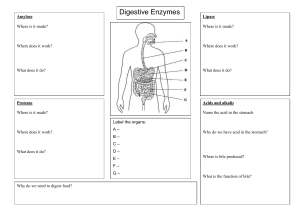
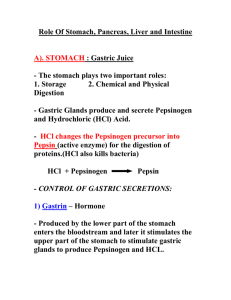
GASTROINTESTINAL DISORDERS DIGESTIVE TRACT → AKA alimentary canal → Starts in the mouth • Mechanical digestion (mastication/chewing) • Chemical digestion (salivary amylase to break down starch into sugar) o Mechanical and Chemical Digestion is inversely proportional ▪ ↓chew = ↑HCL ▪ ↑chew = ↓HCl → Upon swallowing, food reaches the esophagus • Dysphagia → Lower Esophageal Sphincter/Cardiac Sphincter • Ensures downward and prevents reflux, regurgitation • GERD → LES closes once food reaches the stomach • Stomach can be divided into two: o Fundus - upper portion o Antrum - lower portion ▪ Antrectomy - removal of the distal portion of the stomach • Stomach has parietal cells which produces HCl to dilute food and intrinsic factor which absorbs vit b 12 o Pernicious anemia if intrinsic factor became dysfunctional o HCl is acidic (ph 1.5 - 3.5) → Pyloric Sphincter opens around 2-3 hours (gastric emptying) • But depends on the content of food: o Fastest to digest: carbohydrates o Fats and proteins stays longer in the stomach → Small Intestine • Duodenum connected to the hepatobiliary tract o Pancreas → pancreatic enzymes ▪ Amylase → breaks down carbohydrates ▪ Lipase → breaks down fats ▪ Trypsin → breaks down protein o Liver → produces bile (stomach contents that would enter the small intestine should be water soluble → fats are needed to be emulsified (to go along with the water) → bile would be the emulsifier) o Gallbladder → storage of bile • Jejunum absorbs nutrients • Ileum absorbs bile salt and vitamin b12 o ↓absorption of bile salt → steatorrhea (foul smelling) → stool will be more dense (lumulutang) o Resection of the ileum → dec vit b12 absorption → pernicious anemia → Large Intestine absorbs water and formation of stool or feces • Peristalsis (movement of the colon) o Is directly proportional with bowel sounds ▪ ↑peristalsis → ↑bowel sound → irritation of the intestine → diarrhea ▪ ↓peristalsis → ↓bowel sound → constipation ▪ (+) pain → decreased peristalsis o Is indirectly proportional with absorption of water ▪ ↑peristalsis → ↓absorption of water → stool will be wet (diarrhea) ▪ ↓peristalsis → ↑ absorption of water → stool will be dry (constipation) o Immobility will cause decrease peristalsis resulting to constipation ▪ Advice the patient to exercise to increase peristalsis • Ascending Colon • Transverse Colon • Descending • • • Sigmoid Rectum (vascular) o If high risk for bleeding → invasive procedures are contraindicated Anus (opening) Quadrants → Pancreatitis - LUQ → Liver and gallbladder - RUQ → Appen - RLQ → Rectum - LLQ → Sigmoid - LLQ Assessment: → IAPePa → To get an accurate assessment on bowel sounds auscultation is done first → any pressure to the abdomen will cause changes/alter to the peristalsis or bowel sounds GASTROESOPHAGEAL REFLUX DISEASE (GERD) → Weak LES • Anything that may decrease LES pressure, inc HCl • Substances to Avoid: (5CAFPS) o Coffee o Citrus Fruits o Cigarette Smoking o Carbonated Drinks/Cola o Chocolate o Alcohol o Fatty foods o Peppermint o Spicy → Backflow, regurgitation, and reflux of gastric contents into the esophagus → Signs and Symptoms: • Pyrosis (heartburn) burning sensation after eating • Nausea and Vomiting + Hypersalivation • Dyspepsia or Indigestion • Dysphagia (difficulty swallowing) • Injury because esophagus has no mucosal layer → Odynophagia → Management: • “Food should go down” • High carbs, low fat, low protein diet • High fiber diet → increase feeling of fullness (satiety) → prevents overeating • Small frequent feeding • Position: Upright → elevate HOB and turned to left → esophagus will be above → food will not regurgitate • Avoid anything that may increase pressure in the abdomen o Do not bend after eating o Do not wear tight clothing o Avoid heavy lifting o (X) Obesity → Medication: • Avoid medications that increases HCl o E.g. NSAIDS, Aspirin • Antacids • Proton Pump Inhibitor • Histamine 2 blocker • Prokinetics (meds to increase motility) for food to descend o Metoclopramide • Antiemetics → Fundoplication • Fundus is wrapped around the LES → Diagnostics → Endoscopy → Checking of gastric pH PEPTIC ULCER DISEASE Causes: 1. Helicobacter pylori → from raw meat → burrows in the GIT → causes ulceration • DOC: Metronidazole o Should not be mixed with alcohol → disulfiram like effect/reaction 2. ↑HCl and ↑Pepsin 3. ↓mucus → ↓protection • Burn injury → fluid shifting → edema → dec blood volume → dec blood flow to the stomach → less production of mucus → curling’s ulcer → Related to low food intake Career stage Malnourished (weight loss) Well nourished → → → → Pain - ½ - 1 hour after meal (with food) Pain is triggered by food intake Pain relieved by vomiting (pressure is relieved) Nausea, vomiting and hematemesis Pathophysiology: → → → Pain - 2-3 hours after meal (empty) Pain is relieved by food intake Pain is common at night (empty) Melena Management: → Monitor for signs of bleeding → Anything that can cause perforation or rupture → peritonitis (compilation) → Signs and symptoms: • Board like and rigid abdomen → Diet: • Avoid milk → causes hyperacidity o Milk can also increase ph → alkaline → stomach will try to return acidity of the stomach by ↑HCl • Small frequent feeding • Chew food properly • Foods as tolerated; not bland → Avoid risk factors → Stress reduction • Any form of rest/relaxation → Vagotomy: (X) vagus nerve → low production of HCl (decrease stimulus for the production of HCL) → Histamine 2 blocker → (x) proton pump → ↓hcl production → Proton pump inhibitor → ↓HCL production → Octeroride → mimics the action of somatostatin → ↓gastrin → ↓histamine → ↓HCl Factors: → Stress • ↑acetylcholine → ↑HCl → Cigarette Smoking → Alcohol → Caffeine → Aspirin and NSAID • ↑HCL → Zollinger - Ellison Syndrome • Pancreatic tumor → ↑gastrin → ↑HCl → Irregular and Hurried Meals • Dec chewing → ↑HCl → Type A personality • Workaholic → prone to stress → Type O blood • ↑pepsin level → Genetics • ↑parietal cells → ↑HCl non GASTRIC ULCER DUODENAL CANCER Poor Man’s or Laborer’s Ulcer → Related to low food intake Executive Ulcer → Related to stress 20% incidence 80% incidence Common in people 50 yrs old and above Common in people 25-50 yrs old Medications: → Antacids • Neutralizes acid • Taken 1-2 hrs after meal • If empty stomach → longer duration • Aluminum Hydroxide (phosphate binder for hyperphosphatemia) o To be taken with meals o WOF: constipation • Magnesium Hydroxide o WOF: Diarrhea • Aluminum Magnesium hydroxide • Calcium Carbonate • Sodium Bicarbonate o Can cause metabolic alkalosis o Can enter bloodstream → Histamine 2 receptor blockers • Ranitidine • Taken at bedtime → Proton Pump Inhibitors • Omeprazole • Taken before meals → Cytoprotective Drugs • Sucralfate • Coats the stomach; acts a protective barrier → Prostaglandins • Misoprostol • Dec HCl, ↑mucus, for inflammation, induces uterine contraction • Contraindicated to pregnant → abortifacient → Hormone • Octreotide • Increases somatostatin The cause of peptic ulcer is NSAIDS, which medications will you give? A. Histamine 2 receptor blocker B. Proton Pump Inhibitor C. Cytoprotective Drugs D. Prostaglandin ● NSAID is an anti-inflammatory → antiprostaglandin ● WOF: pregnant, do not give Misoprostol Surgery: 1. Vagotomy • To dec stimuli for the production of HCl 2. Gastrectomy • Before imperforation happens / removal of parietal cells • Total - usually done on gastric cancer • Subtotal/Antrectomy - removal of the lower half of the stomach 3. Anastomosis: • Billroth I - gastroduodenostomy o Reconnect the stomach to the duodenum • Billroth II - gastrojejunostomy o Done If the damage in the duodenum is extensive o Rapid gastric emptying → dumping syndrome DUMPING SYNDROME • Chronic constipation with episodes of diarrhea Management: (Diverticulosis) 1. High fiber Diet 2. Increase fluid intake to counter constipation 3. Medication: Laxative to move bowel Acute Phase: “painful episodes” (priority is to rest the bowel) → dec peristalsis (Diverticulitis) → Low fiber diet → Oral Intake • Patient will be placed on NPO status → Activity • Bed rest → Medication • Antispasmodic/Anticholinergic • Propantheline → Monitor for perforation • Complication: Peritonitis APPENDICITIS → Appendix is found on the cecum → Where fecalith could be dislodged d/t irregular bowel pattern → obstruction → injury → necrosis → infection → inflammation sets in → inc peristalsis → rupture (sudden disappearance of pain) → peritonitis (diffused pain) → Management: (To dec peristalsis) • NPO status • IV fluids • Bed rest • Avoid enema, hot application, laxatives • Position: dorsal recumbent, knees flexed • Appendectomy: o If the patient will cough, instruct them to splint to prevent dehiscence or evisceration ▪ Cover with gauze soaked with NSS → Clinical Manifestations • McBurney’s Point – RLQ Management: → Food should stay in the stomach 1. Diet o High fat, high protein, low carb o Small frequent feedings o Avoid fluids during meals ▪ Should be in between meals o Avoid salt, sugar and milk 2. Position: o Supine o Left Side Lying → food will be pulled in the stomach → will not descend immediately DIVERTICULOSIS → Asymptomatic → Outpouching of intestinal mucosa → Common site: Sigmoid Colon → Cause: low fiber diet → constipation • Reversible through dietary modifications → ↑pressure in the intraluminal/wall of the colon → weakening of the wall of the colon → outpouching → trapping of stool → obstruction → injury → infection → inflammation DIVERTICULITIS → Inflammation/infection of 1 or more diverticula → Cause: Accumulation of fecal material Manifestations: 1. Inflammation • Abdominal pain in the LLQ (anatomical position of the sigmoid) • Crampy pain 2. Infection → Fever 3. Injury → blood in stool 4. Obstruction (d/t accumulation of gas in the colon) • Bloating and flatulence • • • • • • • Rovsing’s Sign o Pain elicited in the right lower quadrant when pressure is applied on the left lower quadrant Dunphy’s Sign o Pain is triggered when coughing d/t inc intraabdominal pressure Blumberg’s Sign o Rebound tenderness → pain is felt upon release Inc WBC Bowel Sound o Decreased or absent Psoas’ Sign o Left-side lying while the right leg is flexed backward → triggers pain because iliopsoas stretches and hits the appendix Obturator Sign o Supine position while knees are flexed at 90 degrees → obturator muscle will hit the appendix → triggering pain LIVER CIRRHOSIS → d/t repeated injury to the hepatocytes (basic functioning unit of the liver) → fibrosis (scar tissues) → loss of function • Loss of liver function d/t scarring Types: → Laennec’s Cirrhosis • Alcoholic cirrhosis (d/t alcohol) → Post necrotic • Caused by hepavirus or hepatotoxins (found in analgesics) → Biliary Cirrhosis • d/t obstruction/blockage of gallstones/cholelithiasis → Cardiac Cirrhosis • Right sided heart failure Liver Functions → Metabolism of nutrients (breakdown/processing of proteins, fats, etc.,) → Kupffer cell → swallow/engulf/trap microorganisms (phagocytosis; part of immunity) → Excretion of hormones: • Glucocorticoids (cortisol; sugar) • Mineralocorticoids (aldosterone; potassium, sodium and water) • Androgen (testosterone and estrogen) o Estrogen is a vasodilator → Breakdown of hemoglobin • Heme - iron; globin - protein • Iron → bilirubin → enter the liver → mixed with bile (for emulsification of fats) → fats are for absorption of vit ADEK → vitamin K (clotting factor) o Bile ▪ GIT → urobilin → urine ▪ stercobilin → color of the stool → If the liver is not functioning: • Bilirubin will be retained in the blood → accumulation in the skin → jaundice/icterus → pruritus o Warm bath o Cool environment o Oatmeal bath • Kidneys → dark urine • (X) bile → fats will enter the stools → steatorrhea • (X) clotting → high risk for bleeding o Bleeding precautions: ▪ Use of electric razor ▪ Soft bristled toothbrush ▪ Avoid dental floss ▪ Avoid anticoagulants • (x) urobilin or stercobilin → clay/pale colored stool Clinical Manifestations → ↓metabolism → anorexia & decreased body weight • High caloric intake (↑carbs & ↑protein) • Bed rest → (X) Kupffer cell → low immunity → high risk for infection • Aseptic technique • Handwashing → (X) excretion of hormones → retention of hormones resulting to ↑GMA • ↑cortisol → ↑sugar o Monitor blood glucose level o (X) gluconeogenesis → dec blood glucose level • Retention of sodium and water → edema o Sodium and water restriction • Low potassium o Spironolactone (potassium sparing diuretics) • ↑androgens: o Female: hirsutism, amenorrhea o Male: gynecomastia, atrophy of the genitals ↑vasodilation ❖ Palmar erythema ❖ Spider angioma/telangiectasia o Therapeutic communication d/t altered body image → Heart gives blood supply to the kidneys through renal arteries → heart gives blood to the GIT → portal vein → liver → filters blood → blood goes back to the heart through IVC ▪ → Liver produces albumin (most abundant protein) → maintains oncotic/osmotic pressure → attracts water going into the intravascular space while hydrostatic pressure draws fluid out → if liver is damaged → ↓albumin → ↓oncotic pressure → fluids will go out → edema → ↓fluids in the intravascular space → RAAS activate → ↑aldosterone and ADH → worsen edema → Excrete waste product of protein • Ammonia → goes to liver to be converted into urea → once combined with blood it will be converted into BUN (blood urea nitrogen) → excreted by the kidneys • If the liver is damaged → ammonia will accumulate and is neurotoxic → resulting in hepatic encephalopathy (fatal; brain damage) → Hepatic encephalopathy • Asterixis (flapping hand tremor) • Changes in LOC • Constructional apraxia (hindi magaya yung drawing/sinulat) • Fetor hepaticus Laboratory Tests: → Albumin (3.5-5 g/dL) - low → Partial Thromboplastin time or prothrombin time/INR (25-35 sec. / 11-14sec./.8-1.2) • Prolonged if there is bleeding → Serum Bilirubin (.03-1.9 mg/dL) - increased → Aspartate Aminotransferase (AST/SGOT) (10-40 U/L) - increased → Alanine Aminotransferase (ALT/SGPT) (7-56 U/L) increased → BUN - low d/t high levels of ammonia Management: → High calorie intake → Low protein to prevent hepatic encephalopathy • High protein if there is no hepatic encephalopathy → Low fat → Low sodium → Low fluid intake → Hepatic Encephalopathy • Asterixis • Constructional Apraxia • LOC o Check if oriented o Avoid sedatives • Fetor hepaticus o Assess breath → Esophageal varices • Prevent rupture o Avoid anything that might increase pressure o Beta blockers are used to decrease pressure (prevent bleeding) • (+) rupture → balloon tamponade through the use of sengstaken blakemore tube o Patient should be closely monitored: near the nurse’s station o Esophageal balloon for pressure o Gastric balloon for anchoring ▪ Can be deflated → displaced/dislodged → airway obstruction (DOB/dyspnea) → scissors at bedside to cut the 2-balloon lumen (esophageal and gastric to deflate) Medications: → Spironolactone (potassium sparing diuretic) → edema, ascites, hypokalemia → IV albumin to increase oncotic pressure → Lactulose - laxative → increased defecation → decreased level of ammonia through bowel elimination → Neomycin (antibiotic) to decrease the bacteria in the GIT → ↓protein → ↓ammonia CHOLECYSTITIS → Inflammation of the gallbladder → Can lead to cholelithiasis Types: → Calculous - gallstone → Acalculous - trauma CHOLELITHIASIS → Formation of stone → d/t supersaturation (substance separates from solution) • Cholesterol → d/t high fat diet → stones • Bilirubin (pigment stone) → from hemolysis → Gallstone will cause obstruction → injury to gallbladder → infection → inflammation → bile will not be excreted → trapping in the gallbladder → indigestion of nutrients (fats) Factors: “5 F's” → Fair → Fat → Female → Fertile (multigravid) → Forty Clinical Manifestations: → Inflammation • Biliary colic (severe pain) - cholelithiasis o Stones gets trapped in the biliary duct • Murphy’s sign o Client is in supine; nurse placed the hands on the hepatic margin → tell the client to inhale → upon inhalation diaphragm will contract → inflamed gallbladder will be palpated → pain • Abdominal pain in the RUQ • Rebound tenderness • Radiating o To the right shoulder • Usually after a heavy or fatty meal o Contraction of the gallbladder to release bile → pain → Indigestion of fats → this would accumulate in the colon → gas formation • N&V • Belching • Flatulence → Obstruction • Skin → yellow (jaundice) • Stool → steatorrhea or pale/clay colored • Urine → dark • Vitamin Deficiency of vitamin ADEK → Infection • Fever → increase insensible fluid loss • Dehydration Management: → NPO initially: (+) pain → Diet • Low fat • Small frequent meals • Avoid gas forming foods o Eggs o Cabbage o Broccoli o Cauliflower → Medications • Ursodeoxycholic acid (UDCA) - mild cases; to dissolve the stone • Chenodeoxycholic acid (chenodiol or CDCA) mild cases; to dissolve the stone • Antispasmodics/Anticholinergics (Propanthalin) for pain → Surgery: cholecystectomy (laparoscopic) • Can survive without gallbladder because it is only for storage of bile. Production of bile occur in the liver ACUTE PANCREATITIS → Obstruction leading to trapping of pancreatic enzymes inside the pancreas → autodigestion → bleeding and inflammation • Pancreatic enzymes aid in digestion → Inflammation • Pain in the LUQ radiating at the back because the pancreas is located at the back of the stomach • Aggravated by: o Diet: fatty o Beverage: alcohol o Position: flat on bed • Bowel sound: decreased d/t pain • N&V → Bleeding • Dehydration • Weight loss • Cullen’s & Grey turner’s Sign o Cullen’s: bluish discoloration in the umbilical area o Grey Turner’s: bluish discoloration in the flank area ▪ “Turn your back” Laboratory Findings: → ↑WBC → ↑Glucose → ↑Bilirubin → ↑Alkaline phosphate → ↑Serum and urinary amylase → ↑Serum lipase → Refer to serum amylase & serum lipase during recovery (should return to normal) Management: → Acute phase • NPO o Presence of food increases HCl → stimulates release of pancreatic enzyme • TPN • NGT o To suction hydrochloric acid ▪ (X) HCL → (X) stimulus for pancreatic enzymes • NPO and TPN until the patient is stable (normal amylase and lipase) → Medications: • H2 receptor blocker • Proton pump inhibitor • Morphine for pain o Given with antispasmodic/anticholinergic (atropine) ▪ Morphine can cause spasm of sphincter of oddi o (X) demerol as it can cause seizures CHRONIC PANCREATITIS → Repeated injury → fibrosis (scarring) → loss of function • Exocrine → (X) pancreatic enzyme • Endocrine → (X) insulin → Inflammation • Abdominal pain in the LUQ → Fibrosis • Palpable mass at LUQ • Hypocalcemia → used in the healing process → Loss of function • ↓body weight • ↑Bilirubin • Stool → steatorrhea d/t indigestion of fats • ↑Glucose → DM Management: → Diet • Food o Bland o Avoid gastric stimulants → ↑HCl → ↑production of pancreatic enzyme → causing damage • Small frequent meals • ↓Fat • ↓Protein → Medications • Synthetic pancreatic enzymes (oral) o Pancreatin o Pancrelipase → decreases fats in stool • Insulin & OHA