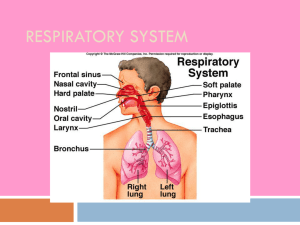
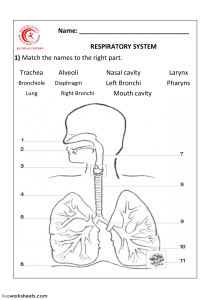
Case 5 pbl 2. Respiratory System Divided in upper and lower respiratory system Upper respiratory system: nose, nasal cavity, paranasal sinuses, pharynx Lower respiratory system: larynx, trachea, bronchi, bronchioles and alveoli of lungs Thoracic inlet narrower Anything that expands here exerts pressure Will squash oesophagus and veins Superior vena cava syndrome or superior mediastinal syndrome Upper respiratory system Nose, nasal cavity, paranasal sinuses Nose primary passageway for air entering the respiratory system Air enters through nares open into nasal cavity Nasal vestibule is space within flexible tissue of nose Nasal septum divides nasal cavity into left and right portion Bony portion: fusion of perpendicular plate of ethmoid bone and plate of vomer Anterior portion: hyaline cartilage nasi and apex of nose Maxillary, nasal, frontal, ethmoid, sphenoid bones form lateral and superior walls of nasal cavity Nasal cavity consists of vestibule, respiratory portion and olfacotyr area. Paranasal sinuses (frontal, sphenoid, ethmoid, paired maxillary and palantine bones) secrete mucous Keep surfaces of nasal cavity moist and clean Olfactory region is superior portion of nasal cavity Areas lined by olfactory epithelium 1. Interior surface of cribiform plate 2. Superior portion of nasal septum 3. Superior nasal conchae Superior, middle, inferior nasal conchae project toward nasal septum Air flows between adjacent conchae to pass from vestibule to internal nares Through superior, middle, inferior meatuses Narrow grooves not open passageways Air bounces off conchal surface Churns As it swirls, small particles come into contact with mucous Turbulences provides extra time for warming and humidifying Bony hard palate Portions of maxillary and palatine bones Forms nasal cavity and separates it from oral cavity Soft palate Fleshy Posterior to hard palate, marks boundary between superior nasopharynx and rest of pharynx Nasal cavity opens into nasopharynx (connection called internal nares) Pharynx Chamber shared by digestive and respiratory system Extends between internal nares and entrances to larynx and oesophagus Superior and posterior walls closely bound to axial skeleton Lateral walls are flexible and muscular Pharynx divided into three regions 1. Nasopharynx Superior portion Connected to posterior portion of nasal cavity through internal nares Separated from oral cavity by soft palate Lined by pseudostratified ciliated columnar epithelium Pharyngeal tonsil located on posterior wall Each auditory tube opens into nasopharynx at nasopharyngeal meatus on either side of tonsil 1. Oropharynx Extends between soft palate and base of tongue at level of hyoid bone Posterior portion of oral cavity and posterior inferior portion communicates directly with oropharynx Boundary between nasopharynx and oropharynx: epithelium changes from pseudostratified columnar epithelial to stratified squamous epithelium 1. Laryngopharynx Inferior portion of pharynx Portion of pharynx between hyoid bone and entrance to pharynx and oesophagus Lined with stratified squamous epithelium Lower respiratory system Larynx Cartilaginous tubes that surrounds and protects glottis At top of trachea Prevents foreign material other than air going down Helps with phonation Begins at level of C or C Ends at level of C Divided into three regions 1. Supraglottis Epiglottis False vocal cords Laryngeal ventricles 1. Glottis Consists of true vocal cords Anterior and posterior commissues 1. Subglottis Region below true vocal cords Extending down to lower border of cricoid cartilage Three, unpaired cartilages form larynx 1. Thyroid cartilage Largest laryngeal cartilage Hyaline cartilage Anterior and lateral walls of larynx U shaped (posteriorly incomplete) Inferior surface articulates with cricoid cartilage Superior surface has ligamentous attachments to hyoid bone and to epiglottis and smaller laryngeal cartilages Superior to cricoid cartilage 1. Cricoid cartilage Hyaline cartilage Posterior portion greatly expanded provide support in absence of thyroid cartilage Protects glottis and entrance to trachea Broad surfaces for attachments of laryngeal muscles and ligaments Ligaments attach inferior surface to first tracheal cartilage Superior surface articulates with arytenoid cartilages 1. Epiglottis Projects superior to glottis Elastic cartilage Ligamentous attachments to anterior and superior borders of thyroid cartilage and hyoid bone During swallowing, larynx elevated epiglottis folds back over glottis prevents liquids and solids entering respiratory tract Larynx contains three pairs of small hyaline cartilages 1. Arytenoid cartilages Articulates with superior border of enlarged portion of cricoid cartilage 1. Corniculate cartilages Articulates with arytenoid cartilages Corniculate and arytenoid cartilages function in opening and closing of glottis and production of sound 1. Cuneiform cartilages 4 6 5 Elongated, curving Lie within folds of tissue that extend between lateral surface of each arytenoid cartilage Ligaments bind varius laryngeal cartilages Ligaments attach thyroid cartilage to hyoid bone and cricoid cartilage to trachea Cricotrachael ligament Median cricothyroid ligament attaches thyroid cartilage to cricoid cartilage Vestibular ligaments and vocal ligaments extend between thyroid cartilage and arytenoid cartilages Vestibular and vocal ligaments covered by folds of laryngeal epithelium Vestibular ligaments: lie within superior pair of folds (vestibular folds) Folds inelastic Lie laterally to glottis Prevent foreign objects entering open glottis Protect vocal folds of glottis Glottis is made up of vocal folds Space between them rima glottides Highly elastic Involved with production of sound known as vocal cords Trachea Tough, flexible tube 2,5cm in diameter, 11cm in length Begins anterior to C in ligamentous attachment to cricoid cartilage Ends in mediastinum at level of T branches into right and left pulmonary bronchi Contains 15-20 tracheal cartilages stiffen tracheal walls and protect airway prevent it from collapsing or over expanding in respiratory system Each tracheal cartilage is C-shaped Closed portion of C protects anterior and lateral surfaces of trachea Open portion of C faces posteriorly toward oesophagus Cartilages not continuous posterior tracheal wall can distort when swallowing Elastic ligament and trachaelis muscle connect ends of tracheal cartilage Tracheal lumen size Adult: 12mm (4,5cm ) 1mm decrease in diameter will result in 16% reduction in lumen size Neonate: 3mm (0,28cm ) 1mm decrease in diameter will result in 43% reduction in lumen size First year of life lumen not >3mm In childhood, in mm. responds roughly to age in year Implications for infections and trauma to trachea and larynx: children vs adults (eg. Croup) 6 5 2 2 Implications for damage to small diameter airways Primary bronchi Extrapulmonary bronchi Trachea branches into mediastinum into left and right primary bronchi Carina separates two bronchi Have C-shaped rings Ends of C overlap Right bronchus supplies right lung, left bronchus supplies left lung right pulmonary bronchus larger in diameter, descends toward lung at steep angle each primary bronchus travels to groove along medial surface of lung groove hilum of lung provides access for entry to pulmonary vessels, nerves, lymphatics entire complex is the root of the lung (anterior to T (right) and T (left)) root attaches to mediastinum and fixes positions of major nerves, blood vessels and lymphatic vessels 5 Lungs surrounded by pleural cavities each lung is a blunt cone its apex points superiorly extend above clavicle apex on each side extends superior to first rib concave inferior rests on superior surface of diaphragm 6 many impressions on lung left: arch of aorta right: azygous vein hilar contents bronchi pulmonary arteries pulmonary veins bronchial arteries lymphatics and nodes parasympathetic nerves sympathetic nerves Lobes and surfaces of lungs lungs have lobes separated by deep fissures right lung has three lobes separated by horizontal and oblique fissures Superior Middle Inferior Left lung has two lobes separated by oblique fissure Superior Has a lingula Inferior Right lung broader than left lung Left lung is longer than right lung Indented by cardiac notch Lymphatic drainage Bronchi As primary bronchi enter lungs, they divide to form smaller passageways Intrapulmonary bronchi Primary bronchus divides to form secondary bronchi (lobar bronchi) One secondary bronchus goes to each lobe Right lung has three secondary bronchi Left lung has two secondary bronchi Secondary bronchi branch to form tertiary bronchi (segmental bronchi) Supplies air to single bronchopulmonary segment Portion of lung supplied by specific tertiary bronchus and arteries Smallest subunit that a surgeon will resect when taking out a bit of lung Has own arterial, lymphatics, venous, air supply Right lung: 10 bronchopulmonary segments Left lung: 8 or 9 bronchopulmonary segments Walls of 1 , 2 and 3 bronchi contain progressively less cartilage 2 and 3 , cartilages form plates arranged around lumen Serve same structural purpose as rings of cartilage in trachea and primary bronchi As amount of cartilage decreases, amount of smooth muscle increases With less cartilaginous support, amount of tension in smooth muscle has greater effect on bronchial diameter and resistance to airflow o o o o o Bronchioles Tertiary bronchus branches within bronchopulmonary segment Forms many bronchioles Bronchioles branch into finest conduction branches Terminal bronchioles Bronchioles have no cartilage Smooth muscle tissue Pulmonary lobules Connective tissue of root of each lung extend into lung’s parenchyma Trabeculae (fibrous partitions) branch repeatedly, dividing lobes into smaller compartments Branches of conducting passageways, pulmonary vessels and nerves of lungs follow these trabeculae Finest partitions (interlobular septa) divide lung into pulmonary lobules Branches of pulmonary arteries, pulmonary veins, respiratory passageways supply each lobule Connective tissues of septa are continuous with those of visceral pleura Terminal bronchiole delivers air to single pulmonary lobule Within lobule, terminal bronchiole branches to form several respiratory bronchioles Thinnest Alveolar ducts and alveoli Respiratory bronchioles connected to individual alveoli and to multiple alveoli along alveolar ducts Alveolar ducts end at alveolar sacs (common chambers connected to multiple individual alveoli) Alveoli give lungs open, spongy appearance Each alveolus associated with extensive network of capillaries Pleura Two layers Visceral layer Seals lung surface Prevents leakage of air into thoracic cavity Parietal layer Thicker Lines inner surface of thoracic c 2. 3. 4. 5. Mechanics of pulmonary ventilation Muscles causing lung expansion and contraction Lungs expanded and contract in two ways: 1. Downward and upward movement of diaphragm 2. Elevation and depression of ribs Normal quiet breathing accomplished mostly by first method Inspiration: contraction of diaphragm pulls lower surfaces of lungs downward Expiration: diaphragm relaxes, elastic recoil of lungs, chest wall and abdominal structures compress lungs and expels air Heavy breathing Elastic forces not powerful enough to cause necessary rapid expiration Extra force achieved by contraction of abdominal muscles Pushes abdominal contents upward against bottom of diaphragm Compresses lungs Expanding lungs by raising rib cage In natural resting position Ribs slant downwards Allows sternum to fall backward toward vertebral column Rib cage is elevated, ribs project directly forward Sternum moves forward Away from spine Makes anteroposterior thickness of chest 20% greater during maximum inspiration than during expiration Muscles that elevate chest cage muscles of inspiration External intercostal Sternocleidomastoid muscle (lift up sternum) Anterior serrati (lift many of ribs) Scalene (life first two ribs) Muscles that depress chest cage muscles of expiration Abdominal recti (powerful effect of pulling downward on lower ribs at same that they and other abdominal muscles compress abdominal contents against diaphragm) Internal intercostals Movement of air in and out of lungs and pressure that cause movement Lung is elastic structure, collapses No attachment between lung and walls of chest case Only suspended at its hilum from mediastinum Lung floats in thoracic cavity Surrounded by pleural fluid Lubricates movement of lungs within cavity Continual suction of excess fluid into lymphatic channels Maintains slight suction between visceral surface of lung pleura and parietal pleural surface of thoracic cavity Pleural pressure and its changes during respiration Pleural pressure: pressure of fluid in thin space between lung pleura and chest wall pleura Slight suction negative pressure Normal pleural pressure at beginning of inspiration: -5cm water Amount of suction need to hold lungs open to their resting level During normal inspiration, expansion of chest cage pulls outward on lungs with greater force Creates more negative pressure -7,5cm water Alveolar pressure Pressure of air inside lung alveoli Glottis open no air flowing into or out of lungs Pressures in all parts of respiratory tree equal to atmospheric pressure (0cm water pressure) To cause inward flow of air into alveoli during inspiration Pressure in alveoli must fall to value slightly below atmospheric pressure Normally -1cm water Enough to pull 0,5l of air into lungs in 2 seconds required for normal quiet inspiration During expiration Alveolar pressure rise to +1cm of water Forces 0,5l of inspired air out of lungs during 2-3 seconds of expiration Transpulmonary pressure Difference between alveolar pressure and pleural pressure Pressure different between that in alveoli and that on outer surface of lungs Measure of elastic forces in lungs that tend to collapse the lungs at each instant of respiration Called recoil pressure Compliance of lungs Extend to which lungs will expand for each unit increase in transpulmonary pressure Total compliance of both lungs together in normal lung: 2ml of air per cm of water transpulmonary pressure Compliance diagram of lungs Relates lung volume changes to changes in transpulmonary pressure characteristics of compliance diagram determined by elastic forces of lungs 1. Elastic forces of lung tissue itself Determined by elastin and collagen fibres interwoven among lung parenchyma In deflated lungs: fibres elastically contracted In expanded lungs: fibres stretched, elongate and exert more elastic force 1. Elastic forces caused by surface tension of fluid that lines the inside wall of the alveoli and other lung air spaces Lungs filled with air interface between alveolar fluid and air in alveoli Transpleural pressures required to expand air-filled lungs are 3x as great as those required to expand saline solution-filled lungs No air-fluid interface Surface tension effect no present Only tissue elastic forces operative in saline-solution filled lungs Tissue elastic forces tending to cause collapse of air-filled lung represent only 1/3 of total lung elasticity, fluid-air surface tension forces in alveoli represent 2/3 Fluid-air surface tension elastic forces increase when surfactant not present 6. Typical versus atypical bacteria: include S. pneumoniae, Haemophilus influenzae, Staphylococcus aureus, group A streptococci and gram-negative bacteria e.g. Klebsiella pneumoniae. Atypical pneumonia refers to pneumonia caused by Legionella spp, Mycoplasma pneumoniae, Chlamydophila pneumoniae, and Chlamydophila psittaci. Typical organisms :Influenza viruses ,Parainfluenza viruses, Respiratory syncytial virus, Coronavirus e.g. SARS-CoV-2. Viruses In paediatrics: -Viruses are the commonest cause – RSV most common, parainfluenza, influenza, adenovirus, human metapneumovirus. -Streptococcus agalactiae, Listeria monocytogenes, Escherichia coli, Bordetella pertussis, Staphylococcus aureus 7. Hypersensitivity The basic pathophysiological reaction of hypersensitivity results from the interaction between antigen of endogenous or exogenous origin with specific antibody, cells or complement (immune effectors). These reactions, instead of protecting the individual, are associated with tissue damage or harm. Allergy is an immune-mediated reaction associated with tissue damage or harm caused by exposure to a particular foreign antigen (allergen), usually harmless. The reaction can be reproduced and is often more severe on repeat exposure 8. 10. a) i) Beta-2 agonits couse smooth muscle dilation, Bronchodilation, Vasodilation and Release of insulin. Types of beta-2 agonists - Short-acting beta-2 agonists Long-acting beta-2 agonists Ultra-long-acting beta-2 agonists Short-acting beta-2 agonists is rescue drugs because they are used to treat acute bronchospasm. E.G - Albuterol (Ventolin, Proventil) - Levalbuteral (Xopenex) - Metaproterenol (Alupent) Long-acting beta-2 agonists are maintenance medications because they are used to control and maintain conditions that cause chronic bronchospasm. Useful for maintaining patients with asthma and COPD who are not having an acute exacerbation. E.G - Arformoterol ( Brovana) - Salmeterol (Serevet) - Form ii) Inhaled β2-agonists and corticosteroids often used together in control of asthma - Corticosteroids increase gene transcription of β2 Corticosteroids protect against down-regulation of β2-receptors after long term administration - The airway smooth muscle has few adrenergic nerve fibres but many β2-receptors stimulation causes bronchodilation - Activation of β2-adrenoreceptors relaxes smooth muscle by increasing intracellular cAMP Activates kinase - Inhibits muscles contraction by phosphorylating and inhibiting myosin-light-chain kinase ) b) Compare the effectiveness and safety of inhaled versus oral corticosteroids. Why are oral corticosteroids are indicated in the acute treatment of severe asthma exacerbations and inhaled steroids preferred for chronic maintenance treatment? - Inhaled steroids are usually effective in 3-7 days hence oral corticosteroids may be indicated in severe asthma exacerbations - Oral administration is associated with many serious adverse effects hence not indicated for long term effects - Low bioavailability of active drug in inhaled corticosteroids - - - c)Controllers act by providing long-acting bronchodilation and/or have anti-inflammatory action prevent/diminish inflammatory process and its increase in airway hyper-reactivity some mediations are primarily directed at underlying inflammatory mechanism of asthma that leads to chronic symptoms and possible permanent lung damage corticosteroid asthma medications are probably most effect controller treatments block or suppress most aspects of inflammation in all individuals inhaled or oral corticosteroids also mast cell stabilizers controller medications are used on daily basis for long-term control of chronic asthma take even when you have no symptoms not effect in treatment of acute symptoms Importance of adherence It is very important to adhere to medication and use the controllers and relievers appropriately Overuse of relievers (more potent drugs) leads to over medication and possible death If one uses a controller instead of a reliever there is a chance of death or hospital admittance because they do not relieve acute symptoms If one does not adhere to the controller: There will be chronic inflammation leas to possible permanent lung damage The asthma is poorly controlled and leads to repeated, increasingly severe acute asthma attacks 14. Definition: large-scale grouping of people who share common economic resources which strongly influence types of lifestyles they are able to leader - - Ownership of wealth with occupation are bases of class differences Upper class – wealthy, employers, industrialists, top executives (those who own or directly control productive resources) Middle class – white-collar workers and professionals Working class – blue collar or manual jobs Peasants – people engaged in traditional types of agricultural production, largest class in third world countries Class determines what opportunities one has access too People in lower class often cannot get opportunities to access health care They may not be able to afford They may not be able to get time off work to access health care Health professionals may not explain things properly because the health professional believes they are uneducated 3. 4.Prevention • Bacillus Calmette–Guérin (BCG) vaccine • Live, attenuated strain of M. bovis • Given intradermally at birth • Variable success • Probably reduces disseminated TB and TB meningitis • Can cause “BCGitis” • Antiretrovirals • Improve patient’s immune status • Population-level effect of reducing TB incidence • Undiagnosed TB can be uncovered by the immune reconstitution inflammatory syndrome (TB-IRIS) • Treated TB can also worsen (“paradoxical” TB-IRIS) Prevention • INH preventive therapy • For latent TB • Prevents progression to active TB • Indicated for children with close household contacts • Still under consideration for people living with HIV (PLHIV) • Usually, INH for 6-9 months • Improvement of socio-economic conditions / health inequalities • Poor living conditions • Overcrowding • Undernutrition • HIV Tuberculin skin test (Mantoux) • Purified protein derivative (PPD) of MTB is injected intradermally • Test for latent TB • Skin surface is monitored for reaction over 3 days • Reaction represents immune response to PPD, • The size of the reaction determines positivity • Used primarily in paediatrics in high burden areas Epidemiology • In 2019, an estimated 10 million people fell ill with TB worldwide • A total of 1.4 million people died from TB in 2019 worldwide • The estimated prevalence of TB (all ages, all forms) in South Africa in 2018 was 737 per 100,000 population • It is estimated that about 80% of the population of South Africa is infected with TB bacteria (latent TB) • In 2019 a total of 58,000 people died of TB in South Africa Molecular diagnosis • GeneXpert (Xpert MTB/RIF Ultra) • Widely implemented in South Africa • First line testing for all pulmonary samples • Decentralised testing through National Health Laboratory Service (NHLS) • Has replaced sputum microscopy • Also WHO-recommended for certain extrapulmonary samples • Line probe assay • Highly technical PCR assay to detect resistance to rifampicin, INH and fluoroquinolones • There are other molecular tests available or in development Molecular diagnosis • GeneXpert platform • Xpert MTB/RIF Ultra • Cartridge based real-time PCR • Detects MTB and rifampicin-resistance (rpoB mutations) • Advantage • More sensitive than acid-fast stain microscopy • Rapid turnaround time ( Lymph Node Gartner: Textbook of Histology Lymph Node functions • Filtration of lymph (non-specific) Removal of particulate matter and microorganisms • Interaction T-Lymphocytes with antigen Involves uptake of antigen by APC • Aggregation and proliferation of lymphocytes Both B- and T-lymphocytes • Activation of lymphocytes Antibody secretion (B-cells) and T-cell-mediated response Histological Structure of the Lymph Node Histologically, a lymph node is divided into three regions: Cortex, Paracortex, and Medulla. Subcapsular sinus Para trabecular sinus Cortex Paracortex Medulla Medullary cords (consist mainly of lymphocytes, macrophages, and plasma cells Medullary sinuses T cell rich Macrophages Dendritic cells High endothelial venules B cell rich B-cell rich follicles Macrophages Dendritic cells Follicular dendritic cells Macrophages Dendritic cells (Stevens and Lowe: Human histology) Lymphoid Follicle Germinal centre (Pale zone) Mantle /Corona (facing the cortex) • Primary follicles (lacks a mantle and germinal centre -non-active) • Secondary follicles (active, with mantle and germinal centre) Dark zone (EL ad Merwe) (Kerr: Functional Histology) Secondary Follicle structure: Histophysiology Mantle Zone (B cells not specific for antigen) Germinal centre contains: •Follicular Dendritic Cells •Macrophages (phagocytose apoptotic B cells) Mitotic and developing B cells Dark Zone: Antigen activation of B cells – differentiate & clonal expansion Parafollicular helper T cells (CD4+) activate B cells to proliferate Mature B cells with high affinity surface IgG determined by FDCs migrate to medulla & become plasma cells – secrete IgG & IgM into lymph. Lymph Circulation through Lymph Node (Wheatear’s: Functional Histology) Afferent lymphatic vessels pierce the capsule and open into the subcapsular sinus Para trabecular sinus arise from the subcapsular sinus and penetrate the cortex and continue into the medulla as branching medullary sinuses surrounded by medullary cords Palatine tonsils Separated from underlying tissue by a fibrous hemi capsule The luminal surface lined by a stratified squamous epithelium Parenchyma contains lymphoid follicles with germinal centres The Thymus Gland • Maturation of immunocompetent T-Lymphocytes Immature T-Lymphocytes derived from bone marrow • Proliferation of mature T-Lymphocytes Supplies the circulating lymphocyte pool • Development of immunological self-tolerance Elimination of self-reactive lymphocytes • Hormone secretion Thymulin, thymopoietin, thymosin: regulate T-cell maturation and lymphoid tissue development • During fetal development: haematopoiesis Kierszenbaum & Tres: Histology and Cell Biology Structure of the Thymus Gland 2 lobes, several “incomplete” lobules Structure of the Thymus Gland • T lymphocytes (thymocytes) • Macrophages • Dendritic cells • Subscapular Thymic epithelial cells • Cortical Thymic epithelial cells • Blood vessels • HEV’s • Blood–thymus barrier Cortex (several distinct lobules) Medulla (shared) • Immunocompetent T cells • Macrophages • Dendritic cells • Small population of B cells • Medullary Thymic epithelial cells • Hassall’s corpuscle Kierszenbaum & Tres: Histology and Cell Biology Cortex: The BloodThymus Barrier Kierszenbaum & Tres: Histology and Cell Biology • Consists of the cTEC, dual-basal lamina and endothelial cells = Blood–thymus barrier • Function: Prevent cTEC from interacting with foreign macromolecules - shield developing thymocytes from exposure to antigens. • Auto-immune reaction T cell maturation 1 2 3 Proliferation double negative T cells Maturing double positive T cells (CD4+ & CD8+) become responsive to MHC class I & II MHC II needed for CD4 MHC I needed for CD8 Cells that recognise self MHC (not self antigens) allowed to mature to single positive cells (CD4+ OR CD8+) – Positive selection 4 Kierszenbaum & Tres: Histology and Cell Biology Cells recognising self MHC & self antigens – apoptosis – Negative selection Hassal’s corpuscles - Whorls of thymic epithelial cells Thymic medulla Kierszenbaum & Tres: Histology and Cell Biology Capillaries that enter the medulla from the cortex at the corticomedullary junction drain into postcapillary venules The venules are more permeable than are capillaries in the cortex, and the medulla has no blood-thymus barrier. Lymphocytes that proliferate in the cortex enter by passing through walls of these vessels. Central hyaline core that is eosinophilic and may show signs of keratinization. Their function is not well understood, but they express the cytokine thymic stromal thymopoietin, which instructs dendritic cells in the human thymus to induce CD4 + regulatory T cell development. They may also play a role in removing apoptotic thymocytes. 1) Lymphocytes enter the thymus from blood vessels in the stroma. 2) Thymocytes enter the cortex. 3) Thymocytes interact with cortical thymic epithelial cells (cTECs) (positive selection for functional MHC binding). 4) Thymocytes that are positively selected pass to the medulla where they interact with medullary epithelial cells (mTECs) and dendritic cells which negatively select cells that bind to self-antigens. 5) T cells leave the medulla to enter blood vessels in the stroma. 6) T cells of different types now migrate to secondary lymphoid organs. Lymphocyte Development in the Thymus Nurse cells Stevens&Lowe: Human Histology The Spleen (Ross et al.) • Mounts immune response to bloodborne antigens • Filters particles and old/defective blood cells from circulation • Fetal development: haemopoiesis Structure of the Spleen Support tissue: - Contains collagen, elastic fibers and smooth muscle cells - Derived from capsule - Contain trabecula arteries and veins https://www.amboss.com/us/knowledge/Spleen Kierszenbaum & Tres: Histology and Cell Biology Cellular components within capsule make up pulp Red pulp contains many red blood cells (no.6 in the image) White pulp resembles lymphoid nodules (no.5 in the image) Structure of the Spleen Kierszenbaum & Tres: Histology and Cell Biology https://www.amboss.com/us/knowledge/Spleen White Pulp Each central arteriole is surrounded by lymphatic tissue calledy PALS (25%) White Pulp: Splenic nodules T cells, B cells, antigen presenting cells & plasma cells “Central Arteriole” Periarteriolar lymphoid sheath (PALS) T cells B cell Corona Germinal centre (EL vd Merwe) Arborizing arteries, surrounded by aggregates of lymphoid tissue (lymphoid sheaths, c. 20% of total spleen mass) Red Pulp https://www.amboss.com/us/knowledge/Spleen 70% of the red pulp is composed of parenchyma and 30% is venous sinuses/sinusoids Sinusoids are surrounded by reticular fibers Sinusoids drain into the splenic vein Red Pulp • Blood filled venous splenic sinusoids – lined by rod-shaped endothelial cells; surrounded by macrophages, plasma cells and reticular fibers • Splenic cords (Cords of Billroth) - separate splenic sinusoids; contain plasma cells, macrophages and blood cells - all supported by a stroma of reticular cells and fibers. • Macrophage-sheathed capillaries – Function: remove aged cells and particulates from blood Function: Blood filtration Kierszenbaum & Tres: Histology and Cell Biology Red Pulp The macrophage-sheathed capillaries drain into the splenic sinusoids (closed circulation; non-human) or into the stroma of the red pulp (open circulation; human) Splenic sinusoids are drained by collecting veins, to trabecular veins, to splenic veins. Kierszenbaum & Tres: Histology and Cell Biology (1) Antigens enter the spleen from blood. Blood flows into spleen through splenic artery and enters central arteriole and marginal channel (2) Antigenpresenting cells detect bloodborne antigens or pathogens present in the red pulp and are sampled by PALS-derived T cells (3) T cells interact with B cells and from this interaction B cells proliferate and differentiate into Plasma cells (4) Plasma cells release immunoglobins into the red pulp and blood circulation to trap specific antigens in the blood (5) Lymphocytes, macrophages and dendritic cells repopulate the white pulp through the marginal channel White Pulp Kierszenbaum & Tres: Histology and Cell Biology Red Pulp: Blood filtering (4) Blood from central arteriole is transported into penicillar arteriole which ends in macrophage-sheathed capillaries (5) Macrophage-sheathed capillaries drain into splenic sinusoids or stroma of the red pulp Kierszenbaum & Tres: Histology and Cell Biology Splenic Circulation • Blood filtration (red pulp) Blood flows through central arteriole, penicillary arteries and sheathed capillaries; extravasate, percolation through splenic cords, enter splenic sinuses/veins. Phagocytic cells remove debris • Interaction with antigen (white pulp) Blood passes through central and radial arterioles into marginal channel; extensive contact with APC, antigen presentation to lymphoid cells A 14-year-old young girl named Cindy Parker lives with her mother, father, sister, and grandmother. It is a low social class family. Their residential property has carpets and curtains which can accommodate a lot of house dust mites. They also own a cat which is a fur pet. Cindy is currently doing grade 9 but nearly did not make it out of grade 8 due to asthma attacking her respiratory system. She passes out sometimes and cannot participate in some of the activities done by other school kids. There is a boy that charms her in class and often misses spending with him. She got a ‘cold’ and started coughing out yellow sputum. Her grandmother believes the cold weather causes chest symptoms to her granddaughter. Her mother believes if they were wealthy, her daughter would not have been so ill. Cindy’s cousin has both eczema and asthma. The doctor did many tests and examination on Cindy including chest x-ray, then told her family a proper way of using inhalers together with space device. The doctor also told the family how to stay away or minimize triggers that may cause exacerbations. There is prove that changes of the world’s climate affect the health of people, with the poor being mostly affected than the rich (2022). The reason being that the rich have adequate shelter when there are world disasters such as earthquakes, tsunamis, cyclones, or extreme cold and hot temperatures. The poor are helpless, even a small disaster can leave them homeless and take a lot of time to recover. Lower class individuals live in shanty houses which can be very hot in hot weathers and very cold in cold weathers. Geography also says the numbers of suicides peaks in extreme high temperature seasons. A combination of stress developed from frustration and drastic temperatures can be deadly due to dehydration and respiratory complications (2022). Cindy and her family live in a breaking new ground built by the government, it is better than a shark but does not provide enough shelter to harsh weather conditions. In cold weather it is much colder which is a trigger for asthma attack, hence Cindy experiences chest symptoms. Environmental pollution is fatal to people especially young children as it can cause irreversible respiratory injuries (2022). Air pollution can cause contractive pulmonary diseases such as empyema and chronic bronchitis. Pregnant women who are exposed to harmful substances can increase chances of congenital diseases to the new-born babies (2022), some toxic substances can limit blood flow/oxygen supply to the foetus leading to a lot of health problems. Harmful substances can also be found in the food we consume and water drink (2022) such as lead and fluoride. Second hand tobacco smoke is also believed to increase the prevalence of asthma and COPD, thus women who are expecting and children must be protected from it (2022). The government should provide clean fuel for heating and cooking, remove pests and dangerous building materials including lead paint. Promote good health and public hygiene, free from noise and pollution. Provide safe water and sanitation (2022). The home of Cyndy has a cat which produces urine and saliva that has proteins that can cause allergic reactions to human Cindy is struggling to spend time with loved one. She is concerned about the effect of asthma medication to contraceptives and the other way around. She wants to be involved in sexual activities, but her condition serves as a barrier. Everyone has the right to equality and non-discrimination rights The right to be free of torture and other brutal, humiliating, or degrading treatment or punishment. A person's right to privacy. The right to the best possible health (including sexual health), as well as social security. The right to marry, start a family, and enter into marriage with the free and complete agreement of the intended spouses, as well as equality in and after divorce. The right to choose how many children to have and how far apart they should be (2022). Sexual health is not only the lack of sickness, malfunction, or infirmity regarding sexuality; it is a condition of physical, emotional, mental, and social well-being. Sexual health necessitates a positive and respectful attitude toward sexuality and sexual relationships, as well as the ability to have joyful and safe sexual encounters devoid of compulsion, prejudice, and violence. To achieve and sustain sexual health, all people's sexual rights must be acknowledged, safeguarded, and satisfied (2022). Sex, gender identities and roles, sexual preference, sexiness, pleasure, intimacy, and reproduction are all important aspects of being human throughout life. Thoughts, fantasies, wants, beliefs, attitudes, values, behaviours, practices, roles, and relationships are all ways in which sexuality is experienced and expressed. While all of these qualities may be found in sexuality, not all of them are always experienced or expressed. The combination of biological, psychological, social, economic, political, cultural, legal, historical, religious, and spiritual variables has an impact on sexuality. Peter Viljoen is a 22-year-old boy whom studies MBChB at the University of Cape Town. He is takes good care of himself and well fit for his age. Peter does pay the price of being a medical student through effort and dedication to his academics. He stays at a UCT residence. Being a senior student, he shares a room with no one except himself. He shares the bathrooms and toilets with other students in the resident. He repeatedly washes his face with liquid that prevent growth of microbes. He recently developed a pimple on his face which made decided to visit Student Wellness Centre to get help. He developed a lot of stress as his final examination was about to begin. The pimple became larger and more painful, which made him start to think people are avoiding him adding to the fact that another student made unkind remark about sharing ablution facilities with him. On examination his vital signs were normal, and the lesion was assessed to be a boil. Further investigations and tests where done, treatment options were given to him by a doctor. I am going to relate Peter Viljoen case with intersectionality and race. Looking influence of skin colour on lives of people. I am going to also to talk about how much harm discrimination can cause in victim’s lives, especially Black women. The other student making unkind remark about Peter skin did not make him feel good. Anyone can get a pimple anytime and should not be punished for that as the person did not request it. People judged because of the skin anytime which is something beyond their control. Skin colour plays a big role in terms of skin discrimination. Some people are classified as black and some as white. Black is defined as anyone with black ancestry of four generations (DJ,2022). In south Africa, apartheid which is an Afrikaans term for apartness made a huge impact from 1948 to 1994. One can be argued that it still exists even today. People were put into racial categories whites, coloureds, Indians and lastly Bantu which means Black Africans (DJ,2022). There was a lot of inequalities among the groups including health inequalities. This resulted in poor education, poor sanitation, lack of nutritious food, and poverty (DJ,2022). Many countries still require citizens to declare their race official documents, while others such as Netherlands do not entertain that (DJ,2022). There is a single human race, which means all of us are the same regardless of skin colour. According to genetics 99,9% of DNA (Deoxyribonucleic acid) matches in all humans matches (DJ,2022), which means we only differ by 0.1%. It is hard to believe as we all look different and have different sex. Africa has more genetic mutations than any other continent. It is also believed that the first women lived in South Africa according to genetic studies. People with different skins experiences life in different ways, some do not need to worry about their skin while some are constantly wishing they had a different skin. Peter also starts to have a different experience at the University of Cape Town. His skin has caused him discrimination. This is apparent with black woman who get to be discriminated about both their sex and race, while white women get to be discriminated of sex (2022). Race discrimination has affected Black woman their social support from other people, loneliness, marriage status, social disruption, environment at work, social status, and social intersectionality (2020). Black women suffer a lot to get a job which leads to them doing sex work to feed their families. There are more black sex workers than any other race. They have unprotected sex with many men every day. This increases the number of HIV infections among the Black woman community. Many do not have access to proper health care which in higher HIV mortality among Black women community. Some have access to healthcare but are afraid of being discriminated against and end up passing away. Blacker women commit suicide more than any other race. Poverty sets in, as the bread winners pass away. The Black woman who are in positions of power are mocked and discriminated on every action they take. They are judged on things that if it was a man doing it, there would not be any problem. They must always be ready for an attack from any angle. They are abused by their partners, or even worse murdered. They are taken advantage of by everyone who wishes to. Peter is also ready for being mocked by the students he shares bathrooms with, it is something that skips his mind every time. There is no intersectionality between him and other students. He is seen in a different eye and treated differently, even though he did nothing wrong. It is possible for him to not want to share the bathrooms anymore, which means he will suffer when he wants to go to the bathrooms. It is possible he no longer enjoys bathing as he does not feel welcome to do so. I believe it would have been even worse if he was a female. He would probably suffer a more severe stress. The other students should understand that it is beyond his control and live with him like the used to. This is a difficult thing for them as they also do not want to be like him and only trying to defend themselves from what infected Peter’s skin. People are treated differently according to their appearance. It is started long time ago and it still occurs today. People are not only discriminated about their colour but also lesions that may occur on their skin. The discrimination can come from something you are born with or something you develop as you get old. There are fortunate ones that get less discrimination as compared to others. It is very important for everyone to understand intersectionality to reduce or completely wipe off discrimination. There are people who discriminate others to protect themselves and there are others who discriminate out of being judgemental. In the case of Peter, students discriminated him to avoid being like him. Discrimination can cause more harm to people than we can think. It can lead to increase in mortality, spread of diseases such as HIV, generational poverty…etc. Granuloma • A localised collection of epithelioid macrophages TB granulomas • Collection of epithelioid macrophages • Often shows central caseous necrosis • Langhans type giant cells • Rim of surrounding lymphocytes • Rim of surrounding fibroblasts PRIMARY PULMONARY TB • Usually in childhood • Primary Gohn Complex • A pulmonary Gohn focus • 1-2cm area of casesous necrosis • Subpleural at upper part of lower lobe or lower part of upper lobe • Regional lymphadenopathy • Necrotising granulomas in hilar and paratracheal lymph nodes POST-PRIMARY / SECONDARY TUBERCULOSIS • Follows reactivation of dormant / walled off bacilli from previous infection • Bacilli dormant in areas of high oxygen tension • Apex of the lung • OR • Reinfection of a person who has had a previous infection • Second or multiple episodes of TB • ↓ immunity or overwhelming infection • Extensive caseation and cavity formation • Usually apex of upper lobes (one or both lungs) • Less regional lymph nodes involvement compared to primary TB Isoniazid (INH) M.O.A: Inhibit mycolic acid synthesis Toxicity: Peripheral neuropathy Hepatitis Pharmacokinetics: Penetrates tissues well Acetylation Rifampicin M.O.A: Inhibits RNA Polymerase Toxicity: Hepatitis Hypersensitivity Pharmacokinetics: Variable bioavailability Induces metabolism Pyrazinamide M.O.A: Non-specific Toxicity: Hepatitis Gout Hypersensitivity Pharmacokinetics: Penetrates tissues well Active at low pH Ethambutol M.O.A: Inhibits arabinogalactan Toxicity: Retrobulbar neuritis Pharmacokinetics: Poor CNS penetration Renal elimination 80% Pathophysiology of Pneumonia A. Description: Acute infection of the lung varying in severity and causing fluid accumulation. B. Aetiology: causative organisms include bacteria, viruses, fungi, and protozoan. C. Pathophysiologic process and manifestations. 1. Organisms may enter the respiratory tract through inspiration or aspiration of oral secretions; staphylococcus and Gram-negative bacilli may reach the lungs through circulation in the bloodstream. 2. Normal pulmonary defence mechanisms (cough reflex, mucocilliary transport, and pulmonary macrophages) usually protect against infection. However, in susceptible hosts, these defences are either suppressed or overwhelmed by the invading organism. 3. The invading organism multiplies and releases damaging toxins, causing inflammation and oedema of the lung parenchyma; this results in accumulation of cellular debris and exudates. 4. Lung tissue fills with exudates and fluid, changing from an airless state to consolidated state. 5. In viral pneumonia, the ciliated epithelial cells become damaged. 6. Severity of symptoms depends on the extent of pneumonia present (e.g., partial lobe, full lobe [lobar pneumonia], or diffuse [broncho pneumonia]). 7. Symptoms include: I. Fever ii. Chills iii. Malaise iv. Cough v. Pleuritic pain vi. Increased tactile fremitus on palpitation vii. Rales and ronchi on auscultation viii. Dyspnoea