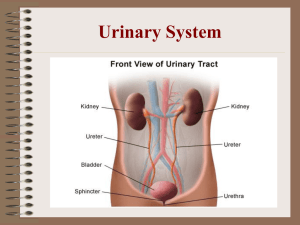
Exam #2 BluePrint Med Math: 3 questions UTI: 5 questions URINARY TRACT INFECTIONS ● Pathogenic microorganisms in the urinary tract. ● Classified based on their locations. ● Lower UTI’s: includes the bladder and structures below the bladder. ● Upper UTI’s: includes the kidneys and ureters. LOWER URINARY TRACT INFECTIONS (Cystitis) ● Causes: female gender, DM, older adults or cognitive impairment, inability to empty bladder, bladder tumors, sexual intercourse, catherization, and calculi. ● S/S: depends on location ● Uncomplicated- burning on urination, urinary frequency & urgency, hematuria, back pain ● Complicated- systemic symptoms such as shock. Organism: E. coli, Proteus, Klebsiella, Pseudomonas, Staphylococcus, and Enterococcus. Labs & Diagnostics: elevated WBC with a “left shift”, RBC & WBC in urine. Culture: identifies organism. Analysis/Dipstick: Leukocytes Esterase (WBC), Nitrates, & Hematuria. X-ray, CT Scans, and Ultrasounds. Management: Medications ● *Nitrofurantoin (Macrobid)- Renal insufficiency. (Treatment of choice) ● Ciprofloxacin (Cipro)- Achilles tendon rupture. ● Trimethoprim-Sulfamethoxazole (Bactrim)– Look out for Steven Johnson Syndrome. ● Phenazopyridine (Pyridium)- turns urine to an orange color. Treatment ● Increase oral hydration. ● Daily intake of cranberry juice to prevent & control symptoms. ● Avoid caffeine, alcohol, and citrus fruits. ● Increase intake of Vitamin C. ● Antispasmodic agents to relieve bladder irritability and pain. Upper Urinary Tract Infections Bacterial infection in the kidney and renal pelvis. It can be acute or chronic and it affects urine elimination. Causes: obstruction by stones, kidney cancer, scarring from pelvic radiation or surgery, recurrent infection, injury, urinary stasis, and reflux. Organism: Escherichia coli, Enterococcus faecalis, Klebsiella species, Pseudomonas aeruginosa, and Candida. History: young adult, recent UTI S/S: chills, fever, leukocytosis, bacteriuria, pyuria, and + CVA tenderness. Labs/Diagnostic: UA & Culture, CT Scan, Ultrasound, & IV pyelogram. ● ● ● ● Tylenol to alleviate pain. Antibiotics- drug depends on the result of the urine culture. Increase fluid intake. Follow-up urine culture is obtained 2 weeks after completion of antibiotic therapy. Renal Calculi/Ureterolithiasis: 4 questions UROLITHIASIS AND NEPHROLITHIASIS Urolithiasis: presence of calculi (stones) in the urinary tract. Nephrolithiasis: formation of stones in the kidney. Stones are formed when the urine concentration of the minerals build up in the body. Causes: inflammatory bowel disorder, medications, & dehydration. S/S: excruciating pain that hematuria, N/V, frequency & urgency. Labs/Diagnostic: CBC, BMET, KUB, non-contrast CT Scan, UA, & 24 -hour urine. Pain management- Opioids PRN. ● IV fluids- 0.9% NS. ● STRAIN all urine. ● Calcium stones- thiazide diuretics. ● Uric acid stones- low purine diet & Allopurinol to decrease uric acid. ● Cystine stones- low protein diet. ● Oxalate- consume foods that get rid of oxalate in the urine. Surgical Management: ● Extracorporeal shock wave lithotripsy (ESWL)- shock waves to break up stone. ● Ureteroscopy- scope is used to visualize stone & a stent is placed. ● Percutaneous nephrolithotomy- removal of stone. Bladder Cancer: 3 questions ● Cancer cells in the bladder. ● Common site of growth is within the lining of the bladder. ● Risk Factors: smoking, family history, pelvic radiation therapy, & occupational exposure to chemicals. ● Older than 55 years old & Caucasian men. S/S: painless hematuria, frequency, urgency, pelvic of back pain, and dysuria. ● Labs & Diagnostic: ● UA- hematuria. ● Biopsy of bladder. ● CT scan, MRI, and Cystoureterography- helps identify obstruction and helps with staging of cancer. BLADDER CANCER MANAGEMENT ● Depends on the grade of the tumor and the stage of tumor growth. ● Chemotherapy and Radiation- can be done before and after surgery. ● BCG Live (bacille Calmette-Guérin): a live virus compound, is used to prevent tumor recurrence of superficial cancers. ● Surgery: Cystectomy & TURBT ● Cystectomy: can be simple or radial removal. Radial removal requires a urinary diversion. ● Transurethral resection of the bladder tumor(TURBT): removal of the tumor. AKI: 4 questions pg. 4168 Acute kidney injury (AKI) is the rapid loss of renal function due to damage to the kidneys. Causes: hypovolemia, hypotension, heart failure, kidneys, and obstruction to kidneys or urinary tract 3 categories: 1. Prerenal – There is hypoperfusion of the kidneys due to the stress response. Causes are hypovolemia, decreased BP, heart failure (left ventricle becomes big and weak, decreasing cardiac output) 2. Intrarenal – There is damage inside the kidneys. Causes are meds (aminoglycosides ending in -mycin, NSAIDS), myoglobin/rhabdomyolysis (toxic to kidneys), and acute pyelonephritis 3. Postrenal – There is something causing pressure in the bladder, causing backflow to the kidneys. Causes are BPH in men and pregnancy in women 4 phases: 1. Initiation - Starts with kidney injury and ends once patient becomes oliguric (due to angiotensin II) 2. Oliguria - Decreased urine output and patient may start to have signs of uremia (waste products/toxins in blood). Hemoconcentration occurs (more solute than solvent in blood). 3. Diuresis - GFR improves/increases and patient will have increased urine output. Hemodilution occurs (more solvent than solute in blood). 4. Recovery - Improvement of renal function. May take 3 to 12 months. Signs and symptoms: Affects ALL systems. ● Decreased oxygenation - drowsiness, confusion, lethargy, headache, seizures, neuro issues ● Increased blood flow to the heart - tachycardia, increased BP ● Increased blood flow to the lungs - tachypnea, shortness of breath (fluid buildup from third-spacing) ● Hypocalcemia - muscle twitching ● Decreased blood flow to the stomach - nausea, vomiting, decreased motility ● Retaining fluid - oliguria ● Decreased blood flow to the skin - dry skin and mucous membranes, pallor, pruritus (buildup of toxins because kidneys can’t excrete, so it goes out through the pores) Lab values: ● Decreased urine output - oliguria ● Kidneys not excreting - elevated BUN/Creatinine, hyperkalemia, hyperphosphatemia, hypocalcemia ● Decreased GFR - kidneys can’t filter ● Decreased H/H - kidneys not making erythropoietin (EPO), leading to anemia Management: ● AVOID or limit exposure to nephrotoxic meds - aminoglycosides, NSAIDs ● TREAT the underlying cause - e.g. treat rhabdomyolysis with 0.9% NS, treat AKI during pregnancy by delivering the baby ● IV fluids - 0.9% NS ● Monitor electrolytes - potassium, calcium, phosphorus, magnesium ● Strict intake and output - due to third spacing ● Promote rest periods to prevent muscle fatigue ● Meticulous skin care and provide emotional support - pruritus and scratching leads to skin breakdown ● If severe - may need emergency dialysis Hemodialysis: 4 questions For anyone that is acutely ill or needs permanent renal replacement therapy. For example, the patient presents with uric frost or toxic buildup. ● 2 main reasons it’s needed: hyperkalemia, metabolic acidosis ● Requires consent ● Need vascular access - fistula - connects artery and vein ○ Assess access site - listen for bruit and feel for thrill ○ Quinton catheter, Permacath, or central line used temporarily while fistula take a couple months to mature - make sure it doesn’t get infected! ● Before dialysis: check weight, vital signs, hepatitis B status, and blood sugar if diabetic ● After dialysis: recheck weight, assess for weakness and fatigue, recheck vital signs (if BP is low, give albumin) ● Hold BP meds, can have blood transfusion and antibiotics ● NPO (risk for aspiration) Epoetin Alfa: 2 questions (Procrit) Epoetin is used to treat severe anemia in patients on kidney dialysis or for those not on dialysis Check the BP before and after administration and report the headache to the provider. Absence of pallor when receiving Epoetin alfa. Peritoneal Dialysis: 3 questions Used for patients that are unable or unwilling to undergo hemodialysis or kidney transplantation. Maintain aseptic technique, wear face mask. Can be done at home Dialysate is warmed up Concern: peritonitis (cloudy dialysate, normal is straw pink tinged), infection, rebound tenderness Rhabdomyolysis: 2 questions This muscle tissue breakdown results in the release of a protein (myoglobin) into the blood. Myoglobin can damage the kidneys. Symptoms include dark, reddish urine, a decreased amount of urine, weakness, and muscle aches. Early treatment with aggressive fluid replacement reduces the risk of kidney damage. *** It is a risk factor for intrarenal AKI darker tea-colored urine – indicating renal failure Renal Transplant: 3 questions Treatment of choice for patients with chronic kidney disease. From a living or deceased donor. Extensive medical evaluation is done (compatibility). Educate (post-op expectations, pain management, recovery) Witness consent Dialysis prior if patient routine VS, head to toe Monitor for rejection ➢ Hyperacute: within 24 hrs. New kidney has to be discarded. ➢ Acute: few days to weeks to happen. S&S of renal disfunction start to happen. Patient has to take immunosupressive therapy. Immunosuppresive therapy Monitor for signs of rejection, infection & prevent it at all cost. Monitor urine output (is the new organ working properly?), electrolyte changes (K, Ph, Ca). Provide opportunities for patient & donor to express thoughts & fears, support and refer to support groups (lifestyle changes fro life. No alcohol, smoking, drugs, balanced diet) . CKD & Labs: 3 questions ⬇️GFR (non functioning glumeruli) ⬇️BUN & Creat (sensitive indicator of renal fnx) GFR & CKD: 2 questions GFR is the true indicative of Kindey function Normal value: > 90 mL/min Stage 4: 15-29 mL/min (in clinical practice, nephologist referral) Stage 5: (End stage) <15 mL/min Nephrotic syndrome: 2 questions There is increased permeability, thus, large proteins pass thru the cell membrane. Oncotic pressure is affected ⬇️ Congenital (inherited, as immune response. Histamine causes vasodilation) Secondary disorder (autoimmune Lupus, HIV, HF, DM) Idiopathic (most common in kids) S/S Weight gain, 3rd spacing, hematuria (affected permeability), high BP Labs Marked proteinuria (>3g/day loss) ⬇️BUN & Creat ⬇️Cholesterol & 3glicerides (liver tries to compensate) Diagnostic: physical exam, kidney biopsy (⬇️risk for bleeding, kidney is very vascular) Management Weight, I&O Temp monitor (⬇️slighliest change: notify provider) Antibiotics, IV lasix, steroids (they supress immune system) AVOID sick contact, use aseptic technique (⬇️⬇️immune system is suppressed, reverse isolation⬇️⬇️) Prostate Cancer: 3 questions ● Second leading cause of death in men. ● Slow growing. ● Risk Factors: increase age, family history, excessive amounts of red meat or dairy products that are high in fat, gene mutations ((HPC1) and BRCA1 and BRCA2 mutations). S/S: difficulty with frequency of urination, urinary retention, decreased size and force of the urinary stream. Labs & Diagnostics: ● Digital rectal exam (DRE). ● PSA. ● Biopsy- diagnose cancer. ● Ultrasound, Bone scan, CT scan & MRI. Treatment: ● Depends on life expectancy, symptoms, risk of recurrence, complications, and patient choice. ● Radical prostatectomy- 1st line ● Chemotherapy ● Radiation therapy ● Teletherapy (external)- beam radiation ● Brachytherapy (internal)- implant of radioactive seeds under anesthesia. ● Hormone (ADT)- decrease the amount of testosterone. Surgical Management: ● Transurethral Resection of the Prostate (TURP) ● ● ● ● ● May cause trigger retrograde ejaculation. Prostatectomy (Simple or Radical) Pre-Op: provide education on surgery and what to expect, labs, and NPO. Intra-Op: Video: Post-Op Care: Monitor for bleeding- light pink is normal. BPH: (BENIGN PROSTATIC HYPERPLASIA) 3 questions ● Noncancerous enlargement or hypertrophy of the prostate. ● Common in men 40 years or older. ● Risk Factors: smoking, heavy alcohol consumption, obesity, reduced activity level HTN, CAD, DM, and a Western diet. S/S: urinary frequency, urgency, nocturia, hesitancy, abdominal straining with urination. Labs & Diagnostics: ● DRE- large, rubbery, and nontender prostate gland. ● CBC, BMET, PSA, UA (hematuria). ● Urethrocystoscopy and ultrasound. ● BENIGN PROSTATIC HYPERPLASIA (BPH) Treatment: ● Alpha-adrenergic blockers (Hytrin & Flomax): improves urine flow. ● 5-alpha-reductase inhibitors finasteride (Proscar): prevent the conversion of testosterone to DHT and decrease prostate size. ● Monitor for side effects of medications. BENIGN PROSTATIC HYPERPLASIA (BPH) ● Alternative therapies: Saw Palmetto. ● Transurethral microwave thermotherapy (TUMT)-application of heat to prostatic tissue. ● Transurethral resection of the prostate (TURP)- done for clients with moderate & severe disease. ● Prostatectomy- surgical removal of the inner portion of the prostate. Prostatitis: 2 questions ● Inflammation of the prostate gland. ● Associated with lower urinary tract infection and sexual discomfort/dysfunction. Organism: Escherichia coli, Klebsiella and Proteus. S/S: fever, dysuria, frequency, urgency, hesitancy, and nocturia. ● ● ● ● ● Monitor vital signs and assess for sepsis. Antibiotics: Bactrium, Cipro, and Flomax. Analgesics PRN. Warm sitz baths (10 to 20 minutes) may be taken several times daily. AVOID foods & liquid that will irritate the prostate. Acute pyelonephritis: 2 questions ● Bacterial infection in the kidney and renal pelvis. ● It can be acute or chronic and it affects urine elimination. ● Causes: obstruction by stones, kidney cancer, scarring from pelvic radiation or surgery, recurrent infection, injury, urinary stasis, and reflux. ● ACUTE Pyelonephritis Organism: Escherichia coli, Enterococcus faecalis, Klebsiella species, Pseudomonas aeruginosa, and Candida. History: young adult, recent UTI S/S: chills, fever, leukocytosis, bacteriuria, pyuria, and + CVA tenderness. Labs/Diagnostic: UA & Culture, CT Scan, Ultrasound, & IV pyelogram. ● ● ● ● Tylenol to alleviate pain. Antibiotics- drug depends on the result of the urine culture. Increase fluid intake. Follow-up urine culture is obtained 2 weeks after completion of antibiotic therapy.