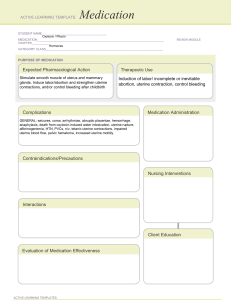
Simulation Centre – Technology Unit Pre-Simulated Clinical Experience Learning Activities SCBScN – 303 MARY DEJARLAIS – Scenario Learning Activities Scenario Synopsis: Time: 1100 Dr. T. Jackson Mary Desjarlais: Age 29, G6 P5. Admitted yesterday for Pitocin induction of labour at 40 weeks gestation due to macrosomia. Following a prolonged Pitocin induction, Mary gave birth 1 hour ago to a 5.13 kg, 55.8 cm long female infant via spontaneous vaginal delivery. EBL at delivery was 500 ml. VS have been stable. BP 110/70, Temp 37.5, P 100, RR 18, and O2 sat 99% on RA. She has had moderate vaginal bleeding and has an ice pack to her perineum for comfort. She was medicated 15 minutes ago with Ibuprofen 400 mg PO and Tylenol 650 mg PO for uterine cramping, pain 6/10. At the time the fundus was firm, one above and to the left of midline. IV RL infusing at 40 ml/hr. Learning Outcomes/Objectives: The student will be able to: Perform an appropriate assessment for a post-partum patient. Correctly identify the patient’s signs and symptoms. Initiate appropriate interventions. Communicate effectively with the patient and health care team. Reflect upon their performance in a simulated event. Medications to Review Prior to Your Scenario: • Oxytocin (Pitocin): hormones/oxytocics. Induction of labor at term & Postpartum control of bleeding after expulsion of the placenta. Stimulates uterine smooth muscle, producing uterine contractions similar to those in spontaneous labor. Has vasopressor and antidiuretic effects. ROUTE ONSET PEAK DURATION IV immediate unknown 1 hr IM 3–5 min unknown 30–60 min Adverse Effects: maternal: COMA, SEIZURES, ↑ uterine motility, painful contractions fetal: INTRACRANIAL HEMORRHAGE, ASPHYXIA Contraindicated in: Hypersensitivity; Anticipated nonvaginal delivery. Use Cautiously in: 1st and 2nd stages of labor; slow infusion over 24 hr has caused water intoxication with seizure and coma or maternal death due to oxytocin's antidiuretic effect. Revised December 1 Induction/Stimulation of Labor IV (Adults): 0.5–1 mU/min; ↑ by 1–2 mU/min every 30–60 min until desired contraction pattern established; dose may be ↓ after desired frequency of contractions is reached and labor has progressed to 5–6 cm dilation. Postpartum Hemorrhage IV (Adults): 10 units infused at 20–40 mU/min. IM (Adults): 10 units after delivery of placenta. Assess: -Fetal maturity, presentation, and pelvic adequacy should be assessed prior to administration of oxytocin for induction of labor. -Assess character, frequency, and duration of uterine contractions; resting uterine tone; and fetal heart rate frequently throughout administration. If contractions occur <2 min apart and are >50–65 mm Hg on monitor, if they last 60–90 sec or longer, or if a significant change in fetal heart rate develops, stop infusion and turn patient on her left side to prevent fetal anoxia. Notify health care professional immediately. -Monitor maternal BP and pulse frequently and fetal heart rate continuously throughout administration. -This drug occasionally causes water intoxication. Monitor patient for signs and symptoms (drowsiness, listlessness, confusion, headache, anuria) and notify physician or other health care professional if they occur. -Advise patient to expect contractions similar to menstrual cramps after administration has started. Lab Test Considerations: Monitor maternal electrolytes. Water retention may result in hypochloremia or hyponatremia. -Do not administer oxytocin simultaneously by more than one route. IV Administration Continuous Infusion: Rotate infusion container to ensure thorough mixing. Store solution in refrigerator, but do not freeze. -Infuse via infusion pump for accurate dose. Oxytocin should be connected via Ysite injection to an IV of 0.9% NaCl for use during adverse reactions. -Magnesium sulfate should be available if needed for relaxation of myometrium. Induction of Labor: Dilution: Dilute 1 mL (10 units) in 1 L of compatible infusion fluid (0.9% NaCl, D5W, or LR). Concentration: 10 mU/mL. Rate: Begin infusion at 0.5–2 mU/min (0.05–0.2 mL); increase in increments of 1–2 mU/min at 15–30-min intervals until contractions simulate normal labor. Postpartum Bleeding: Dilution: For control of postpartum bleeding, dilute 1–4 mL (10–40 units) in 1 L of compatible infusion fluid. Concentration: 10–40 mU/mL. Rate: Begin infusion at a rate of 20–40 mU/min to control uterine atony. Adjust rate as indicated. Y-Site Incompatibility: dantrolene Revised December 2 diazepam diazoxide indomethacin methohexital phenytoin remifentanil trimethoprim/sulfamethoxazole Solution Compatibility: dextrose/Ringer's or lactated Ringer's combinations dextrose/saline combinations Ringer's or lactated Ringer's injection D5W D10W 0.45% NaCl 0.9% NaCl • Misoprostol (Cytotec): Antiulcer agents/Prostaglandins. Prevention of gastric mucosal injury from NSAIDs, including aspirin, in high-risk patients (geriatric patients, debilitated patients, or those with a history of ulcers), Cervical ripening and labor induction. Acts as a prostaglandin analogue, decreasing gastric acid secretion (antisecretory effect) and increasing the production of protective mucus (cytoprotective effect) & Causes uterine contractions. ROUTE ONSET PEAK PO 30 min DURATION unknown 3–6 hr Adverse Effects: Abdominal pain, diarrhea Contraindicated in: Hypersensitivity to prostaglandins; OB: Should not be used to prevent NSAID-induced gastric injury due to potential for fetal harm or death; Lactation: May cause severe diarrhea in the nursing infant. Exercise Extreme Caution in: When used for cervical ripening (unlabeled use) or to induce abortion, may cause uterine rupture (risk factors are late trimester pregnancy, previous Cesarian section or uterine surgery, advanced gestational age, or ≥5 previous pregnancies). Intravaginally: (Adults): 25 mcg (¼ of 100–mcg tablet); may repeat every 3–6 hr, if needed. -Assess patient routinely for epigastric or abdominal pain and for frank or occult blood in the stool, emesis, or gastric aspirate. -Assess women of childbearing age for pregnancy. Misoprostol is usually begun on 2nd or 3rd day of menstrual period following a negative pregnancy test result. -Cervical Ripening: Assess dilation of cervix periodically during therapy. - Administer medication with meals and at bedtime to reduce severity of diarrhea. Revised December 3 • Tranexamic Acid (Cyklokapron): hemostatic agents/antifibrinolytics/plasminogen inactivators. IV Prevention or reduction of hemorrhage during and following dental surgery in hemophiliacs. Inhibits activation of plasminogen, thereby preventing the conversion of plasminogen to plasmin. ROUTE ONSET PEAK DURATION IV unknown unknown 7–8 hr PO unknown 2.5 hr unknown Adverse Effects: SEIZURES, headache, pain, ANAPHYLAXIS Contraindicated in: Hypersensitivity Thromboembolic disorders (current, history of, or at risk for) Acquired defective color vision (IV) Subarachnoid hemorrhage; Concurrent use of combination hormonal contraception (PO). Use Cautiously in: Renal impairment (↑ dosing interval) Hematuria originating in the upper urinary tract Conditions associated with ↑ thrombus formation Use of hormonal contraceptives (PO) OB: Lactation -Observe site for excessive bleeding - Advise patient to stop medication and inform health care professional of any changes in vision. Inform patients on prolonged therapy of the importance of regular ophthalmologic follow-up. -Instruct patient to notify health care professional if signs and symptoms of thrombosis (severe, sudden headache; pains in chest, groin, or legs, especially calves; sudden loss of coordination; sudden and unexplained shortness of breath; slurred speech; visual changes; weakness or numbness in arm or leg) or anaphylaxis (shortness of breath, throat tightness, rash) occur. IV (Adults and Children): 10 mg/kg just prior to surgery with appropriate replacement therapy, then 10 mg/kg 3–4 times daily for 2–8 days. PO (Adults): 1300 mg 3 times daily for a maximum of 5 days during menstruation. Solution for injection: 100 mg/mL PO Administer 3 times daily without regard to food. Swallow tablets whole; do not crush, break, or chew. IV Administration Intermittent Infusion: Dilution: May be diluted with most solutions, such as electrolyte, carbohydrate, amino acid, and dextran solutions. Prepare mixture on day of infusion. Rate: Infuse at a rate not to exceed 100 mg (1 mL)/min. More rapid administration has resulted in hypotension. Y-Site Compatibility: heparin Revised December 4 Y-Site Incompatibility: ampicillin ampicillin/sulbactam blood penicillin piperacillin/tazobactam • Ergonovine (Ergotrate): oxytocics. Prevention and treatment of postpartum or postabortion hemorrhage caused by uterine atony or involution. Directly stimulates uterine and vascular smooth muscle. ROUTE ONSET PO PEAK DURATION 5–15 min unknown ≥3 hr Contraindicated in: Hypersensitivity Avoid chronic use Should not be used to induce labor. Use Cautiously in: Hypertensive or eclamptic patients (increased susceptibility to hypertensive and arrhythmogenic side effects) Severe hepatic or renal disease Sepsis Third stage of labor. Adverse Effects: nausea, vomiting PO SL (Adults): 0.2–0.4 mg q 6–12 hr (usual course is 48 hr). IM IV (Adults): 200 mcg (0.2 mg) q 2–4 hr for up to 5 doses. Injection: 0.25 mg/mL - Monitor BP, pulse, and respirations every 15–30 min until transfer to the postpartum unit, then every 1–2 hr. Report hypertension, chest pain, arrhythmias, headache, or change in neurologic status. -Monitor amount and type of vaginal discharge. Report symptoms of hemorrhage (increased bleeding, hypotension, pallor, tachycardia) immediately. -Palpate uterine fundus; note position and consistency. Notify health care professional if fundus fails to contract in response to ergonovine. Assess patient if cramping is severe; dose may be decreased. -Assess for signs of ergotism (cold, numb fingers and toes; nausea; vomiting; diarrhea; headache; muscle pain; weakness). -If patient fails to respond to ergonovine, check serum calcium level. Correction of hypocalcemia may restore responsiveness. Lab Test Considerations: May cause ↓ serum prolactin level, which inhibits synthesis of breast milk - Review symptoms of toxicity with patient. Instruct the patient to report occurrence of these immediately. -Inform patient that uterine cramping demonstrates effectiveness of therapy. -Explain need for pad count to determine degree of bleeding. Instruct patient to report immediately an increase in degree of bleeding or passage of clots. Revised December 5 -Instruct patient to report breastfeeding difficulties. -Caution patient not to smoke while receiving ergonovine; nicotine is also a vasoconstrictor. -Do not administer solution that is discolored or contains a precipitate. PO Administration is usually limited to 48 hr postpartum, by which time the danger of hemorrhage from uterine atony has passed. Tablets may be administered SL. IM The preferred route. Firm uterine contractions are produced within a few minutes. Dose may need to be repeated every 2–4 hr for full therapeutic effect. IV Administration IV Push: The IV route is reserved for severe uterine bleeding. Dilution: Dilute with 5 mL of 0.9% NaCl. Rate: Administer slow IV push over at least 1 min through Y-site injection of an IV of D5W or 0.9% NaCl. Preparatory Exercise: Answer the following questions prior to your lab experience: 1. Choose True (T) or False (F) for the following statements. Be prepared to explain your answers. A. (T)(F) The Fourth stage begins after the placenta is expelled and continues 4-5 hours post-partum. - lasts until the patient is stable in the immediate postpartum period, usually within the first 2 hours after birth B. (T)(F) Vital Signs are taken every 15 minutes for one hour, then every 30 minutes for the next three hours during the fourth stage of labour. - Every 30 minutes for one hour & PRN C. (T)(F) Decreased BP is an early reliable source to detect hemorrhage. - Late sign D. (T)(F) A woman’s respirations, pulse, skin condition, urinary output, and level of consciousness can be used as early warning signs in identifying PPH. E. (T)(F) A full bladder causes the uterus to be displaced below the umbilicus and directly in the midline of the abdomen. - A full bladder causes the uterus to be displaced above the umbilicus and well to one side of the midline in the abdomen. It also prevents the uterus from contracting normally. F. (T)(F) Traditionally, PPH is defined as the loss of more than 500mls of blood during a vaginal birth and more than 1000mls of blood during a Caesarean birth, but Revised December 6 definitions have changed in that any blood loss that has the potential to cause hemodynamic instability should be considered PPH. - PPH may be defined as a 10% decline in hemoglobin concentration and the need for a transfusion G. (T)(F) Uterine atony, or failure of the uterine muscle to contract firmly is the least common cause of early PPH. - Most common H. (T)(F) The two most important interventions for preventing excessive uterine bleeding are maintaining good uterine tone and preventing bladder distension. I. (T)(F) Postpartum hemorrhage is preventable in less than 25% of cases. - 50% J. (T)(F) PPH not a leading cause of maternal death worldwide. - Leading cause K. (T)(F) The following are all risk factors of PPH: large fetus, high parity, prolonged labour, and oxytocin-induced labour. Tone: Uterine Atony • Overdistended uterus—large fetus, multiple fetuses, hydramnios, distension with clots • Anaesthesia and analgesia—conduction anaesthesia • Previous history of uterine atony • High parity • Prolonged labour, oxytocin-induced labour • Magnesium sulphate administration during labour or postpartum period • Chorioamnionitis • Uterine subinvolution • Obesity Trauma • Lacerations of the birth canal • Trauma during labour and birth—forceps-assisted birth, vacuum-assisted birth, Caesarean birth • Ruptured uterus • Inversion of the uterus • Manual removal of a retained placenta Revised December 7 Tissue • Retained placental fragments • Placenta accreta, increta, percreta • Placental abruption • Placenta previa Thrombin • Coagulation disorders 2. What does nursing care during the fourth stage of labour include? - mother assessment of Vital Signs, Pain, Breasts/nipples, Uterus/incision, Bladder, Lochia, Legs/Extremeties, Episiotomy, Psychological wellbeing - monitoring for hemorrhage - keeping them warm/comfortable - fundal massage - encourage voiding - Assist with breastfeeding and baby bonding (skin to skin is important) - Patient teaching about their recovery and caring for their new baby - Newborn assessment/ Apgar assessment: Vital Signs, weight, skin, head, sutures, fontanelles, face, eyes, mouth, nose, neck, shoulders arms, chest, abdomen, cord, genitailia, hips/legs, back. Reflexes, muscle tone, fingers and toes 3. What happens to the patient’s vital signs after delivery/in the fourth stage? - During this time, the postpartum patient’s organs undergo their initial readjustment to the nonpregnant state, and the functions of body systems begin to stabilize. - Heart rate, Blood Pressure, Resp Rate, Pulse Temp should all be decreasing back to normal baseline 4. Tone (Uterine Atony), Tissue, Trauma, and Thrombin (Coagulopathies) are the 4 T’s of PPH. Match the T’s with the statements below. There may be more than one statement for each T. _____Tone_____ Uterine muscle tone can be effected by over-distention of the uterus by multifetal gestation, fetal macrosomia, hydramnios, fetal abnormality, placental fragments, and prolonged or rapid/forceful labour (especially if induced). Bacterial toxins, use of some drugs like halothane and magnesium sulphate can also affect uterine muscle tone. _____Trauma_____ Damage to the genital tract and vaginal area can be the result of surgical or manipulative maneuvers, prolonged and forceful labour (especially by induction), or previous surgical procedures to the uterine wall. Rupture or lacerations may occur during labour, birth, and delivery. Rupture and significant lacerations must be surgically remediated. _____Tissue_____Failure of complete placental expulsion as this does not allow for full contraction of the uterus which needs to happen fully to clamp off the vessels. It is necessary to inspect the placenta to confirm nothing is left in the uterus. If the placenta Revised December 8 adheres to the myometrium and does not separate and deliver, profuse hemorrhage will result. ______Thrombin____Blood clots help prevent PPH right after birth by homeostasis in the woman’s circulatory system. Coagulation disorders can disrupt this clotting process but may not be found immediately as the contracting uterus will clamp off the bleeding vessels. Coagulation problems should be considered if bleeding continues and the reason is not apparent. ITP, von Willebrand disease and DIC are coagulopathies that may present post-partum. _____Trauma_____ Uterine inversion can occur by abnormal adherence of the placenta or excessive traction on the umbilical cord, vigorous fundal pressure, precipitous delivery or vigorous manual extraction of the placenta. ____Tone______The pregnant uterus processes 500 mL of blood per minute, making it essential for the myometrium to contract after birth. If the uterus does not contract after the expulsion of the uterus, placenta venous bleeding will occur and continue until the uterine muscle is contracted. 5. What is the Nursing Management for PPH? Fundal massage urination/catheterization medications surgery ensure entire placenta comes out ensure site repair is initiated right away, apply pressure, stitches medications IV fluids/blood products to ensure adequate circulating volume 6. Review the attached: Physician Order Set for Patients with Significant Post-Partum Hemorrhage. What would be your priorities be? Revised December 9 Management of Patients with Significant Postpartum Hemorrhage These orders will apply to all post-partum patients with both: • Abnormal maternal vital signs (one or both of the following): o pulse rate at least 100 bpm, or 20 bpm above admission baseline o BP less than 90/50 mmHg AND • Post-Partum bleeding (one or both of the following): o Poor uterine tone and constant trickle with fundal massage o One saturated peripad in 1 hour or less Based on an individual assessment of each patient, Registered nurses (RNs) will initiate orders as directed below Treatments ● ● ● ● ● ● ● ● Call for additional nursing help Notify MRP AND designate via phone or overhead stat call (based on patient’s condition) Lay bed flat Apply suprapubic pressure and massage the uterine fundus continuously NOTE: Have sterile gloves and lubricant available at the bedside Ensure patient has at least two large bore, patent IVs Infuse Ringer’s Lactate at 250 mL/hr in each IV Insert Foley catheter O2 PRN to maintain SpO2 above 93% Medication ● oxytocin (30 units in 500 mL Ringer’s Lactate) IV at 80 mL/hr via piggyback ● misoprostol 600 mcg sublingual once as soon as possible if not given postpartum ● Tranexamic Acid 1 gram IV over 10 minutes if not given postpartum NOTE: Have ergonovine and carboprost (Hemabate®) available at bedside Observation ● ● ● Vital signs (BP, HR, RR), EBL, fundal height and tone at minimum q15min for one hour, and until patient condition stable SpO2 and Level of Consciousness (LOC) continuously for at least one hour, and until patient condition stable. Notify MRP or designate if altered LOC. Monitor urinary output every hour. Notify MRP or designate if output is less than 30 mL/hr.