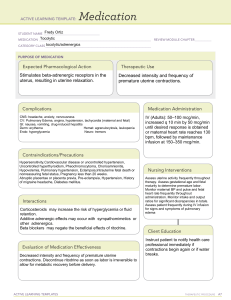
What is Labor? Labor refers to the process of childbirth, during which a pregnant woman experiences rhythmic uterine contractions that lead to the progressive opening of the cervix and the eventual delivery of the baby. It is a natural and dynamic process that signifies the end of pregnancy and the beginning of motherhood. Establishing Therapeutic Relationship To gain the patient and family’s cooperation and trust, it is important that the nurse should be able to establish a therapeutic relationship with them. The nurse should introduce himself and make them feel welcome. At this point, they are all anxious and it is best for the nurse to convey his message gently and confidently. Expectations of the family about birth should be determined and it is also the best time to ascertain cultural values. Admission Assessment When a patient arrives at the labor floor, pertinent information about the pregnant woman’s health history is taken during admission. These include personal data (e.g. blood type, allergies, etc.), previous illness, pregnancy complications, preferences for labor and delivery, and childbirth preparations. Standard obstetric, medical, and social history taking is also done. In addition, the nurse assesses the following: vital signs, physical exam, contraction pattern (frequency, interval, duration, and intensity), intactness of membranes through a vaginal exam, and fetal well-being through fetal heart rate, characteristic of amniotic fluid, and contractions. The nurse performs Leopold’s maneuver to determine the fetal presenting part, point of maximum impulse, fetal descent, and engagement. Admission into the labor room is only done when the patient is in active labor. Stages of Labor The progress of cervical effacement, cervical dilatation, and descent of the fetal presenting part dictate stages of labor. Here are the stages of labor and significant events that mark their beginning and end: Duration Stages of Labor Start End Nullipara Multipa 10-12 hr but 6-20 hrs is the normal limit 6-8 hrs but 2is the normal First Stage True labor contractions Full cervical dilatation Latent phase Onset of regularly perceived uterine contractions (mild contractions lasting 20-40 sec) 3 cm cervical dilatation 6 hrs 4.5 hrs Active phase Stronger uterine contractions lasting 40-60secs 7 cm cervical dilatation 3 hrs 2 hrs Transitional phase Uterine contractions reaching their peak, occurring every 2-3 minutes for 60-90 s 10 cm cervical dilatation 3 hrs 1.5-2 hrs <2 hrs 0.5-1 hrs 3 hrs with epidurals 2 hrs with ep Second Stage Third Stage Full cervical dilatation Infant birth Infant birth Placental delivery Maximum of 30 min. First Stage of Labor As mentioned above, the first stage of labor is divided into three sub-phases, namely: latent, active, and transitional phases. Latent Phase Latent (Preparatory) Phase starts from the onset of true labor contractions to 3 cm cervical dilatation. Here are nursing responsibilities during this phase: 1. Assess patient’s psychological readiness. Provide continuous maternal support (compared to usual care). 2. Measure duration of latent phase. For nulliparas, it should not be more than 6 hours. On the other hand, for multiparas, it should be within 4.5 hours. Determine if patient received anesthesia because it can prolong latent phase. One of the most common cause of prolonged latent phase is cephalopelvic disproportion (CPD) and it requires cesarean birth. 3. Allow patient to be continually active. Upright maternal positions are recommended for women on the first stage of labor. Patients without pregnancy complications can still walk around and make necessary birth preparations. 4. Conduct interviews and filling in of forms (e.g. birth certificate) at this phase while the patient experiences minimal discomfort and has control over contraction pains. 5. Conduct health teaching on breastfeeding, newborn care, and effective bearing down because during this time, patient’s anxiety is controlled and she is able to focus on nurse’s instructions. 6. Educate patient on different relaxation techniques. As early as this phase, encourage patient to begin alternative therapy of pain relief. 7. Ensure that the total number of internal examinations the woman receives in the entire course of labor is limited to 5 only. 8. Ensure that birthing companion of choice is present all throughout the course of labor. Active Phase Active Phase starts from 4 cm cervical dilatation to 7 cm cervical dilatation. During this phase, contraction intensity is stronger, interval shortens, and duration lengthens. This is where true discomfort is first felt by the patient so she is dependent and her focus is on herself. Here are nursing responsibilities in this phase: 1. Inform patient on the progress of her labor to lessen her anxiety and obtain her trust and cooperation. 2. Start monitoring progress of labor with the use of WHO partograph, 2hour action line. 3. Encourage patient to be continually active to maximize the effect of uterine contractions. Upright maternal positions are recommended if tolerated. 4. Assist patient in assuming her position of comfort. For those who can’t stay upright, left-side lying is recommended to avoid disruption in fetal oxygenation. 5. Monitor maternal vital signs and fetal heart rate every 2 hours, or depending on the doctor’s order. 6. Anticipate patient needs (e.g. sponging face with cool cloth, keeping bed clean and dry, providing ice chips or lip balm) to promote comfort. 7. Determine when patient last voided because a full bladder can hinder fast labor progress. 8. Institute non-pharmacological pain measures (e.g. breathing exercises, distraction method, imagery, music therapy, etc.) Transition Phase Transition Phase starts from 8 cm cervical dilatation to 10 cm (full) cervical dilatation and full cervical effacement. During this time, patient may be exhausted and withdrawn or aggressive and restless. Patient’s urge to push is noticeable. Here are nursing responsibilities in this phase: 1. Inform patient on progress of her labor. 2. Assist patient with pant-blow breathing. 3. Monitor maternal vital signs and fetal heart rate every 30 minutes -1 hour, or depending on the doctor’s order. Contraction monitoring is also continued. 4. When perineal bulging is noticeable, prepare for delivery. Check room temperature (25-280C and free of air drafts). The nurse should also notify staff and prepare necessary supplies and equipment, including resuscitation machine. Lastly, perform handwashing and double gloving. WHO do not recommend the following nursing interventions during labor because they have low quality of evidence: 1. Routine perineal shaving 2. Routine use of enema 3. Admission cardiotocography (CTG) for low-risk women 4. Vaginal douching 5. Routine amniotomy for patients in spontaneous labor 6. Massage and reflexology Second Stage of Labor Second Stage of Labor starts when cervical dilatation reaches 10 cm and ends when the baby is delivered. At this stage, the patient feels an uncontrollable urge to push. The patient may also experience temporary nausea together with increased restlessness and shaking of extremities. The nurse at this stage must coach quality pushing and support delivery. Here are nursing care tips for this stage: 1. Instruct patient on quality pushing. The abdominal muscles must aid the involuntary uterine contractions to deliver the baby out. 2. Provide a quiet environment for the patient to concentrate on bearing down. 3. Provide positive feedback as the patient pushes. 4. Repeat the doctor’s instructions. At this phase, the patient barely hears the conversation around the room because all her energy and thoughts are being directed toward giving birth. 5. Take note of the time of delivery and proceed to initiate essential newborn care. Delayed cord clamping is recommended. 6. Assist in restrictive episiotomy for patients who had vaginal births. WHO do not recommend the following interventions during delivery because they provide low quality evidence: 1. Perineal massage 2. Use of fundal pressure Third Stage of Labor Third Stage of Labor or the placental stage starts from birth of infant to delivery of placenta. It is divided into two separate phases: placental separation and placental expulsion. Five minutes after delivery of baby, the uterus begins to contract again, and placenta starts to separate from the contracting wall. Blood loss of 300-500 mL occurs as a normal consequence of placental separation. Placenta sinks to the lower uterine segment or upper vagina. The placenta is then expelled using gentle traction on the cord. Here are the signs of placental separation: 1. 2. 3. 4. 5. Lengthening of umbilical cord Sudden gush of vaginal blood Change in the shape of uterus (globular in shape) Firm uterine contractions Appearance of placenta in vaginal opening At this stage, here are the nursing care tips: 1. Coach in relaxation for delivery of placenta. 2. Congratulate on delivery of baby. 3. Encourage skin-to-skin contact to facilitate bonding and early breastfeeding. 4. Ask patient whether placenta is important to them before it is destroyed. For those who want to take it home, ensure that they understand and follow standard infection precautions and hospital policy. 5. Administer prophylactic oxytocin as ordered. 6. Utilize controlled cord traction technique for placental expulsion. 7. Utilize absorbable synthetic suture materials (over chromic catgut) for primary repair of episiotomy or perineal lacerations. For immediate postpartum, the nurse checks the vital signs and monitors for excessive bleeding. The first four hours after birth is sometimes referred to as the fourth stage of labor because this is the most critical period for the mother. The nurse is set to perform nursing interventions that would prevent the patient from infection and hemorrhage. Also, they are being reminded of the importance of breastfeeding, ambulation, and newborn care. Here are WHO recommendations for immediate postpartum: 1. Early (<6 hours) resumption of feeding for patients who have vaginal birth 2. Prophylactic antibiotics for women who sustained third to fourth degree of perineal tear during delivery 3. In healthy women who delivered vaginally to term infants, early postpartum discharge is recommended. On the other hand, here are interventions not recommended during immediate postpartum: 1. Routine use of ice packs 2. Oral methylergometrine for patients who delivered vaginally Assessment The key to a successful individualized care plan is the precise assessment and accurate obtaining of data. The woman would be placed under observation during labor to monitor her progress and ensure a safe delivery for her and the child. Assess for the signs of true labor. The signs of true labor are contractions that begin irregularly but progresses regularly and predictably, the pain is felt first at the lower back and circles towards the abdomen, continues to progress no matter what the woman’s activity level is, increases in duration, frequency, and intensity and cervical dilation is already present. Assess for the appearance of show, which is blood mixed with mucus and would be present once the operculum or mucus plug is expelled. Assess for the rupture of membranes. This is the scanty or sudden gush of clear fluid from the vagina. Assess for the engagement of the fetal head. Engagement refers to the settling of the presenting part into the pelvis at the level of the ischial spines. Assess for the station. Station is the relationship of the presenting part to the level of the ischial spines. Assess for the effacement and dilatation of the cervix. Effacement is the shortening and thinning of the cervical canal. In cervical dilatation, the enlargement or widening of the cervical canal is assessed. Planning With all the data gathered during assessment and through an accurate diagnosis, a care plan for the woman in labor would be made to aid her through her progress. Care of a woman in the first stage of labor Labor should be allowed to start naturally, not artificially induced. The woman must also be allowed to move freely throughout the labor. Artificial interventions should also be prohibited. Allow the woman to assume a non-supine position for delivery. Upon delivery of the newborn, mother and child should be given unlimited opportunity for breastfeeding and bonding. Care of a woman in the second stage of labor During the second stage of labor, the place of delivery of the woman must be prepared. The position of birth wherein the woman is most comfortable must also be determined at this stage. Another important part is the promotion of second stage effective pushing. Perineal cleaning is also an integral part of the second stage. Care of the woman in the third stage of labor Placental delivery should be given focus at this stage. Once the placenta is delivered, oxytocin should be administered intramuscularly to promote uterine contractions. If there is episiotomy performed, perineal repair should be integrated into the care plan. Implementation Some interventions are implemented to give comfort and safety for the mother during and after the labor period. These are essential in promoting the strength that the mother would need during delivery. Encourage the client to void every 2 hours. Observe and review the client’s breathing techniques. Inform the client if c interventions are necessary. Create a birth plan with the client so she could integrate her preferences in the care plan. Provide ice chips, hard candies, or fluids to relieve dry mouth. Provide a comfortable environment to aid in the effective coping management of the client. Allow the client to walk and move around freely during labor. Do not intervene with the client during a contraction to avoid disturbing her focus on her technique. Evaluation After the labor has passed, delivery would commence immediately. And when the labor period for the woman has gone smoothly, a great chance for a safe and healthy delivery is within reach. Client should exhibit no signs of bladder distention and have the ability to void every 2 hours. Client has a good to tolerable level of pain. Client can express her preferences during labor. Client has the ability to understand the usual process of labor. Client reports that her environment is comfortable and secure. Client would be able to verbalize her feelings about her experiences during her labor period. Induction and Augmentation of Labor Cervical Ripening Cervical ripening must be complete during early labor. If there is no cervical ripening, there would be no dilatation and coordination of uterine contractions. To determine whether the cervix is ripe, Bishop established criteria for scoring the cervix. If the woman’s score is 8 or greater, the cervix is already ready or birth and would respond to induction. One of the ways to ripen the cervix is known as “stripping the membranes”, or separating the membranes from the lower uterine segment manually using a gloved finger in the cervix. Complications that may arise from this procedure include bleeding due to undetected low-lying placenta, inadvertent rupture of membranes, and infection when the membranes rupture. Another method that is also considered is the use of hygroscopic suppositories or suppositories of seaweed that swell upon contact with cervical secretions. These suppositories gradually and gently urge dilatation. They are held in place by gauze sponges saturated with povidone iodine or an antifungal cream. The number of sponges and dilators should be documented accordingly to avoid leaving behind one of them inside the cervix. A more common method of speeding cervical ripening is the application of a prostaglandin gel to the interior surface of the cervix by a catheter or suppository, or to the external surface by applying it to a diaphragm and then replacing it against the cervix. Additional doses may be applied every six hours, but two or three doses are usually enough to achieve ripening. Instruct the woman to remain in a side lying position to avoid leakage of the medication. Continuously monitor the FHR at least every 30 minutes after each complication. Side effects of this method include diarrhea, fever, hypertension, and vomiting. Oxytocin administration may also be started, but that would be 6 to 12 hours after the last prostaglandin dose. Use prostaglandin with caution in women with asthma, renal or cardiovascular disease, or glaucoma. Women who underwent cesarean birth in the past are contraindicated with prostaglandin method. Induction of Labor by Oxytocin Administration of oxytocin can initiate contractions in a uterus in pregnancy term. Oxytocin is administered intravenously so that when there is hyperstimulation, then it could be quickly discontinued. The effects happen immediately because the half-life of oxytocin is approximately 3 minutes. Oxytocin is usually mixed with Ringer’s lactate, 10 units of oxytocin in 1000 mL of Ringer’s lactate. The infusion could also be administered piggyback to a maintenance IV solution, so that if the infusion would be discontinued, the main IV line could still be maintained. The oxytocin solution must always be attached to the port nearest to the woman so that little solution remains in the tubing if it is discontinued. Use of an infusion pump is recommended to regulate the infusion rate and make sure that the rate would not change even if the woman moves. Do not increase the rate without any further instructions because it can cause tetanic contractions. Artificial rupture of membranes may be done when cervical dilatation reaches 4 cm to further induce labor. Be aware of peripheral vessel dilatation, a side effect of oxytocin administration, which can cause hypotension. Assess the woman’s pulse and blood pressure every 15 minutes to be certain of a safe induction. Monitor uterine contractions and FHR accordingly. Contractions should occur no more often than every 2 minutes, should not be longer than 70 seconds, and not stronger than 50 mmHg. Stop the IV infusion if the contractions become more frequent or longer in duration than the safe limits or if there are signs of fetal distress. Excessive stimulation of the uterus by oxytocin may lead to tonic uterine contractions with fetal death or rupture of the uterus. In the event that hyperstimulation is not stopped even if the infusion has been discontinued, a beta-adrenergic receptor drug or magnesium sulfate may be prescribed to decrease myometrial activity. A complication of oxytocin infusion is water intoxication because oxytocin has an antidiuretic effect that results in decreased urine flow. Symptoms of water intoxication are headache and vomiting. Water intoxication in its most severe form can cause seizures, coma, and even death because of the large shift in interstitial tissue fluid. Monitor the intake and output appropriately and assess urine specific gravity to detect fluid retention. Limit the amount of IV fluid to 150 mL/hr by making sure that the main line is infusing at a rate not greater than 2.5 mL/min. Induced labor tends to have shorter first stage than the average unassisted labor. Assure the woman that uterine contractions in an induced labor are basically normal so she can use her breathing techniques effectively. However, hyperbilirubinemia and jaundice in a newborn are possible because of induction of labor with oxytocin. The infant should be observed closely for these conditions during the first few days of life. Augmentation by Oxytocin If labor contractions begin spontaneously but become weak, irregular, and ineffective, augmentation of labor is required. Precautions for oxytocin administration are the same as for primary induction of labor. The uterus may respond effectively to oxytocin used as augmentation. The drug should be increased in small increments only and fetal heart sounds should be monitored during the procedure. The labor process is the gateway towards a safe delivery. Once the woman has undergone labor, it is imminent that delivery would follow suit. It is important for the woman to have a smooth labor process for this is where she would be gathering her strength to deliver her precious bundle of joy. Labor Complications Getting through labor is one of the most anticipated events during a woman’s pregnancy. To avoid complications during labor, a thorough assessment should be conducted by the health care providers early during the woman’s pregnancy. Uterine Rupture Uterine rupture is a rare but serious complication. Uterine rupture is a condition wherein the uterus cannot sustain the strain that it underwent. Factors that contribute to uterine rupture are abnormal presentation, prolonged labor, multiple gestation, improper use of oxytocin, and traumatic effects of forceps use or traction. Fetal death can be avoided in uterine rupture if immediate cesarean birth can be performed. Symptoms that a woman may feel preceding rupture are a sudden, severe pain during a labor contraction or a tearing sensation. Rupture can be complete or incomplete. With complete uterine rupture, the rupture goes through the endometrium, myometrium, and peritoneum, and then the contractions would immediately stop. With incomplete uterine rupture, the rupture only goes through the endometrium and the myometrium only, with the peritoneum still intact. Symptoms of complete uterine rupture include hemorrhage, shock, fading fetal heart sounds, distinct swellings of the retracted uterus and extrauterine fetus. For incomplete rupture, there is localized tenderness, persistent aching pain in the lower uterine segment, and lack of contractions and fetal heart sounds. Confirmatory diagnosis of uterine rupture can be revealed through ultrasound. Administration of emergency fluid replacement as ordered should be anticipated as well as IV oxytocin. Laparotomy would be performed to control the bleeding and repair the rupture. Cesarean hysterectomy or tubal ligation can also be performed with consent from the patient to remove the damaged uterus and remove the childbearing activity of the woman. Fetal outcome, the woman’s safety, and the extent of the surgery must be revealed to the patient and allow time for them to express their emotions. The woman would be advised not to conceive again after a rupture of the uterus unless the rupture is in the inactive lower segment. The viability of the fetus and the woman’s prognosis depends on the extent of the rupture. Inversion of the Uterus Uterine inversion occurs when the uterus turns inside out due to the delivery of the fetus or the placenta. Factors that contribute to inversion are application of traction to the umbilical cord to remove the placenta, if pressure is applied to the uterine fundus when the uterus is not contracting, or if the placenta is attached to the fundus so during birth the fundus pulls it down. Signs of inversion include sudden gush of a large amount of blood from the vagina, a non-palpable fundus, signs of blood loss such as hypotension, dizziness, and paleness, and if bleeding continues, exsanguinations. The inversion should never be replaced and the placenta, if still attached, should never be removed. Administration of oxytoxic drugs could only worsen the inversion and make the uterus tense so that it is difficult to replace. To manage uterine inversion, an IV line with a large-gauge needle should be established to restore fluid volume, oxygen administration should be started, assessment of vital signs, and cardiopulmonary resuscitation if the woman undergoes arrest. Nitroglycerin or a tocolytic drug would be given intravenously to relax the uterus, and the physician would replace the fundus manually. Oxytocin would be given after manual replacement to help the uterus contract and remain in its natural place. Antibiotics would be prescribed because the endometrium was exposed to prevent infection. Inform the woman that a future pregnancy would need to be delivered via cesarean section because there is a possibility that the inversion would re-occur. Amniotic Fluid Embolism Amniotic fluid embolism occurs when the amniotic fluid is forced into an open maternal uterine blood sinus or after membrane rupture or partial premature separation of the placenta. The most likely cause of the embolism is anaphylactoid or humoral response. Amniotic fluid embolism cannot be prevented because it cannot be predicted. Risk factors include abruption placenta, hydramnios, and oxytocin administration. The woman experiences sharp chest pain, inability to breathe, pallor, and lack of blood flow. Emergency measures include oxygen administration and CPR. The woman’s prognosis would depend on the speed of the detection of the condition, the skill and speed of the emergency interventions, and the size of the embolism. Endotracheal intubation and fibrinogen therapy would be needed because the risk for DIC is high. The prognosis for the fetus is uncertain because reduced placental perfusion happens from a severe drop in maternal blood pressure. Prolapse of the Umbilical Cord In prolapsed of the umbilical cord, a loop of umbilical cord slips down in front of the presenting fetal part. Factors that occur with prolapse are a small fetus, placenta previa, CPD, premature rupture of membranes, hydramnios, and multiple gestation. During assessment of the presenting fetal part through vaginal examination, the cord might be felt. Diagnosis of prolapsed of the membrane can be made through ultrasound. Cesarean section should be performed before rupture of the membrane or the cord would slide down the vagina. However, cord prolapsed is mostly discovered after rupture of the membranes, when the fetal heart rate has a variable deceleration. Assessment of fetal heart sounds is necessary after rupture of membranes to rule out cord prolapse. The goal in therapeutic management is to relieve cord compression to avoid fetal anoxia that can be achieved through manually lifting the head of the fetal head off the cord through the vagina or placing the woman in a Trendelenburg position. Oxygen administration is also necessary to improve the fetal oxygenation. Uterine activity and pressure of the fetus should also be reduced through a tocolytic agent. Once the cord has prolapsed and is exposed to air, drying of the umbilical cord and atrophy of the umbilical vessels would begin. Cover any exposed portion of the cord with a sterile saline compress to avoid drying. If there is already complete dilatation, the physician can deliver the baby to prevent fetal anoxia. If the cervical dilatation is not yet complete, cesarean birth would be performed as an emergency procedure because of the reduced blood flow that can harm the fetus. Amnioinfusion, which is the addition of a sterile fluid into the uterus to supplement the amniotic fluid, can be performed just to prevent additional cord compression. During the infusion, monitor the fetal heart rate and uterine contractions internally and record maternal temperature hourly to detect infection. Multiple Gestation When a woman has multiple gestation, additional personnel are needed for the birth and there is excitement inside the birthing room. Be aware of the needs of the woman during a multiple birth because she may be more frightened than excited of the delivery. Multiple gestations often result in fetal anoxia on the part of the second fetus, so cesarean birth is more preferable than normal delivery. Anemia and pregnancy-induced hypertension mostly occur in women with multiple gestations, so assessment of the blood pressure and hematocrit is necessary. If the woman plans to give birth vaginally, she should be advised to come to the hospital early in labor. Instruct the woman breathing techniques to minimize the use of analgesia or anesthesia, thereby decreasing the possibility of respiratory difficulties that the infants might experience because of lung immaturity. There may not be firm head engagement for multiple gestations because the babies are small. Common conditions that occur with multiple gestations are abnormal fetal presentation, an overstretched uterus, premature separation of placenta, and uterine dysfunction due to a long labor. Twin pregnancies usually have vertex presentations, but in gestations with three or more fetuses, the presentations are varied. Oxytocin is administered after the birth of the last fetus unlike in singleton pregnancies to avoid compromising the remaining fetuses. If the next fetus does not have a vertex presentation, external version might be attempted to make it vertex or cesarean birth can be performed. To shorten the time span between births, an oxytocin infusion can be started. To relax the uterus, nitroglycerin may be administered. The first infant’s placenta separates before the birth of the second fetus which causes a sudden, profuse bleeding at the vagina, creating a great risk for the woman. If the separation of the first placenta causes loosening of the other placentas or there is a common placenta, the fetal heart rate of the other fetuses would signal distress. Most multiple gestations today which are not in vertex presentation are born through cesarean section because they need to be born all at once so they can survive. Parents should be given an opportunity to view and inspect their fetuses to dispel the fears that they have that their infants are less than perfect. Assess the woman thoroughly and immediately after birth because an overly distended uterus might have difficulty in contracting, placing her at risk for hemorrhage due to uterine atony. Infants also need careful assessment to determine their gestational age and if any unusual conditions have occurred. Ineffective Uterine Force Ineffective labor occurs when uterine contractions become abnormal or ineffective, as uterine contractions are the basic force behind moving the fetus through the birth canal. Hypotonic Contractions The number of uterine contractions in hypotonic contractions is unusually slow or infrequent. There are only two or three contractions occurring within a 10-minute period. The strength of contractions does not rise above 10 mmHg, and they occur mostly during the active phase of labor. Hypotonic contractions occur after administration of analgesia, bowel or bladder distention, if the uterus is overstretched due to multiple gestation, a large fetus, hydramnios, or a uterus that is lax from grand multiparity. Hypotonic contractions increase the woman’s risk for postpartal hemorrhage. In the first hour after birth following a labor of hypotonic contractions, palpate the uterus and assess the lochia every 15 minutes to ensure that there are no postpartal hypotonic contractions and inadequate to halt bleeding. Hypertonic Contractions Hypertonic contractions are marked by an increase in resting tone to more than 15 mmHg. Hypertonic contractions tend to occur more frequently and during the latent phase of labor. They are more painful than usual, and they make the woman frustrated with her breathing techniques because they are ineffective. The lack of relaxation between contractions may not allow optimal uterine artery filling that could lead to fetal anoxia. A uterine and fetal external monitor should be applied for at least 15 minutes to check the resting phase of the contractions and that the fetal pattern is not showing a late deceleration. Cesarean birth would be necessary if there is late deceleration, an abnormally long first stage of labor or lack of progress with pushing. Explain to the woman and her partner that although the contractions are very strong, they are ineffective and are not achieving cervical dilatation. Uncoordinated Contractions More than one pacemaker may be initiating contractions with uncoordinated contractions, or receptor points in the myometrium may be acting independently of the pacemaker. It would be difficult for the woman to rest between contractions because they occur erratically. A fetal and uterine external monitor must be attached to the woman to assess the rate, pattern, resting tone, and fetal response to contractions for at least 15 minutes. Oxytocin administration can also be done to stimulate a more effective and consistent pattern of contractions with a better, lower resting tone. Dysfunctional Labor Dysfunctional labor during the first stage involves prolonged latent phase, protracted active phase, prolonged deceleration phase, and secondary arrest of dilatation. Prolonged latent phase can be managed through helping the uterus to rest, providing adequate fluid for hydration and pain relief. Oxytocin is prescribed during a protracted active phase to augment labor. Cesarean birth would also be necessary in a prolonged deceleration phase. In secondary arrest of dilatation, there is no progress with cervical dilatation for more than 2 hours, and then cesarean birth would be necessary. Dysfunction during the second stage of labor involves prolonged descent and arrest of descent. If the rate of descent is less than 1 cm/hr in a nullipara or 2.0 in a multipara, then there is prolonged descent of the fetus. Encourage the woman to rest and increase her fluid intake. Intravenous oxytocin may also be administered to induce the uterus to contract effectively. A semi-Fowler’s position, squatting, kneeling, or more effective pushing may speed up the descent. When no descent occurs for 1 hour in a multipara and 2 hours in a nullipara, there is an arrest of descent. The most likely cause of arrest of descent in the second stage of labor is CPD, so cesarean birth is necessary. Oxytocin could also assist labor if there is no contraindication to vaginal birth. Precipitate Labor Precipitate labor occurs when uterine contractions are so strong that a woman gives birth with only a few and rapidly occurring contractions. Grand multiparity facilitates this kind of labor, or it can also happen after induction of labor by oxytocin or amniotomy. Subdural hemorrhage for the fetus may occur from the rapid release of pressure on the head. The woman may also obtain lacerations of the birth canal due to forceful birth. If the rate is greater than 5 cm per hour in a nullipara or 10 cm/hr in a multipara, precipitate labor is already occurring. Caution a multipara by her 28th week that her labor might still be brief if she has had a brief labor in the past to allow the woman to plan her transportation. A birthing room must be converted to birth readiness before full dilatation is obtained. Comfort and Pain Management Etiology and Physiology of Pain Pain is a basic protective mechanism that alerts a person that something threatening is happening somewhere in the body. Involuntary muscles do not normally cause pain when contracting, which is why uterine contractions are unique. Blood vessels constrict during contractions, reducing the blood supply to uterine and cervical cells resulting to anoxia of the muscle fibers. The anoxia causes the pain just like what happens in a heart attack. Ischemia to the cells increases as labor progresses, and anoxia also increases leading to intense pain. Another explanation for the pain is the stretching of the cervix and perineum. The moment that the stretching of the cervix is complete, the woman would feel the strong urge to push, and the pain disappears as the woman pushes. The pressure of the fetal presenting parts to the tissues also contributes to the discomfort that the woman is feeling. Cultural differences also determine the way a woman may perceive the pain. Pain sensations start in nociceptors which are stimulated by mechanical, chemical, or thermal stimuli. As they are stimulated, chemical mediators help transmit the pain impulse along myelinated and unmyelinated fibers to the spinal cord. Neurotransmitters assist the pain impulse across the synapse between the peripheral and the spinal nerve. The pain impulse ascends the spinal cord to the brain cortex where it would be interpreted as pain. The Melzack-Wall gate control theory of pain proposes that pain can be halted at three points: the peripheral end terminals, the synapse points, or at the point where the impulse is interpreted as pain. The major action of pain medications is to block the spinal cord neurotransmitters to halt the pain impulse from crossing towards the spinal nerve. Comfort Measures Relaxation Relaxation is mostly taught in preparing for childbirth classes. Relaxing keeps the abdominal wall from becoming tense and allows the uterus to rise during contractions without pressing against the abdominal wall. As the woman focuses on relaxing, it will also serve as a distraction technique because it distracts her from the pain she is feeling. Advise the woman to find her position of comfort during labor as it will greatly help her to relax. Another way for the woman to relax is to listen to her favorite music or do aromatherapy while inside her birthing room. Focusing and Imagery Focusing is concentrating intently on an object that will serve as the distraction. It also keeps the sensory input from reaching the cortex of the brain, thus avoiding pain. A photograph would be used by the woman and she concentrates on it during contractions. Avoid disturbing the woman by asking questions while she is focusing because it would break her concentration. Prayer There are women who find prayers comforting whenever they are in a stressful situation. Worship objects such as Bibles, rosaries, and crosses could give comfort to a woman during labor. Be careful in changing the sheets because the worship objects might be thrown away; these are sacred to the woman. Breathing Techniques Most preparing for childbirth classes also teach breathing techniques or patterns. Breathing techniques help relax the woman’s abdomen during contractions. It can be considered as a distraction technique because the woman concentrates on slow-paced breathing instead of minding the pain. Breathing techniques are best taught to the woman before labor, but if she is not familiar with it, she can still be coached even while she is in labor. Herbal Preparations There may be little evidence that shows the effectiveness of herbal medicines against pain during labor, but it is still widely used by some women. Raspberry leaves, life root, and fennel are some of the examples of these herbs. Heat or Cold Application Women who are experiencing back pain during labor will find heat application to their lower backs soothing. After labor, a cool cloth to the forehead could also soothe the woman from too much exertion. Ice chips also help relieve the dryness of the woman’s mouth during labor. Therapeutic Touch and Massage Therapeutic touch is the use of touch to comfort and relieve pain. According to its philosophy, the body contains energy fields. If the energy fields are plentiful, it results to good health. If the energy fields are few, it results to ill health. Therapeutic touch redirects the energy fields that lead to pain through the laying of hands. The release of endorphins is increased as touch or massage is applied, leading to decrease in pain. Effleurage is a form of therapeutic touch taught at Lamaze classes and is especially helpful during the first and second stages of labor. Pharmacologic Measures Narcotic Analgesics Narcotics have potent analgesic effects but are used cautiously because they can cause fetal CNS depression. Women in preterm labor should not have any narcotics as pharmacologic measure because of the lung immaturity of the fetus. Meperidine is an advantageous drug during labor because of its sedative and antispasmodic effects which relieve pain and helps relax the cervix. Meperidine is given 3 hours before birth to allow the peak action of the drug in the fetus to pass by the time of birth. Regional Anesthesia Regional anesthesia involves the injection of a local anesthetic to block specific nerve pathways. Research has proven that some effects of the anesthesia to the fetus result to fetal heart rate decelerations and symptoms of flaccidity, bradycardia, and hypotension in the newborn. Regional anesthesia allows the woman to stay awake and aware of the happenings during birth. It also helps prevent postpartum hemorrhage as it does not depress the uterine tone, so the uterus remains capable of contraction after birth. Local Anesthesia Local anesthesia reduces the ability of local nerve fibers to conduct pain. Local infiltration uses the injection of a local anesthetic into the superficial nerves of the perineum. The effect lasts for 1 hour, which allows for a pain-free birth and suturing of episiotomy. The pudendal nerve block is the injection of an anesthetic near the right and left pudendal nerve at the level of the ischial spine. This anesthetic provides pain relief after 2 to 10 minutes for 1 hour. FHR and the maternal blood pressure should be checked immediately after injection to detect maternal hypotension. The types of pain relief during labor and birth vary widely, and it is up to the woman if she would want to employ these measures during the right time. Proper education and information from the healthcare providers is a must so that the couple could make the right decision when it comes to the procedures and measures that they would want during labor and birth. Fetal Position, Presentation, Size, & Passage A pregnant woman would always want the best for the fetus growing inside of her. However, when problems arise regarding the welfare of the growing fetus, she may feel fear and anxiety. This is where healthcare providers enter the scene, to educate and assist the woman in caring for her fetus and also herself. Occipitoposterior Position The usual fetal position is posterior rather than anterior. Assuming that the presentation is vertex, the occiput is directed diagonally and posteriorly, either to the left or to the right. During internal rotation in these positions, the fetal head must rotate through an arc of approximately 135 degrees. Rotations from a posterior position can be aided by having the woman assume a hands-and-knee position, squatting or lying on her side; however, this is tiring for women in labor. Posterior positions usually occur in women with android, anthropoid, and contracted pelvis. Posterior positions happen in dysfunctional labor patterns such as prolonged active phase, arrested descent, or fetal heart sounds heard best at the lateral sides of the abdomen. A head in the posterior position does not fit the cervix like a head in the anterior position does. This can be confirmed through vaginal examination or through ultrasound because it might cause umbilical cord prolapse. Labor is prolonged because the arc of rotation is greater. Pressure and pain would be experienced by the woman in her lower back owing to sacral nerve compression when the fetal head rotates against the sacrum. To relieve a portion of the pain, applying counterpressure on the sacrum by a back rub may be done, and heat or cold application can also help. To help the fetus rotate, the woman may lie on the side opposite the fetal back or assume a hands-and-knees position. The woman should void every 2 hours to keep her bladder empty and avoid impeding the descent of the fetus. The woman may also need an oral sports drink or IV glucose solution to replace glucose stores used for energy. Maternal exhaustion can cause uterine dysfunction, so a rotation of 135 degrees may not be possible if the contractions are ineffective or if the fetus is larger than average. The fetal head might arrest in the transverse position or there might be no rotation at all, so cesarean birth would be necessary. Provide reassurances to the woman that even though her labor is not “by the book” it is still within safe and controlled limits. Oversized Fetus Macrosomia or an oversized fetus weighs more than 4000 to 4500g, and this size may become a problem. Macrosomic babies are usually born to women with diabetes or develop gestational diabetes, and multiparas. Uterine dysfunction might result from an oversized fetus because of the overstretching of the fibers of the myometrium. The wide shoulders pose a problem at birth because it can cause fetalpelvic disproportion or uterine rupture from obstruction. Cesarean birth is necessary if the fetus is so oversized to be born vaginally. To compare the size of the fetus with the woman’s pelvic capacity, pelvimetry or ultrasound can be performed. If a macrosomic baby is born vaginally, there are high risks for cervical nerve palsy, diaphragmatic injury, or fractured clavicle due to shoulder dystocia. The woman is at risk for over because of the overdistended uterus and uterine atony. Shoulder Dystocia Shoulder dystocia occurs during the second stage of labor when the fetal head is born but the shoulders are too broad to enter and be born through the pelvic outlet. The woman is at risk for vaginal and cervical tears, while the fetus is at risk for cord compression between the fetal body and the bony pelvis. If birth is forced through the vaginal opening, the fetus would sustain a fractured clavicle or a brachial plexus injury. Shoulder dystocia usually occurs in women who have diabetes, in multiparas, and in post-date pregnancies. Shoulder dystocia is discovered often during the birth of the head and the shoulders lock beneath the symphysis pubis. Other conditions that may suggest shoulder dystocia are prolonged second stage of labor, arrest of descent, or when the head starts to crown, it retracts instead of protruding with each contraction. Instruct the woman to flex her thighs sharply on her abdomen (McRobert’s maneuver) to widen the pelvic outlet and allow the anterior shoulder to be born. Applying suprapubic pressure can also help the shoulder out from beneath the symphysis pubis. Breech Presentation Most fetuses are in a breech presentation early in pregnancy; however, by week 38, it turns into a cephalic presentation. The fetal head may be the widest single diameter but the fetus’ buttocks and legs take up more space. The fetus turns into a cephalic position mostly because the fundus is the largest part of the uterus, so the buttocks and the lower extremities are in the fundus. Types of breech presentation include complete, frank, and footling. Breech presentation increases the fetal risk for anoxia, traumatic injury to the head, fracture of the spine or arm, dysfunctional labor, and early rupture of membranes. Meconium present in the amniotic fluid is a sign of buttock pressure, and this can lead to meconium aspiration once the infant inhales amniotic fluid. Fetal heart sounds are heard high in the abdomen in breech presentation. Leopold’s maneuver and vaginal examination can determine breech presentation. Be certain to monitor the FHR and uterine contractions continuously to detect fetal distress early and provide prompt intervention. In a breech birth, the birth of the head is the most dangerous part because a loop of the umbilical cord that has passed down alongside the head may be compressed. Intracranial hemorrhage is another danger of breech birth because of the pressure changes that have occurred spontaneously. An infant born from a frank breech position usually extends his or her legs continuously during the first 2 or 3 days of life, so be sure to point out to the parents that this is normal. Face Presentation Face and brow presentations are called asynclitism or a fetal head presenting at a different angle than expected. In face presentation, the head diameter the fetus presents to the pelvis is often too large for birth to proceed. The back would be difficult to outline because it is concave. Face presentation can be determined through vaginal examination when the nose, mouth, or chin is felt as the presenting part or through ultrasound. Face presentation usually occurs in women with contracted pelvis, or placenta previa, in a relaxed uterus of a multipara, with prematurity, hydramnios, or fetal malformation. If the chin is anterior and the pelvic diameters are within normal limits, the infant can be born vaginally. If the chin is posterior, cesarean birth is the birth method of choice. Facial edema and ecchymosis are present in a baby born after a face presentation. Assess the patency of the infant’s airway closely. Reassure the parents that the edema is transient and will disappear after a few days. Brow Presentation The rarest among the presentations is the brow presentation. This presentation usually occurs in multipara women or in a woman with relaxed abdominal muscles. Obstructed labor occurs because the head becomes jammed in the brim of the pelvis as the occipitomental diameter presents. Cesarean birth would be necessary unless the presentation spontaneously corrects itself. Extreme ecchymosis on the face is also present in infants born after a brow presentation. Reassure the parents that the bruising over the same area as the anterior fontanelle is normal. Inlet Contraction Inlet contraction is the narrowing of the anteroposterior diameter to less than 11 cm or the transverse diameter to 12 cm or less. The usual cause is rickets in early life or an inherited small pelvis. If the fetal head engages during the 36th to 38th week of pregnancy, then the pelvic inlet is adequate. If there is no engagement in primigravidas, then either a fetal abnormality or a pelvic abnormality should be suspected. Every primigravida should have pelvic measurements taken and recorded before week 24 of pregnancy so that a birth decision can be made. In CPD, the fetus remains in a floating position which could further complicate the already difficult situation. If the membranes rupture, then the risk of cord prolapse increases greatly. Outlet Contraction Outlet contraction is the narrowing of the transverse diameter at the outlet to less than 11 cm. This is the distance between the ischial tuberosities, a measurement that is easy to make during a prenatal visit, so the narrow diameter can be anticipated before labor starts. This can also be assessed easily during labor. Trial Labor Trial labor refers to the determination of the progress of labor in a woman who has borderline inlet measurement with a good fetal lie and position. Trial labor may continue as long as the descent of the presenting part and dilatation of the cervix continue to occur. Monitor fetal heart sounds and uterine contractions continuously. Instruct the woman to void every 2 hours to aid in fetal descent. After the rupture of membranes, assess the FHR closely; if the fetal head is still high, there is an increased danger of prolapsed cord and anoxia in the fetus. Cesarean birth would be necessary if there is no progress in labor after 6 to 12 hours. If trial labor fails and cesarean birth is scheduled, provide an explanation about why cesarean birth is the best birth method. Women undergoing trial labor need to be reassured, as well as her support person, that cesarean birth is only an alternative, not an inferior, method of birth because the labor is not progressing. External Cephalic Version External cephalic version is the turning of a fetus from a breech to a cephalic position before birth. As early as 34 to 35 weeks external cephalic version can be done but the usual time is 37 to 38 weeks of pregnancy. Record FHR and ultrasound continuously during the procedure. The uterus should relax, so the administration of a tocolytic agent is done. The breech and vertex of the fetus are located and grasped transabdominally by the examiner’s hands on the woman’s abdomen. External cephalic versions can decrease the number of cesarean births necessary from breech presentations. Contraindications to the procedure include multiple gestations, severe oligohydramnios, vaginal birth, cord coil, and unexplained thirdtrimester bleeding which could be placenta previa. The feeling of pressure may be uncomfortable for the woman. Women who are Rh-negative should receive Rh immunoglobulin after the procedure in case bleeding occurs. Nursing Process During Labor and Delivery Assessment Assessment for delivery starts at the second stage of labor, which is the full cervical dilatation until the birth of the baby. This would be a crucial time since the mother would need to deliver her baby at this stage without any troubles and with her strength intact so she could push for a normal vaginal delivery. Assess the responses of the mother towards the intensity and duration of the contractions. Assess the comfortability of the mother with her birthing position. Assess her breathing techniques if they are effective or could add to the difficulty that the mother might be experiencing. Assess the ability of the support person to assist the mother during labor and birth. Assess the fetal heart sounds to make sure that there is no occlusion in the cord that could hinder fetal circulation. Assess if the environment is comfortable for both the mother and the baby. Diagnosis The difficulties that the mother may encounter during delivery are endless. Not all deliveries have gone smoothly, so every caregiver must be capable of whipping up a diagnosis and care plan immediately to assist the mother towards a safe and meaningful delivery. Pain related to intensity of uterine contractions Planning The place of birth must be prepared prior to delivery. For multigravidas, preparation of the room could start when the cervix has dilated to 9 to 10 cm. For primiparas, preparation of the birth place should start when the head has crowned to the size of a quarter. The newborn care area must also be prepared within the same room and include supplies for eye care, suction and resuscitation equipment, radiant heat warmer, sterile towels, and identification of the newborn. The mother should choose a position that will be most comfortable for her during birth. Alternative birthing positions today are the dorsal recumbent position, the lateral Sim’s position, squatting, and semi-sitting. A health care provider must be situated at the foot of the birthing table already so that the infant would not fall off if birth happened precipitously. Implementation Now that the care plan is already established, time to take some action and implement those interventions listed on your cheat sheet. If the client has a birth plan, make sure all health care providers are aware of her individual preferences. Encourage the mother to void before delivery to reduce the discomfort. Allow client to take ice chips or hard candies for relief of dry mouth. Provide a comfortable environment for both the mother and the baby. Allow the client to assume a birthing position of her choice as long as it is not contraindicated. Assist the client in venting out any emotions with regards to her delivery experience. Evaluation A care plan would not be complete if no evaluation was done to test the effectiveness of your plan. Client will be able to manage her discomfort using nonpharmacologic methods. Client will be able to identify other pain relief measures. Client has no signs of bladder distention and can void every 2 hours. Client states that she has reduced or no mouth discomfort. Client states that the environment is comfortable enough. Client reports that the delivery is a tolerable and highly meaningful part of her life