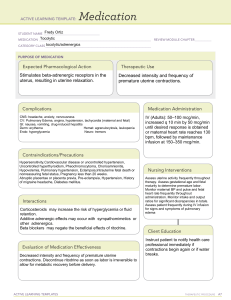
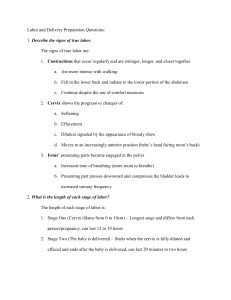
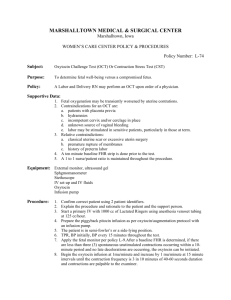
Exam 2 Notes: Chapter 12: Processes of Birth Stages of Labor: Full term baby is 37-42 weeks. Pre-term before 37 weeks. 4 Stages of labor: Stage 1: uterine contractions: cervix dilation up to 10 cm. Stage 2: delivery of baby Stage 3: placenta delivery Stage 4: postpartum recovery stage Don’t let mother bleed to death. Usually 12-18 hours. 4 Signs of True labor before birth: 1. Mucus and blood 2. Water breaking: Amniotic sac ruptures. 3. True labor contractions: incr frequency that is regular and rhythmic. Increased intensity and duration. Does NOT decr with rest. Becomes more intense with walking. “Increases with intensity” 4. Cervix dilation: how wide is cervix opening: goal 10 cm. Dilation= door is opening. Progress change with effacement: Cervix gets thinner and shorter with contractions: 3.5 cm before labor. Elastic cervix that gets thinner and shorter measured in percentages from 0-100%. Stick a finger to find the percentage. Cervical effacement and dilation is only true diagnostic values indicative of true labor. Effacement and dilation occur concurrently during labor but at different rates. Side note: Lower Back pain with contractions “back labor” is when the baby is in” occiput posterior position.” “OP””Oh poop! not good!” back of baby’s head is against the maternal spine slow progression, long labor, and severe back pain. Need to move and groove to have baby change position. 2 interventions: Apply counterpressure to the sacrum during contractions. Reposition mother on hands and knees with birth ball and encourage to change positions every 30-60 minutes. UAPs can help with position changes. Nullipara: A woman that has never given birth. Woman who has not completed a pregnancy to at least 20 weeks of gestation. Completes most cervical effacement early in the process of cervical dilation. Para: Woman who has given birth after a pregnancy of at least 20 weeks’ gestation. Cervix is usually thicker than that of a nullipara at any point during labor. Maternal Cardiovascular System: Blood flow to the placenta decreases during a contraction. Vital signs are best assessed during the interval between contractions. Supine hypotension may occur during labor, if the woman lies on her back. The woman should be encouraged to rest in positions other than supine to promote blood return to her heart. Maternal Respiratory System: Increased depth and rate of respirations due to anxiety or pain Hyperventilation It may occur with rapid and deep breathing. Respiratory alkalosis occurs as she exhales too much carbon dioxide. She may feel tingling of her hands and feet, numbness, and dizziness. The nurse should help her slow her breathing and breathe into a paper bag or her cupped hands to restore normal blood levels of carbon dioxide and relieve these symptoms. Maternal GI: Reduced gastric motility. Results in nausea and vomiting Ice chips, ok Food is generally held incase anesthesia is req’d for C-section. Maternal hematopoietic System 500 mL normal blood loss for vaginal delivery Usually tolerate this loss well because the blood volume increases during pregnancy by 30% to 60% Levels of several clotting factors, especially fibrinogen, are elevated during pregnancy and continue to be higher during labor and after delivery. Provides protection from hemorrhage. Increases the mother’s risk for a venous thrombosis during pregnancy and after birth. Maternal Urinary System: Reduced sensation of a full bladder Could be due to anesthesia. Distention can contribute to discomfort. Full bladder can inhibit fetal descent by occupying space in the pelvis. 4P’s/5P’s: Passenger, Passageway, Power, & Position! Four major factors interact during normal childbirth: Occur in 1st and 2nd stage of labor when baby is being delivered. Passenger (baby) Depends on fetal head and body size. Positioning: Fetal attitude: how baby holds positioning, flexed is good, extended is bad. Best to have fully flexed or curled up and tucked tight chin to chest, rounded back, and flexed arms and legs. BAD flaccid indicative of CNS problem. Fetal Lie: Positioning of baby’s back in relation to moms back. Best for vaginal delivery: “Longitudinal Lie”. Both baby’s and mom’s body are parallel. High Risk: Breech Requires C-section. When the baby’s head does not present first. Happens with Transverse: ‘sideways baby” & Oblique: baby is at an angle. Complication: umbilical cord compression. A breech presentation occurs when the fetal buttocks or legs enter the pelvis first, which happens in approximately 3% to 4% of births. Breech presentations more common in preterm births, hydrocephaly (enlargement of the head with fluid), multiple gestations, abnormalities of the maternal uterus and pelvis, and with placenta previa (placenta in the lower uterus). 3 main types: Complete: buttocks present first with legs tucked in. Frank: butt presents first but legs are stretched up. Footling: Foot is first. Passenger Cont’d. Interventions to fix breech: ECV External Cephalic Version: method of turning the baby from breech to head down position while it’s still inside of uterus. Provider uses two hands to turn baby while it’s inside. If ECV doesn’t work, then use C-section. Presentation of the baby: Is what the world will see first. Cephalic presentation: Headfirst. Head feels diamond shaped and soft in the middle. Station: Fetus must descend into pelvic inlet. Descent- movement of fetus through the birth canal. The degree of descent is “Fetal Station” Degree of fetal descent into the pelvis. How far the baby has descended into the pelvis. Station 0: at the level of mom’s ischial spine. Negative station- the farther up baby is in pelvis. Positive Station-Farther the baby is down. Station -1 to -5: (Pelvic inlet) baby’s head is ABOVE mom’s ischial spine and baby is deeper inside the pelvis and inside mom. Station 0: Baby’s head is at ischial spine and engagement. Baby’s head is level with mom’s ischial spine is called Engagement: “Baby’s head is engaged and ready for labor”. The presenting part fully enters the pelvic inlet. Station +1 to +5: See crowning and emerging from the vagina baby’s head is coming out crowning and start pushing! Restitution: head external rotates as coming out of vagina Expulsion: baby’s shoulders exit the vagina Passenger also includes the placenta! Big complication: placenta previa: placenta blocks the cervix, preventing baby from coming out. Position of the baby in relation to mother’s pelvis. Best ROA: Right Occiput Anterior Baby’s head is down in the pelvis and facing the mom’s spine towards the right hip. Best: LOA Left Occiput Anterior Baby’s head is down facing the mom’s spine towards the left hip. “OA is OK!” Position mom on her left side to facilitate labor process. Bad position: “Sunny Side up” OP & OT Baby’s head is down but it’s at an angle put a ton of pressure on mom’s back causing complication “Back Labor” possible C-section. OP: Occiput Posterior (left or right) OT: Occiput transverse (left or right) Passageway: The birth canal depends maternal pelvis and soft tissues. If baby is too large for birth canal or if pelvis is not wide enough may need C-section. Bony pelvis more important to the outcome of labor than soft tissue. Most important in childbirth Inlet Midpelvis Outlet Power: “CDE” contractions, dilation, and effacement. Contractions to open the cervix. Contractions are the primary force that pushes the fetus through the maternal pelvis. Maternal pushing efforts During the second stage of labor (full cervical dilation to birth of the baby), uterine contractions continue to propel the fetus through the pelvis. In addition, the woman feels an urge to push and bears down as the fetus distends her vagina and puts pressure on her rectum. Her voluntary pushing efforts add to the force of uterine contractions in second-stage labor. 3 Contraction Assessment: “FDI” “Contractions to open the cervix”. Frequency how often contractions occur, in minutes. 2-3 minutes apart for progressing labor is what is expected for contractions. Duration how long in seconds Typically lasting 60 seconds. Intensity How strong Measured by palpation or by an internal monitor. Contractions incr closer to delivery. Dilation: 10 cm fully opened. Avoid pushing until 10 cm! Pushing before can cause damage to baby’s head. Effacement: 100% thin, cervix is basically gone, so baby can pass through. Position: Position of the mother: Squat position makes labor easy. Promotes fetal descent. Psychological response of mother: Cultural considerations let pt. express pain in her way. Coping mechanisms: family or husband in room for support. Characteristics of contractions: Coordinated Involuntary Intermittent Interval Contraction cycle Interval is the period between the end of one contraction and the beginning of the next. The uterus should palpate soft during this time. Most fetal exchange of oxygen, nutrients, and waste products occurs in the placenta at this time. Contraction Cycle o Increment (period of increasing strength, occurs as the contraction begins in the fundus and spreads throughout the uterus). o Acme (peak, period during which the contraction is most intense) and will be over soon. o Decrement (period of decreasing intensity as the uterus relaxes) Side note: Labor contractions facilitate cervical dilation by pulling the cervix upward at the same time the fetus and amniotic sac are pushed downward. Blood flow decr to the uterus during a contraction. Contractions are stronger at the fundus. Internal size becomes smaller with the contractions, this helps push the fetus down. Side Note: The intensity of the contractions can be estimated by touching the uterus. The relaxed or mildly contracted uterus usually feels about as firm as a cheek. Moderately contracted uterus feels as firm as the end of the nose. Strongly contracted uterus is as firm as the forehead. Braxton Hicks Contractions: False labor contractions aka practice contractions Disappear with walking or position change. No dilation of cervix or changes. Irregular and alleviated with rest or changing position. irregular, mild uterine contractions that occur throughout pregnancy and become stronger in the last trimester. True Vs False Labor: True labor Increased contractions Increased discomfort Cervical change: progressive effacement and dilation most important Bloody show & water breaking False labor (prodromal or pre-labor) Contractions inconsistent Discomfort is more annoying than truly painful. Cervix does not change. Lightening Fetus descends toward the pelvic inlet (“dropping”), breathes more easily because upward pressure on diaphragm is reduced, increase pressure on bladder causes frequent urination. Increased vaginal mucus secretion – occurs as fetal pressure causes congestion of vaginal mucosa. Cervical changes Softening – cervix softens effects of hormone relaxin Possible dilation Bloody show Happens 2-4 weeks before delivery. 1st stage of labor includes early/latent phase, active phase, & transitional phase. Longest stage 20 hours, broken down into 3 phases. Begins with onset of true labor contractions ends with complete dilation of 10 cm. Phase 1: Early/Latent Phase: Client is relaxed, sociable and contractions are mild. 0-3 cm cervix dilation. Early education and encouragement. 0-30% effaced: thinner cervix- longest phase for 1st time mothers. As cervix begins to stretch it releases oxytocin which stimulates uterine contractions. Contractions are irregular, short, and far apart, every 5-30 min over the span of 30 seconds. Monitor fetal heart rate: Watch for late decelerations! not enough O2 getting to baby. Need fetal monitor. Phase 2: Active phase: breathing techniques are used, and client is irritable. Go to hospital! Breathing techniques and pain management. Cervix dilation: 4-7 cm and cervix cont. to thin Contractions stronger and longer: 3-5 min. Water may break and mom may feel restless and anxious. Patient wants pain meds. For the nullipara women the active phase can last 8-10 hours. Last change for epidural Can provide pain meds: Epidural: into space around spinal nerves in lower back. IV narcotics: Given slowly and at peak of contractions reduces amt of narcotic that crosses placental barrier. Phase 3: Transitional phase: cervix dilates to perfect 10, rapid intense contractions often with vomiting and urge to poop with intense moans and groans! Begins with onset of labor and ends with full cervical dilation at 10 cm. 8-10 cm of dilation but want 10 cm which cervix will be 100% effaced (fully thinned) Contractions stronger and closer. Loss of control and irritability. 5 key points: Anxiety and vomiting Urge to have bowel movement from pressure. Strong urge to push. Do not push until 10 cm dilated. (Fully dilated) risk for cervical swelling and lacerations if you push too early. Amniotic sac ruptures “bloody show” thick bloody mucus happens when cervical dilation and or effacement has occurred. Assess color of amniotic fluid Meconium-stained fluid (dark fluid)- signs of fetal distress or hypoxia, BIG aspiration risk. 2nd stage of labor: -Delivery of the baby AKA descent or pushing phase. Expulsion begins with complete 10 cm dilation and 100% effacement of cervix, ends with birth of the baby. Increase in contractions. Ferguson Reflex: spontaneous urge to push during labor. Happens when presenting part of the fetus reaches the pelvic floor. You want to bear down. Interventions: Positioning of mother is priority: high fowlers, lithotomy, or side lying. Educate client to push properly: Avoid holding breath or tightening of the abdomen. Push when feeling the urge. Breathe in deep and breathe out slowly through the mouth & keep mouth open while pushing down to help incr oxygen to fetus. Assessments: Fetal HR before, during, and after the contraction. Frequency of the contraction Duration of contractions Uterine tone between contractions 3rd Stage of Labor: -Placenta delivery Uterus contracts & placenta slowly detaches from uterine wall. You will see a gush of blood appear, uterus rises upward in abdomen, the cord descends further from the vagina. Remove placenta carefully: NEVER pull on the cord. Don’t want to rip the placenta into two parts leaving it inside the mom and to prevent uterine inversion, entire uterus flips inside out which is a big risk for infection and hemorrhage decr BP, incr HR-shock. Pharm after placenta delivery: P=placenta, P= Pitocin (oxytocin) to prevent hemorrhage. Oxytocin stimulates uterine contractions, helps uterus to contract to stop bleeding. 4th Stage of labor: -Recovery period Can last 2-4 hrs. after birth. Encourage skin to skin and breast feeding. Breast feeding stimulates maternal oxytocin release which helps to contract uterus, provides nourishment, and supports blood sugar of the newborn. Assessments for mother: Priority on blood loss and infection Temp >100.4, slightly elevated after delivery is normal. Hemorrhage: PRIORITY: monitor peri pads Fully saturated in <1 hr or 1 pad in 15 mins or 1 pad every 5 mins hemorrhage. Also monitor decr in BP and incr in HR Shocky. Interventions: Check fundus first: Top portion of uterus. Boggy: massage until firm so it contracts and stops bleeding. Encourage voiding or use straight catheter since a full bladder can displace fundus which can stop fundus from contracting to stop bleeding. Pitocin (oxytocin) IV or IM to control bleeding after childbirth. Breast feeding- stimulates natural release of oxytocin. Uterine involution occurs as uterus returns to prepregnant size and location and can take 15-21 days after delivery. Fundus assessment is key to help stop bleeding; it must be firm. Assess 3 times every 5 mins then every 15 mins for a full hour. Fundus Assessment: Normal fundus should be firm, midline, and level with the umbilicus. 12 hrs after it should be at 1 cm above the umbilicus then will descend 1-2 cm every 24 hours. NOT NORMAL: displace fundus above umbilicus or to one side typically from bladder distension/ a full bladder. Intervention: Ask client to void every 2-3 hours, bed pan preferred, if client has been given pain meds. If client can’t void use in/out catheter/straight cath. Soft or boggy fundus uterine atony, increases the risk for hemorrhage. Uterine atony: soft and weak uterus after childbirth. Give oxytocin infusion Contracts uterus to Control bleeding. Fundal massage to make fundus firm. Methergine: analgesic and uterotonic used to treat severe bleeding from the uterus after birth BUT it drastically increases BP and cannot be used safely with mothers that have HTN or preeclampsia. Lochia: Normal discharge after birth should get lighter with each postpartum day passing. Red (rubra)lasts 3-4 days, small clots are expected. Pink/brown (Serosa) 4-10 days, mucus, fewer clots White/clear (alba) 10-28 days or longer, cream color, no foul order or real flow. Sudden gush of blood means lochia pooled in client’s vagina. Not normal: Large clots Foul odor Excessive bleeding 1 pad in 15 mins. Peri care (Recovery) Use squeeze bottle with warm water. Wipe front to back Blot peri area dry. Pain: Give sitz baths. Ice packs Pharm opioids and nsaids: Topical witch hazel helps with swelling and hemorrhoids. Laxatives and stool softeners to help prevent constipation. Molding: can cause the baby’s head to look cone shaped The sutures and fontanels allow the bones of the fetal head to move slightly, changing the shape of the fetal head so it can adapt to the size and shape of the pelvis. Lightening is the descent of the fetus toward the pelvic inlet before labor. Lie is the relationship of the long axis of the fetus to the long axis of the mother. Presentation is the fetal part that first enters the pelvic outlet. Chapter 13: Pain Management During Childbirth: Non-pharmacological Interventions: Includes breathing techniques. Imagery Massage: effleurage Back labor pain: Sacral counter pressure: applying pressure to sacral area. Monitor for nonverbal signs for ineffective coping with labor: Panic Anxiety Squirming movements Some cultures are stoic. Pain medication: -includes sedatives & opiates Best given during early stages of labor as they can cause serious side effects like resp depression. Give 2-4 hours before birth, So, drug has time to wear off before birth. Sedatives: Barbitutes, IV Phenobarbital Caution: resp depression in baby esp when given close to birth. Opiates: Meperidine hydrochloride Butorphanol tartrate: Stadol Nalbuphine hydrochloride: Nubian -These 2 meds are mixed agonists-antagonists opiate analgesics with less abuse potential. ONLY give opiates during contractions after the cervix is 4cm dilated or it will slow labor. Low and slow vitals: monitor for low BP, HR, and slow RR. Assess fetal HR 10 mins prior and maternal vital signs. Have Naloxone present. Epidural Anesthesia AKA epidural block: Injection into lower back that blocks pain from waist down belly button to legs Takes 20-30 mins to reach full effect. Only given after cervix is 4 cm dilated. Do not give before. Not possible to give in late 2nd stage of labor. Clients lie on side with knees tucked in or sit up and lean forward to open space between bones in spine. Provider places Needle into epidural space: between dura mater and vertebral wall just outside spinal cord. Caution: causes maternal hypotension. Monitor for dizziness. If mom is hypotensive baby isn’t being perfused either will see fetal bradycardia and low platelet count in mother, <150k is a bleeding risk. Adverse effects Maternal hypotension Bladder distention Prolonged second stage Catheter migration Cesarean birth Maternal fever N/V, pruritis, shivering, respiratory depression Spinal Anesthesia AKA Spinal block Works same as epidural but are more powerful used for C-section. 100% loss of motor movement and loss of sensation. Higher risk for low BP in mother and fetal bradycardia Epidural and Spinal block Interventions: Give IV fluids to counteract side effects of maternal hypotension. Nurse action for maternal hypotension: Turn mother to the left lateral position and incr IV fluid rate. Pudendal Nerve Block: Injects local anesthesia like lidocaine into areas of tissue that surround pudendal nerve in lower vagina perineum, vulva, and rectum. Good at blocking pain from vaginal tears and episiotomy. Episiotomy: provider surgically cuts perineum to aid in the delivery of the baby. Good: can be given quickly when birth is imminent, best pain relief with least amt of side effects. Bad: does not relieve contraction pain but it relieves perineal pressure and sharp pain R/T tears. Ch 14: Intrapartum Fetal Surveillance Heart Rate Monitor: Fetal Monitors fetal oxygenation and well-being during labor. Important to monitor uterine contractions and baby’s heart rate. 2 Types of Devices Used: External fetal monitoring: Sono aka ultrasound used for baby’s heart rate. Toco Meter: Used for mom’s uterine activity. External Fetal Monitor: Find the point of maximal impulse “PMI” baby’s heart rate can be heard the loudest. It is found between the baby’s shoulder blades. Best place to put fetal heart rate sensor. If the baby is cephalic or head down, it will be placed on mother’s lower abdomen. If the baby is breech it will be placed on the upper abdomen to find the PMI. 2nd sensor is contraction monitor sensor to monitor contractions. More accurate but invasive method is Internal fetal monitor. “Fetal Scalp electrode “FSE”: Only used for high-risk pregnancies Requires cervical dilatation and ruptured membranes. Electrodes applied directly to fetal presenting part (head or buttocks) Most accurate since it is not affected by movement. Accurately displays FHR between 30 and 240 bpm. Only can be used after amniotic sac has ruptured and cervix is open at least 2 cm. High risk of infection since it goes through mom’s vagina then onto baby’s head. FSE Limitations: Requires ruptured membranes. Cervix must be dilated sufficiently to allow placement. Improper insertion can cause maternal trauma such as vaginal lacerations. Presenting part must be accessible and identifiable. May record maternal HR in presence of fetal demise. May not have adequate ECG conduction when excessive fetal hair is present. Possible increased risk for infection Intrauterine pressure catheter (IUPC) Sterile, flexible catheter inserted directly into the uterus transcervically Measures uterine contractions and actual uterine pressure in millimeters of mercury (mm Hg) Measures strength/intensity of contractions. Only true accurate measure of all UA (uterine activity). Allows for use of amnioinfusion. IUPC Limitations: Requires ruptured membranes. Cervix must be dilated sufficiently to allow placement. Improper insertion can cause maternal or placental trauma such as uterine perforation or placental abruption. Maternal position may change uterine hydrostatic pressure resulting in inaccurate readings. Different IUPC types may give higher pressure readings than other types. Possible increased risk for infection Fetal Heart Rate: Normal 110-160 BPM Variability: How wiggly the line is on the strip, as labor progresses the line becomes squigglier, which is good & baby’s neuro system is intact. “The wigglier the line is, the happier baby is”. Red Light: Absent variability: Not Jiggly=Not good! Means the baby is not responding and is at risk for major complications. Means the baby needs to come out right now via C-section. Yellow light: Minimal Variability: Flatter line, that looks sleepy and sad. Baby is sleeping or in trouble. Green light: Moderate Variability: This is a normal and desired finding! Marked Variability: Jagged lines/jiggles means stressed baby! Marked Variability Typically seen during labor as baby is being pushed out. Accelerations: Temporary increases in FHR. Indicates great oxygenation for the baby. “Happy little mountains” Baby gets A’s for Accelerations Baby’s strip is onto and mom’s contractions on bottom. Decelerations: “Dips from baseline” 3 diff types and look at shape and timing with each contraction. Green Light: Early Decels: Shallow bowel shaped dips that mirror mother’s contraction/look attracted to each other. Indicates head compression. “Good to be early with earl decels” Yellow: Variable Decels= Very Concerning Look for the V’s! “Very concerning with sharp V dips”. Indicates cord compression that cuts off oxygen to the fetus. Want to change mom’s position and consider amnioinfusion if position change doesn’t fix problem. Position should be in a knee-chest position. Red: Late Decels= LETHAL!! Indicates decr oxygenation (hypoxia) Comes right after uterine contraction. They don’t line up. Late Decels= late deoxygenation, the FHR decreases with decels. Key Term for Uterine Contractions: During contractions baby holds their breath and fetal oxygen is impaired. Frequency: Measures how far apart the contractions are. Starts at the beginning of one contraction to the beginning of the next. Measured in minutes. Duration: How long the contractions last. Count small boxes under the “hill” of the contraction. Measured in seconds. Intensity: How strong the contractions are. mmHg To Determine: External Monitor: Nurse palpates the uterine tone. Internal Monitor: Nurse counts and charts pressure units. Rest: Tone and Time Uterus should be soft to palpation between contractions for at least 60 seconds. As baby needs to recover for loss of oxygen flow during contractions. Normal Contractions: “Rule of 60” Frequency: contractions that are 2-3 min apart in active labor. Duration: should be 60 seconds Intensity: should be 60 mmHg. Anything >90 is a cause of concern. Rest: should be 60 sec of rest in between contractions. Complications: TachysystoleMore than 5 contractions in 10 mins= BAD! Too many contractions leads to fetal distress. Such as hypoxia and reduced placental blood flow. Look at bottom strip for contractions. Fetal Accelerations & Decelerations: “VEAL CHOP” For L & P Late Decelerationsplacenta insufficiency, BAD! Think ROADI “Road to recover”. R: Reposition Mom O: Oxygen via Face Mask A: Alert the provider. D: Discontinue oxytocin and give tocolytics like Terbutaline, helps to slow turbulent contractions, esp since oxytocin increases contractions! I: Increase IV fluids! 7 Strip Review: 7 STRIP Review: Normal FHR: 110-160 BPM Baseline is between contractions. Accelerations: Temporary incr in FHR. Which is A-OK! Means you have good oxygenation. Early Decelerations: Mirror contractions with decr FHR during contractions which is ok! Cause: head compression during contractions, means baby is ready for delivery. Present or absent early decels are normal/reassuring. NOT Reassuring & are RISKY: Fetal Tachycardia: Incr in FHR >160 BPM for over 10 mins. Anything less is considered an acceleration, which is good/normal. Early sign in fetal distress. Also used as a compensatory mechanism when baby undergoes a stressor from various causes requiring baby to use more oxygen. Causes: Trauma to the mother a broken bone. Maternal infection or fever Fetal anemia Dehydration Use of stimulants (cocaine) Interventions: Oxygen IV fluids Antipyretic meds: if mom has a fever. Fetal Bradycardia: Decr in FHR <110 BPM for over 10 mins. Anything less than 10 mins is considered a deceleration. Causes: Uteroplacental insufficiency Umbilical cord prolapse. Maternal hypotension Use of analgesic meds which makes vitals low and slow. Fetal Bradycardia: Interventions: “ROADI” Reposition mom on side to incr mom’s cardiac output never supine. Which compresses aorta and causes decr placental perfusion. Oxygen via face mask. Alert HCP Discontinue oxytocin Priority! Incr IV fluids to incr blood volume and cardiac output which incr oxygen supply to fetus. Variable decelerations: Abrupt decr in FHR Deep dips and long drops like V’s. Drops that are <30 seconds from onset to baseline and 15 BPM below basline for 14 sec to 2 mins. Causes: Umbilical cord compression critical since baby’s oxygen tube is being compressed and baby can run out of oxygen. Decreased amniotic fluid can incr amniotic fluid with an amnio infusion. Interventions: ROADI Amnioinfusion: Installation of sterile saline into amniotic cavity to refill the lost fluid. This is done after multiple position changes did not relieve cord compression. Amnioinfusion requires instillation of isotonic fluid, such as lactated Ringer’s solution or normal saline, through an IUPC into the uterus to restore amniotic fluid volume to normal or near-normal levels (Miller, 2016). The physiologic principle behind amnioinfusion is that decreased amniotic fluid, oligohydramnios, can cause interruptions in the oxygen pathways via umbilical cord compression, which can lead to variable or prolonged decelerations. By replacing fluid, umbilical cord compression may be relieved, resulting in optimal blood flow through the umbilical cord vessels with oxygenated blood. Indications for over filling with amnioinfusion: Report immediately! Uterine resting tone that incr to 45 mm Hg. Overfilled uterus can lead to complications from too much pressure uterine rupture or labor dystocia. Late Decelerations: These are the worst! Decr FHR after contractions with prolonged time before returning to baseline, around 60 seconds. Indicates oxygenation is compromised. FHR cont to decr beyond end of uterine contraction. Causes: Placental insufficiency Uteroplacental insufficiency Uterine tachysystole side effect of oxytocin causing severe contractions. Leads to reduced placental blood flow and impaired fetal oxygenation. Stop oxytocin. Contractions are over 5 contractions in 10 minutes or late decels. Hypotension can also cause late decels. Interventions: ROADI Prepare for C-section if late decels persist after ROADI. Sinusoidal FHR VERY bad! Critical finding, notify ASAP and do something ASAP. Repetitive, wave-like fluctuations (hills) with NO variability and NO response to contractions. Baby can die from lack of oxygen. MOST DEADLY Causes: Mother can have abdominal trauma from a fall or MVA leads to fetal blood loss or anemia. Rh incompatibility which can cause hemolysis. Interventions: Emergency C-section. Fetal HR interpretation: Baseline FHR variability (10 min window) Factors that decrease. Classification of variability – defined as fluctuations in baseline FHR that are irregular in amplitude or frequency. • Absent – amplitude undetectable • Minimal – 5bpm or less amp • Moderate - amp range 6bpm to 25 (predicts absence of fetal metabolic acidemia) Marked – amp 25 or greater (considered normal) Absent/minimal does not confirm hypoxic injury or acidemia because baby could be sleep or other pathologic causes. Periodic and episodic FHR patterns Periodic: Associated with uterine contractions Episodic: Not associated with uterine contractions • Accelerations: abrupt increase in FHR, Periodic or episodic Peak 15bpm above baseline lasting 15 sec or more. • Decelerations Early (head compression): Periodic, symmetric in shape, gradual decrease mirrors uterine contraction Late (uteroplacental insufficiency, fetal hypoxia): Periodic, decel after peak of contraction – maternal lateral positioning Variable (cord compression): Periodic or episodic Prolonged: Periodic or episodic, 2-10mins Two guiding principles Variable, late, or prolonged decelerations indicate interruption of oxygen transfer from the environment to the fetus at one or more points. Moderate variability and/or accelerations reliably exclude ongoing hypoxic injury at the time they are observed. Amniotomy: Artificial Rupture of membranes: Indications Induce labor. Augment labor Allow internal fetal monitoring. Risks Prolapse cord. Infection Abruptio placenta Technique Done by physician or nurse-midwife. Amnio hook snags membrane Nursing considerations Obtain baseline information. Fetal heart rate (FHR) 20 to 30 minutes before procedure Assist with procedure. Place absorbent pads Equipment Provide care after procedure. Identify complications. Promote comfort. Categorization of Fetal Heart Rate Patterns: Standardized Intrapartum Interpretation and Management: Two guiding principles Variable, late, or prolonged decelerations indicate interruption of oxygen transfer from the environment to the fetus at one or more points. Moderate variability and/or accelerations reliably exclude ongoing hypoxic injury at the time they are observed. ABCD Approach to Fetal Heart Rate Management A: Assess oxygen pathway and identify the etiology of FHR changes, both maternal and fetal B: Begin corrective measures (intrauterine resuscitation) C: Clear obstacles to delivery D: Determine a delivery plan Commonly Performed Corrective Measures: Maternal repositioning improve fetal oxygenation and uteroplacental perfusion. Intravenous fluid boluses Administering oxygen Reducing uterine activity: Removal of prostaglandin cervical ripening agents Decreasing or discontinuing oxytocin Assessment to rule out conditions such as chorioamnionitis or placental abruption. Administration of a tocolytic agent such as a beta-sympathomimetic agent Correcting maternal hypotension Performing amnioinfusion Modifying second stage pushing efforts Chapter 15: Nursing Care During Labor and Birth: Admission to birth facility: Patient teaching when to go to hospital: Bleeding—Bright—red bleeding should be evaluated promptly. Normal bloody show is thicker, pink or dark red, and mixed with mucus. Decreased fetal movement—A substantial decrease in the baby's normal activity requires evaluation, your physician or nurse—midwife should be notified, or come to the labor unit. Other concerns—These guidelines cannot cover all situations and do not replace specific instructions given to you by your physician or nurse midwife. Therefore, go to the hospital for evaluation of any concerns and feelings that something may be wrong. These are guidelines for providing individualized instruction to women about when to enter the hospital or birth center. Contractions—A pattern of increasing regularity, frequency, duration, and intensity. Nullipara—Regular contractions, 5 minutes apart, lasting 1 minute, for 1 hour. Multipara—Regular contractions, 10 minutes apart, lasting 1 minute, for 1 hour. Ruptured membranes—A gush or trickle of fluid from the vagina should be evaluated, regardless of whether contractions are occurring or not. Nursing Responsibilities DURING Admission: Fetal heart rate (FHR): FHR 110 to 160 bpm Regular rhythm: Presence of acceleration; absence of deceleration Maternal vital signs: Identify signs of hypertension and infection. Impending birth: Grunting sounds Bearing down Urgency to push. Database assessment: Basic information Physical exam Fetal assessment Labor status Contraction pattern Establish if rupture of membranes. Admission procedures: Notify the provider. Give report. Obtain orders. Consent forms Laboratory tests Intravenous (IV) access Ongoing assessments Nursing Responsibilities AFTER Admission: Maternal assessments: Labor progress Contractions Intake and output Response to labor Support person’s response Fetal assessments: FHR Fetal membranes and amniotic fluid Nursing Process- Fetal Oxygenation: Assess at frequent intervals: FHR evaluation Amount and character of amniotic fluid and time of rupture Maternal vital signs Contractions: Frequency, duration, intensity, and relaxation interval and resting tone Identification of patient problems Planning Interventions Promote placental function. Observe for conditions associated with fetal compromise. Evaluation Fetal Compromise S/S: Fetal heart rate (FHR) outside the normal range of 110 to 160 bpm or loss of FHR variability with electronic FHR monitoring. Meconium—stained (greenish) amniotic fluid. Cloudy, yellowish, or foul—smelling amniotic fluid (suggests infection). Excessive frequency or duration of contractions (reduces placental blood flow). Incomplete uterine relaxation and intervals shorter than 45 to 60 seconds between contractions (reduces placental blood flow). Maternal hypotension (may divert blood flow away from the placenta to ensure adequate perfusion of the maternal brain and heart). Maternal hypertension (may be associated with vasospasm in spiral arteries, which supply the intervillous spaces of the placenta). Maternal fever (38°C [100.4°F] or higher). Discomfort: Assessment: Identification of patient problems Determine whether anxiety is contributing to discomfort. Planning: Pain relief is not a realistic goal. Goal is for positive birth experience. Interventions: Comfort measures • Lighting • Temperature • Cleanliness • Oral care • Bladder -Positioning Alterations in Normal Labor: Version Indications: External cephalic version Change the fetal position from a breech, shoulder (transverse lie), or oblique presentation to cephalic. An ECV (changing the fetal presentation from breech to cephalic) is more successful when the pregnancy is at least 37 weeks and there is still adequate room and fluid to manipulate the fetus but prior to term or onset of labor. A low-lying placenta, previous cesarean birth, and uterine fibroids are contraindications for version. Internal version Change the position of a second twin in a vaginal birth. Version: Contraindications Uterine malformations Previous cesarean birth Placenta abnormalities Third trimester bleeding Cephalopelvic disproportion Multifetal gestation Oligohydramnios Intrauterine growth restriction Uteroplacental insufficiency Engagement of fetal head into the pelvis Risks: Complications occur in 1% to 2% of attempted versions. Changes to FHR common, but usually return to normal. Serious risks to fetus: Umbilical cord entanglement Fetal hypoxia Abruptio placentae Maternal sensitization to fetal blood type Version: Technique - External cephalic version Nonstress test (NST) to evaluate fetal well-being. Determine gestational age beyond 37 weeks. Administer tocolytic drug to relax uterus. Use ultrasound to guide manipulations. Rho(D) immune globulin (RhoGAM) given if indicated. Induction and Augmentation of Labor: Artificial methods to stimulate uterine contractions. Inductions associated with higher cesarean rate. Focus on waiting until 39 weeks for elective inductions has reduced cesarean rate. Inductions of Labor Indications: Hostile intrauterine environment Spontaneous rupture of the membranes (SROM) Post term pregnancy Chorioamnionitis (infection and inflammation of the amniotic sac) Hypertension Abruptio placentae Maternal medical conditions that worsen with continuation of the pregnancy Fetal demise Inductions of Labor Contraindications: Placenta previa Vasa previa Umbilical cord prolapse. Abnormal fetal presentation Active genital herpes Previous uterine surgery Breech presentation Overdistended uterus due to multifetal pregnancy or polyhydramnios Severe maternal conditions such as heart disease and severe hypertension Fetal presenting part above the pelvic inlet. Inductions of Labor Risks: Excessive uterine activity Uterine rupture Maternal water intoxication Chorioamnionitis Cesarean birth Postpartum hemorrhage Induction and Augmentation of Labor: Techniques Determining whether induction is indicated. Cervical assessment (Bishop score) Cervical ripening Pharmacologic methods Mechanical methods Oxytocin administration Dilute in an isotonic solution. Secondary (piggyback) infusion. Insert oxytocin into the primary intravenous line. Start slowly, increase gradually. Monitor uterine activity, FHR, and fetal heart patterns frequently. Induction and Augmentation of Labor: Nursing Considerations Observe fetal response: Tachysystole reduces placental blood flow. Assess FHR pattern. Reduce or stop infusion for nonreassuring FHR. Side lying position. Oxygen by face mask Observe the mother’s response: Assess uterine activity. Assess blood pressure and pulse. Be aware of pain management techniques. Record intake and output. Observe for signs of water intoxication. Assess for uterine atony in postpartum period. PROM & AROM: PROM: water breaks too early and premature leakage of amniotic fluid. -Premature Rupture of Membranes, after 37 weeks. PPROM: Preterm Premature Rupture of membranes - Before 37 weeks. Risk Factors: Anything that weakens the strength of the chorioamniotic membrane. Infections that weaken membranes UTI, STI, bacterial vaginosis, smoking, abdominal trauma, prior distension-polyhydramnios- (increased amniotic fluid), & multiple gestations: twins/triplets +, pregnancy with more than one babies at a time, puts distension on amniotic membrane. Dx: Nitrazine Test vaginal fluid placed on paper changes from yellow to blue from pH >7 of amniotic fluid, not best test can change color due to infection or blood. Speculum exam “pooling”. Ultrasound Screen for STIs S/S: Pelvic pressure Sm. leakage of fluid Pink discharge Temperature 100.4 tx with antibiotics and/or antipyretics >37 weeks will go into spontaneous labor within 24 hrs. or should be induced since membranes have rupture incr risk for infection. Tx: Give prophylactic antibiotics to prevent GBS infection: Group B strep infection which can be transferred to baby GBS. Especially if: membranes ruptured at/over 18 hours, temp >100.4, gestation less than 37 weeks. AROM: Artificial Rupture of Membranes AKA Amniotomy Manually induce labor by rupturing the amniotic membrane aka breaking mom’s water. Risk: for umbilical cord prolapse fetal brady cardia due to cord compression if fetal head is not engaged in pelvis. Interventions: Assess fetal HR before and after 1st priority. Assist to upright position after AROM to ensure drainage. Supine is BAD which decr placenta perfusion. Temp done every 2 hrs. to spot infection. As well as amniotic fluid color, amt, and odor. After amniotomy assess fetal heart rate as priority! Non-Reassuring FHR patterns: FHR <110 BPM or >160 BPM Presence of repetitive or prolonged decelerations > 5 contractions in a 10 min period. Procedures to Assist Labor: Terbutaline: slows labor down “Gotta wait in line for the baby” Used for preterm labor, slows down, doesn’t stop labor. given for turbulent contractions in pre-term labor. Calms the uterus by activating Beta 2 receptors to activate sympathetic nervous system to suppress labor. Oxytocin: Given to induce labor and stimulate uterine contractions. “Tocin to contract”. Administer 6-12 hours after last dose of dinoprosone, which is a cervical ripening drug also used during labor. Watch mom’s uterine contractions, BP, and HR Monitor FHR continuously! Monitor contractions slowly should be < 60 seconds and 2-3 mins apart. Discontinue oxytocin if contractions are lasting longer than 60 seconds and maintain one on one care. Piggyback oxytocin into the main IV fluids. Turn the client to the side if late decelerations are noted. Priority action for 3 consecutive late decelerations=turn off oxytocin. Decels are expected with Demerol/merpidine (IV narcotic pain med). With minimal variability do not have to discontinue oxytocin. Stop Oxytocin: Contractions > 90 seconds Frequency <2 min apart, like contractions every minute Contraction intensity >90 mmHg, baby will get stressed. Resting tone >20 mmhg. Late decels in FHR >5 contractions in 10 mins uterine tachysystole. Oxytocin Complications: Uterine Rupture Late Decelerations Water intoxication – very low sodium dilutional hyponatremia. Increased risk for placental abruption Uterine atony soft boggy uterus, incr risk for PPH. Uterine tachysystole side effect of med causing severe contractions which causes reduced placental blood flow and impaired fetal oxygenation. Non-Pharm ways to induce Labor: Forceps: Spoon like device used to assist delivery. NEVER apply fundal pressure during forceps use! Can cause uterine rupture. Use: During fetal distress or abnormal fetal presentation. Complications: Uterine rupture Bladder injury- encourage mom to empty bladder or use catheter to empty bladder. Vaginal lacerations Vacuum: Traction applied to the fetal head. Never apply fundal pressure! The vacuum extractor is applied on the occipital bone and may create scalp edema at the application site. The posterior fontanel connects the occipital bone to the parietal bones. Use: When mother is unable to push or not pushing effectively from exhaustion or epidural. Fetal distress, rotation, or abnormal FHR. Complications: Uterine rupture Lacerations Infant subdural hematoma Bishop Score: Want a ripe cervix that is ready for change. Higher the Bishop score, the higher the readiness. Over 6-8 score, induction will be successful! A Bishop score of 10 is perfect A cervix that is firm and posterior is associated with a low Bishop score and has a low labor induction. Cesarean Birth: Performed after 28 weeks of gestation. Planned or unplanned (emergency). Top reasons for a planned: Previous C section Large baby or twins or triplets Genital herpes or other infections Placenta previa- placenta is covering cervix. Emergency C-section: Unplanned performed when emergency develops during labor or pregnancy. Fetal distress baby’s life is in danger. Placental abruption placenta detaches from the wall of the uterus. Prolapsed cord umbilical cord is compressed, limiting oxygen to the baby. Long labor or contractions that are not strong enough leads to lack of O2. Breech birth can also be planned. Complications of C-section: Monitor client for hemorrhage and shock. Placental previa- placenta attaches over cervical opening. Placentae accrete—placental attaches to uterus too firmly and grows into the tissues. Uterine rupture uterus could have soft spots from previous C-SECTION, and it could rupture. Post Op Care: Only the surgeon removes the initial first dressing. Then after initial we can assess the wound. Chapter 16: Intrapartum Complications: Dystocia: Slow or difficult labor or delivery. D= dystocia, D for difficult labor. Causes & Risk Factors: Macrosomia: big baby >8lbs 13 oz usually secondary to gestational diabetes, can cause uterine distension. Overweight, BMI >25 Older age Previous difficulty with fertility. Failure of uterus and cervix to contract. Insufficient cervix dilation & descent of baby. Interventions: Reposition or ambulate mother. Oxytocin to induce labor. Get ready for amniotomy: provider manually breaks the water. Not to be confused with shoulder dystocia! Shoulder Dystocia: Occurs during vaginal delivery. Fetal head delivers but the top of the shoulder becomes wedged behind or under the mother’s pubis symphysis the baby is stuck in the mom’s birth canal. If it lasts longer than 5 minutes high risk for fetal asphyxia (hypoxia) from prolonged compression on the umbilical cord. Need quick action to save the baby! Nursing Intervention: Document time of event and position. Verbalize passing time to provider 1 min has passed. Maneuver’s to relives shoulder impaction McRoberts maneuver: Flex the client’s legs back against the abdomen. Apply suprapubic pressure press downward on the symphysis pubis. Request additional assistance from staff. Avoid: Administering tocolytic agents (Terbutaline, Mag Sulfate) Fundal Pressure Use of forceps or vacuum Uterine Rupture: Spontaneous tearing of the uterus that may result in the fetus being expelled into the peritoneal cavity. Causes: Previous C-section and attempting VBAC. Forceps delivery Trauma: car accident, fall Overdistension of uterus like twins, etc. Too much oxytocin S/S: Severe, sudden abdominal pain like tearing or ripping. Non reassuring FHR Variable or late decels Fetal distress Mother s/s of bleeding: Hypovolemic shock Hypotension Tachycardia Interventions: Immediate C-section Hysterectomy, not always IV fluids and blood products Uterine Inversion: Placenta fails to detach from the uterine wall and pulls the uterus inside-out. Life threatening! Can happen in vaginal or C-section. Causes: S/S: Pulling on the umbilical cord too soon and too forcefully. Excess fundal massage—to firm Placenta accrete. Too much oxytocin or uterine relaxing agents Labor lasting longer 24 hrs. Short umbilical cord Previous inversion Severe abdominal pain S/S of bleeding in mother hypovolemic shock, hypotension, and tachycardia Interventions: Relax the uterus with tocolytics terbutaline & Mag Sulfate Provider repositions the uterus. After uterus is repositioned/corrected give oxytocin to prevent re-inversion. IV fluids and blood products. Umbilical Cord Prolapse & Compression: Umbilical cord protrudes out of mother’s cervix or vagina, before the baby! Cuts off oxygen-rich blood to the baby. If oxygen cord is compressed, cuts off oxygenations leaving lifelong brain damage or death. Common after SROM (water breaks) or amniotomy. Will see fetal bradycardia as fetal HR is being interrupted by compressed cord. Abrupt fetal HR decelerations think compression. If you see drop in FHR after mom’s membranes rupture think umbilical cord prolapse and assess the vagina. Nursing Interventions: Call for assistance Insert sterile gloved hands 1-2 fingers into mother’s vagina to relieve compression. Reposition mom: knee to chest or Trendelenburg position to help lift baby off of cord. If umbilical cord is protruding from vaginaWrap cord loosely with a sterile towel or gauze soaked with sterile normal saline. Prepare for an emergency C-section. Meconium-Stained Amniotic Fluid: Fetus has defecated/pooped in the amniotic fluid. Amniotic fluid is supposed to be clear but with meconium in it, it turns various shades of green, yellow, or brown and smells foul. Very common in breech, after fetal distress and in term or post term. Can also indicate fetal hypoxia prepare for neonatal resuscitation. Infant could breathe in or aspirate meconium. Meconium Aspiration Syndrome: Baby breathes in/aspirates foul smelling fluid into lungs around time of delivery. Is like coating inside of lungs with tar and gas exchange becomes decreased/impossible making it the leading cause of severe illness and death in newborns. Risk factors: >40 weeks of gestation Diabetes High BP Long or difficult labors Perinatal asphyxia. Prostaglandins are cervical ripening agents. Prostaglandins are contraindicated in patients who have had a previous surgery in the upper uterus, such as a previous classic cesarean incision or extensive surgery for uterine fibroids. A side effect of prostaglandin administration is hyperstimulation of the uterus. Promote thermoregulation of infant: b. Dry the infant off with sterile towels. c. Place stockinette cap on infant’s head. e. Remove wet linen as needed. Dry the infant to prevent heat loss! Induction of labor reasons: Fetal death, post-term pregnancy, rupture of members, and chorioamnionitis are all acceptable indications for induction. Other conditions include intrauterine growth retardation (IUGR), maternal-fetal blood incompatibility, hypertension, and placental abruption. Write down crowning from chap 16 questions.