Hypothyroidism Case Study: Symptoms, Etiology, Pathophysiology
advertisement

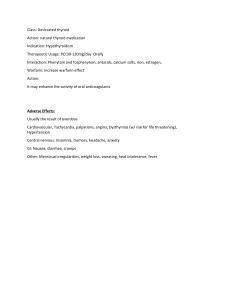
Hypothyroidism Clinical Case with the answer being hypothyroidism A 78-year-old woman is brought to the physician by her son because of progressive memory loss for the past year. She feels tired and can no longer concentrate on her morning crossword puzzles. She has gained 11.3 kg (25 lb) in the last year. Her father died from complications of Alzheimer disease. She has a history of drinking alcohol excessively but has not consumed alcohol for the past 10 years. Vital signs are within normal limits. She is oriented but has short-term memory de cits. Examination shows a normal gait and delayed relaxation of the achilles re ex bilaterally. Her skin is dry, and she has brittle nails. Which of the following is the most likely underlying etiology of this woman’s memory loss? 1. Thiamine de ciency 2. Autoimmune thyroid disease 3. Normal pressure hydrocephalus 4. Vitamin B12 de ciency 5. Alzheimer disease Function of the Thyroid Gland The thyroid gland is an integral part of the endocrine system and serves as the body's primary site for thyroid hormone synthesis and storage. It is controlled by the hypothalamic-pituitary-thyroid (HPT) axis, a complex feedback loop that maintains hormone levels within a narrow range. When the hypothalamus senses low thyroid hormone levels in the bloodstream, it releases thyrotropin-releasing hormone (TRH). This hormone signals the pituitary gland, situated at the base of the brain, to produce thyroid-stimulating hormone (TSH). In response to TSH, the thyroid gland synthesizes and releases T3 and T4 into the bloodstream. Thyroid hormones overview (T3 and T4) Triiodothyronine (T3) and thyroxine (T4) are the primary thyroid hormones responsible for regulating various physiological functions in the body. While T4 is the more abundant hormone, T3 is considered the more active and potent form. After synthesis and secretion by the thyroid gland, the majority of T4 is converted into T3 in peripheral tissues, such as the liver and kidneys. T3 and T4 play a crucial role in maintaining the body's metabolic rate, heat production, heart rate, and protein synthesis. They also in uence brain development, bone health, and various other organ systems. Dysfunction in the synthesis, secretion, or utilization of these hormones results in the clinical manifestations of hypothyroidism. Epidemiology I. Prevalence of Hypothyroidism Hypothyroidism is a prevalent endocrine disorder worldwide, with varying rates across di erent populations and geographical regions. Its incidence has been steadily rising over the past few decades, making it a signi cant public health concern. Studies estimate that approximately 1-2% of the global population is a ected by hypothyroidism. However, the prevalence may be higher in certain regions, particularly those with iodine de ciency or a higher incidence of autoimmune disorders. II. Age and Gender Distribution Hypothyroidism can a ect individuals of all age groups, from neonates to the elderly, but its prevalence varies signi cantly with age. Congenital hypothyroidism, present at birth, is one of the most common preventable causes of intellectual disabilities, a ecting about 1 in 2000 to 1 in 4000 newborns. In contrast, acquired hypothyroidism becomes more common with advancing age, especially in individuals over 60 years old. ff fl fi ff fi fl ff fi ff fi fi fi Gender also plays a crucial role in hypothyroidism, as it is more common in females than males. The female-to-male ratio for hypothyroidism is 3:1. The reasons for this gender disparity are not entirely clear but may involve hormonal and immunological factors. Etiology I. Primary Hypothyroidism A. Autoimmune Thyroiditis (Hashimoto's Thyroiditis) Hashimoto's thyroiditis is the leading cause of primary hypothyroidism in iodine-su cient regions. It is an autoimmune disorder in which the body's immune system mistakenly targets and attacks the thyroid gland. Over time, this immune assault leads to chronic in ammation, progressive destruction of thyroid tissue, and impaired thyroid hormone production. As the disease advances, the thyroid gland may become enlarged, resulting in a condition known as a goiter. B. Iodine De ciency Iodine is a crucial component in the synthesis of thyroid hormones. In areas where dietary iodine intake is insu cient, the thyroid gland cannot produce an adequate amount of thyroid hormones. This de ciency triggers the release of excess TSH from the pituitary gland, causing the thyroid gland to enlarge in an attempt to compensate for the lack of iodine. However, this enlarged thyroid, known as a colloid goiter, still fails to produce su cient thyroid hormones, leading to primary hypothyroidism. II. Secondary Hypothyroidism A. Pituitary Disorders Tumors, infections, or other structural abnormalities a ecting the pituitary gland can disrupt the secretion of TSH. Pituitary tumors, especially non-functioning adenomas, can lead to diminished TSH production, causing secondary hypothyroidism. Additionally, pituitary surgeries or radiation therapy aimed at treating pituitary tumors may inadvertently damage the normal pituitary function, including TSH secretion. B. Hypothalamic Disorders The hypothalamus plays a pivotal role in regulating the HPT axis. Abnormalities in the hypothalamus can lead to reduced production of thyrotropin-releasing hormone (TRH), which stimulates the pituitary gland to produce TSH. Conditions like hypothalamic tumors, traumatic brain injuries, or radiation therapy to the brain can interfere with TRH production, subsequently causing secondary hypothyroidism. Pathophysiology I. Thyroid Hormone Synthesis and Release The synthesis and release of thyroid hormones are complex processes orchestrated by the thyroid gland in response to signals from the hypothalamic-pituitary-thyroid (HPT) axis. The thyroid gland actively takes up iodine from the bloodstream through specialized iodine transporters located on its surface. Iodine is a critical component of thyroid hormones, as both T3 and T4 molecules contain iodine atoms. Inside the thyroid follicular cells, iodine is combined with the amino acid tyrosine to form the precursors of thyroid hormones—monoiodotyrosine (MIT) and diiodotyrosine (DIT). The coupling of one molecule of MIT and one molecule of DIT results in the formation of triiodothyronine (T3), while the combination of two molecules of DIT gives rise to thyroxine (T4). These thyroid hormones are then stored within the colloid of the thyroid follicles. Upon receiving stimulation from thyroid-stimulating hormone (TSH) secreted by the pituitary gland, the stored thyroid hormones are released from the thyroid follicles into the bloodstream. The ratio of T3 to T4 released is approximately 1:20, with the majority of circulating thyroid hormones being T4. In peripheral tissues, particularly the liver and kidneys, a process known as deiodination converts a portion of T4 into the more active and potent T3. This conversion ensures that tissues receive an adequate supply of biologically active thyroid hormones to exert their metabolic e ects. ffi fl ff ff ffi ffi fi fi II. Mechanism of Autoimmune Thyroiditis Hashimoto's thyroiditis is an autoimmune disorder characterized by the presence of autoantibodies directed against various components of the thyroid gland, especially thyroglobulin and thyroid peroxidase. These autoantibodies, termed thyroid peroxidase antibodies (TPOAb) and thyroglobulin antibodies (TgAb), initiate an immune-mediated attack on the thyroid gland. The in ammatory process triggered by the autoimmune response leads to in ltration of lymphocytes and other immune cells into the thyroid tissue. This in ltration disrupts the normal architecture of the thyroid gland and causes the destruction of thyroid follicular cells, reducing their ability to synthesize and secrete thyroid hormones. Over time, this progressive destruction results in a decrease in the production of both T3 and T4, leading to hypothyroidism. Symptoms I. Fatigue and Weakness Fatigue and weakness are hallmark symptoms of hypothyroidism and often the most common complaints reported by a ected individuals. The reduction in circulating thyroid hormones slows down the body's metabolic processes, leading to a decrease in energy production and utilization. Patients may describe feeling tired and lethargic, even after adequate rest, and may experience di culty performing routine activities. Muscle weakness can also be present due to the diminished metabolic activity in muscle tissues. II. Weight Gain Unintentional weight gain is a frequent symptom observed in individuals with hypothyroidism. The reduced metabolic rate associated with low thyroid hormone levels causes a decrease in caloric expenditure. This, combined with increased uid retention and alterations in fat metabolism, leads to weight gain. Patients may nd it challenging to manage their weight despite e orts to control their diet and engage in physical activity. III. Cold Intolerance Patients with hypothyroidism often experience heightened sensitivity to cold temperatures. The decrease in thyroid hormone levels interferes with the body's ability to generate heat and maintain a stable body temperature. As a result, a ected individuals may feel unusually cold, even in mildly cool environments. Cold intolerance may contribute to a preference for warm surroundings and an increased need for layers of clothing. IV. Dry Skin and Hair Hypothyroidism can manifest in the integumentary system, leading to dry and coarse skin as well as brittle and dry hair. Thyroid hormones play a vital role in regulating the turnover and hydration of skin cells. Reduced thyroid hormone levels can disrupt this process, leading to decreased sebum production and compromised skin barrier function. Consequently, patients may experience rough and aky skin. Similarly, hair follicles become less e cient at producing natural oils, resulting in dry, brittle, and thinning hair. V. Constipation Gastrointestinal symptoms are prevalent in individuals with hypothyroidism, and constipation is a frequent complaint. Sluggish bowel movements occur due to the reduced motility of the digestive tract, which is in uenced by thyroid hormones. The decreased metabolic rate a ects smooth muscle contractions, leading to slower transit times and increased water absorption in the colon. This combination results in harder stools and di culty passing them, leading to constipation. fi ff fl ff ffi fi ff fi fl fi fi ff ffi ffi ff fl ffi fl ff VI. Depression and Mood Changes Hypothyroidism can have a signi cant impact on mental health and emotional well-being. The de ciency of thyroid hormones is associated with alterations in neurotransmitter activity in the brain, particularly a ecting serotonin, which plays a crucial role in regulating mood. Consequently, patients may experience feelings of sadness, depression, anxiety, and irritability. Cognitive functions may also be a ected, leading to di culties with memory and concentration. VII. Bradycardia Bradycardia, or a slower-than-normal heart rate, is a cardiac manifestation frequently observed in hypothyroidism. Thyroid hormones play a pivotal role in regulating the heart's electrical activity and cardiac output. In hypothyroidism, the reduction in thyroid hormone levels leads to a decreased heart rate, which can manifest as palpitations, lightheadedness, and even syncope in severe cases. The heart's overall contractility and response to physical and emotional stressors may be compromised. VIII.High Cholesterol Low thyroid hormone levels can decrease the number of LDL receptors on cells. LDL receptors are responsible for removing low-density lipoprotein (LDL) cholesterol from the bloodstream. When their activity is reduced, less LDL cholesterol is cleared from the blood, leading to higher LDL cholesterol levels. Diagnosis I. Clinical Evaluation and History The diagnosis of hypothyroidism begins with a comprehensive clinical evaluation and a detailed patient history. Attentive to patients presenting with symptoms, such as fatigue, weight gain, cold intolerance, constipation, and dry skin. A thorough medical history may reveal risk factors, family history of thyroid disorders, previous thyroid surgeries, or exposure to radiation therapy. Additionally, clinicians should inquire about any current medications such as amiodarone and lithium that may contribute to thyroid dysfunction. II. Thyroid Function Tests Thyroid function tests are essential for con rming the diagnosis of hypothyroidism and assessing the severity of thyroid hormone de ciency. These tests help evaluate the levels of thyroid hormones (T3 and T4) and thyroid-stimulating hormone (TSH) in the blood. Thyroid function tests are typically the rst line of investigation for suspected thyroid disorders. A. TSH (Thyroid-Stimulating Hormone) Levels TSH is a hormone secreted by the pituitary gland in response to thyroid hormone levels in the blood. In primary hypothyroidism, where the thyroid gland is underactive, the pituitary gland increases TSH secretion in an attempt to stimulate the thyroid to produce more hormones. As a result, elevated TSH levels are characteristic of primary hypothyroidism. B. T3 and T4 Levels Thyroid hormones, T3, and T4 are measured to assess the overall thyroid hormone production. In hypothyroidism, the levels of both T3 and T4 are typically lower than the reference range. However, T4 levels are generally more commonly measured, and T3 levels can be a ected to a lesser extent. III. Imaging Studies (Ultrasound) Imaging studies may be employed to evaluate the structure and size of the thyroid gland. Ultrasound helps identify goiter, nodules, or signs of in ammation and is especially useful in di erentiating between di use and nodular goiters and may aid in guiding ne-needle aspiration for further evaluation of thyroid nodules. IV. Other Labs Serum thyroid antibody testing can con rm suspected autoimmune thyroid disease. Additionally, thyroid peroxidase antibody measurements may also be considered in patients with subclinical hypothyroidism or recurring miscarriages. Treatment fi ff ff fi fi fl fi Levothyroxine (T4 Replacement) Levothyroxine, a synthetic form of the T4 hormone, is the cornerstone of hypothyroidism treatment. As T4 is the major thyroid hormone produced by the thyroid gland, levothyroxine serves as an excellent replacement therapy. Levothyroxine is more chemically stable, unlike thyroxine which easily degrades fi ff I. outside the body. It e ectively replenishes the de cient thyroid hormones, restoring the body's metabolic balance. A. Mechanism of Action Levothyroxine acts similarly to endogenous T4 by entering target cells and binding to thyroid hormone receptors in the nucleus. This binding initiates a cascade of events that regulate gene expression and cellular metabolism. The increased availability of thyroid hormones through levothyroxine administration helps reverse the clinical manifestations of hypothyroidism and alleviates the associated symptoms. B. Starting Dose and Monitoring Synthroid recommends a starting dose of 1.6 mg/kg/day. 12.5 to 25 mcg increments every 4 to 8 weeks as needed until the patient is euthyroid. Tablets start from 25 up to 300 mcg per tablet. C. Interactions and Precautions Levothyroxine can interact with certain foods such as co ee, soy, and dietary ber, a ecting its absorption and e cacy. Patients should take levothyroxine on an empty stomach (1 hour before a meal). D. Adverse E ects If the dosage is to elevated, the patient may present with hyperthyroidism symptoms. These include, anxiety, nervous energy, tremors, di culty concentrating, feeling overheated, racing heart, di culty sleeping, and feeling irritable, or erratic. II. Liothyronine (T3 Replacement) Liothyronine, a synthetic form of T3, is less commonly used in the treatment of hypothyroidism due to its relatively short half-life and potential for causing uctuations in hormone levels. Unlike levothyroxine, liothyronine may be taken multiple times a day to maintain steady levels of T3. It may be considered in certain cases where T4 alone is insu cient to alleviate symptoms. Nonetheless, CYTOMEL o ers daily leothyronine dosages. ff ffi ffi ff fi ff fl fi ffi ffi ff fi ffi ff A. Limited Use and Considerations Liothyronine is not a rst-line treatment due to its short duration of action and the potential for causing hyperthyroid symptoms if not dosed appropriately. It may be considered in patients who have di culty converting T4 to T3 or those with persistent symptoms despite adequate levothyroxine therapy. B. Adverse E ects Liothyronine causes more adverse cardiac e ects such as fast or irregular heartbeats, chest pain and di culty breathing. It may also present with common hyperthyroidism symptoms. C. Cost On average, liothyronine is more expensive the levothyroxine. On GoodRX, the cost of 5 mcg tablets is $26.92, while 50 mcg levothyroxine tablets are $9.26. D. Starting and Maintenance Dose The starting dose for liothyronine is 25 mcg orally once daily. Increase the dose by 25 mcg daily every 1 or 2 weeks, if needed. The usual maintenance dose is 25 mcg to 75 mcg once daily. Prognosis I. Long-term Outlook with Proper Treatment With appropriate and timely treatment, the long-term prognosis for individuals with hypothyroidism is generally favorable. Levothyroxine, the standard treatment for most cases, e ectively restores thyroid hormone levels, leading to symptom resolution and improved quality of life. When patients adhere to their prescribed medication regimen and undergo regular follow-up with healthcare providers, they can achieve stable thyroid hormone levels within the normal range. Consequently, most individuals experience relief from hypothyroid symptoms and can lead healthy, productive lives. II. Complications of Untreated Hypothyroidism If left untreated, hypothyroidism can lead to various complications that may signi cantly impact a patient's health and well-being. Prolonged de ciency of thyroid hormones can a ect multiple organ systems and increase the risk of several medical conditions, including: A. Cardiovascular Complications: Untreated hypothyroidism can lead to increased levels of cholesterol and triglycerides, which may contribute to atherosclerosis (plaque buildup in arteries) and raise the risk of heart disease, including heart attacks and strokes. B. Myxedema Coma: In severe cases of untreated hypothyroidism, a life-threatening condition known as myxedema coma can occur. This rare but critical condition results from extreme thyroid hormone de ciency and is characterized by altered mental status, hypothermia, and multi-organ failure. C. Infertility and Pregnancy Complications: Hypothyroidism can lead to menstrual irregularities and fertility problems in women. Pregnant women with untreated or poorly controlled hypothyroidism have an increased risk of pregnancy complications, including miscarriage, preterm birth, and developmental issues in the baby. D. Mental Health Impairment: Chronic untreated hypothyroidism can contribute to cognitive impairment, memory di culties, and mood disorders such as depression and anxiety. E. Myopathy and Muscle Weakness: Untreated hypothyroidism can lead to muscle weakness, aches, and myopathy, a ecting the individual's mobility and daily activities. III. Potential Risks and Challenges in Management While hypothyroidism is generally well managed with thyroid hormone replacement therapy, there are certain challenges and potential risks in its management: A. Suboptimal Dosage: Determining the correct dosage of thyroid hormone replacement can be complex and requires ongoing monitoring. Over-treatment or under-treatment may lead to adverse e ects, including symptoms of hyperthyroidism or persistence of hypothyroid symptoms. fi ff ff fl ff fi ffi ff ff fi ffi ff B. Medication Compliance: Adherence to medication is essential for maintaining stable thyroid hormone levels. Non-compliance or inconsistent dosing can lead to uctuations in thyroid hormone levels and compromise symptom control. C. Interactions and Absorption: Some medications and supplements can interact with thyroid hormone replacement, a ecting its absorption or metabolism. Healthcare providers must consider potential drug interactions and educate patients about proper medication administration. D. Subclinical Hypothyroidism: Management of subclinical hypothyroidism (mild elevation of TSH with normal T3 and T4 levels) remains controversial. In this condition, the decision to initiate thyroid hormone therapy depends on the patient's symptoms and risk factors. E. Pregnancy Management: Pregnant women with hypothyroidism require careful monitoring and adjustment of thyroid hormone replacement, as hormone requirements may change during pregnancy. Harder Clinical Case A 44-year-old woman comes to the physician because of a 6-month history of fatigue, constipation, and a 7kg (15.4-lb) weight gain. Menses occur irregularly in intervals of 40–50 days. Her pulse is 51/min, and blood pressure is 145/86 mm Hg. Examination shows conjunctival pallor and cool, dry skin. There is mild, nonpitting periorbital edema. Serum thyroid-stimulating hormone concentration is 8.1 μU/mL. Treatment with the appropriate pharmacotherapy is initiated. After several weeks of therapy with this drug, which of the following hormonal changes is expected? 1. Decreased T4 2. Increased reverse T3 3. Increased thyroxine-binding globulin 4. Increased TRH ff 5. Decreased T3 References 1. amboss.com 2. C Y T O M E L ® H i g h l i g h t s ( l i o t h y r o n i n e s o d i u m ) | P z e r M e d i c a l I n f o r m a t i o n - U S . www.p zermedicalinformation.com. Published 2023. Accessed July 26, 2023. https:// www.p zermedicalinformation.com/en-us/cytomel/highlights#S2.1 3. Dirar AM, Kalhan A. Hypothyroidism during pregnancy: Controversy over screening and intervention. World Journal of Obstetrics and Gynecology. 2018;7(1):1-16. doi:https://doi.org/10.5317/wjog.v7.i1.1 4. Dosing & Administration - SYNTHROID® (levothyroxine sodium tablets). www.synthroidpro.com. Accessed July 26, 2023. https://www.synthroidpro.com/ dosing#:~:text=Full%20replacement%20dose%20is%201.6 5. Kumar V, Abbas AK, Aster JC, Perkins JA. Robbins Basic Pathology. 10th ed. Philadelphia, Pennsylvania Elsevier; 2018. 6. Le T, Vikas Bhushan, Tolles J. First Aid for the USMLE Step 1 2011. Mcgraw Hill Medical; 2011. 7. Sattar HA. Fundamentals of Pathology : Medical Course and Step 1 Review. Pathoma.com; 2021. 8. Stevens CW. Brenner and Stevens’ Pharmacology. 7th Edition. Elsevier - Health Science; 2022. Answers Question #1 Attending’s Notes: In the early stages of this condition, patients may present with weight loss, heat intolerance, and ne tremor. 2. Autoimmune thyroid disease (72%) Hashimoto thyroiditis is the most common cause of hypothyroidism in the United States and is characterized by progressive destruction of thyroid tissue by antithyroid peroxidase antibodies and antithyroglobulin antibodies. Initially, it may manifest with transient hyperthyroidism, before progressing to hypothyroidism. Hypothyroidism results in a generalized decrease of the basal metabolic rate, which can present with weight gain, fatigue, dry skin and brittle nails, along with concentration and memory impairment. Questions #2 Attending's Notes: The patient's signs and symptoms of fatigue, constipation, weight gain, menstrual irregularities, bradycardia, hypertension, dry skin, and periorbital edema are all suggestive of hypothyroidism. The increased serum thyroid-stimulating hormone (TSH) concentration indicates that she has primary hypothyroidism, for which the treatment is hormone replacement with levothyroxine. fi fi fi fi 2. Increased reverse T3 (52%) Levothyroxine is a synthetic form of T4, which is converted to reverse T3 (biologically inactive) and T3 (biologically active) by a deiodinase in the blood. Since an increase of reactants leads to an increase in products, rT3 would be expected to increase after several weeks of levothyroxine therapy. T3 and T4 negatively regulate the secretion of TRH from the hypothalamus and of TSH from the anterior pituitary.