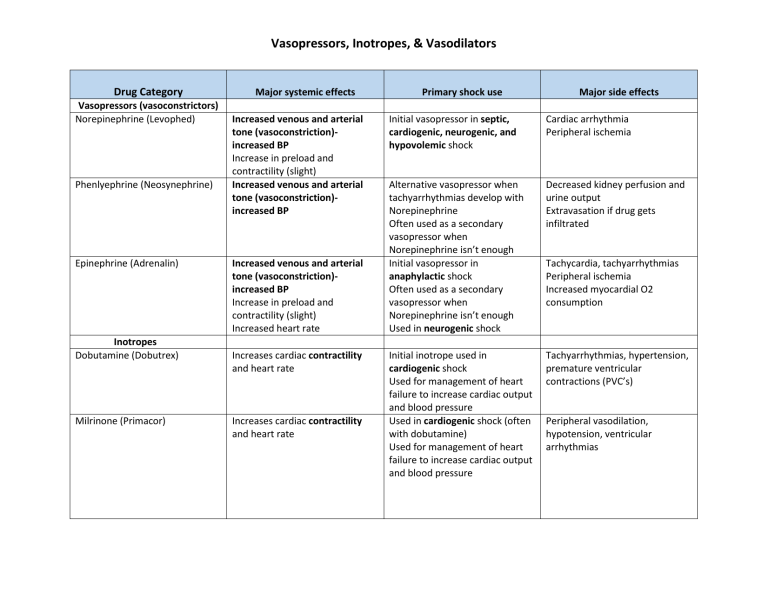
Vasopressors, Inotropes, & Vasodilators Drug Category Vasopressors (vasoconstrictors) Norepinephrine (Levophed) Phenlyephrine (Neosynephrine) Epinephrine (Adrenalin) Inotropes Dobutamine (Dobutrex) Milrinone (Primacor) Major systemic effects Increased venous and arterial tone (vasoconstriction)increased BP Increase in preload and contractility (slight) Increased venous and arterial tone (vasoconstriction)increased BP Increased venous and arterial tone (vasoconstriction)increased BP Increase in preload and contractility (slight) Increased heart rate Increases cardiac contractility and heart rate Increases cardiac contractility and heart rate Primary shock use Major side effects Initial vasopressor in septic, cardiogenic, neurogenic, and hypovolemic shock Cardiac arrhythmia Peripheral ischemia Alternative vasopressor when tachyarrhythmias develop with Norepinephrine Often used as a secondary vasopressor when Norepinephrine isn’t enough Initial vasopressor in anaphylactic shock Often used as a secondary vasopressor when Norepinephrine isn’t enough Used in neurogenic shock Decreased kidney perfusion and urine output Extravasation if drug gets infiltrated Initial inotrope used in cardiogenic shock Used for management of heart failure to increase cardiac output and blood pressure Used in cardiogenic shock (often with dobutamine) Used for management of heart failure to increase cardiac output and blood pressure Tachyarrhythmias, hypertension, premature ventricular contractions (PVC’s) Tachycardia, tachyarrhythmias Peripheral ischemia Increased myocardial O2 consumption Peripheral vasodilation, hypotension, ventricular arrhythmias Vasopressors, Inotropes, & Vasodilators Vasodilators Nitroprusside Nitroglycerin Improve myocardial perfusion by vasodilation of coronary arteries From a hemodynamic perspective, the net result is a decrease in systemic vascular resistance (afterload), ventricular filling pressures, and systemic blood pressure with an increase in cardiac output Relaxation of smooth muscle within blood vessels, resulting in vasodilation Used with inotropes in cardiogenic shock Hypotension, cyanide toxicity Increased intracranial pressure (ICP): related to cerebral vasodilation. *Use with caution with other vasodilators Used with inotropes in cardiogenic shock Dizziness, weakness, palpitations, vertigo, headaches, nausea, vomiting, diaphoresis, syncope *Use with caution with other vasodilators Dose-dependent drug that acts as a peripheral vasostimulant used to treat hypotension, bradycardia, and cardiac arrest 0.5 to 2 mcg/kg/min: act on the visceral vasculature to produce vasodilation, including the kidneys, resulting in increased urinary flow. 2 to 10 mcg/kg/min: stimulate myocardial contractility and increase electrical conductivity in the heart leading to increased cardiac output. >10mcg/kg/min: vasoconstriction and increased blood pressure via the adrenergic receptors alpha-1, beta-1, and beta-2 Tachycardia, dysthymias Peripheral ischemia at doses greater than 10mcg/kg/min Other Dopamine Vasopressors, Inotropes, & Vasodilators