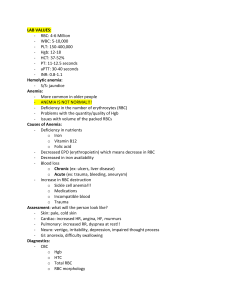
Chapter 30 - Hematologic Problems Anemia ➢ Definition and Classification • Anemia is a deficiency in the number of erythrocytes, the quantity or quality of hemoglobin and/or volume of packed RBCs (hematocrit). • Ultimately lead to tissue hypoxia due to blood loss, impaired production and destruction of erythrocytes which accounts for the signs and symptoms of anemia. • It is a manifestation of a pathologic process not a specific disease. • Anemia is diagnosed by CBC, reticulocyte, and peripheral blood smear. • Anemia can result from primary hematologic problems or can develop as a secondary consequence of disease or disorders of other body systems. ➢ The various types of anemia can be classified by either morphology (cellular characteristics or etiology (cause)) • Morphologic - RBC size and color. • Etiologic - clinical condition causing the anemia. • Morphologic - discuss patient care by focusing on the etiology. MORPHOLOGIC CLASSIFICATION OF ANEMIA Morphology Etiology Normocytic, normochromic Acute blood loss, hemolysis, chronic kidney disease, cancers, sideroblastic anemia, endocrine disorders, starvation, aplastic anemia, sickle cell anemia, pregnancy Microcytic, hypochromic Iron deficiency anemia, vitamin B6 deficiency, copper deficiency, thalassemia, lead poisoning Macrocytic (megaloblastic) normochromic Cobalamin (vitamin B12) deficiency, folic acid deficiency, liver disease (including effects of alcohol abuse) ETIOLOGIC CLASSIFICATION Decreased RBC production Blood Loss Decreased Hgb Synthesis Iron deficiency Thalassemia (decresed globin synthesis Sideroblastic anemia (decreased porphyrin Acute Trauma Blood vessel rupture Splenic sequestration crisis Defective DNA Synthesis Cobalamin (vitamin B12) deficiency Folic acid deficiency Chronic Gastritis Menstrual Flow Hemorrhoids Decreased Number of RBC Precursors Aplastic anemia and inherited disorders (e.g. Fanconi syndrome Increased RBC Destruction (Hemolytic Anemias) Hereditary (Intrinsic) Abnormal Hgb (sickle cell disease) Enzyme deficiency (G6PD) Anemia of myeloproliferative disease (e.g. leukemia) and myelodysplasia Chronic diseases or disorders Medications and chemicals (e.g. chemo and lead) Radiation Membrane abnormalities (paroxysmal nocturnal hemoglobinuria, hereditary spherocytosis) Acquired (Extrinsic) Physical destruction Prosthetic heart valves Extracorporeal circulation Disseminated intravascular coagulation (DIC) Thrombotic Thrombocytopenic Purpura (TTP) Antibodies against RBCs Infectious agents (e.g. malaria) and toxins ➢ Causes Of Anemia • • • Decreased RBC Production o Deficient nutrients - Iron - Cobalamin - Folic acid Blood Loss o Chronic - Bleeding duodenal ulcer - Colorectal cancer - Liver disease o Acute - Acute trauma - Ruptured aortic aneurysm - GI bleeding Increased RBC Destruction o Hemolysis - Sickle cell disease - Medication (e.g. methyldopa [aldomet] - Incompatible blood - Trauma (e.g. cardiopulmlonary bypass) ➢ Cultural and Ethnic Health Disparities • Sickle cell disease o high incidence among African Americans • Thalassemia o high incidence among African Americans and people of middle eastern origin • Tay-Sachs o highest incidence in families of Eastern European Jewish origin, especially the Ashkenazi Jews. • Pernicious anemia o high incidence among Scandinavians and African Americans. ➢ Clinical Manifestations • Clinical manifestations of anemia are caused by the body response to tissue hypoxia. • Hgb levels are often used to determine the severity of anemia. • Mild states of anemia (Hgb 10-12 g/dL [100-200 g/L] o May exist w/o symptoms unless pt has an underlying disease experiencing a compensatory response to exercise. o Symptoms include palpitations, dyspnea, and mild fatigue • Moderate anemia (Hgb 6-10 g/dL [60-100 g/L] o The above cardiopulmonary symptoms are increased o • Pt may experience them while resting as well as with activity Severe anemia (Hgb less than 6 g/dL [60 g/L] o Pt may have clinical manifestations involving many body systems ➢ Integumentary Manifestations • Pallor (reduced Hgb and reduced blood flow to the skin) • Jaundice (hemolysis of RBC resulting in increased serum bilirubin) • Pruritus (increased serum and skin bile salt concentrations) *The sclera of the eyes and mucous membranes should be evaluated as well because it reflects integumentary changes more accurately especially those of darker complexion. * ➢ Cardiopulmonary Manifestations • • Result from additional attempts of the heart and lungs to provide adequate amounts of O2 to the tissues. o CO is maintained by increasing HR and SV. o Low viscosity of the blood contributes to heart murmurs and bruits. MI, angina pectoris, HF, cardiomegaly, pulmonary and systemic congestion, ascites, and peripheral edema may develop if heart is overworked for an extended period of time. ➢ Pulmonary • Tachypnea, orthopnea, dyspnea at rest ➢ Neurological • Headaches, vertigo, irritability, depression, impaired though process ➢ GI • Anorexia, hepatomegaly, splenomegaly, difficulty swallowing, sore mouth (glossitis and smooth pruritus) ➢ Musculoskeletal • Bone pain ➢ General • Fatigue, sensitivity to cold, weight loss, lethargy NURSING AND INTERPROFESSIONAL MANAGEMENT: ANEMIA ➢ Diagnoses • Fatigue r/t inadequate oxygenation of the blood • Imbalanced nutrition: less than body requirements r/t inadequate nutritional intake and anorexia • Ineffective health management r/t lack of knowledge about appropriate nutrition and medication regimen ➢ Planning • The overall goals are that the pt with anemia will: o Assume normal activities of daily living o Maintain adequate nutrition o Develop no complications related to anemia. ➢ Nursing Implementation • Acute intervention may include o blood transfusion o drug therapy (e.g., erythropoietin, vitamin supplements) o RBC replacement o O2 therapy • Adequate nutritional intake • • Safety cautions to prevent cardiopulmonary stress, falls, and injury Food source to promote RBC maturation: o Avocadoes, red meat (rich in vit b12) ➢ Gerontologic Considerations • Anemia is not a normal finding • Anemia is rt an underlying cause such as iron deficiency, bleeding, chronic disease/inflammation. Renal insufficiency, or a hematologic cancer • S/s: o pallor, confusion, ataxia, fatigue, and worsening cardiovascular and resp problems ANEMIA CAUSED BY DECREASED ERYTHROCYTE PRODUCTION ➢ Erythrocyte • The normal life span is 120 days. • Three alterations in erythropoiesis may occur that decrease RBC production: o Decreased Hgb synthesis → iron deficiency anemia, thalassemia, and sideroblastic anemia. o Defective deoxyribonucleic acid synthesis in RBCs → megaloblastic anemias o Diminished availability of erythrocyte precursors → aplastic anemia and anemia of chronic disease IRON-DEFICIENCY ANEMIA ➢ Iron-deficiency anemia • The most common nutritional disorder in the world • The most susceptible to anemia are the very young, those on poor diets, and women in their reproductive years. • Normally 1mg of iron is lost daily in urine, bile, sweat, sloughing of epithelial cells from the skin and intestinal mucosa, and minor bleeding. ➢ Etiology • May develop because of: o inadequate dietary intake o malabsorption - Occurs in GI surgery and malabsorption syndrome such as removal or bypass if the duodenum or disease of the duodenum - blood loss - melena: black stool from upper GI bleed - peptic ulcers - gastritis - esophagitis - diverticula - hemorrhoids - neoplasia - GU blood loss (menstruation) - Postmenopausal bleeding - Chronic kidney disease - dialysis o Hemolysis ➢ Clinical manifestations • In early stages, there is no symptoms • Pallor (common) • Glossitis (inflammation of tongue) • Cheilitis (inflammation of lips) • Headache, paresthesia, burning sensation of tongue ➢ Diagnostic Studies • History and physical exam • HCT and Hgb lvls • RBC count, reticulocyte count • Serum iron, ferritin, and transferrin • Stool occult test o Done to determine the cause of iron deficiency • Endoscopy and colonoscopy o used to detect GI bleeding • Bone marrow biopsy o may be done if other test are inconclusive ➢ Food great in iron • Liver and muscle meats • Dried fruit • Legumes • Dark green leafy vegetables • Whole-grain and enriched bread and cereals • Beans ➢ Interprofessional Care • The main goal is to treat the underlying disease that is causing the reduced intake (e.g. malnutrition, alcoholism) or absorption of iron. • Drug therapy o Oral iron should be used whenever possible. When administering iron, consider the following five factors: - Iron is absorbed best from the duodenum and proximal jejunum ▪ Enteric-coated or sustained release caps, which release iron farther down the GI tract are counterproductive and expensive - The daily dose: 150-200 mg of elemental iron ▪ Can be ingested in three or four daily dosage which each tablet or cap of iron preparation containing between 50-100mg of iron. - Iron is best absorbed in an acidic environment. ▪ Should be taken about an hour before meals, when the duodenal mucosa is most acidic. ▪ Taking iron with vit C (ascorbic acid) or orange juice, which contains ascorbic acid, enhance iron absorption. - Undiluted liquid iron may stain the patient’s teeth. ▪ Iron should be diluted and ingested through a straw - GI side effects of iron administration: ▪ Black tarry stool ▪ Constipation – use stool softener or laxative if needed o Parental use of iron is indicated for: - Malabsorption, intolerance of oral iron, a need for iron beyond normal limits or poor patient adherence in taking the oral preparations of iron Parental: ▪ IM (z-track bc iron can stain tissues) or IV ➢ Nursing Management: Iron-deficiency Anemia • Certain groups of individuals are at an increased risk for the development of iron deficiency anemia. These include: o Premenopausal o Pregnant women o Person from a low social economic background o Older adults o Individuals experiencing blood loss • Diet teaching with an emphasis on foods with iron and ways to maximize absorption is important for these groups. • To replenish the body's iron stores, the patent needs to take iron therapy for 2-3 months after the Hgb level returns to normal. • Patients who require lifelong iron supplementation should be monitored for potential liver problems related to the iron storage. MEGALOBLASTIC ANEMIAS ➢ Megaloblastic anemia • A group of disorders caused by impaired DNA synthesis and characterized by the presence of large RBCs o When DNA synthesis is impaired, defective RBC maturation results. • The RBCs are large (macrocytic) and abnormal are referred to as megaloblasts. They are easily destroyed due to their fragile membranes. • Although most result from cobalamin and folic acid deficiency, this type of RBC deformity can also occur from DNA synthesis by drugs, inborn error f cobalamin and folic acid metabolism and erythroleukemia (malignant blood disorder characterized by. A proliferation of erythropoietic cells in bone marrow). Cobalamin (vitamin B12) Deficiency • • Normally a protein termed intrinsic factor (IF) is secreted by the parietal cells of the gastric mucosa if they are not cobalamin (extrinsic factor) cannot be absorbed. Vit B12 is needed for the myelin sheath ➢ Etiology • Pernicious Anemia o Most common cause; absence of intrinsic factor (IF) o Gastric mucosa is not secreting IF bc of either gastric mucosal atrophy or autoimmune destruction of parietal cells - Parietal cells secretes hydrochloric (HCI) acid, and there for is also decreased o Affects ages 40-60 (60 most common age of diagnosis) o Common in Northern European (esp. Scandinavians) and African Americans ➢ Other Causes of Cobalamin Deficiency • GI surgery (gastrectomy or gastric bypass) • Small bowel resection involving the ileum • Crohn's disease • Ileitis • Celiac disease • Dverticula of the small intestine • Chronic atrophic gastritis *In these cases it is because of the loss of IF-secreting gastric mucosal cells* • • • • Excessive alcohol or hot tea ingestion Smoking Long-term users of H2-histamine receptor blockers and proton pump inhibitors Strict vegetarians ➢ Clinical manifestations • • • • • • • Sore, red, beefy shiny tongue Anorexia, nausea Vomiting Abdominal pain. Neurological manifestations: o Weakness o Paresthesia of feet and hands o Reduced vibratory and position senses o Ataxia o Muscle weakness o Impaired though processes (confusion to dementia) It may take several months for these to develop (insidious disease) ➢ Diagnostic Studies • RBCs appear large (macrocytic) and have abnormal shapes. • Serum cobalamin levels are reduced. • If serum folate levels are normal but cobalamin is low then that suggest anemia is due to cobalamin deficiency • Serum test anti-IF antibodies done for pernicious anemia • Upper GI endoscopy and biopsy because pernicious anemia increases risk for stomach cancer • Serum methylmalonic acid (MMA) is elevated in cobalamin deficiency • Serum homocysteine elevated in both cobalamin and folic acid deficiencies • Testing for serum methylmalonic acid (MMA) (elevated mainly in cobalamin deficiency) and serum homocysteine (elevated in both cobalamin and folic acid deficiencies) helps determine the cause of this type of anemia. ➢ Interprofessional care • Instruct pt on adequate dietary intake to maintain goal of good nutrition. • Parental vitamin B12 or intranasal cyanocobalamin is the treatment of choice. Without it these individuals will die in 1-3 years. • Oral and sublingual versions are available for those whose GI absorption is intact. As along as supplements are used anemia can be reversed. ➢ Foods that contain Vit B12 • Red meats, especially liver, eggs, enriched grain products, milk, and dairy foods, fish Folic Acid Deficiency ➢ Folic Acid is also required for DNA synthesis and RBC formation and maturation. • • Common causes: o Dietary deficiency (green leafy vegetables, citrus fruits) Malabsorption syndromes: o Celiac disease o Crohn's disease o Small bowel resections o Drugs interfering with absorption or use of folic acid - Methotrexate - Antiseizure drugs o Increased requirement (pregnancy) o Chronic alcoholism o Chronic hemodialysis ➢ Clinical manifestations • Similar to those of cobalamin deficiency. • GI disturbances included dyspepsia and a smooth, beefy red tongue. • The absence of neurologic problem is a differentiating factor from cobalamin deficiency. ➢ Diagnostic findings • Serum folate is low (normal is 3-16 ng/mL [7-36 nmol/L]) and the cobalamin level is normal. ➢ Interprofessional care • • • Folic acid is treated by replacement therapy. Usual dosage id 1mg/day by mouth. In malabsorption of alcoholism states up to 5 mg/day may be required. Encourage pt to eat food containing large amounts of folic acid. ➢ Foods containing Folic Acid: • Green leafy veggies, liver, meat, fish, legumes, whole grains, orange juice, permute, avocado ➢ Nursing Management: Megaloblastic Anemia • Evaluate those with a positive family history. • Bring signs and symptoms to attention of HCP. • Carefully asses neurologic problems • Pt should have frequent ad careful appropriate screening for gastric cancer. • Protein patient of injuries, falling, burning and trauma. • If heat therapy is used evaluate skin frequently for redness. SICKLE CELL DISEASE ➢ Sickle cell disease (SCD) • A group of inherited, autosomal recessive disorders characterized by an abnormal form of hgb in the RBC. • Usually identified during routine neonatal screening. It is an incurable disease that is often fatal by middle age because of renal failure, infection, pulmonary failure and/or stroke. ➢ Etiology and Pathophysiology • • • • • • • In SCD the abnormal hgb S results from the substitution of valine for glutamic acid of the B-globin chain of hgb. Hgb S causes the erythrocyte to stiffen and elongate, takin on a sickle shape in response to low O2 levels. Types of SCD: o Sickle cell anemia - Most severe - Occurs when a person is homozygous for hemoglobin S (Hgb SS) - Person has inherited Hgb S from both parent o Sickle cell-thalassemia and Sickle cell Hgb C disease - Occurs when a pt inherited Hgb S from one parent and another type of abnormal hemoglobin (Such as thalassemia or hemoglobin C) from the other parent o Sickle cell train - Occur when a person is heterozygous for hemoglobin S (Hgb AS) - Pt has inherited hemoglobin S from one parent and normal Hemoglobin (Hgb A) from the other parent Sickling Episodes o Commonly triggered by low O2 tension in blood o Hypoxia or deoxygenation of the RBCs can be caused by: - Viral or bacterial infection (common) - High altitude - Emotional or physical stress - Surgery - Blood loss - Dehydration - Increased hydrogen ion concentration (acidosis) - Increased plasma osmolality - Decreased plasma volume - Low body temperature - No obvious cause Sickled cells cannot easily pass through capillaries or other small vessels and can cause vascular occlusion leading to acute or chronic tissue injury. Circulating sickled cells are hemolyzed by the spleen, leading to anemia. Sickle cell crisis: o A severe, painful, acute exacerbation of RBC sickling, causing a vaso-occlusive crisis - As blood flow is impaired by sickled cells, vasospasm occurs, further restricting blood glow - Severe capillary hypoxia causes changes in membrane permeability, leading to plasma loss, hemoconcentration, thrombi, and further circulatory stagnation - Tissue ischemia, infarction, and necrosis eventually occur from lack of O2 - Shock is a possibly life-threatening consequences bc of severe O2 depletion and reduction of circulating fluid volume - Crisis can begin suddenly and persist for days to weeks. ➢ Clinical manifestations • • • • • Primary symptom: pain o Pain episodes are accompanied by fever, swelling, tenderness, tachypnea, HTN, n/v - Affect any area of the body or several site simultaneously, with back, chest, extremities and abdomen Pt may have chronic health problems and pain bc of organ tissue hypoxia and damage (e.g., involving the kidneys or liver) Pallor (check mucous membrane) Skin may have grayish cast Jaundice because of hemolysis and pt become more prone to gallstone (Cholelithiasis) ➢ Complications • W/ repeated episodes of sickling, there is gradual involvement of all body systems, especially spleen, lungs, kidney, and brain • Infection is a major cause or morbidity and mortality o Autosplecnectomy: spleen becomes small bc of repeated scarring o Spleen fails to phagocytize foreign substance as it become infarcted and dysfunctional • Acute chest syndrome: o Used to describe acute pulmonary complication that include pneumonia, tissue infarction, and fat embolism - Characterized by: ▪ Fever ▪ Chest pain ▪ Cough ▪ Pulmonary infiltrates ▪ Dyspnea • Infarction may cause pulmonary HTN, MI, HF, and cor pulmonale • Heart may become ischemia and enlarge leading to HF • Priapism: persistent penial erection ➢ Diagnostic studies • • • • • • • Peripheral blood smear may reveal sickled cells and abnormal reticulocytes o The presence of Hgb S can be diagnosed by the sickling test, which uses RBCs (in vitro) and exposes them to a deoxygenation agent. Clinical findings include hemolysis (jaundice, elevated serum bilirubin levels) and abnoral lab test results. Hgb electrophoresis may be done to determine the about of hgb S, Skeletal X-rays demonstrate bone and joint deformities and flattening MRIs may be used to dx a stroke caused by blocked cerebral vessels from sickled cells. Doppler students used to assess for DVT, Chest X-ray to dx infection or organ malfunction etc. ➢ Nursing and Interprofessional Management Sickle cell disease • • • • • • • • • • Interprofessional care for a patient with SCD is directed toward: o Prevention of sequealae from the disease o Alleviating manifestation for the complication of the disease o Minimizing end-organ damage o Promptly treating serious sequelae, such as acute chest syndrome, that can lead to immediate death, Teach patients with SCD to avoid high altitudes, maintain adequate fluid intake and treat infections promptly. Screening for retinopathy should begin at age 10 Immunizations should be administered (such as pneumococcal, haemophilus influenzas, influenzas, and hepatitis) O2 may be administered to treat hypoxia and control sickling Assess for any changes in respiratory status, rest may reduce metabolic requirements and DVT prophylaxis. Fluids and electrolytes are administered to reduce blood viscosity and maintain renal function. Priapism is managed with pain meds, fluids and nifedipine (procardia). o If not resolved call urologist who can inject corpus carvernosum eith a filute solution of epinephrine to preserve penile function. During an acute pain crisis, optimal pain control usually includes large dosages of continuous opioid analgesics along with breakthrough analgesia often in the form of pain controlled analgesia (PCA). A holistic approach should be used that addresses the pain and its impact on the patients psychologic, social and spiritual well-being • • • Occupational and physical therapy can optimize functioning, o Referral of social and chaplain services can assist. Infection is a frequent complication and must be treated, Although may sickling agents have be tried, hydroxyurea (hydrea) is the only one that has been shown to be beneficial. This drug produces the about of fetal hgb (hgb F) and alters the adhesion of sickled RBCs to the endothelium. Acute chest syndrome are treated w/ broad spectrum antibiotics, O2 therapy, fluid therapy, and possible exchange transfusion POLYCYTHEMIA ➢ The production and presence of increased numbers of RBCs • Increase causes increased blood viscosity (hyperviscosity) and volume (Hypervolemia) ➢ Etiology • Primary polycythemia Vera o A chronic myeloproliferative disorder, includes increase in RBCs, WBCs, and platelets o 60 years old w/ slight male predominance o Enhanced blood viscosity and blood volume w/ congestion of organs and tissues w/ blood o Splenomegaly and hepatomegaly are common o Hypercoagulopathies that predispose clothing problems o Associated w/ mutations in the Janus Kinarse-2 (JAK2) gene - Gene provides instructions for making a protein that promotes proliferation of cells, especially blood cells from hematopoietic stem cells - Begins w/ one or more DNA mutations of a single hematopoietic stem cells • Secondary polycythemia o Hypoxia driven secondary polycythemia, hypoxia stimulates erythropoietin (EPO) production in the kidney, which in turn stimulate RBC - The need for increase O2 results from high attitudes, pulmonary disease, cardiovascular disease, alveolar hypoventilation, defective O2 transport, or tissue hypoxia o Hypoxia independent secondary polycythemia, EPO is produced by a malignant or benign tumor tissue - Serum EPO remains elevated o Splenomegaly does not accompany secondary polycythemia ➢ Clinical manifestation and Complications • Occur because if HTN caused by hyperviscosity and hypervolemia • First manifestations: o Headache, vertigo dizziness, tinnitus, visual disturbances • Generalized pruritus’ (often exacerbated by a hot bath) rt histamine release from an increased number of basophils • Paresthesia and erythromelalgia (painful burning and redness of ands and feet) • Angina, FH, intermittent claudication, thrombophlebitis, which may be complicated by embolization o Caused by blood vessel distention, impaired blood flow, circulatory stasis thrombosis, tissue hypoxia caused by hypervolemia and hyperviscosity • Stroke secondary thrombosis • Hemorrhagic caused by either vessel ruptures from overdistention or inadequate platelet function may result in petchia, ecchymoses, epistaxis, or GI bleeding • Hepatomegaly and splenomegaly from organ engorgement may contribute to pt complaints of satiety and fullness • Plethora: ruddy complexion • Hyperuricemia caused by the increase RBC destruction that accompanies excessive RBC production o Uric acid is a product of cell destruction ➢ Diagnostic Studies • o (1) Elevated hemoglobin and RBC count w/ microcytosis o (2) Low to normal EPO level (secondary polycythemia has high EPO Level) o (3) Elevated WBC count w/ basophilia o (4) Elevated platelet count (thrombocytosis) and platelet dysfunction o (5) Elevated leukocyte alkaline phosphatase, uric acid, and cobalamin levels o (6) Elevated histamine levels Bone marrow examination shows hypercellularity or RBCs, WBCs, and platelets ➢ Interprofessional Care • Treatment is directed toward reducing blood volume and viscosity and bone marrow activity • Phlebotomy is to reduce hematocrit and keep it less than 45% in men and 42% in women • Hydration therapy is used to reduce the blood’s viscosity • Ruxolitnib (Jakafi), which inhibits the expression of JAK2 mutation, is used for pts who have not responded o hydroxyurea • Low-dose heparin used to prevent clotting • Anagrelide may be used to reduce the platelet cunt and inhibit platelet aggregation. ➢ Nursing Management • Primary is not preventable • Evaluate hydration for overhydration and underdehydration • Myelosuppressive agents used • Assess pt nutritional status, since inadequate food intake can result in HI symptoms of fullness, pin, dyspepsia PROBLEMS OF HEMOSTASIS ➢ Hemostasis involves: • Endothelium, platelets, and coagulation factors, which normally function together to stop hemorrhage and repair vascular injury o Disruption of any of these components could result in bleeding or thrombotic disorders • Three major disorders: o Thrombocytopenia (low platelet count) o Hemophilia and von Willebrand disease (inherited disorders of specific clotting factors) o Disseminated Intravascular Coagulation (DIC) (process of clotting and unclotting) THROMBOCYTOPENIA ➢ Etiology and Pathophysiology • A reduction of platelets below 150,000 o Acute, severe, or prolonged decreases from this normal range can result in abnormal hemostasis that manifests are prolonged bleeding from minor trauma or spontaneous bleeding without injury • Inherited (e.g., Wiskott-Aldrich syndrome) • Acquired o Drugs - Chemotherapy drugs - Aspirin o Quinine o Infections - Viral infection (hep C virus, HIV, cytomegalovirus) - Bacterial infections o Hematologic malignancy Hematologic malignancy (Leukemia, lymphoma, myeloma) o Disseminated Intravascular Coagulation (DIC) o Immune thrombocytopenic purpura (ITP) - Most common cause of acquired - Syndrome of abnormal destruction of circulating platelets - Primarily an autoimmune disease; platelets are coated w/ antibodies ▪ Function normally, when they reach the spleen the antibody coated platelets are recognized as foreign and are destroyed by macrophages ▪ Decreased platelet production contribute to this o Thrombotic thrombocytopenic purpura (TTP) - Uncommon syndrome characterized by hemolytic anemia, thrombocytopenia, neurologic abnormalities, fever (in absence of infection), and renal abnormalities not all feature are present in all pts - Almost always associated w/ hemolytic-uremia syndrome (HUS); often referred to as TTP-HUS - Enhanced aggregation of platelets, which formation thrombi that deposit in arterioles and capillaries - Deficiency of a plasma enzyme (ADAMS13) that usually break down the von Willebrand clotting factory (vWF) into normal size ▪ W/o enzyme, usually large amounts of vWF attach to activated platelets, thereby promoting platelet aggregation - Predominate in female o Heparin-induced thrombocytopenia (HIT) - Also called heparin-induced thrombocytopenia and thrombosis syndrome (HITTS) - Pts develop 5-10 days after the onset of heparin therapy - Should never be given heparin - Major clinical problem: ▪ Venous and arterial thrombosis ▪ Arterial vascular infarcts resulting in skin necrosis, stoke, and end-organ damage - Platelet factor 4 (PF4) (protein made and release by platelets) binds to heparin ▪ Then binds to platelet surface, leading to further platelet activation and release of more PF5 thus creating a positive feedback - Management therapies: ▪ Heparin may be discontinued ▪ To maintain anticoagulation pt should be started on other anticoagulant ▪ If severe clotting, protamine sulfate, thrombolytic agent, and surgery removal of clots ➢ Clinical Manifestation • Many are asymptomatic • Bleeding is the most common symptoms o Petechia – small red/purple marks on the skin o Ecchymoses – discoloration of the skin resulting from bleeding underneath • Hemorrhage • Confusion, headache, seizures, and coma due to TTP-related thrombosis may be seen ➢ Diagnostic Studies • Thrombocytopenia: platelet <150,000 • Prolong bleeding doesn’t occur till platelets <50,000 • <20,000 spontaneous life-threatening bleeding • ITP antigen specific assay, platelet action/function assay, PF4 heparin complex for HIT ➢ Nursing Management • Acute care o Goal is to prevent or control hemorrhage o If subcut injection are unavoidable the use of small-gauge needle and application of direct pressure for 10-15 minutes o In a woman, menstrual bleeding may exceed the usual amount and duration - Counting sanitation napkins is helpful - Blood loss of 50ml will completely soak napkin - Suppression of menses w/ hormonal agents may be indication w/ predictable periods • Pt / caregiver teaching o o o o o o o o o o o o Notify HCP for manifestation of bleed (Stool, vomit, bruising, headaches) Ask HCP for restriction on activities Do not blow nose forcefully Do not bed down w/ head lower than your waist Prevent constipation by drinking plenty of fluids Shave only w/ electric razor Do not tweeze eyebrows Do not puncture skin (tattoos, piercing) Avoid meds that prolong bleeding Use soft bristly toothbrushes Women menstruation should keep tract of flow Ask HCP before any invasive procedures NEUTROPENIA • • • Leukopenia refers to decrease in total WBC count o Granulocytpenia- include neutrophils, eosinophils, basophils o Neutrophilic granulocytes - play a major role in phagocyting pathogenic microbes, closely monitor indicating infection Neutropenia - reduction in neutrophils o Absolute neutrophil count (ANC) - Determined by multiplying the total WBC count by the percentage of neutrophils o Neutropenia defined as ANC less than 1000 o Severe neutropenia <500 Important to know where the decrease in neutrophil count was gradual or rapid, the degree of neutropenia, and duration o Faster drop, the longer the duration, the most susceptible to infection, sepsis, and death ➢ Clinical Manifestation • • • • A low-grade fever is of great significance because it may indicate infection and lead to septic shock and death Neutropenic fever (>100.4 and neutrophil count <500) is an emergency Blood culture should be drawn STAT and antibiotics started within 1 hour Complaints of sore throat and dysphagia, ulcerative lesion of the pharyngeal and buccal mucosa, diarrhea, rectal tenderness, vaginal itching or discharge, SOB, and nonproductive cough ➢ Diagnostic Studies • • • • • Peripheral WBC count Bone marrow aspiration Biopsy Differential WBC count Peripheral blood smear used to assess immature form of WBCs ➢ Nursing Management • • • • • • (1) Determine the cause of neutropenia (2) instituting antibiotic therapy promptly (3) Identifying the offending organism if an infection has developed (4) Administering hematopoietic growth factors prophylactically after chemotherapy (5) implementing protect practice (hand washing) Teaching o Wash hands frequently • • • • • • • • Notify HCP: o Fever >100.4 o Chills or felling hot o Redness, swelling, discharge, or new pain on or in your body o Changes in urination or bowel movements o Cough, sore throat, mouth sores or blister If at home take temp as directed Avoid crowds and people w/ flu, or infection o If in public place wear mask, use hand sanitizer frequently Avoid uncooked meats, seafood or eggs, and unwashed fruits and veggies Bathe or shower daily and use moisturizer to avoid cracking skin Maintain some daily activity Brush teeth w/ soft brush 4 times a day Do not perform garden or clean up after pets LEUKEMIA • • A group of malignant disorder affecting the blood and blood-forming tissues of the bone marrow, lymph system, and spleen Accumulation of dysfunctional cells because of loss of regulation in cell division ➢ Etiology and Pathophysiology • • All cancer begins w/ mutation of DNA of certain cells Chemical agents, chemo, viruses, radiation, and immunologic deficiencies have been associated w/ development ➢ Classifications • Acute o Characterized by the clonal proliferation of immature hematopoietic cells • o Acute Myelogenous Leukemia (AML) - Adults - Uncontrolled proliferation of myeloblastic (macrophages..), the precursor of granulocytes - Hyperplasia of bone marrow - Strongly linked to toxins, congenital, and hematologic disorders - infiltration of malignant cells in skin, gums, and other soft tissue - S/s: ▪ fatigue, weakness, headache, mouth sores, anemia, bleeding, fever, infection, sternal tenderness, gingival hyperplasia, milk hepatosplenomegaly o Acute Lymphocytic Leukemia (ALL) - Children mostly - Immature small lymphocytes (T and B cells, NK cells) proliferation in bone marrow; most are B cell origin - Generalized lymphadenopathy, infections, weight loss, hepatosplenomegaly, headache, mouth sores - Increased intracranial pressure (n/v, lethargy, cranial nerve dysfunction) secondary to meningeal infiltration - S/S: ▪ Fever, pallor, bleeding, anorexia, fatigue, weakness, bone, joint, and ab pain Chronic o Involve more mature form of WBC, and the disease onset is more gradual o Chronic Myelogenous Leukemia (CML) - Excessive development of mature neoplastic granulocytes in bone marrow - Infiltrate liver and spleen - Blastic phase: more acute, aggressive phase - Philadelphia chromosome originates from the translocation b/w the BCR gene on chromosome 22 and ABL gene on chromosome 9 creating BCR-ABL - No symptoms in early stages - S/S: ▪ Fatigues and weakness, fever, sternal tenderness, weight loss, joint pain, bone pain, massive splenomegaly, increase in sweating o Chronic Lymphocytic anemia (CLL) - Most common in adults - Production and accumulation of functionally inactive but long-lived small matureappearing lymphocytes - Infiltrate bone marrow spleen and liver - Frequently no symptoms ➢ Diagnostic Studies • Peripheral blood evaluation and bone marrow exam diagnose and classify types ➢ Interprofessional Care • Attaining remission or disease control is a realistic option for majority of pts o Complete remission: - no evidence of overt disease on physical examination, and bone marrow and peripheral blood appear normal o Partial remission: - lesser state of control; lack of symptoms and a normal peripheral blood smear but still evidence of disease in bone marrow - Minimal residual disease tumor cells that cannot be detected by morphologic examination but can be identified by molecular testing o Molecular remission: all molecule studies are negative for residual leukemia • Stages of chemo o Induction therapy - Aggressive seeks to destroy leukemic cells in the tissues, peripheral blood, and bone marrow to eventually restore normal hematopoiesis on bone marrow recovery o Postinduction or postremission therapy - Intensification therapy (high-dose) therapy, may be given immediately after induction therapy for several months - Consolidation therapy: ▪ Started after remission is achieved ▪ Purpose is to eliminate remaining leukemia cells that may not clinically or pathological evident o Maintenance therapy - Treatment w/ lower doses of some drugs used in induction given every 3 to 4 weeks for prolonged period - Goal is to keep body free of leukemic cells ➢ Nursing Management • Acute care: o Maximizing the pt physical function o Teaching pts that acute side effects of treatment are usually temporary o Encouraging pts to discuss their quality of life issues LYMPOMAS • Malignant neoplasm originating in the bone marrow and lymphatic structure resulting in proliferation of lymphocytes HODGKIN’S LYMPHOMA • • Reed-Sternberg cells, located in lymph nodes Occurs b/w 15 and 30 and above 55 ➢ Etiology • • • Infection of Epstein Barr viruses (EBV), genetic predisposition and exposure to occupational toxins Increased w/ HIV infection Normal structure of lymph nodes is destroyed by hyperplasia of monocytes and macrophages ➢ Clinical Manifestations • • • • • • Initially development is most often enlargement of cervical (80%), mediastinal, axillary, or inguinal lymph nodes Nodes remain moveable and nontender S/S: o Weight loss, fatigues, weakness, fever, chills, tachycardia, or night sweats Initial findings include fever (>100,4), drenching night sweats, weight loss termed B symptoms Alcohol induced pain hepatomegaly, splenomegaly, anemia ➢ Diagnostic and Staging Studies • • • • • • Peripheral blood analysis Excisional lymph node biopsy Bone marrow examination Radiologic evaluation can help define all sites and determine the clinical stage of disease Staging: o Stage 1: involvement of single lymph node o Stage 2: involvement of 2 or more on one side of diaphragm o Stage 3: lymph node involvement above and below diaphragm o Stage 4: involvement outside diagram (e.g., liver, bone marrow) o Stages followed by A (Absent) or B (presence) to indicated systemic symptoms Dx: Undergo a liver function test ➢ Interprofessional Management • • Standard chemo that is the ABVD regimen o Doxorubicin (Adriamycin) o Bleomycin o Vinblastine o Dacarbazine Advanced stages use BEACOPP o Brentuximab vedotin (Adcetris), bleomycin, etoposide, doxorubicin (Adriamycin), cyclophosphamide, vincristine (Oncovin), procarbazine and prednisone NON-HODGKIN’S LYMPHOMA (NHLs) • Heterogenous group of malignant neoplasm of primary B-, T-, and NK cells organ affecting all ages ➢ Etiology and Pathophysiology • May result from: o Chromosol translocation o Infections o Environmental infections o Immunodeficiency states ➢ Clinical Manifestation • • • • • Can originate outside the lymph nodes the method of spread is unpredictable Primary: painless lymph node enlargement Manifest in nonspecific ways such as airway obstruction, hyperuricemia, and renal failure from tumor lysis syndrome, pericardial tamponade, and HI complaints B symptoms Pt undergoing chemotherapy is at risk for developing tumor lysis syndrome ➢ Diagnostic and Staging Studies • Treatment is guided by the cell type, cytogenetic studies, and clinical behavior: indolent (low grade), aggressive (high grade), highly aggressive (very high grade) MULTIPLE MYELOMA* • • Or plasma cell myeloma, condition in which neoplastic plasma cells infiltrate the bone marrow and destroy bone More common in men and African Americans ➢ Etiology and Pathophysiology • • Instead of plasma cells producing antibodies to fight different infection, myeloma tumors produce monoclonal (M proteins) (they are all one of a kind) antibodies o They don’t fight infection and infiltrate bone marrow o M protein are made up of 2 light chains and 2 heavy chains - Bence jones protein are the light chain part o Show up in urine Plasma cell production of excessive and abnormal number of cytokines also play a role in pathologic process of bone destruction ➢ Clinical Manifestations • • • • • Pain in pelvis, spine, and ribs common and trigged by movement Diffuse osteoporosis develops as bone is destroyed Osteolytic lesions are seen in skill, vertebrae, and ribs Hypercalcemia causing GI, renal, or neurological manifestations such as polyuria, anorexia, confusion, seizures, coma, cardiac problems Serum hypervelocity symptoms leading to central, pulmonary, renal, and organ dysfunction can occur in some pts ➢ Interprofessional Care • Hydration and ambulation treat hypercalcemia, dehydration, and potential renal damage • • • • • • Weight bearing helps reabsorb some calcium and fluids dilute calcium and prevent protein precipitates from causing renal tubular obstruction Control pain and preventions of pathology fracture Analgesic orthopedic supports and local radiation help reduce skeletal pain Kyphoplasty control spine vertebral disease by injecting cement to stabilize vertebrae Bisphosphonates inhibit bone breakdown and used for treatment of skeletal pain and hypercalcemia o Inhibit bone reabsorption without inhibiting born formation and mineralization Chemotherapy reduced plasma cells ➢ Nursing Management • • Use caution when moving pt bc of pathological fractures Hydration