Electrocardiogram (ECG) Guide: Heart Anatomy & Interpretation
advertisement

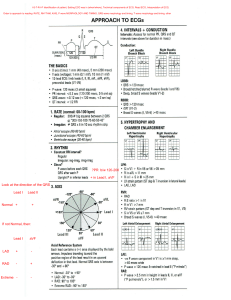
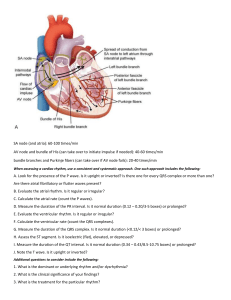
Electrocardiogram (ECG) Outline - Introduction - Anatomy and physiology of heart • layers of heart • cardiac cycle • heart valves • conduction system - properties of Cardiac cells - Definition of ECG - Indications - Types of ECG - Definitions and related ECG terms - Normal and abnormal ECG ECG Introduction Electrocardiography is the process of producing an electrocardiogram (ECG or EKG ), a recording of the heart's electrical activity. It is an electrogram of the heart which is a graph of voltage versus time of the electrical activity of the heart using electrodes placed on the skin. These electrodes detect the small electrical changes that are a consequence of cardiac muscle depolarization followed by repolarization during each cardiac cycle (heartbeat). Changes in the normal ECG pattern occur in numerous cardiac abnormalities, including cardiac rhythm disturbances (such as atrial fibrillation and ventricular tachycardia ), inadequate coronary artery blood flow (such as myocardial ischemia and myocardial infarction ), and electrolyte disturbances (such as hypokalemia and hyperkalemia ). Traditionally, "ECG" usually means a 12-lead ECG taken while lying down as discussed below. However, other devices can record the electrical activity of the heart such as a Holter monitor but also some models of smartwatch are capable of recording an ECG. ECG signals can be recorded in other contexts with other devices. Anatomy and physiology of heart ( 1 ) Layers of the heart 1– Epicedium the outer layer of the wall of the heart. 2– Myocardium the muscular middle layer of the wall of the heart. 3– Endocardium the inner layer of the heart. ( 2 ) Cardiac Cycle Is the sequence of events that occurs when the heart beats. 1- Systole Phase the ventricles contract and pump blood to the arteries. 2- Diastole Phase the heart ventricles are relaxed and the heart fills with blood. ( 3 ) Heart valves Are flap-like structures that allow blood to flow in one direction. 1- Aortic Valve prevents the back flow of blood as it is pumped from the left ventricle to the aorta. 2- Mitral Valve prevents the back flow of blood as it is pumped from the left atrium to the left ventricle. 3- Pulmonary Valve prevents the back flow of blood as it is pumped from the right ventricle to the pulmonary artery. 4- Tricuspid Valve prevents the back flow of blood as it is pumped from the right atrium to the right ventricle. ( 4 ) Conduction System Is the rate at which the heart conducts electrical impulses. The following structures play an important role in causing the heart to contract. 1- Sinoatrial (SA) node. This node is the dominant pacemaker of the heart, located in the upper portion of the right atrium. Intrinsic rate is 60–100 bpm. 2- Internodal pathways. These cells direct electrical impulses between the SA and AV nodes and spread them across the atrial muscle. 3- Atrioventricular (AV) node. This node is part of an area called AV junction tissue, which includes some surrounding tissue plus the connected bundle of His. Although AV junction tissue contains pacemaker cells, none are thought to exist in the AV node itself. The AV node slows conduction, creating a slight delay before electrical impulses are carried to the ventricles. Intrinsic rate is 40–60 bpm. 4- Bundle of His. Located at the top of the interventricular septum, this bundle of fibers extends directly from the AV node and connects the atria and ventricles electrically. 5- Bundle branches. The bundle of His splits into two conduction paths called the right and left bundle branches. These bundles carry electrical impulses at high speed to the tissue of the interventricular septum, and to each ventricle simultaneously. 6- Purkinje system. The bundle branches terminate with this network of fibers, which spread electrical impulses rapidly throughout the ventricular walls. Intrinsic rate is 20–40 bpm. Properties of Cardiac Cells 1- Automaticity Generates electrical impulse independently, without involving the nervous system. 2- Excitability Responds to electrical stimulation. 3- Conductivity Passes or propagates electrical impulses from cell to cell. 4- Contractility Shortens in response to electrical stimulation. Definition of ECG ECG is a series of waves and deflections recording the heart’s electrical activity from a certain view. Is the first diagnostic measure to asses‟ cardiovascular disease. Is a recording of cardiac electrical activity made from the body surface and displayed on graph paper. Indication of ECG 1- Check the heart's electrical activity. 2- Find the cause of unexplained chest pain, which could be caused by a heart attack, inflammation of the sac surrounding the heart (pericarditis), or angina. 3- Find the cause of symptoms of heart disease, such as shortness of breath, dizziness, fainting, or rapid, irregular heartbeats (palpitations). 4- Find out if the walls of the heart chambers are too thick (hypertrophied). 5- Check how well medicines are working and whether they are causing side effects that affect the heart. 6- Check how well mechanical devices that are implanted in the heart, such as pacemakers, are working to control a normal heartbeat. 7- Check the health of the heart when other diseases or conditions are present, such as high blood pressure, high cholesterol, cigarette smoking, diabetes . Types of ECG There are 3 main types of ECG: 1- Resting ECG carried out while you're lying down in a comfortable position Procedure 1- Equipment – Trolley, couch or bed with private area – ECG machine – Electrodes – Safety razor – Recording paper – Disposable pre-gelled electrodes – 4 × 4 gauze pads or washcloth – marking pen 2- Assessment ☆Chart – Verify the order for the ECG – Diagnosis of the patient – Previous ECG – Medication – Lab investigation ☆Patient – Confirm the client's ID – Vital signs – Age – Sex – Level of consciousness – Surgery (CABG) – Patients Extremities – Signs and symptoms as chest pain, tachycardia ☆Machine – Ensure that it is functioning – There is sufficient Paper – The paper speed selector is set to the standard 25 mm/second – Calibrate to 10mm/mV – The machine is set to full voltage ☆Environment – Close door and window – Keep privacy – Provide a bed/couch or trolley – Emphasize that no electrical current will enter the body. – Ensure the environment is warm 3- Implementation Patient 1– Explain the procedure to the client 2– Explain that the test records the heart's electrical activity and that it may be repeated at certain intervals. 3– Prepare skin of chest area by removing hair. 4– Have the client lie supine in the center of the bed with arms at his sides. 5– Expose the arms and legs and cover the client appropriately 6– The arms and legs should be relaxed to minimize muscle trembling 7– Remove any metal, such as keys or a wristwatch 8– Make sure the feet are not touching the bed board. 9– Hand Washing 10– Place the ECG machine close to the client's bed and plug the cord into the wall outlet or, battery-operated 11– Place electrodes on the inner aspect of the wrists and lower legs • Yellow 》 Lt Arm • Green 》 Lt Leg • Red 》 RT arm • Black 》 RT leg ☆ Place chest leads • V1: 4th intercostal space (ICS), RIGHT margin of the sternum. • V2: 4th ICS along the LEFT margin of the sternum. • V3: midway between V2 and V4. • V4: 5th ICS, mid-clavicular line. • V5: 5th ICS, anterior axillary line (same level as V4) • V6: 5th ICS, mid-axillary line (same level as V4) 12– Avoid muscular and bony areas. 13– After all electrodes are in place, connect the lead wires. 14– Press the START button and input any required information. 15– Make sure that all leads are represented in the tracing. If not, determine which electrode has come loose, reattach it, and restart the tracing. 16- – Print ECG 17– Disconnect the electrode (pump) 18– Remove the gel with a moist cloth towel 19– If the patient is having recurrent chest pain or if serial ECG‟s are ordered mark over the chest with marker. 20– Reassurance patient 21– Return equipment 4- Documentation – Name of the patient – Unit – Age – Diagnosis – Date and Time 2Stre ss or exe rcis e ECG carried out while you're using an exercise bike or treadmill. An exercise ECG is performed to assess the heart's response to stress or exercise. The ECG is monitored while a person is exercising on a treadmill or stationary bike. Purpose 1- Determine physical fitness 2- Locate areas of the heart that receive an insufficient blood and oxygen supply 3- Reveal heart rhythm abnormalities 4- Evaluate a person's prognosis after a heart attack 5- Verify the effectiveness of medical and surgical therapies 6- Determine an appropriate exercise program for people with known heart disease. Contraindications 1- Unstable angina 2- Sever pulmonary hypertension 3- Uncontrolled arrhythmia 4- Pulmonary embolism 5- Aortic dissection PRE-TEST GUIDELINES 1- Avoid eating or drinking before test with 2-3 hours 2- avoid strenuous exercise 3- avoid using tobacco products for approximately two hours before the test 4- Avoid alcohol or caffeine for 24 hours before the test. Procedure 1- Attached 10 electrodes to the person's chest and back. 2- The electrodes record the heart's electrical impulses and transmit them to an electrocardiograph 3- A machine that turns the impulses into waves on graph paper or on a monitor screen. 4- Patient will also wear a blood pressure monitoring cuff or monitoring device during the test. The electrodes may be placed on top of a light layer of gel that conducts electricity and helps ensure clear readings. 5- Men should expect to have some chest hair shaved so that the electrodes will press directly against the skin. 6- Recordings of the heart's activity are made before exercise begins 7- These readings can be used to make sure the person is ready for the test and to compare to the stress test with the resting heartbeat. 8- As exercise begins, the patient walks slowly on the treadmill. 9- The speed of the treadmill increase slowly, typically about every 3 minutes. 10- The test ends once the patient reaches the target heart rate (usually 220 b\m the person's age), or if the patient cannot continue because of fatigue, shortness of breath, or chest pain. 11- The physician evaluates the test results and discusses them with the patient after the test. 3- Ambulatory ECG (sometimes called a Holter monitor) the electrodes are connected to a small portable machine worn at your waist so your heart can be monitored at home for 1 or more days. Holter monitoring is used to determine how the heart responds to normal activity. The monitor may also be used to diagnose: – Atrial fibrillation or flutter – Multifocal atrial tachycardia – Palpitations – Paroxysmal supraventricular tachycardia – Reasons for fainting – Slow heart rate (bradycardia) – Ventricular tachycardia While wearing the device avoid: – Electric blankets – High-voltage areas – Magnets The type of ECG you have will depend on your symptoms and the heart problem suspected. For example, an exercise ECG may be recommended if your symptoms are triggered by physical activity, whereas an ambulatory ECG may be more suitable if your symptoms are unpredictable and occur in random, short episodes. Definitions and related ECG terms 1- ablation removal of material, by mechanical means, from the surface of an object; in the context of cardiology, it is the purposeful destruction of heart muscle cells, usually in an attempt to correct or eliminate a dysrhythmia 2- artifact distorted, irrelevant, and extraneous electrocardiographic (ECG) waveforms 3- automaticity ability of the cardiac cells to initiate an electrical impulse 4- cardiac resynchronization therapy (CRT) biventricular pacing used to correct interventricular, intraventricular, and atrioventricular conduction disturbances that occur in patients with heart failure 5- cardioversion electrical current given in synchrony with the patient’s own QRS complex to stop a dysrhythmia 6- chronotropy rate of impulse formation 7- conduction transmission of electrical impulses from one cell to another 8- defibrillation electrical current given to stop a dysrhythmia, not synchronized with the patient’s QRS complex 9- depolarization process by which cardiac muscle cells change from a more negatively charged to a more positively charged intracellular state 10- dromotropy conduction velocity 11- dysrhythmia disorder of the formation or conduction (or both) of the electrical impulse within the heart, altering the heart rate, heart rhythm, or both and potentially causing altered blood flow (also referred to as arrhythmia) 12- elective replacement indicator (ERI) a signal produced by a pacemaker when it is interrogated to indicate a neardepleted battery 13- electrocardiogram (ECG) a record of a test that graphically measures the electrical activity of the heart, including each phase of the cardiac cycle 14- implantable cardioverter defibrillator (ICD) a device implanted into the chest wall to treat dysrhythmias 15- inotropy force of myocardial contraction 16- P wave the part of an ECG that reflects conduction of an electrical impulse through the atrium; atrial depolarization 17- paroxysmal a dysrhythmia that has a sudden onset and terminates spontaneously; usually of short duration, but may recur. 18- PP interval the duration between the beginning of one P wave and the beginning of the next P wave; used to calculate atrial rate and rhythm 19- PR interval the part of an ECG that reflects conduction of an electrical impulse from the sinoatrial node through the atrioventricular node 20- QRS complex the part of an ECG that reflects conduction of an electrical impulse through the ventricles; ventricular depolarization 21- QT interval the part of an ECG that reflects the time from ventricular depolarization through repolarization 22- repolarization process by which cardiac muscle cells return to a more negatively charged intracellular condition, their resting state 23- RR interval the duration between the beginning of one QRS complex and the beginning of the next QRS complex; used to calculate ventricular rate and rhythm 24- sinus rhythm electrical activity of the heart initiated by the sinoatrial node 25- ST segment the part of an ECG that reflects the end of the QRS complex to the beginning of the T wave 26- T wave the part of an ECG that reflects repolarization of the ventricles 27- TP interval the part of an ECG that reflects the time between the end of the T wave and the beginning of the next P wave; used to identify the isoelectric line 28- U wave the part of an ECG that may reflect Purkinje fiber repolarization; usually, it is not seen unless a patient’s serum potassium level is low. Normal ECG Components of the Electrocardiogram The ECG waveform reflects the function of the heart’s conduction system in relation to the specific lead. The ECG offers important information about the electrical activity of the heart and is useful in diagnosing dysrhythmias. ECG waveforms are printed on graph paper that is divided by vertical and horizontal lines at standard intervals. Time and rate are measured on the horizontal axis of the graph, and amplitude or voltage is measured on the vertical axis. When an ECG waveform moves toward the top of the paper, it is called a positive deflection. When it moves toward the bottom of the paper, it is called a negative deflection. When reviewing an ECG, each waveform should be examined and compar ed with the others. ( Waves, Comple xes, and Intervals ) The ECG is composed of waveforms (including the P wave, the QRS complex, the T wave, and possibly a U wave) and of segments and intervals (including the PR interval, the ST segment, and the QT interval). 1- The P wave represents the electrical impulse starting in the SA node and spreading through the atria. Therefore, the P wave represents atrial depolarization. It is normally 2.5 mm or less in height and 0.11 seconds or less in duration. 2- The QRS complex represents ventricular depolarization. Not all QRS complexes have all three waveforms. The Q wave is the first negative deflection after the P wave. The Q wave is normally less than 0.04 seconds in duration and less than 25% of the Rwave amplitude. The R wave is the first positive deflection after the P wave, and the S wave is the first negative deflection after the R wave. When a wave is less than 5 mm in height, small letters (q, r, s) are used; when a wave is taller than 5 mm, capital letters (Q, R, S) are used to label the waves. The QRS complex is normally less than 0.12 seconds in duration. 3- The T wave represents ventricular repolarization (when the cells regain a negative charge; also called the resting state). It follows the QRS complex and is usually the same direction (deflection) as the QRS complex. Atrial repolarization also occurs but is not visible on the ECG because it occurs at the same time as ventricular depolarization (i.e., the QRS). 4- The U wave is thought to rep res ent rep ola riza tio n of the Purkinje fibers; although this wave is rare, it sometimes appears in patients with hypokalemia (low potassium levels), hypertension, or heart disease. If present, the U wave follows the T wave and is usually smaller than the P wave. If larger in amplitude, it may be mistaken for an extra P wave. 5- The PR interval is measured from the beginning of the P wave to the beginning of the QRS complex and represents the time needed for sinus node stimulation, atrial depolarization, and conduction through the AV node before ventricular depolarization. In adults, the PR interval normally ranges from 0.12 to 0.20 seconds in duration. 6- The ST segment which represents early ventricular repolarization, lasts from the end of the QRS complex to the beginning of the T wave. The beginning of the ST segment is usually identified by a change in the thickness or angle of the terminal portion of the QRS complex. The end of the ST segment may be more difficult to identify because it merges into the T wave. The ST segment is normally isoelectric (see later discussion of TP interval). It is analyzed to identify whether it is above or below the isoelectric line, which may be, among other signs and symptoms, a sign of cardiac ischemia. 7- The PP interval is measu red from the beginni ng of one P wave to the beginning of the next P wave. The PP interval is used to determine atrial rate and rhythm. 8- The RR interval is measured from one QRS complex to the next QRS complex. The RR interval is used to determine ventricular rate and rhythm. ECG Interpretations 1st step 》Confirm details Before beginning ECG interpretation, you should check the following details: • Confirm the name and date of birth of the patient matches the details on the ECG. • Check the date and time that the ECG was performed. • Check the calibration of the ECG (usually 25mm/s and 10mm/1mV). 1- Heart rhythm A patient’s heart rhythm can be regular or irregular. Irregular rhythms can be either: • Regularly irregular (i.e. a recurrent pattern of irregularity) • Irregularly irregular (i.e. completely disorganised) Mark out several consecutive R-R intervals on a piece of paper, then move them along the rhythm strip to check if the subsequent intervals are similar. - If you are suspicious that there is some atrioventricular block (AV block), map out the atrial rate and the ventricular rhythm separately (i.e. mark the P waves and R waves). As you move along the rhythm strip, you can then see if the PR interval changes, if QRS complexes are missing or if there is complete dissociation between the two. 2- Heart rate normal adult heart rate • Normal: 60-100 bpm • Tachycardia: > 100 bpm • Bradycardia: < 60 bpm A- Regular heart rhythm If a patient has a regular heart rhythm their heart rate can be calculated using the following method: - Count the number of large squares present within one R-R interval. - Divide 300 by this number to calculate heart rate. Heart rate calculation example • 4 large squares in an R-R interval 300/4 = 75 beats per minute B- Irregular heart rhythm If a patient’s heart rhythm is irregular the first method of heart rate calculation doesn’t work (as the R-R interval differs significantly throughout the ECG). As a result, you need to apply a different method: - Count the number of complexes on the rhythm strip (each rhythm strip is typically 10 seconds long). - Multiply the number of complexes by 6 (giving you the average number of complexes in 1 minute). Heart rate calculation example 10 complexes on a rhythm strip 10 x 6 = 60 beats per minute 3- Cardiac axis Cardiac axis describes the overall direction of electrical spread within the heart. In a healthy individual, the axis should spread from 11 o’clock to 5 o’clock. To determine the cardiac axis you need to look at leads I, II and III. Normal cardiac axis Typical ECG findings for normal cardiac axis: Lead II has the most positive deflection compared to leads I and III. Right axis devia tion Typic al ECG findin gs for right axis deviation: Lead III has the most positive deflection and lead I should be negative. Right axis deviation is associated with right ventricular hypertrophy. Left axis deviation Typical ECG findings for left axis deviation: Lead I has the most positive deflection. Lead s II and III are nega tive. Left axis devi atio n is asso ciated with heart conduction abnormalities. 4- P waves The next step is to look at the P waves and answer the following questions: 1. Are P waves present? 2. If so, is each P wave followed by a QRS complex? 3. Do the P waves look normal? check duration, direction and shape 4. If P waves are absent, is there any atrial activity? • Sawtooth baseline → flutter waves • Chaotic baseline → fibrillation waves • Flat line → no atrial activity at all NB 》 If P waves are absent and there is an irregular rhythm it may suggest a diagnosis of atrial fibrillation. 5- PR interval The PR interval should be between 120-200 ms (3-5 small squares). Prolonged PR interval (>0.2 seconds) A prolonged PR interval suggests the presence of atrioventricular delay (AV block). A- First-degree heart block (AV block) First-degree heart block involves a fixed prolonged PR interval (>200 ms). B- Second-degree heart block (type 1) Second-degree AV block (type 1) is also known as Mobitz type 1 AV block or Wenckebach phenomenon. Typical ECG findings in Mobitz type 1 AV block include progressive prolongation of the PR interval until eventually the atrial impulse is not conducted and the QRS complex is dropped. AV nodal conduction resumes with the next beat and the sequence of progressive PR interval prolongation and the eventual dropping of a QRS complex repeats itself. C- Second-degree heart block (type 2) Second-degree AV block (type 2) is also known as Mobitz type 2 AV block. Typical ECG findings in Mobitz type 2 AV block include a consistent PR interval duration with intermittently dropped QRS complexes due to a failure of conduction. The intermittent dropping of the QRS complexes typically follows a repeating cycle of every 3rd (3:1 block) or 4th (4:1 block) P wave. D- Third-degree heart block (complete heart block) Third-degree (complete) AV block occurs when there is no electrical communication between the atria and ventricles due to a complete failure of conduction. Typical ECG findings include the presence of P waves and QRS complexes that have no association with each other, due to the atria and ventricles functioning independently. Cardiac function is maintained by a junctional or ventricular pacemaker. Narrow-complex escape rhythms (QRS complexes of <0.12 seconds duration) originate above the bifurcation of the bundle of His. Broad-complex escape rhythms (QRS complexes >0.12 seconds duration) originate from below the bifurcation of the bundle of His. Tips for remembering types of heart block To help remember the various types of AV block, it is useful to know the anatomical location of the block within the conducting system. First-degree AV block: Occurs between the SA node and the AV node (i.e. within the atrium). Second-degree AV block: Mobitz I AV block (Wenckebach) occurs IN the AV node (this is the only piece of conductive tissue in the heart which exhibits the ability to conduct at different speeds). Mobitz II AV block occurs AFTER the AV node in the bundle of His or Purkinje fibres. Third-degree AV block: Occurs at or after the AV node resulting in a complete blockade of distal conduction. 6- QRS complex When assessing a QRS complex, you need to pay attention to the following characteristics: Width Height Morphology Width Width can be described as NARROW (< 0.12 seconds) or BROAD (> 0.12 seconds): • A narrow QRS complex occurs when the impulse is conducted down the bundle of His and the Purkinje fibre to the ventricles. This results in well organised synchronised ventricular depolarisation. • A broad QRS complex occurs if there is an abnormal depolarisation sequence – for example, a ventricular ectopic where the impulse spreads slowly across the myocardium from the focus in the ventricle. In contrast, an atrial ectopic would result in a narrow QRS complex because it would conduct down the normal conduction system of the heart. Similarly, a bundle branch block results in a broad QRS complex because the impulse gets to one ventricle rapidly down the intrinsic conduction system then has to spread slowly across the myocardium to the other ventricle. Height Height can be described as either SMALL or TALL: Small complexes are defined as < 5mm in the limb leads or < 10 mm in the chest leads. Tall complexes imply ventricular hypertrophy (although can be due to body habitus e.g. tall slim people). There are numerous algorithms for measuring LVH, such as the Sokolow-Lyon index or the Cornell index. Morphology To assess morphology, you need to assess the individual waves of the QRS complex. Delta wave The mythical ‘delta wave‘ is a sign that the ventricles are being activated earlier than normal from a point distant to the AV node. The early activation then spreads slowly across the myocardium causing the slurred upstroke of the QRS complex. Note – the presence of a delta wave does NOT diagnose Wolff-Parkinson-White syndrome. This requires evidence of tachyarrhythmias AND a delta wave. 7- Q-waves Isolated Q waves can be normal. A pathological Q wave is > 25% the size of the R wave that follows it or > 2mm in height and > 40ms in width. A single Q wave is not a cause for concern – look for Q waves in an entire territory (e.g. anterior/inferior) for evidence of previous myocardial infarction. 8- ST segment The ST segment is the part of the ECG between the end of the S wave and the start of the T wave. In a healthy individual, it should be an isoelectric line (neither elevated nor depressed). Ab nor ma liti es of the ST seg me nt should be investigated to rule out pathology. A- ST-elevation ST-elevation is significant when it is greater than 1 mm (1 small square) in 2 or more contiguous limb leads or >2mm in 2 or more chest leads. It is most commonly caused by acute full-thickness myocardial infarction. B- ST depression ST depression ≥ 0.5 mm in ≥ 2 contiguous leads indicates myocardial ischaemia. 9- T waves T waves represent repolarisation of the ventricles. A- Tall T waves T waves are considered tall if they are: > 5mm in the limb leads AND > 10mm in the chest leads (the same criteria as ‘small’ QRS complexes) Tall T waves can be associated with: Hyperkalaemia (“tall tented T waves”) Hyperacute STEMI B- Inverted T waves T waves are normally inverted in V1 and inversion in lead III is a normal variant. Inverted T waves in other leads are a nonspecific sign of a wide variety of conditions: - Ischaemia - Bundle branch blocks (V4-6 in LBBB and V1-V3 in RBBB) - Pulmonary embolism - Left ventricular hypertrophy (in the lateral leads) - Hypertrophic cardiomyopathy (widespread) - General illness C- Biphasic T waves Biphasic T waves have two peaks and can be indicative of ischaemia and hypokalaemia. 10- U waves U waves are not a common finding. The U wave is a > 0.5mm deflection after the T wave best seen in V2 or V3. These become larger the slower the bradycardia – classically U waves are seen in various electrolyte imbalances, hypothermia and secondary to antiarrhythmic therapy (such as digoxin, procainamide or amiodarone). Abnormal ECG ( Cardiac dysrhythmias ) Definition Dysrhythmias (or arrhythmia) are a problem that affects the electrical system of the heart muscle, producing abnormal heart rhythm. It can cause the heart to pump less effectively. Types of abnormal ECG 1- SA node dysfunctions - Sinus Bradycardia - Sinus Tachycardia - Sinus Dysrrhythmia 2- Atrium dysfunctions ( P wave ) - (PAC) Premature atrial contraction - Atrial tachycardia ( SVT ) - Atrial fibrillation - Atrial flutter 3- AV dysfunctions ( P-R interval ) - 1st degree AV block - 2nd degree AV block (type 1) - 2nd degree AV block ( Type 2 ) - 3rd degree AV block 4- Junctional dysfunctions ( Around AV node ) - (PJC) premature Junctional contraction - Junctional escape rhythm - Accelerate Junctional - Junctional Tachycardia 5- Ventricle dysfunctions ( QRS complex ) - (PVC) Premature ventricle contraction - (IVR) Idioventricular rhythm - ( VT ) Ventricle Tachycardia - (VF) or (Vfib) Ventricle fibrillation 6- Coronary artery dysfunction ( S-T segment ) - Angina - Inferior MI ( Myocardial infarction ) - Anterior MI - Septal MI - Lateral MI - Posterior MI SA nod e dysf unct ions 1- Sinus Bradycardia Sinus Bradycardia occurs when the sinus node creates an impulse at a slowerthan-normal rate. May normal in sport people or at rest or sleep. Causes of bradycardia •vagal stimulation •medications (digoxin and beta blocker & calcium channel blockers) •Lower metabolic needs (e.g., sleep, hypothermia, hypothyroidism). •Myocardial infarction (MI) The ECG criteria for sinus bradycardia ▪Ventricular and atrial rate: Less than 60 in the adult. ▪Ventricular (R-R) : Regular ▪QRS shape and duration: Usually normal. ▪P wave: Normal and consistent shape; always in front of the QRS ▪PR interval: Consistent interval between 0.12 and 0.20 seconds ▪P: QRS ratio: 1:1 Treatment 1- Atropine, 0.5 to 1.0 mg given rapidly as an intravenous (IV) bolus, is the medication of choice in treating sinus Bradycardia, allowing a normal rate to occur. 2- Emergency transcutaneous pacing may be implemented. 2-Sinus Tachycardia • Occurs when the sinus node creates an impulse at a faster-than-normal rate. • Tachycardia lead to decrease ventricular filling and SV causes hypoxia and work load of the heart. Causes of tachycardia • Anemia, Acute blood loss (hemorrhage) , shock hypovolemia early stage • pain, anxiety & emotion • hyper metabolic states, fever & exercise • drugs in critical care cause tachycardia as (dopamine, atropine, aminophillin, dopamine, hydralazine &catecholamine • Thyrotoxicosis • illegal drug as cocaine The ECG criteria for sinus tachycardia ▪ Ventricular and atrial rate: Greater than 100 and less than (150 b\min) dangerous if more than 180 beat\min in the adult ▪ Ventricular and atrial rhythm: Regular ▪ QRS shape and duration: Usually normal. ▪ P wave: Normal and consistent shape; always in front of the QRS, but may be buried in the preceding T wave ▪ PR interval: Consistent interval between 0.12 and 0.20 seconds ▪ P: QRS ratio: 1:1 Treatment Usually directed at treating its cause. Calcium channel blockers and beta blockers may be used to reduce the heart rate quickly. 3- Sinus Arrhythmia • abnormal rhythm (irregular) called tachy-brady dysrhythmias • Sinus arrhythmia occurs when the sinus node creates an impulse at an irregular rhythm. • It is often occurs in children and young adults and the incidence decreases with age. • Sinus arrhythmia does not cause any significant hemodynamic and usually is not treated. The ECG criteria for sinus arrhythmia ▪Ventricular and atrial rate: 60 to 100 in the adult ▪Ventricular and atrial rhythm: Irregular ▪ QRS shape and duration: Usually normal. ▪ P wave: Normal and consistent shape; always in front of the QRS ▪ PR interval: Consistent interval between 0.12 and 0.20 seconds ▪ P: QRS ratio: 1:1 Atrium dysfunctions ( P-Wave ) 1- Premature Atrial Complex • Ectopic focus in the area around SA node conductivity and automaticity to produce Ectopic impulses. • PACs are common in normal hearts. • Occurs before next SA node produce new impulse. Causes • Caffeine, alcohol & nicotine • Stretched atrial myocardium (as in Hypervolemia) • Anxiety • Hypokalemia (low potassium level) • Hyper-metabolic states • Atrial ischemia, injury, or infarction • Mitral valve prolapsed and heart failure. The ECG criteria for PACs • Ventricular and atrial rate: Depends on the underlying rhythm(eg, sinus tachycardia) • Ventricular and atrial rhythm: Irregular due to early P waves, creating a PP interval that is shorter than the others. This is sometimes followed by a longer than normal PP interval. • QRS shape and duration: The QRS that follows the early P wave is usually normal, but it may be abnormal. • P wave: An early and different P wave may be seen; other P waves in the strip are consistent. • PR interval: may be longer, shorter or the same as PR interval of a sinus impulse. • P: QRS ratio: usually 1:1 Treatment 1- If PACs are infrequent, no treatment is necessary. 2- If frequent, treatment is directed toward the cause. 2Subraventricular tachycardia(PSVT) tachycardia(SVT) paroxysmal subraventricular •SVT specified with narrow QRS complex less than 0.12 sec. •SVT person characterize of syncope (lose consciousness) •Sudden interruption of sinus rhythm and the atrial Ectopic focus to produce firing (150-250 b\m). •Characterize by tachycardia and abnormal P wave shape. •Rapid rates cause decrease ventricular filling time, increase myocardial demand and increase oxygen supply. •Present in many case as HF, angina, MI. The ECG criteria for SVT ▪ Ventricular and atrial rate: more than 180 beat\min in the adult ▪ Ventricular and atrial rhythm: Regular ▪ QRS shape and duration: Usually normal shape but veru narrow ▪ P wave: Normal and consistent shape; always in front of the ▪ PR interval: Consistent interval between 0.12 and 0.20 seconds ▪ P: QRS ratio: 1:1 Management 1- Vegal maneuver • Valsava maneuver : ask patient to bear down as going to bathroom • carotid massage :only in one side in the neck 2- Pharmacological •Block conduction system activity as adenosine (adenecore) 6mg IV rapid push followed by normal saline (my increase dose to 12 mg ) but may contraindicated in patients with asthma. •Amiodarone (corderone) antidysarrhythmia •Diltazm •IV calcium channel blocker. 3- Electrical cardioversion 3- Atrial Flutter •occurs in the atrium and creates impulses at an atrial rate between 250 and 350 times per minute •Because the atrial rate is faster than the AV node can conduct, not all atrial impulses are conducted into the ventricle. •If all atrial impulses were conducted to the ventricle, the ventricular rate would also be 250 to 350, which would result in ventricular fibrillation. Signs and symptoms • Chest pain • shortness of breath & low blood pressure The ECG criteria for atrial flutter •Ventricular and atrial rate: Atrial rate ranges between 250 and 350 ventricular rate usually ranges between 75 and 150. •Ventricular and atrial rhythm: The atrial rhythm is regular; the ventricular rhythm is usually regular. • QRS shape and duration: Usually normal but may be abnormal or may be absent •P wave: Saw-toothed shape. •PR interval: it is difficult to determine the PR interval. •P: QRS ratio: 2:1, 3:1, or 4:1 Management 1- Anti Dysrrhythmia medications • To slow conduction system as (ca channel blocker , beta blocker) •To convert and return to normal pattern as amiodarone. 2- Electrical cardioversion 4- Atrial Fibrillation •Atrial fibrillation causes a rapid, disorganized, and uncoordinated twitching of atrial musculature. •( no P wave and rapid fibrilator Appear) atrial fibrillation appear in lead (І, П, AVF) •It is the most common Dysrrhythmia that causes patients to seek medical attention. •produce by Ectopic impulses by the atrial no by SA node (atrial kick) • atrial fibrillation lead or absent of P wave. Risk factors •Hypertension, Heart failure •Obesity, Myocardial infarction Signs and symptoms •Hypotension •Irregular palpitations • fatigue and malaise • There is usually a pulse deficit. The ECG criteria for atrial fibrillation •Ventricular and atrial rate: Atrial rate is more than 350. •Ventricular rate: is usually 120 to 180 in untreated atrial fibrillation •Ventricular and atrial rhythm: Highly irregular •QRS shape and duration: Usually normal. •P wave: No discernible P waves •PR interval: Cannot be measured (absent) •P: QRS ratio: many:1 Treatment 1. Rhythm control by cardioversion or chemical by amidrone, quiudin 2. Rate control to slow conduction system by : • Calcium channel blocker. 3. Anticoagulant : to prevent embolic formation as warfarin (INR should be maintained 2.5). 3.Atrial pacing or surgery is sometimes indicated for patients who are unresponsive to medications. Atrio-ventricular conduction disturbance (AV block) P-R interval 1- First degree of AV block •Occurs when all atrial impulses are conducted to ventricles but the PR interval more than 0.12 sec. •Increase of PR interval caused by delay within the atrial conduction pathway. Cau ses fibr oses or scleroses of conduction system, leak of blood supply to conduction system, valvular heart disease, myo- cardities, cardiac surgery, hyperkalemia, drug toxicity as digoxin. The ECG criteria for first degree AV block •Ventricular and atrial rate: Atrial rate is mainly regular and sometimes Bradycardia •Ventricular and atrial rhythm: regular •QRS shape and duration: become wide •P wave: normal P wave •PR interval: prolong in constant manner in all ECG heart beats •P: QRS ratio: 1:1 2- Second degree of AV block It is classified to 1- Mobitz type 1 (wenkbach block) The ECG criteria for Mobitz type 1 (wenkbach block) • Ventricular and Ventricular and atrial rate: Bradycardia • atrial rhythm: irregular • QRS shape and duration: become wide • P wave: normal P wave • PR interval: prolong and irregular manner in all ECG heart beats • P: QRS ratio: (5:4—4:3—3:2). 2- Mobitz type 2 The ECG criteria for Mobtiz type 2 • Ventricular and atrial rhythm Ventricular and atrial rate: Bradycardia • Atrial rhysthm: irregular • QRS shape and duration: become wide and R, R prime (M shape) • P wave: normal P wave • PR interval: cannot be measure • P: QRS ratio: (2:1) 3- Third degree of AV block (Complete AV block) The ECG criteria for Third degree of AV block (Complete AV block) • Ventricular and atrial rate: Bradycardia • Ventricular and atrial rhythm: irregular • QRS shape and duration: become wide and unidentifed shape • P wave: normal P wave • PR interval: cannont be measure • P: QRS ratio: no P wave related to QRS complex (SA node implses completely separated and AV node complete block . Management of patient with AV block 1- in first degree close observation about progression of abnormal conduction 2- second degree mobitz 1 : temporary pacemaker 3- second degree mobitz 2 : temporary pacemaker and may elective pacemaker 4- third degree : TCP : trancutanous pacemaker ● all AV block must prevent patient from orthostatic hypotension and syncope. Junctional dysfunctions around AV node - Junctional Dysrrhythmia appear in lead II - The ECG record characteristic of Junctional 1.retrograde(backward) : conduction system characterize by P wave in lead П • innervated • absent and merged complex 2.Antgrade (forward) conduction : normal QRS complex 3.all Junctional Dysrrhythmia produced Bradycardia. 1- Premature Junctional contraction(PJC) The ECG criteria for Premature Junctional contraction(PJC) • Rate: BradyCardia • Rhythm is regular • P wave : innervated In lead II • QRS complex : normal • PR interval is less than 0.12, If the p wave appears before QRS. 2- Junctional escape rhythm (Junctional rhythm) The ECG criteria for Junctional escape rhythm (Junctional rhythm) • Rate 40- 60 Bradycardia • Rhythm is regular • P wave: Can be entirely absent and entry in QRS • QRS wave: is 0.06-0.10 • PR interval is less than 0.12, If the p wave appears before QRS ❖Because the junction 40 -60 b\m and SA node 60-100 b\m the junction can not escape the impulses ( can not overridden the SA node Treated (prophylactic) : by A pacemaker is inserted as a protective, because of concern that the AV junction may also fail. Ventricular arrhythmia (QRS complex) 1- Premature Ventricular Complex • Premature ventricular complex (PVC) is an impulse that starts in a ventricle and is conducted through the ventricles before the next normal sinus impulse. Causes • Cardiac ischemia. • Metabolic abnormalities (hypokalemia, hypoxemia, acidosis). • Heart diseases. • Use of caffeine, nicotine, or alcohol. • Emotional stress The ECG criteria for PVCs •Ventricular and atrial rhythm: Irregular due to early QRS, creating •one RR interval that is shorter than the others. PP interval may be regular. •QRS shape and duration: Duration is 0.12 seconds or longer; shape is bizarre and abnormal. •P wave: Visibility of P wave depends on the timing of the PVC; may be absent (hidden in the QRS or T wave) or in front of the QRS. If the P wave follows the QRS, the shape of the P wave may be different. •PR interval: If the P wave is in front of the QRS, the PR interval is less than 0.12 seconds. •P: QRS ratio: 0:1; 1:1 Treatment •Treat the underlying causes •Without previous history PVCs are not serious but In the patient with an acute MI, PVCs may indicate the need for more aggressive therapy as antiarrhythmic drugs ( beta blockers or amiodarone) 2- Ventricular Tachycardia Definition Ventricular tachycardia (VT) is defined as three or more PVCs in a row, occurring at a rate exceeding 100 beats per minute Causes •Myocardial ischemia. •Congenital heart diseases. •Valvular dysfunction. •Cardiomyopathy. •Drug toxicity. • Electrolyte disturbance. Note -Ventricular tachycardia is a serious Dysrrhythmia and must treated correctly It leads to: - Decrease cardiac out put - Hypotension - Loss of consciousness The ECG criteria for ventricular tachycardia •Rate: more than100 beats per minute. •Rhythm: Usually irregular •QRS shape and duration: Duration is more than 0.12 seconds, bizarre, abnormal shape. •P wave: Very difficult to detect ( absent or retrograde). •PR interval: None. •P: QRS ratio: Difficult to determine, but if P waves are apparent, there are usually more QRS complexes than P waves. Treatment •If the patient is stable continuing the assessment, 12-lead ECG and antiarrhythmic drugs (amiodarone and beta blocker and Lidiocaine •If the patient is unstable immediate defibrillation. 3- Ventricular Fibrillation •rapid but disorganized ventricular rhythm that causes ineffective quivering of the ventricles •the different between poly morphic VT and VF , the QRS complex in poly morphic VT high voltage more than 0.2 mv and VF QRS complex voltage not more than 0.15 MV It is always characterized by the absence of: • An audible apical heartbeat, • A palpable pulse, • Respirations Decrease CO lead to • Syncope. • Un-recordable blood pressure • Hypoxia The ECG criteria for Ventricular fibrillation • Ventricular rate: None • Ventricular rhythm: Extremely irregular, without specific pattern. • P wave and PR interval: None • QRS shape and duration: Irregular, fibrillatory waves. Treatment • Treatment of choice is immediate defibrillation and activation of emergency services, and initiating cardiopulmonary resuscitation (called VF\VT algorithm) • Antiarrhythmic medications as amidarone to convert the rhythm to normal sinus rhythm . Abnormality of ST segment Coronary arteries There are two coronary arteries: The left and right coronary arteries and their branches. The main function of them is to supply arterial blood to the heart muscle. These arteries originate from the aorta. The left coronary artery has three branches: ➢The left main coronary artery. The left anterior descending artery, (which supply the anterior wall of the heart) ➢The circumflex artery, (which circles around to the lateral left wall of the heart). • The right side of the heart is supplied by the right coronary artery, which progresses around to the bottom or inferior wall of the heart. • The posterior wall of the heart receives its blood supply from: ❑Right coronary artery ❑ An additional branch from the right coronary artery called the posterior descending. Abnormality of ST segment Any change from the base line indicate myocardial ischemia if the ST segment elevate less than 1 mm or depressed down ● If ST segment elevated more than 1 mm indicate myocardial infarction. Myocardial infarction The expected ECG changes are T-wave inversion, ST-segment elevation, and development of an abnormal Q wave. Because infarction evolves over time, the ECG also changes over time. The first ECG signs of an acute MI are usually seen in the T wave and ST segment. 1- ST segment elevation 2- ST segment depression Other arrhythmia Asystole Isoelectric line in all ECG because there is no any atrial or ventricle depolarization. Medical Management Ventricular asystole is treated the same as PEA, focusing on high-quality CPR with minimal interruptions and identifying underlying and contributing factors. The key to successful treatment is a rapid assessment to identify a possible cause, which is known as the Hs and Ts: hypoxia, hypovolemia, hydrogen ion (acid–base imbalance), hypo- or hyperglycemia, hypo- or hyperkalemia, hyperthermia, trauma, toxins, tamponade (cardiac), tension pneumothorax, or thrombus (coronary or pulmonary). After the initiation of CPR, intubation and establishment of IV access are the next recommended actions, with no or minimal interruptions in chest compressions. Practical ECG Example 1- Sinus 2- Irregular 3- HR = 6 × 10 = 60 4- p wave : present and normal 5- PR interval : normal 6- QRS Complex : narrow 7- ST Segment : elevation in lead | , ||| , avf 8- T wave : normal 9- Diagnosis : inferior STEMI