Pediatric Osteomyelitis: Overview, Diagnosis & Treatment
advertisement
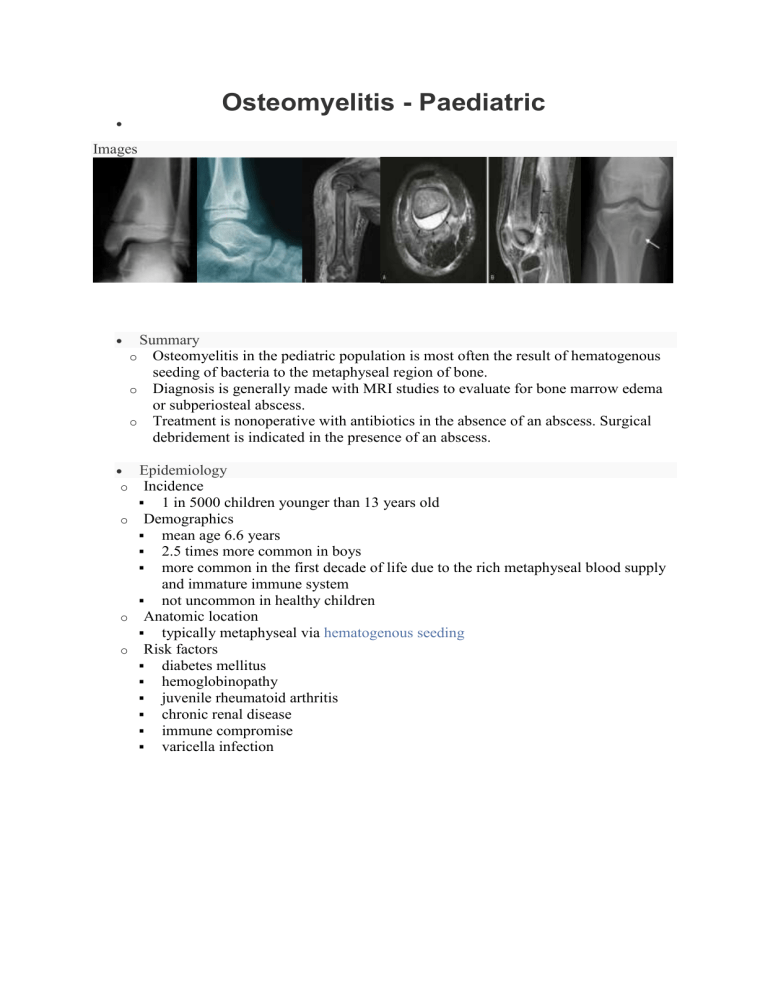
Osteomyelitis - Paediatric Images o Summary o Osteomyelitis in the pediatric population is most often the result of hematogenous seeding of bacteria to the metaphyseal region of bone. o Diagnosis is generally made with MRI studies to evaluate for bone marrow edema or subperiosteal abscess. o Treatment is nonoperative with antibiotics in the absence of an abscess. Surgical debridement is indicated in the presence of an abscess. Epidemiology Incidence 1 in 5000 children younger than 13 years old o Demographics mean age 6.6 years 2.5 times more common in boys more common in the first decade of life due to the rich metaphyseal blood supply and immature immune system not uncommon in healthy children o Anatomic location typically metaphyseal via hematogenous seeding o Risk factors diabetes mellitus hemoglobinopathy juvenile rheumatoid arthritis chronic renal disease immune compromise varicella infection Etiology o Pathophysiology mechanism local trauma and bacteremia lead to increased susceptibility to bacterial seeding of the metaphysis history of trauma is reported in 30% of patients microbiology Staph aureus is the most common organism in all children strains of community-acquired (CA) MRSA have genes encoding for Panton-Valentine leukocidin (PVL) cytotoxin PVL-positive strains are more associated with complex infections, multifocal infections, prolonged fever, abscess, DVT, and sepsis MRSA is associated with increased risk of DVT and septic emboli Group B Strep is most common organism in neonates Kingella kingae becoming more common in younger age groups Pseudomonas is associated with direct puncture wounds to the foot H. influenza has become much less common with the advent of the Haemophilus influenza vaccine Mycobacteria tuberculosis children are more likely to have extrapulmonary involvement biopsy with stains and culture for acid-fast bacilli is diagnostic Salmonella more common in sickle cell patients Pathoanatomy acute osteomyelitis most cases are hematogenous initial bacteremia may occur from a skin lesion, infection, or even trauma from tooth brushing microscopic activity sluggish blood flow in metaphyseal capillaries due to sharp turns results in venous sinusoids which give bacteria time to lodge in this region the low pH and low oxygen tension around the growth plate assist in the bacterial growth infection occurs after the local bone defenses have been overwhelmed by bacteria spread through bone occurs via Haversian and Volkmann canal systems purulence develops in conjunction with osteoblast necrosis, osteoclast activation, the release of inflammatory mediators, and blood vessel thrombosis macroscopic activity a subperiosteal abscess develops when the purulence breaks through the metaphyseal cortex septic arthritis develops when the purulence breaks through an intra-articular metaphyseal cortex (hip, shoulder, elbow, and ankle) (NOT KNEE) Infants <1 year of age can have infection spread across the growth plate via capillaries causing osteomyelitis in the epiphysis and septic arthritis chronic osteomyelitis periosteal elevation deprives the underlying cortical bone of blood supply leading to necrotic bone (sequestrum) sequestrum the necrotic bone which has become walled off from its blood supply and can present as a nidus for chronic osteomyelitis an outer layer of new bone is formed by the periosteum (involucrum) involucrum a layer of new bone growth outside existing bone seen in osteomyelitis chronic abscesses may become surrounded by sclerotic bone and fibrous tissue leading to a Brodie's abscess Anatomy o Blood supply the metaphyseal blood capillaries undergo sharp turns prior to entering venous sinusoids leading to turbulent flow and predisposition of bacterial deposition Classification o Acute osteomyelitis see pathoanatomy above o Subacute osteomyelitis uncommon infection with bone pain and radiographic changes without systemic symptoms increased host resistance, decreased organism virulence, and/or prior antibiotic exposure radiographic classification types IA and IB show lucency type II is a metaphyseal lesion with cortical bone loss type III is a diaphyseal lesion type IV shows onion skinning type V is an epiphyseal lesion type VI is a spinal lesion o Chronic osteomyelitis see pathoanatomy above