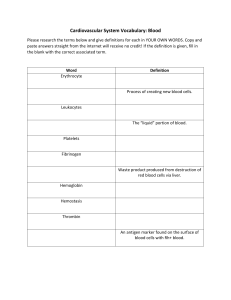
Circulation pattern Characteristics Blood is what type of tissue? Blood Formed elements & plasma Processes & Regulation Veins Arteries Pulmonary Circuit Venules Arterioles Right Side Lungs Left Side Body Capillary beds Functions Distribution • • • • • O2 Nutrients CO2 Waste Hormones Regulation • • • • Temperature pH Volume Osmolarity Protection • Prevent blood loss • Prevent infection Plasma Solutes Proteins Lactic acid, urea, creatinine 90% water Nutrients O2 CO2 Common Proteins Albumins Globulins 60% Transport Fibrinogen Prothrombin Blood clotting Transport lipids Protection Formed Elements • Erythrocytes (RBCs), Leukocytes (WBCs), Platelets • Hematocrit – %RBC / total blood volume Erythrocyte Leukocyte Thrombocyte No nuclei Complete cells Platelets Biconcave Gas transport 2 categories Surveillance & Immunity Pieces of cells Clotting Note the biconcave shape Interesting facts about RBCs O2 is not very soluble in blood About 2.4 million are made every second Each RBC contains about 280 million hemoglobin molecules (each binds 4 O2) They live 100 – 120 days Erythrocyte • • • • anaerobic, >surface area, Hemoglobin binds O2 & CO2 reversibly Heme + Globin 2alpha, 2beta Fe within Heme Hemoglobin (Hb) Hemoglobin + O2 = Oxyhemoglobin Oxygen Loading Lung Hemoglobin – O2 = Deoxyhemoglobin Oxygen Unloading Tissue Hemoglobin + CO2 = Carbaminohemoglobin Tissue Vit. B12 Folic Acid Proteins Lipids Erythropoiesis Carbs Iron stores EPO Stimulates marrow Ferritin Hemosiderin Transferrin Erythropoiesis red bone marrow It’s highly controlled with Erythropoietin Too few RBC Anemia Too many RBC Polycythemia Negative or Positive Feedback? More RBC increases O2 in blood Tissue Hypoxia Kidney produces EPO EPO stimulates Erythropoiesis What gets created must be destroyed… After 100-120 days… membranes become fragile RBCs die and are phagocytized Liver/Spleen Macrophage phagocytize Hg Globin & Heme Globin’s amino acids are recycled Liver Bilirubin, Ferritin, Hemosiderin Bilirubin (intestines) bile stercobilin (bacteria) Stercobilin excreted in feces Test Yourself Why Does Poor Liver Function Result In Jaundice? Thalassemia results in malformed globin. How might this affect Hct? Sickle cell anemia results in ‘sickled’ RBCs with brittle plasma membranes. How might this affect their function? Leukocytes… note the diversity Interleukins Macrophage T cells Leukopoiesis Increase with infection Colony stimulating factors Stem cells Hemocytoblast Myeloid stem cell Committed Myeloblast cells Myeloblast Lymphoid stem cell Myeloblast DevelopPromyelocyte Promyelocyte Promyelocyte mental pathway Eosinophilic myelocyte Basophilic myelocyte Neutrophilic myelocyte Eosinophilic band cells Basophilic band cells Neutrophilic band cells Eosinophils Basophils Neutrophils (a) (b) (c) Lymphoblast Promonocyte Prolymphocyte Monocytes Lymphocytes (e) (d) Agranular leukocytes Granular leukocytes Some become Macrophages (tissues) Some become Plasma cells Thrombocytes megakaryocytes, granules Serotonin, Ca2+, enzymes, platelet-derived growth factor Form Platelet Plug Inactivated by NO Hemocytoblast Megakaryoblast Promegakaryocyte Megakaryocyte Platelets Figure 17.12 SEM 4100x Broken vessels must be plugged 1 3 Coagulation Vascular spasm Hemostasis 2 Platelet plug formation Vasoconstriction Platelets Fibrin strands in clot Blood clot Collagen fibers Platelet plug Vessel injury Erythrocyte in clot Erythrocyte Endothelial cells 1 Vascular spasm Blood vessel constricts to limit blood escape. 2 Platelet plug formation Platelets arrive at site of injury and stick to exposed collagen fibers. 3 Coagulation phase Coagulation cascade converts inactive proteins to active forms and forms a blood clot. Vascular Spasm Platelet Plug Formation Coagulation Chemicals from Endothelial cells Endothelial cell damage Cascade soluble proteins Smooth muscle contraction Localized Intrinsic & Extrinsic Positive feedback Serotonin 30 minutes Chemotaxis Prothrombin Activator Prothrombin Thrombin Fibrinogen Fibrin Clot Retraction and Repair • Stabilizes clot (serum squeezed from fibrin) • Repair – PDGF rebuilding of vessel wall – Fibroblasts new connective tissue – Growth Factors endothelial cells divide Why control clotting? Bleeding occurs Blood flow is blocked Remove clotting factors quickly Inhibit clotting factors • Thrombin blocked by Fibrin, Antithrombin III, Heparin Preventing Undesirable Clotting