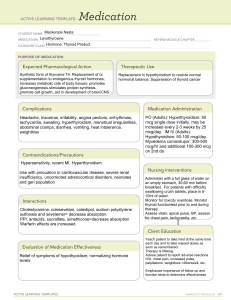
DRUGS ACTING ON THE THYROID GLAND : HYPOTHYROIDISM CLASSIFICATION DRUGS PHARMACODYNAMICS PHARMACOKINETICS INDICATIONS SIDE EFFECTS / INTERACTIONS NURSING CONSIDERATIONS THYROID REPLACEMENTS LEVOTHYROID Converts to T3, then binds to Variable, incomplete absorption Hypothyroidism PO: thyroid receptor proteins exerting from GI tract. Protein binding: ADULTS metabolic effects through control greater than 99%. Widely 60 YRS OR of DNA transcription and protein distributed. Deiodinated in YOUNGER synthesis. Therapeutic Effect: peripheral tissues, minimal WITHOUT Involved in normal metabolism, metabolism in liver. Eliminated EVIDENCE growth and development. Increases by biliary excretion. Half-life: 6– OF basal metabolic rate, enhances 7 days. CORONAR gluconeogenesis, stimulates protein Y HEART synthesis DISEASE: 1.6 mcg/kg/day as single daily dose. Adjust dose by 12.5–25 mcg/day q3–6 wks. Usual maintenanc e: 100–125 mcg/day. ADULTS OLDER THAN 60 YRS WITHOUT EVIDENCE OF Occasional: Reversible hair loss at start of therapy in children. Rare: Dry skin, GI intolerance, rash, urticarial, pseudotumor cerebri, severe headache in children Excessive dosage produces signs/symptom s of hyperthyroidis m (weight loss, palpitations, increased appetite, tremors, anxiety, tachycardia, hypertension, headache, insomnia, menstrual BASELINE ASSESSMENT Obtain baseline TSH, T3, T4, weight, vital signs. Signs/symptoms of diabetes, diabetes insipidus, adrenal insufficiency, and hypopituitarism may become intensified. Treat with adrenocortical steroids before thyroid therapy in coexisting hypothyroidism and hypoadrenalism. INTERVENTION/E VALUATION Monitor pulse for rate, rhythm (report pulse greater than 100 or marked increase). Observe for tremors, anxiety. Assess appetite, sleep pattern. Children: (Undertreatment): May decrease CORONAR Y HEART DISEASE: Initially, 25–50 mcg once daily. ADULTS WITH CARDIAC DISEASE: Initially, 12.5–50 mcg/day. Adjust dose by 12.5– 25 mcg/day at 6–8-wk intervals. CHILDRE N OLDER THAN 12 YRS, GROWTH AND PUBERTY INCOMPL ETE: 2–3 mcg/kg/day. CHILDRE N 6–12 YRS: 4–5 mcg/kg/day. CHILDRE N 1–5 YRS: 5–6 mcg/kg/day. CHILDRE N 6–12 MOS: 6–8 mcg/kg/day. CHILDRE N 3–5 MOS: 8–10 irregularities). Cardiac arrhythmias occur rarely. Long-term therapy may decrease bone mineral density intellectual development, linear growth. (Overtreatment): Adversely affects brain maturation, accelerates bone age. Monitor thyroid function tests. PATIENT/ FAMILY TEACHING • Do not discontinue drug therapy; replacement for hypothyroidism is lifelong. • Follow-up office visits, thyroid function tests are essential. • Take medication at the same time each day, preferably in the morning. • Monitor pulse for rate, rhythm; report irregular rhythm or pulse rate over 100 beats/ min. • promptly report chest pain, weight loss, anxiety, tremors, insomnia. • Children may have reversible hair loss, increased aggressiveness during first few mos of therapy. • Full therapeutic effect may take 1–3 wks. mcg/kg/day. LIOTHYRONINE In hormonal replacement, liothyronine is more potent and present a faster action when Liothyronine replaces endogenous thyroid hormone and then exerts its physiologic effects by controlling DNA transcription and protein CHILDRE N YOUNGER THAN 3 MOS: 10– 15 mcg/kg/day. Myxedema Coma IV: ADULTS, ELDERLY: Initially, 200–400 mcg, then 50–100 mcg once daily until able to tolerate PO administratio n. Pituitary ThyroidStimulating Hormone (TSH) Suppression PO: ADULTS, ELDERLY: Doses greater than 2 mcg/kg/day usually required to suppress TSH below 0.1 milliunits/L. Thyroid supplementation in hypothyroidism. Treatment or suppression of weight loss nervousness Monitor and report signs of excessive or inadequate dosing. compared to synthesis. This effect on DNA euthyroid goiters. levothyroxine but the is obtained by the binding of Diagnostic agent time of action is liothyronine to the thyroid for suppression significantly shorter. receptors attached to DNA. tests to differentiate The type of treatment Exogenous liothyronine exerts mild needs to be well all the normal effects of the hyperthyroidism evaluated as the fast endogenous thyroid T3 from thyroid gland correction of thyroid hormone. Hence, it increases autonomy. hormones in certain energy expenditure, Treatment of diseases presents accelerates the rate of cellular myxedema coma additional risks such as oxidation stimulating growth, (IV formulation). heart failure.3 The onset maturation, and metabolism of of activity is observed a the body tissues, aids in few hours after myelination of nerves and administration and the development of synaptic maximum effect is processes in the nervous observed after 2-3 days. system and enhances carbohydrate and protein metabolism excessive sweating Excessive doses mimic sensitivity to heat hyperthyroidism, as indicated by nervousness, weight loss, muscle wasting, tachycardia, and heat intolerance. Inadequate doses mimic temporary hair loss (particularly in children during the first months of therapy) hypothyroidism, as indicated by lethargy, weight gain, bradycardia, and cold intolerance. Assess heart rate, ECG, and heart sounds, especially during exercise (See Appendices G, H). Report any rhythm disturbances or symptoms of increased arrhythmias, including palpitations, chest discomfort, shortness of breath, fainting, and fatigue/weakness. Assess episodes of angina pectoris at rest and during exercise. Attempt to determine if pain is drug related, or caused by cardiovascular dysfunction (e.g., angina that occurs during exercise). Assess height in children periodically; inform physician of delayed growth that might indicate premature skeletal maturation and closure of epiphyseal plates. Monitor and report signs of CNS toxicity, including irritability and sleep loss. Sustained or severe CNS signs are typically consistent with hyperthyroidism and may require an adjustment in drug dose. LIOTRIX Thyroid hormone drugs are The hormones, T4 and T3, are May be used to fatigue, sluggishness, natural or synthetic preparations tyrosine-based hormones treat primary, containing T4 or T3 or both. produced by the thyroid gland. secondary or increase in weight, T4 and T3 are produced in the Iodine is an important tertiary alopecia, palpitations, human thyroid gland by the component in their synthesis. hypothyroidism. iodination and coupling of the The major secreted form of May also be used to dry skin, urticaria, amino acid tyrosine. Liotrix is a thyroid hormone is T4. T4 is suppress thyroid headache, synthetic preparation of T4 and converted T3, the more active stimulating hyperhidrosis, T3 in a 4:1 weight-based ratio. thyroid hormone, by hormone (TSH) These hormones enhance deiodinases in peripheral secretion in patients pruritus, asthenia, oxygen consumption by most tissues. T3 acts in the body to with simple increased blood tissues of the body and increase increase basal metabolic rate, (nontoxic) goiter, the basal metabolic rate and the alter protein synthesis and subacute or chronic pressure, arthralgia, metabolism of carbohydrates, increase the body's sensitivity lymphocytic myalgia, tremor, lipids and proteins. Thus, they to catecholamines (such as thyroiditis hypothyroidism, exert a profound influence on adrenaline). Thyroid hormones multinodular goiter, increase in TSH, every organ system in the body are essential for proper and in the and are of particular importance development and management of decrease in TSH, in the development of the differentiation of all cells of thyroid cancer. nausea, chest pain, central nervous system. the human body. T4 and May be used in T3 regulate protein, fat and conjunction with hypersensitivity, carbohydrate metabolism to other antithyroid keratoconjunctivitis varying extents. The most agents to treat pronounced effect of the thyrotoxicosis to sicca, increased heart hormones is in altering how prevent rate, irregular heart human cells use energetic goitrogenesis and rate, anxiety, compounds. The thyroid hypothyroidism. hormone derivatives bind to May also be used depression, and the thyroid hormone receptors for differential insomnia. initially to initiate their diagnosis of downstream effects. suspected mild hyperthyroidism or thyroid gland autonomy. Thyroid hormones should be used with great caution in a number of circumstances where the integrity of the cardiovascular system, particularly the coronary arteries, is suspected. These include patients with angina pectoris or the elderly, in whom there is a greater likelihood of occult cardiac disease. In these patients therapy should be initiated with low doses, i.e., one tablet of Thyrolar (liotrix) % or Thyrolar (liotrix) %. When, in such patients, a euthyroid state can only be reached at the expense of an aggravation of the cardiovascular disease, thyroid hormone dosage should be reduced. Thyroid hormone therapy in patients with concomitant diabetes mellitus or diabetes insipidu s or adrenal cortical insufficienc y aggravates the intensity of their symptoms. Appropriate adjustments of the various therapeutic measures directed at these concomitant endocrine diseases are required. THYROID DESICCATED Desiccated thyroid treats hypothyroidism (low thyroid hormone). Desiccated thyroid is also used to treat or prevent goiter (enlarged thyroid gland), and is also given as part of a medical tests for thyroid disorders. Thyroxine (T4): 40% to 80%; T3: 95%; desiccated thyroid contains T4, T3, and iodine (primarily bound). Hepatic to triiodothyronine (active); ~80% T4 deiodinated in kidney and periphery; glucuronidation/conjugation also occurs; undergoes enterohepatic recirculation Initial dose: 30 mg orally per day Maintenance dose: Increase in increments of 15 mg per day every 2 to 3 weeks to a usual maintenance dose of 60 to 120 mg/day Fast heart rate Hair loss Muscle pain Irregular heartbeats (arrhythmias) Nervousness Tremor Diarrhea Cramps Thyroid desiccated is generally acceptable for use during pregnancy. Controlled studies in pregnant women show no evidence of fetal risk. Adrenal insufficiency: Use with caution in patients with adrenal insufficiency; symptoms may be exaggerated or aggravated; contraindicated in patients with uncorrected adrenal insufficiency. Treatment with glucocorticoids should precede thyroid replacement therapy in patients with adrenal insufficiency (ATA/AACE [Garber 2012]). Cardiovascular disease: Use with caution and reduce dosage in patients with angina pectoris or other cardiovascular disease; chronic hypothyroidism predisposes patients to coronary artery disease. Diabetes: Use with caution in patients with diabetes mellitus and insipidus; symptoms may be exaggerated or aggravated. Myxedema: Use with caution in patients with myxedema; symptoms may be exaggerated or aggravated; initial dosage reduction is recommended in patients with longstanding myxedema.