy and birth so blood circulation is sluggish. Thrombophlebitis • Tends to occur in women who; • Are relatively inactive in labor and during the early puerperium because this increases the risk of blood clot formation • Have spent prolonged time in a birthing room with their legs positioned in stirrups • Have preexistent obesity and a pregnancy weight gain greater than the recommended weight gain, which can lead to inactivity and lack of exercise Thrombophlebitis • Tends to occur in women who; • Have preexisting varicose veins • Develop a postpartal infection • Have a history of a previous thrombophlebitis • Are older than age 35 years or have increased parity • Have a high incidence of thrombophlebitis in their family • Smoke cigarettes because nicotine causes Femoral Thrombophlebitis • Femoral, saphenous, or popliteal veins are Thrombophlebitis involved • Accompanying arterial spasm often occurs, diminishing arterial circulation to the leg • Decreased circulation with edema – white or drained appearance of the leg • Formerly known as milk leg or phlegmasia alba dolens (white inflammation) Femoral Thrombophlebitis • Assessment: Thrombophlebitis • Pelvic thrombophlebitis • Fever, chills, pain • Redness, swelling, warmth, hard inflamed vessel • Skin so stretched that it appears shiny and white • Affected leg diameter (thigh/calf level) is increased • Homans sign • Pain in the calf of the leg on dorsiflexion of the Femoral Thrombophlebitis • Management: Thrombophlebitis • Early ambulation • Use padded stirrups on examining tables • Support stockings for first 2 weeks after birth • Worn before getting up from bed • Removed twice a day to assess skin • Adequate fluid intake • Do not sit with knees crossed • Avoid constrictive clothing • Quit smoking Femoral Thrombophlebitis • Management: • Anticoagulants – heparin (IV) or LMWH (SQ) Thrombophlebitis • blood coagulation study • Heparin antidote; protamine sulfate • Warfarin antidote: Vit K • • • • • thrombolytics Application of moist heat Bed rest Assess risk for pressure ulcer Never massage the skin over the clotted area because this could loosen the clot, causing a pulmonary or cerebral embolism Femoral Thrombophlebitis • Management: Thrombophlebitis • Heparin – continue BF • Warfarin – discontinue BF • monitor lochia • Assess for signs bleeding: • Bleeding gums • Ecchymotic spots on the skin • Oozing from episiotomy suture line PelvicThrombophlebiti • Involves ovarian, uterine, or s Thrombophlebitis hypogastric veins • Occurs later than femoral thrombophlebitis • Inflammation may cause partial obstruction leadint to slowed blood flow and clots (stagnant blood) • Prevention of endometritis helps PelvicThrombophlebiti s Thrombophlebitis • Assessment: • High fever, chills, abdominal pain, weakness, general malaise • Severe infection necroses veins – pelvic abscess • Can become systemic – lung, kidney or heart valve abscess PelvicThrombophlebiti s Thrombophlebitis • Management: • Total bed rest • Analgesics, antibiotics, anticoagulants • Abscess – USG to locate and incision via laparotomy PelvicThrombophlebiti s Thrombophlebitis • Management: (Edx) • Wear nonconstricting clothing in lower extremities • Rest w/ feet elevated • Ambulate daily • Inform OB about previous history Pulmonary Embolus Thrombophlebitis • Obstruction of the pulmonary artery by a blood clot • Complication of thrombophlebitis – blood clot moves from leg vein to pulmonary artery Pulmonary Embolus Thrombophlebitis • Assessment: • Sudden sharp chest pain • Tachypnea • Tachycardia • Orthopnea • cyanosis Pulmonary Embolus Thrombophlebitis • Management: • Oxygen administrations • Strict monitoring - ICU Mastitis • Infection of the breast • Organism enters the cracked and fissured nipples, which comes from the nasal-oral cavity of the infant – epidemic mastitis/ epidemic breast abscess • Staph. Aureus or MRSA, or candidiasis (hosp. acquired) Mastitis • Assessment: • Unilateral or bilateral (epidemic mastitis) • Painful, swollen, and reddened breast • Fever • Scant breastmilk Mastitis • Management: • Antibiotics – dicloxacillin or cephalosphorin • Cold or ice compress/warm, wet compress • Good supportive bra • I&D if with abscess, purulent drainage Mastitis • Management: • To prevent nipples from cracking: • Making certain the baby is positioned correctly and grasps the nipple properly, including both the nipple and areola • Helping a baby release a grasp on the nipple before removing the baby from the breast • Washing hands between handling perineal pads and touching breasts • Exposing nipples to air for at least part of every day • Possibly using a vitamin E ointment daily to soften nipples • Encouraging women to begin breastfeeding (when the infant sucks most forcefully) on an unaffected nipple (if a Urinary Retention Urinary System Disorders • Bladder is unable to empty completely • Bladder sensation for voiding is decreased due to bladder edema caused by pressure of birth • Compounded by prolonged labor, perineal lacerations and use of epidural anesthesia • Incomplete emptying causes overdistention w/c may lead to permanent damage to bladder tone – permanent incontinence Urinary Retention Urinary System Disorders • Assessment • Primary overdistention – doesn’t void at all • With retention and overflow – woman voids frequently in small amounts • If first voiding is less than 100ml, suspect urinary retention • Residual urine is greater than 100 ml Urinary Retention Urinary System Disorders • Management: • Catheterization for residual urine • bladder training • Encourage voiding • Analgesic for relaxation • Reinsertion of catheter if woman is unable to void 8 hrs after removal of IFC UTI Urinary System Disorders • Pushing with labor may have allowed some secretions to enter the urinary urethra • Bacteria may be introduced during catheterization UTI Urinary System Disorders • Assessment: • Burning urination • Hematuria • Feeling of frequency or she always has to void • Pain in voiding • Resistance to voiding (due to pain) may cause urinary stasis, • Low grade fever • Lower abdominal pain UTI Urinary System Disorders • Assessment: • Clean-catch urine for analysis – independent nursing action UTI Urinary System Disorders • Assessment: • Clean-catch urine for analysis – independent nursing action • Make sure urine is not contaminated by lochia – provide sterile cotton ball to tuck in her vagina after perineal cleansing • Mark the specimen “possibly contaminated by lochia” UTI Urinary System Disorders • Management: • Increase OFI – a glass per hour • Analgesics - acetaminophen • Sulfa drug are CI in BF – may cause neonatal jaundice • Broad-spectrum antibiotics • Amox/ampicillin Cardiovascular System Disorders • Excess volume and pressure changes can still be present in the postpartal period Postpartal Preeclampsia Cardiovascular • Symptoms are the same with System Disorders Preec in pregnancy • Rarely develops in this period • Usually occurs due to retention of placental material – usually resolves after D & C Cardiovascular Disorders •System Management: • Bed rest • Quiet atmosphere • Monitoring of VS and UO • MgSO4 or antihypertensives • Seizures may occur 6 to 24 hours after birth • If seizures occur more than 72 hrs after birth, it may be unrelated to childbearing Cardiovascular Disorders •System Management: • Bed rest • Quiet atmosphere • Monitoring of VS and UO • MgSO4 or antihypertensives • Seizures may occur 6 to 24 hours after birth • If seizures occur more than 72 hrs after birth, it may be unrelated to childbearing Reproductive System Disorders • Organs may be weakened or displaced by pregnancy, especially in grand multiparty or those who had an instrument birth Reproductive Tract Displacement Reproductive Disorders •System Retroflexion, anteflexion, retroversion, and anteversion or prolapse of the uterus • Ligaments of the uterus are weakened due to pregnancy • Can interfere with childbearing and fertility • May cause pain or lower abdominal Reproductive Tract Displacement Reproductive System Disorders • Cystocele – outpouching of the bladder into the vaginal wall due to weakened vaginal walls • Rectocele – outpouching of the rectum into the vaginal wall Reproductive Tract Displacement Reproductive Disorders •System Management: • Surgery or repair if extensive • Stress incontinence (involuntary voiding on exertion) • Kegel’s exercise to strengthen perineal muscles • Pelvic floor physical therapy • botox Separation of the Symphysis Pubis Reproductive System Disorders • Due to relaxation of the joint and tearing or stretching of ligaments caused by large babies or abnormal fetal positions Separation of the Symphysis Pubis Reproductive System Disorders • Assessment: • Pain on turning or walking • Legs tend to rotate externally – waddling gait • Defect over symphysis pubis can be palpated • Area is swollen and feels tender to touch Separation of the Symphysis Pubis System Disorders •Reproductive Management: • Bed rest • Pelvic binder to immobilize joint, relieve pain and allow healing • 4-6 week for complete healing • Avoid heavy lifting • Have someone to help her with child care • Maybe advised CS for future pregnancy Emotional and Psychological •Complications Depression may cause impaired mother-infant bonding Postpartal Blues • Baby Blues • MC and least severe • Occurs w/in 3-5 days after birth • A normal, hormonally generated PP occurrence • Mothers who delivered prematurely and those who have an infant in NICU are at risk Postpartal •Depression May be related to hormonal shifts as pregnancy hormones decline • Women notices immediate feelings of sadness – postpartal blues • More serious problem that may continue beyond postpartum period – postpartum depression Postpartal •Depression Manifested by overwhelming sadness, extreme fatigue, inability to stop crying, increased anxiety about infant’s health, insecurity, psychosomatic symptoms (N & V, diarrhea), extreme mood fluctuations • Can occur in new mothers and fathers • Can interfere with BF, childcare and Postpartal •Depression Risk factors • History of depression • Troubled childhood • Low self-esteem • Stress in the home or at work • Lack of effective support • Different expectations between partners (e.g., if a woman wants a child and her partner does not) • Disappointment in the child (e.g., a boy instead of a girl) Postpartal Depression • Assessment: Tests • Postpartum Depression Predictors Inventory (PDPI) • Postpartum Depression Screening Scale (PDSS) Postpartal Depression • Management: • Selective Serotonin Reuptake Inhibitors (SSRIs) • Safe for BF • E.g. • Paroxetine (Paxil) • Fluoxetine (Prozac) • Sertraline (Zoloft) Postpartal Depression • Nursing Interventions • Teach pt about warning signs • Encourage verbalization of feelings • Help the woman understand that it’s normal to feel sadness or a lack of enthusiasm about motherhood. • Instruct the woman and her family that postpartum depression can occur at any time after delivery. • Advise the family of the warning signs of postpartum depression. Inform them that it’s important not to ignore even the subtlest of signs. Urge them to immediately report these signs to the practitioner. • Assist the woman in contacting a support group that can help to alleviate her feelings of isolation Postpartal Psychosis • 1 woman in 500 are considered psychiatrically ill a year after birth • A response to the crisis of childbearing • Exists when a person has lost contact with reality Postpartal Psychosis • Occurs 2-3 weeks after birth but can occur as early as first or second day PP • An emergency situation that requires immediate intervention • Causes: (predisposing factors) • Changing hormone levels • Lack of support system • Low self-esteem • Financial difficulties • Major life changes • History of mental illness Postpartum Psychosis • Assessment: Look for: • feelings that her baby is dead or defective • hallucinations that may include voices telling her to harm the baby or herself • severe agitation, irritability, or restlessness • poor judgment and confusion • feelings of worthlessness, guilt, isolation, or overconcern with the baby’s health • sleep disturbances • euphoria, hyperactivity, or little concern for self or infant Postpartum Psychosis • Assessment: Tests: • PDSS • Eating/sleeping disturbances • Anxiety/insecurity • Emotional liability • Mental confusion • Loss of self • Guilt/shame • Suicidal thoughts Postpartal Psychosis • Management: • Do not leave the woman alone • Do not leave her alone with infant • Do not contradict her opinions, instead, refer her to psychiatric counselor • Immediate hospitalization • Antipsychotics • Antidepressants • Suicidal precautions • Involve the family in the treatment plan Postpartal Psychosis • Nursing Interventions: • Include teaching about postpartum depression and psychosis as part of the patient’s discharge teaching plan. • Instruct the woman and her family that postpartum depression and psychosis can occur at any time after delivery. • Advise the family of the warning signs of postpartum depression and psychosis. Inform them that it’s important not to ignore even the subtlest of signs. Urge them to immediately report these signs to the practitioner Women with Unique Postpartal Care Needs • The Woman Whose Child Is Born With an Illness or a Physical Challenge • Loss of self-esteem due to an imperfect child and also see themselves as imperfect • Woman responds with grief reaction thinking that the image of a perfect child has died • Parents should be shown their child moments after birth so if a condition or problem exists, the newborn’s condition, prognosis, and usual plans for care can be immediately explained to them Women with Unique Postpartal Care Needs • The Woman Whose Child Is Born With an Illness or a Physical Challenge • Encourage parents to care for their child so they can touch, relate to, and “claim” the infant in as nearly normal a manner as possible • Open communication with parents and staff to discuss feelings of fear Women with Unique Postpartal Care Needs • The Woman Whose Newborn has Died • Show her the baby to help them begin grieving • Clean the baby and wrap in an infant blanket • Remain with them but give them time to handle and inspect their child • Prepare the forms needed for parents to