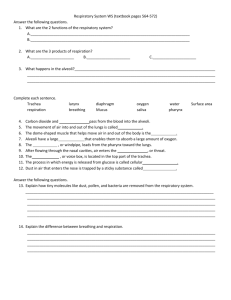
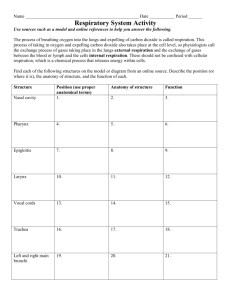
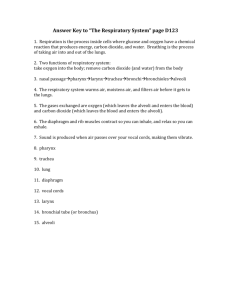
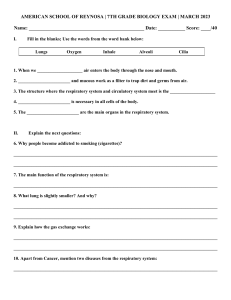
Respiratory System Chapter 13 Learning Objectives Identify the organs of the respiratory system & general function of each. Compare the volumes & capacities of air exchanged during ventilation. Explain the following gas principles: Dalton’s Law, Boyle’s Law and Henry’s Law. Explain how blood transports both oxygen & carbon dioxide. Describe the factors that affect the binding of hemoglobin & oxygen. Compare & contrast the roles of peripheral and central chemoreceptors in the regulation of respiration. Functions Gas exchange – between the external environment and the blood Filters, humidifies, and warms inspired air Production of sound Smell Maintains pH homeostasis Anatomy Review Nose Pharynx Larynx Trachea Bronchi Bronchioles Alveolar ducts Alveoli Anatomy Review Respiratory Membrane Site of gas exchange between the alveoli and the blood Formed by the alveolar wall and the capillary wall Anatomy Review Pleural Sac – double walled membrane surrounding the lungs Visceral pleura - covers the lung surface Parietal pleura - lines the walls of the thoracic cavity Pleural fluid fills the area between layers to allow gliding and resist separation ↑ pleura → ↑ pressure → lung collapse ↓ pleura → ↑ friction Respiratory Pressures Respiratory pressures are described relative to atmospheric pressure @ sea level Patm = 760 mm Hg OR 0 mm Hg = 760 mm Hg Negative pressure: -1mm Hg = 759 mm Hg Positive pressure: + 1 mm Hg = 761 mm Hg Respiratory Pressures Intrapulmonary pressure (Ppul) – pressure within the alveoli Intrapleural pressure (Pip) – pressure within the pleural cavity Respiratory Pressures Transpulmonary pressure – difference between the intrapulmonary and intrapleural pressures Intrapleural pressure is always less than intrapulmonary pressure ( -4 mmHg ) Keeps the airways open Pneumothorax (puncture in lung wall) tabbed chest wound, outside air travels in Ex: edema due to bleeding or fluid build air from lung travels into pleural cavity Events of Respiration Pulmonary ventilation External respiration Gas transport Internal respiration Pulmonary Ventilation Pulmonary ventilation – moving air in and out of the lungs Mechanical process that depends on volume changes in the thoracic cavity Caused by the contraction/relaxation of intercostal muscles and the diaphragm ∆ Volume → ∆ Pressure → flow of gases Boyle’s law – the relationship between the pressure and volume of gases P1V1 = P2V2 P = pressure of a gas in mm Hg V = volume of a gas in cubic millimeters Respiratory Pressures Intrapulmonary pressure and intrapleural pressure fluctuate with the phases of breathing Phases of Ventilation Two phases Inspiration – flow of air into lung Intrapulmonary P decreases as thoracic cavity expands; air moves in Expiration – air leaving lung Intrapulmonary P increases as lungs recoil; air moves out Events of Inspiration Events of Expiration Factors Affecting Ventilation Lung Compliance - the ease with which the lungs can be expanded Elasticity – how readily the lungs recoil after stretch Reduced by factors that decease distension of the lung tissue and surrounding thoracic cage Reduced by pulmonary edema, fibrosis (scar tissue), surface tension of the alveoli Elastic CT and surface tension of the alveoli Compliance vs. Elasticity Ex: Plastic bag vs. Balloon Factors Affecting Ventilation Surface tension The attraction of liquid molecules to one another in the alveolus The liquid coating is always acting to reduce the alveoli to the smallest possible size Surfactant, a detergent-like complex, reduces surface tension and helps keep the alveoli from collapsing Factors Affecting Ventilation Airway Resistance Friction is the major source of resistance to airflow The relationship between flow (F), pressure (P), and resistance (R) is: Affected by: P F= R Autonomic Nervous System – controls diameter of bronchioles Sympathetic – bronchodilation decreases resistance Parasympathetic – bronchoconstriction increases resistance Chronic Obstructive Pulmonary Diseases: asthma, bronchitis, emphysema Airway Resistance Example Normal breathing COPD- intrapleural pressure closes off already blocked small airways Testing Respiratory Function Spirometer – an instrument consisting of a hollow bell inverted over water, used to evaluate respiratory function Spirometry can distinguish between: Obstructive pulmonary disease – increased airway resistance Difficulty exhaling Restrictive disorders – reduction in lung compliance and capacity from structural or functional lung changes Difficulty inhaling Respiratory Volumes Tidal volume (TV) – air that moves into and out of the lungs during normal breathing (~ 500 ml) Inspiratory reserve volume (IRV) – air that can be inspired forcibly beyond the tidal volume (2100–3200 ml) Respiratory Volumes Expiratory reserve volume (ERV) – air that can be evacuated from the lungs after a tidal expiration (1000–1200 ml) Residual volume (RV) – air left in the lungs after strenuous expiration (1200 ml) Respiratory Volumes Dead space volume Air that remains in conducting zone and never reaches alveoli ~150 ml Functional volume Air that actually reaches the respiratory zone ~350 ml Respiratory Capacities Inspiratory capacity (IC) – total amount of air that can be inspired after a tidal expiration (IRV + TV) Expiratory capacity (EC) - total amount of air that can be expired after a tidal inspiration (ERV + TV) Functional residual capacity (FRC) – amount of air remaining in the lungs after a tidal expiration (RV + ERV) Respiratory Capacities Vital capacity (VC) – the total amount of exchangeable air (TV + IRV + ERV) Total lung capacity (TLC) – sum of all lung volumes (approximately 6000 ml) (VC + RV) Testing Respiratory Function Total ventilation – total amount of gas flow into or out of the respiratory tract in one minute (respiratory rate X tidal volume) Ex: 12 breaths/min X 500 mL/breath = 6000mL/min Forced vital capacity (FVC) – gas forcibly expelled after taking a deep breath Forced expiratory volume (FEV) – the amount of gas expelled during specific time intervals of the FVC Testing Respiratory Function Obstructive vs. Restrictive diseases Obstructive disease - increase in RV, decrease in ERV Restrictive disease -reduction in VC, TLC, and IRV External Respiration External respiration – gas exchange between pulmonary capillaries and alveoli across the respiratory membrane Oxygen movement from the alveoli into the blood Carbon dioxide movement out of the blood into the alveoli External Respiration Factors influencing the movement of oxygen and carbon dioxide across the respiratory membrane Partial pressure gradients and gas solubility Matching of alveolar ventilation and pulmonary blood perfusion Structural characteristics of the respiratory membrane Dalton’s Law – partial pressure gradients Total pressure exerted by a mixture of gases is the sum of the pressures exerted independently by each gas in the mixture The partial pressure of each gas is directly proportional to its percentage in the mixture Percent Partial Pressure 78% Nitrogen = 593 mmHg 21% Oxygen= 160 mmHg 0.9% Carbon Dioxide = 7 mmHg Factors Influencing External Respiration Partial Pressure Gradients Oxygen movement into the blood from the alveoli The alveoli have a higher PO2 than the blood Oxygen moves by diffusion towards the area of lower partial pressure Carbon dioxide movement out of the blood to the alveoli Blood returning from tissues has a higher PCO2 than the air in the alveoli Henry’s Law – gas solubility Gas will dissolve into liquid in proportion to its partial pressure The amount of gas that will dissolve in a liquid also depends upon its solubility Various gases in air have different solubilities: Carbon dioxide is the most soluble; 20X more soluble than oxygen Nitrogen is practically insoluble in plasma Factors Influencing External Respiration Hemoglobin acts as a “storage depot” for O2 by removing it from the plasma as soon as it is dissolved This keeps the plasma’s PO2 low and prolongs the partial pressure gradient between the plasma and the alveoli Leads to a large net transfer of O2 Factors Influencing External Respiration Ventilation and perfusion are matched for efficient gas exchange Ventilation – the amount of gas reaching the alveoli Perfusion – the blood flow reaching the alveoli Changes in PCO2 and PO2 in the alveoli cause local changes: Poor ventilation Alveolar CO2 is high and O2 is low: Bronchioles will dilate and arterioles constrict Poor perfusion Alveolar CO2 is low and O2 is high: Bronchioles will constrict and arterioles will dilate Local Controls of Ventilation & Perfusion Factors Influencing External Respiration Structural characteristics of the respiratory membrane: Are only 0.5 to 1 m thick, allowing for efficient gas exchange Have a total surface area (in males) of about 60 m2 (40 times that of one’s skin) Thickening causes gas exchange to be inadequate: inflammation, edema, mucus, fibrosis Decrease in surface area with emphysema, when walls of adjacent alveoli breakdown Pathological conditions that reduce ventilation and gas exchange Gas Transport in the Blood Oxygen transport in the blood 98% of oxygen is transported attached to hemoglobin (oxyhemoglobin [HbO2]) A small amount is carried dissolved in the plasma (~2%) Each Hb molecule binds four oxygen atoms in a rapid and reversible process Hemoglobin Saturation/Dissociation Curve The % hemoglobin saturation depends on the PO2 of the blood In the alveoli – 98% saturation In the tissues - ~75% saturation In an exercising muscle the PO2 equals ~ 20 mmHg What would be the % saturation of Hb? Factors Affecting Saturation of Hemoglobin Increases in the following factors decreases hemoglobin’s affinity for oxygen Temperature H+ PCO2 2,3-diphosphoglycerate (DPG) (byproduct of glycolysis) These factors modify the structure of hemoglobin and alter its affinity for oxygen and enhances oxygen unloading from Hb These parameters are higher in systemic capillaries supplying tissues, where oxygen unloading is the goal Factors Affecting Saturation of Hemoglobin Summary of factors contributing to total oxygen content of arterial blood: Internal Respiration Exchange of gases between blood and body cells Oxygen diffuses from blood into tissue Carbon dioxide diffuses out of tissue into blood Gas Transport in the Blood Carbon dioxide is transported in the blood in three forms: Dissolved in plasma – 7% Bound to hemoglobin – 23% is carried in RBCs as carbaminohemoglobin, at a different binding site than oxygen Most is carried as bicarbonate ions in plasma – 70% is transported as bicarbonate (HCO3–) Transport of Carbon Dioxide Carbon dioxide diffuses into RBCs and combines with water to form carbonic acid (H2CO3), which quickly dissociates into hydrogen ions and bicarbonate ions Exchange of Carbon Dioxide At the tissues: Bicarbonate quickly diffuses from RBCs into the plasma The chloride shift – to counterbalance the outrush of negative bicarbonate ions from the RBCs, chloride ions (Cl–) move from the plasma into the erythrocytes Exchange of Carbon Dioxide At the lungs, these processes are reversed Bicarbonate ions move into the RBCs and bind with hydrogen ions to form carbonic acid Carbonic acid is then split by carbonic anhydrase to release carbon dioxide and water Carbon dioxide then diffuses from the blood into the alveoli Gas Transport in the Blood Control of Respiration Medullary centers: The dorsal respiratory group (DRG), or inspiratory center: Appears to be the pacesetting respiratory center Excites the inspiratory muscles and sets eupnea (12-15 breaths/minute) Becomes dormant during expiration The ventral respiratory group (VRG) is involved in forced expiration Control of Respiration Pons centers – pneumotaxic and apneustic areas Influence and modify activity of the medullary centers Smoothes out inspiration and expiration transitions Depth and Rate of Breathing Cortical controls are direct signals from the cerebral motor cortex that bypass medullary controls (conscious control) Examples: voluntary breath holding, taking a deep breath Hypothalamic controls act through the limbic system to modify rate and depth of respiration Example: breath holding that occurs in anger, hyperventilation from anxiety Depth and Rate of Breathing Three chemical factors affecting ventilation: Carbon dioxide levels- main regulatory chemical for respiration ↑ CO = ↓ blood pH 2 Increased CO increases respiration 2 Changes in CO act directly on central chemoreceptors 2 in the medulla oblongata Oxygen levels Peripheral chemoreceptors in the aorta and carotid artery detect oxygen concentration changes Information is sent to the medulla oblongata via the vagus nerve Arterial pH PCO2 Levels A rise in PCO2 levels (hypercapnia) increases ventilation Changing PCO2 levels are monitored by central chemoreceptors of the medulla Carbon dioxide in the blood diffuses into the cerebrospinal fluid where it is hydrated Resulting carbonic acid dissociates, releasing hydrogen ions (decreases pH) PCO2 Levels Hyperventilation – increased depth and rate of breathing that: Occurs in response to hypercapnia Quickly flushes carbon dioxide from the blood Acidosis- do not breath into bag so that you can reduce CO2 Anxiety- breath into bag to keep CO2 PCO2 Levels Hypoventilation – slow and shallow breathing due to abnormally low PCO2 levels Apnea (breathing cessation) may occur until PCO2 levels rise PO2 Levels Arterial oxygen levels are monitored by peripheral chemoreceptors in the aortic and carotid bodies Substantial drop in arterial PO2 (to 60 mm Hg) is needed before oxygen levels become a major stimulus for increased ventilation If carbon dioxide is not removed (e.g., as in emphysema and chronic bronchitis), chemoreceptors become unresponsive to PCO2 chemical stimuli In such cases, PO2 levels become the principal respiratory stimulus (hypoxic drive) Arterial pH Levels Changes in arterial pH can modify respiratory rate even if carbon dioxide and oxygen levels are normal Increased ventilation in response to falling pH is mediated by peripheral chemoreceptors in the aorta and carotid body Arterial pH Levels Acidosis may reflect: Accumulation of lactic acid Excess fatty acid metabolism in patients with diabetes mellitus Respiratory system controls will attempt to raise the pH by increasing respiratory rate and depth Depth and Rate of Breathing: Reflexes Depth and Rate of Breathing Other Reflexes Pulmonary irritant reflexes – irritants promote reflexive constriction of air passages Inflation reflex (Hering-Breuer) – stretch receptors in the lungs are stimulated by lung inflation Upon inflation, inhibitory signals are sent to the medullary inspiration center to end inhalation and allow expiration Respiratory Adjustments High Altitude Quick movement to high altitude (above 8000 ft) can cause symptoms of acute mountain sickness – headache, shortness of breath, nausea, and dizziness A more severe illness is high-altitude pulmonary edema caused by high pulmonary arterial pressure from constriction of pulmonary arteries (perfusion) in response to low PO2 High pressure causes bleeding into alveoli, cough up pink foam High-altitude cerebral edema – increased cerebral blood flow and permeability when hypoxic Increase BP in brain may lead to death Respiratory Adjustments: High Altitude Acclimation to hypoxia – respiratory and hematopoietic adjustments to altitude include: Increased ventilation – 2-3 L/min higher than at sea level Chemoreceptors become more responsive to PCO2 Substantial decline in PO2 stimulates peripheral chemoreceptors Kidneys accelerate production of erythropoietin (slower response ~4 days)