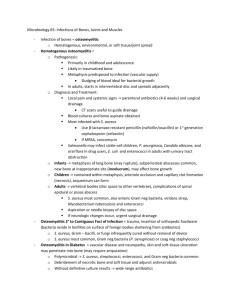
Osteomyelitis Name: Saif Omar Kitaz Reg NO: 2021NS01 Subject: PAP Introduction Osteomyelitis is a condition in which a bacterial infection causes inflammation of the bone. It can affect people of any age and both sexes, and while it can affect any bone, it most often affects the arms, legs, spine, and pelvis. The condition can be acute or chronic, and if left untreated, it can result in significant morbidity and mortality. Accurate diagnosis can be challenging, and successful treatment generally involves a combination of antibiotics and surgery. Definition Osteomyelitis is a bone infection, most times the infection spreads through the blood or can spread from the tissue near the bone. Moreover, this type of infection can start from the bone by trauma or open wound injury where the bone will be exposed directly to the bone. Causes of Osteomyelitis Bacterial infections of bones and joints are most often caused by S. aureus, which accounts for 50-80% of cases. The next most common pathogens are those responsible for respiratory infections. Group A streptococci are responsible for 5-10% of cases. H. influenzae type B infections tend to result in septic arthritis more than osteomyelitis. Immunization has all but Osteomyelitis eliminated H. influenzae osteomyelitis. S. pneumoniae infections now mostly affect healthy infants and young children, with only a small proportion causing bone or joint problems. Salmonella osteomyelitis is common in the tropics and in children with sickle cell disease. Newborns may have GBS, gram-negative bacteria, or Candida in their bones or joints due to exposure during birth. Tuberculous osteomyelitis may look like a tumor or Brodie abscess. Pathogenesis of osteomyelitis The special anatomical shape of the end of the long bones make a slope-like shape, which localizes the area for the bacteria. Following, in the metaphysis, nutrient arteries branch into the non-connecting (nonanastomosing) capillaries under the physis, which make a narrow loop before reaching the venous sinusoids to drain into the bone marrow. Following, low-velocity type blood flow in this space predisposing to bacterial invasion attack. Next, once the bacteria is set in a place, the phagocytes navigate to the zone and produce an inflammatory response resulting in an exudate which we call (metaphyseal abscess). Subsequently, the production of proteolytic enzymes, toxins, cytokines, and oxygen radicals at the end result in decreased oxygen tension, reduced pH, tissue destruction and osteolysis. Following, as the inflammation and exudates continue, the pressure increases and leads to spreading via the porous metaphyseal space through the haversian system and Volkmann canals into the subperiosteal space. As well as, the Purulence beneath the periosteum may lift the periosteal membrane of the bony surface, further disturbing the blood supply to the cortex and metaphysis. clinical manifestations of Osteomyelitis The symptoms of osteomyelitis, which can be subtle and unspecific, vary based on the age of the patient. Neonates may show signs of pseudoparalysis or discomfort when the affected limb is moved, and some may not develop a fever or show signs of being ill. In older infants and children, common symptoms include pain, fever, swelling, warmth, and redness in the affected area. Limping or refusal to walk is common in those who have osteomyelitis in the lower extremities. A significant sign of the disease is the focal tenderness over a long bone. Spread of Osteomyelitis the infection into the subperiosteal space beyond the metaphysis can cause inflammation in the surrounding soft tissues, leading to local swelling and redness. Pelvic osteomyelitis can have nonspecific symptoms such as pain in the hip, thigh, groin, or abdomen. Vertebral osteomyelitis typically presents as back pain, often with tenderness over the vertebral processes. Osteomyelitis most commonly affects long bones, including the femur and tibia, which account for almost 50% of all cases. The bones of the upper extremities are affected in 25% of cases, while flat bones are less frequently involved. Diagnosis of Osteomyelitis The diagnosis of osteomyelitis begins with clinical suspicion and requires appropriate imaging studies and cultures. It is recommended to perform blood cultures in all suspected cases. The optimal specimens for confirming the diagnosis and improving the yield compared to relying on blood culture alone are bone or subperiosteal abscess aspiration or biopsy. These specimens can be obtained by the interventional radiologist or the orthopedic surgeon during surgical drainage. Direct inoculation of clinical specimens into aerobic blood culture bottles can improve the chances of detecting K. kingae, particularly if held for a week. PCR is the most sensitive technique to detect K. kingae, even if antibiotics have been initiated up to six days earlier.