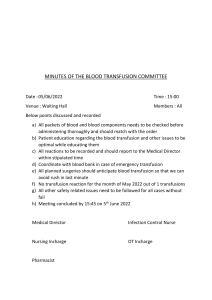
BLOOD TRANSFUSION • Go through the pre-administration, administration procedure of blood transfusion • Care of patient during blood transfusion • Complications of blood transfusion. DEFINATION • Iv administration of a component of blood or whole blood. PURPOSE: To restore hemodynamic status of the patient. To treat factor specific deficiencies For immunotherapy INDICATIONS • Massive blood loss of >25-50%of a persons total blood volume • Severe haemolysis in the newborn • Severe anemia • Peri-operative in major surgeries. • Bleeding disorders thrombocytopenia,haemophilia and disseminated intravascular coagulopathies. Blood components 1.Whole blood-used in extreme cases of acute hemorrhage .Replaces blood volume and all blood products i.e. red blood cells, plasma proteins, fresh platelets and other clotting factors 2.PACKED CELLS Are packed red blood cells with 80%of the plasma removed from the whole blood. Used in situations where the patient is at risk for circulatory overload but has need of Hb or its oxygen carrying capacity e.g. continuation a)Patients with severe anemia who have relatively normal blood volume b)Patients with risk of heart failure c)Transfusion of infants. Packed cells needs a large bore needle as flow rate is lower than normal blood volume. 3.Fresh frozen plasma • Is plasma which has been separated immediately from freshly donated blood and then promptly frozen Given to boost coagulation factors. 3.Platalets transfusion Is platelets suspended in 20mls of plasma Given to patients with severe thrombocytopenia(reduced platelets) Normal value(150,000-400,000/ml) 4.Clotting factors Used for clients with clotting factor deficiencies. Each provides different factors involved in the clotting pathway e.g. factor VIII, factor IX Pre-administration procedure The doctors orders: -Number of units to be x-matched -Rate of transfusion When blood has been x-matched and screened it is kept in the blood bank then laboratory staff: continuation • Sends a small slip to the ward with patients full name and blood particulars which is used for collecting blood the bank • The nurse collecting blood goes with the transfusion record form, which is filled by the technologist. • He/she checks the patients full names, inpatient number, ward, doctor, blood group and rhesus factor and whether blood is screened for infection and is compatible, and expiry date continuation • Checks the pack number on the bottle against the number on the slip • Fill the blood bank book with full details and sign In the ward,2 people, one being a qualified nurse or a doctor will check the blood against the patients chart for correct name and also against the laboratory slip and the bottle. Warming of blood should not be done unless under doctors instructions Requirements • A sterile blood transfusion set with a filter • disposable gloves • vital signs observation set • Unit of blood/blood component in a receiver • strapping • Galipot with cotton wool swabs • Receiver for soiled swabs • Sterile intravenous needle or branula • Tourniquet • Drip stand PROCEDURE 1.Wash and dry hands-minimize transfer of micro organisms 2.Explain the procedure to the patient-to gain cooperation 3.Take equipments to patients bed side-to promote efficiency of the procedure 4.Review patients understanding of the procedure, side effects. 5.Position the patient with pillows and offer a urinal or bed pan if need be before start transfusion-to make them comfortable during transfusion N/B: Do not leave blood at room temperature for more than 6hrs because it destroys blood cells which release potassium causing hyperkalemia and increases bacterial growth. 6.Obtain vital signs before transfusion i.e. TPR and BP-base line measurements are used for later comparisons 7.Verify the blood product with another nurse on identification data.ie patients name, blood group, rhesus factor, cross match compatibility and if blood has been screened for infection, type of product compared with the prescription order and expiry date of the blood product-if information does not match report to the senior nurse 8.Patients locker, bell, water etc. is positioned at a convenient site for easy reach-to limit patients movements during transfusion 9.Set up the infusion equipments as in intravenous fluid but now blood giving set which has a filter 10.Mix the blood cells by gently inverting the bag several times 11.Hang the unit of blood about a meter above the level of the heart-----the rate of flow is determined by the height at which the bottle is suspended and size of the needle 12.Commence the transfusion and adjust the flow rate to 10 DPM during the first 15 minutes of transfusion stay with the patients for at least 15 minutes after the start of transfusion. If no reaction adjust it to run between 4-5hrs OR adjust according to the doctors Instruction----- Symptoms of blood reactions are usually manifested during the initial 50-100mls of blood transfused. If transfusion is stopped early acute renal failure and death rarely occur. 13.Give blood at slower rate if the patient is elderly or has a heart disease-----Rapid transfusion may overload the circulatory system and induce congestive cardiac failure and pulmonary edema 14.Remain with the client for the first 15-30 minutes and monitor vital signs every 15 mins for 1 hour then monitor hourly and after the transfusion is completed-----a change in condition of the patient may signal the development of a transfusion complication 15.Change the transfusion set if another unit of blood is to be given---the filter may become clogged after a unit of blood has been given 16.Record the transfusion in red to include the time you started the blood, the vital signs during the transfusion period and the time the blood ended and maintain the fluid chart. Reactions to transfusion Signs and symptoms Nursing intervention Fever Chills Stop transfusion immediately Keep the vein open with normal saline Monitor TPR and BP Notify patients doctor Observe urine output Collect blood(5cc) and urine samples and send to laboratory Return pack to laboratory along with a copy of transfusion record form Discontinue the transfusion immediately. Run an intravenous infusion of normal saline, send the remaining blood, a sample of the clients blood and urine sample to the Tachycardia Tachyponea Hypotension(decreased BP) Dysponea Restlessness Flank pain Chest constriction Lower back pain Dark urine Nursing intervention Circulatory overload `Stop transfusion immediately Signs and symptoms Dysponea, cough, Distended neck veins haemoptysis Elevate the patient at 450 Commence on oxygen Notify patients doctor Transmission of disease AIDS ,Hepatitis B ,Malaria Careful screening of blood donors Febrile reaction- fever, chills, headaches, nausea and vomiting Stop the transfusion Monitor vital signs Notify doctor Administer antihistamines and antipyretics as ordered. Allergic reaction Mild hives,itching,flushing,severe shortness of breath, bronchospasms and wheezing Stop transfusion Notify doctor Give anti-histamines as ordered continuation Air embolus-cyanosis, dysponea shock cardiac arrest Lower patients head and turn Patients on the left side Notify the doctor Treat shock or cardiac arrest appropriately Hypothermia Slow transfusion Keep patient covered Prevention: give blood at room temperature Hyperkalemia Prevention: Check expiry date on blood pack • To discontinue blood transfusion refer to intravenous fluids THE END QUESTIONS??