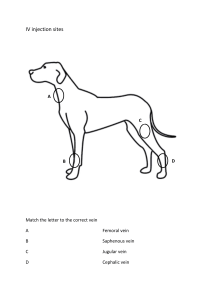
IV Initiation and Care Algonquin College 2021 Purpose By starting a peripheral IV you are gaining access to the peripheral circulation of a patient which will enable you to sample blood as well as infuse fluids and IV medications. The aim of intravenous management is safe, effective delivery of treatment without discomfort or tissue damage and without compromising venous access. Indication Fluid and electrolyte replacement Administration of medication Administration of blood/blood products Administration of Total Parenteral Nutrition Hemodynamic monitoring Therapy regime short duration (generally <6 days) Vascular access is one of the most common invasive procedures performed by health care professional world wide; therefore competence and dexterity are essential to safe patient care. Equipment Basic equipment includes Non sterile gloves Universal precautions IV cannula: appropriate size according to age and purpose Adults 20G – 22G Older adults 24G Blood products and CT contrast 18G – 20G Trauma and rapid transfusion 16G – 18G Extension (if not included) Non-latex tourniquet Tape Transparent dressing to secure site 2x2 gauze Alcohol or chlorohexidine swabs Saline flush Sharps bin Prior to Insertion Check and verify physician’s order Review patient’s history for allergies Gather equipment Hand hygiene Explain procedure to patient Verify patient with ID Provide privacy Adjust height of bed for working comfort of the nurse Ensure good lighting Verify if no stick arm Assess veins on non-dominant arm if possible Quick Quiz! (1 of 2) Which vaccination is recommended for health care providers to reduce the risk of disease from exposure to bloodborne pathogens? A. Hepatitis B B. Influenza C. Pertussis D. Tetanus Copyright © 2020, Elsevier Inc. All rights reserved. . Quick Quiz! (2 of 2) Answer: A. Hepatitis B Rationale: Hepatitis B is transmitted through direct and indirect contact with blood- and serum-derived fluids. Pertussis has a respiratory transmission through droplets. Tetanus typically enters the body through a wound contaminated with soil or feces, and influenza has a respiratory transmission. This is why we do Universal Precautions with everyone! 7 Copyright © 2020, Elsevier Inc. All rights reserved. Person Centred Care Communication Concerns and expectations Correct patient, correct procedure checks Verify orders Confirm name/DOB/MRN with patient and ID Comfort Alleviating anxiety and fear Techniques to minimize discomfort Education All aspects of IV therapy, goals of therapy, and self-care practices . . Assessing Veins Healthy Vein Avoid These Veins Bouncy Bruised Soft Thrombosed/sclerosed/Fibrosed Thin/frail Near bony prominences Above previous site Visible Inflamed/phlebitis Straight Multiple previous punctures Easily palpable Avoid extremity affected by stroke Collaborate with patient to choose best location (ex/ non-dominant hand/activity needs) DO NOT insert on side of mastectomy or renal AVF/AVG Need a physician order for pedal starts Avoid in patients with DM VeinsThe most commonly used veins include the median cubital, cephalic, and basilic veins in the antecubital area. You may also use veins in the hand if necessary. What Veins to Choose: Hands Dorsal digital veins flow along the lateral portions of the fingers. If large enough they may accommodate a small gauge needle, however they are used as a last resort. Metacarpal veins are formed by the union of the digital veins. They are usually visible, lie flat on the hand, are easy to feel, and are easily accessible. The hand provides a flat surface for stabilization and as this vein is in the extremity it allows successive venipunctures to be performed above the site. These veins may therefore be the first choice for venipuncture and can often accommodate 20 to 24 gauge catheters. Hignell, P. (2018). What Veins to Choose: Forearm Basilic vein originates in the dorsal venous network of the hand, ascending the ulnar aspect of the forearm. It is large and usually prominent that may be visualized by flexing the elbow and bending the arm upward. The vein will accommodate a large needle (usually up to a 16 gauge). It is often ignored as it tends to “roll” during insertion, therefore needs to be stabilized well during venipuncture. Cephalic vein flows upward along the radial aspect of the forearm. Its size readily accommodates a large needle (often up to 16 gauge), while its position provides easy access and natural splinting. This vein can be accessed from the wrist to the upper arm (using the most distal region of the vein first). These veins tend to “roll” so “anchoring” the vein during venipuncture essential. The large size is an excellent choice for infusing irritants. However, because the fadial nerve is close to this vein, perform venipuncture 10 to 13 cm above the wrist. Median (antibrachial) vein may be difficult to palpate and the location and size of this vein varies. It is usually spotted on the ulnar side of the inner forearm. It is easily accommodates 20 to 24 gauge IV catheters, just be sure to stay well clear of the inner wrist area as it may be more painful and there is a risk of nerve damage. Hignell, P. (2018). What Veins to Choose: Antecubital Accessory cephalic vein ascends the arm and joins the cephalic vein below the elbow. Its large size accommodates a large needle (usually up to an 18 gauge). Be cautious not to place the IV catheter tip in the bend of the arm. Median cubital vein lies in the antecubital fossa and is used mostly for emergency, short term access or blood withdrawal. It should be used only as a last resort for routine IV therapy due to the high rate of complications, such as infiltration, associated nerve injuries, and phlebitis. Accidental arterial puncture is a concern in this area. A catheter in this site also limits mobility. Hignell, P. (2018). Can you name the veins? Using a Vein Locator Procedure Prep equipment Attach syringe and flush extension set Tighten luer lock Flush/prime IV tubing set Open dressing Open angiocath as per product instructions Maintain sterility Preparing the Site Apply a tourniquet 4-6 inches above site. Assess the patient's veins in the upper extremity and identify potential sites that are easily seen or palpated. Check for a pulse distal to the tourniquet location; release the tourniquet and reapply it if necessary. Lightly palpate the vein with the index and middle fingers of your non-dominant hand. Stretch the skin to anchor the vein. If it feels hard or ropelike, select another. If the vein is easily palpable but not sufficiently dilated, place the extremity in a dependent position for several seconds or lightly stroke the vessel. Apply dry heat if necessary. (Glove filled with hot water or paper towel moistened with hot water) Release the tourniquet for site preparation. Encourage Venous Filling Correctly apply tourniquet At least 4 inches/10 centimeters above intended site Lowering arm below heart level prior to tourniquet application to encourage capillary filling Have patient open and close their hand several times (hand should be relaxed during venipuncture) Venous distension may take longer in elderly or dehydrated patients If needed, use a warm compress for 10 to 15 minutes prior to venipuncture for vasodilation Cleaning the Site If the intended insertion site is visibly soiled, clean it with soap and water before applying the antiseptic solution Clip hair around the insertion site, if needed, with single-patient-use scissors (DO NOT shave) to facilitate dressing application after IV insertion Clean the intended insertion site and surrounding skin with chlorhexidine or alcohol swab using a circular scrubbing motion working your way outward for at least 15 seconds to remove flora that would otherwise be introduced into the vascular system with the venipuncture Allow the antiseptic to dry completely for 30 seconds (it continues to clean the surface, as well as preventing skin trauma due to covering a moist area) To prevent adhesive trauma, use a sterile skin barrier product after cleansing solution has dried If you must palpate the intended insertion site after cleaning, remove and discard your gloves, perform hand hygiene, and put on sterile gloves to avoid contaminating the insertion site. Infection Control Phlebitis and Catheter Related Bloodstream Infections are a preventable nosocomial infections and adverse events. These infections increase hospital length of stay and facility costs. General Measures to Reduce IV-Related Infections Use of strict aseptic technique Tourniquets and all insertion equipment are to be single patient use (i.e. IV Start Pack) Careful skin preparation Careful site management Examine equipment for integrity and expiry date Proper aseptic technique with flushes Assess IV site as per protocol (some facilities state Q1hr to 2hrs assessment) The use of “IV baskets/trays” is strongly discouraged as the potential for crosscontamination between patients is greatly increased. Single patient use IV start packs should be used whenever possible. Hignell, P. (2018). Accessing the Vein Tell the patient that you're about to insert the device Re-apply tourniquet Rotate the catheter 360 degrees to release the catheter from the stylet as they are heat sealed during the manufacturing process. Press the vein lightly to check for rebound elasticity and to get a sense of its depth and resilience. Palpate the portion where the cannula tip will rest, not the point where you intend to insert the cannula. Note: If you touch the insertion site after cleansing, you will need to re-clean the site and let it dry completely before proceeding. DO NOT remove fingertips from gloves for IV insertion. Immobilize the vein by pressing 1" to 2" below the site with your thumb and drawing the skin taut. Stabilizing the Vein Superficial veins have a tendency to roll because they lie in loose, superficial connective tissue. To prevent rolling, maintain vein in a taut, distended, stable position. Hand Vein - Grasp the patient’s hand with your non-dominant hand. Place your fingers under his palm and fingers, with your thumb on top of his fingers below the knuckles. Pull his hand downward to flex his wrist, creating an arch Use your thumb to stretch the skin down over the knuckles to stabilize the vein. Forearm Vein - Encircle the patient’s arm with your non-dominant hand and use your thumb to pull downward on the skin below the venipuncture site. If the skin is particularly loose, the vein may need to be held taut downward below the vein and to the side of the intended site. Inserting the Device Place the bevel up of the needle at a 10- to 15-degree angle Puncture the skin and anterior vein wall (bevel should not appear, and some describe a “popping” sensation with access) Watch for blood to appear in the flashback chamber, then lower angle to parallel with skin Encourage patient to relax and breath slowly in and out As you continue to hold the skin taut, use the device's push-off tab to separate the catheter from the needle stylet, advancing the catheter Advance the catheter into the vein, watch for 2nd flashback in catheter until hub to skin Apply pressure on vein beyond catheter tip with finger of non-dominant hand to reduce blood leakage Remove stylet by pressing button for retraction of sharps Extension Tubing Release the tourniquet Place 2x2 under the catheter hub Attach the saline flushed extension tubing Make sure connection tight Flush the catheter Observe for swelling, leaking, discomfort Common Problems with IV Insertion Problem Possible Causes Corrective Action Approaching a palpable vein that is only visible for a short segment Patient anatomy • Missed Vein Vein rolled or moved with inadequate “anchoring” allowing stylet to push the vein aside • Anchor vein, maintain traction and reposition catheter slightly • DO NOT excessively probe the area and NEVER RESINSERT STYLET BACK INTO CATHETER (can shear off a piece of the plastic). Hematoma develops with insertion • Failure to lower the angle after entering the vein (trauma to the posterior vein wall) • Angle too great • Used too much force during insertion • Failure to release the tourniquet promptly when the vein is sufficiently cannulated (increased intravascular pressure) • Wrong angle • Lower angle after entering skin • Stopping too soon after insertion (so only the stylet, not the plastic catheter, enters the lumen, blood return disappears when you remove the stylet because the catheter is not in the lumen). – • Heat seal on catheter not released prior to use • Pull catheter back slightly Cannot advance the catheter off the stylet Insert the cannula 1 – 2 cm distal to the visible segment and tunnel the cannula through the tissue to enter the vein • Decrease angle with insertion • Use a smoother approach (to avoid piercing posterior wall) • Release tourniquet once catheter has been “threaded” • Ensure angle is reduced once stylet is in the vein and advance slightly to ensure catheter is in the vein • Rotate catheter 360 degrees on needle and re-seat before insertion Hignell, P. (2018). Dressing Apply a transparent semipermeable dressing the insertion site. Curl the extension set to the side and tape it to the patient's arm Do not place tape over clear dressing window Label the dressing with the current date and time, gauge size, and initials Consider tubular netting for pediatrics to help secure catheter Must pull back netting every 2 hours for site assessment Avoid circumferential taping Tegaderm IV Advanced Dressing • Innovative adhesives hold strongly and release easily. • Waterproof film coating • Resists soil and provides a barrier to external contamination • Deep notch, assists in securement • Transparent for continuous monitoring Finishing Up Return the bed to the lowest level to prevent falls and maintain patient safety Discard used supplies in appropriate receptacles Remove and discard your gloves Perform hand hygiene Document the procedure Paresthesia During Start If the patient reports symptoms of paresthesia while inserting the IV, such as radiating electrical pain, tingling, burning, prickly feeling, or numbness, immediately stop the insertion procedure and carefully remove the catheter. Also stop the procedure upon the patient's request or when the patient's actions indicate severe pain. Notify the practitioner of the patient's report of symptoms because early recognition of nerve damage produces a better prognosis. Document the details of the patient's report of symptoms in the medical record Documentation Date and time Site/location Size of cannula Dressing Patient tolerance/concerns Electronic Document •“ add LDA” • • • Peripheral Add new Any old sites that have not been discontinued will appear IV Site Care: Check Your Policy Flush IV Q12hr for patency Change dressing if soiled Some hospitals are mandating checking and documenting site every 1 to 2 hours Instruct the patient and family to obtain assistance from nursing staff whenever there is a real or perceived need to connect or disconnect devices or infusions Advise the patient to avoid getting the IV dressing and site wet during bathing and hand washing Instruct patients to use hand sani-wipes if IV is located in their hand Change out site per protocol Usually Q72 to 96hr Pediatric Considerations Consider performing venipuncture in a neutral space to allow the child’s room to be a safe place. In addition to the usual venipuncture sites, the four scalp veins and the dorsum of the foot may be used in infants. Needle selection is based on vein assessment and potential use. A typical gauge for PVAD is 26- to 24-gauge for neonates, 24- to 22-gauge for children. Use local anaesthetics and distraction strategies to minimize distress associated with venipuncture. Apply latex-free tubing or rubber band or use a blood pressure cuff inflated to just below diastolic blood pressure. Allow older children to select IV site to increase cooperation, so they believe that they have some control over their treatment. To increase success rate and improve safety for PVAD insertion, have assistance to support and position the child. Use therapeutic holding, usually in a sitting position, to provide close contact and decrease movement that may result in unsuccessful initiation or dislodgement. Consider the use of securement devices to aid in preventing dislodging PVAD during daily activities and play. Choose age-appropriate activities compatible with maintenance of the IV infusion to maintain normal growth and development. Considerations for the Older Adult • Consider that older persons may have fragile veins and skin. Older persons have less subcutaneous support tissue, and their skin is thinning. Consider the use of barrier film before dressing application to protect fragile skin • Avoid sites that are easily moved or bumped (e.g., the hand) and areas that may affect mobility and independence. • Use a commercial protective device to protect the site and reduce manipulation. • Appropriate gauge selection is a key factor for successful insertion and maintaining access (e.g. 22- or 24-gauge catheter). Smaller-gauge catheters are less traumatizing to the vein and will allow better blood flow, increasing hemodilution of infusates. • If possible, avoid the back of the older person’s hand or the dominant arm for venipuncture because use of these sites interferes with the individual’s independence. • If possible, do not use a tourniquet to avoid rupturing vein during initiation. IV Daily Assessment At least every 4 hours Patients who are receiving non-irritant/ nonvesicant infusions and who are alert and oriented and who are able to notify the nurse of any signs of problems such as pain, swelling, or redness at the site. More frequently: every 5 to 10 minutes Patients receiving intermittent infusions of vesicants (NOTE: The nurse should advocate for central vascular access administration of vesicant medications whenever possible. The peripheral infusion of vesicant agents should be limited to less than 30 to 60 minutes. In addition to visual assessment of the site, a blood return should be verified every 5 to 10 minutes during the infusion.) Patients receiving infusions of vasoconstrictor agents. (NOTE: The nurse should advocate for central vascular access administration of vasoconstrictor agents whenever possible as these agents can cause severe tissue necrosis with extravasation.) At least every 1 to 2 hours Critically ill patients Adult patients who have cognitive/ sensory deficits or who are receiving sedative-type medications and are unable to notify the nurse of any symptoms PIVs placed in a high-risk location (e.g. external jugular, area of flexion) At least every hour Neonatal patients Pediatric patients NSL Qshift Hignell, P. (2018). Delegation and Collaboration The skill of inserting a short-peripheral IV access device cannot be delegated to unregulated care providers (UCP). The nurse instructs UCP to: Notify the nurse if the patient complains of any IV site–related complications such as redness, pain, tenderness, swelling, bleeding, drainage, or leaking from under dressing. Inform nurse if IV becomes wet. Inform nurse if solution of fluid in IV bag is low or electronic infusion device (EID) alarm is sounding. Copyright © 2020, Elsevier Inc. All rights reserved. . Complications Infiltration Infusion fluid leaks into surrounding tissue Tip of catheter slips out of vein or Blood vessel wall allows fluid to leak Phlebitis Inflammation of the vein Patient may complain of pain and tenderness along vein May notice redness, or red streak along vein and warmth to touch Thrombophlebitis Inflammation of the vein that results in blood clots Extravasation (chemical damage) Accidental infiltration of a vesicant or chemotherapeutic drug into surrounding tissue Vesicants cause tissue damage, ischemia and necrosis Infection IV cannula is direct access to a patient’s vascular system and provided a potential port of entry for microorganisms Phlebitis: Causes The most frequent and under-reported complication of PIV infusion is phlebitis, which may occur at rates as high as 50% or even as high as 75% in patients with infectious diseases Chemical- infusion chemically erodes internal layers of the vein wall; can happen when skin not allowed to dry after cleaning Mechanical- irritation to internal lumen of vein during insertion; movement of the cannula due to placement; catheter too large Bacterial- introduction of bacteria into the vein Images of Complications Extravasation Stop medication and seek further treatment options and orders from physician Do not remove IV until instructed to do so MD may aspirate content Some antidotes are given through same line Don't apply pressure to the area. Elevate the patient's extremity Mark the affected area to document progression Have extravasation kit at beside Incident report Common meds include: chemo agents, phenytoin, calcium chloride and gluconate, acyclovir, digoxin, diazepam, potassium, cefotaxime, IV contrast, mannitol Norepinephrine extravasation Embolism occurs when a substance (usually a blood clot) becomes free and circulates to the pulmonary artery causing occlusion. Even small recurrent emboli may cause pulmonary hypertension and right heart failure Air embolism is the presence of air in the vascular system caused by improperly primed IV lines, failure to occlude needle hub or accidental disconnect, or inadvertent infusion of air Risk Factors: Irrigation of a clogged IV Use of veins in lower limbs (increased risk) Debris in IV solution Debris caused by incompletely dissolved, reconstituted drugs Unfiltered blood or plasma Prevention: NEVER irrigate the catheter if the IV is not flowing. Do not force NS flush if resistance met Use in-line filters where applicable Avoid siting IV’s in the lower extremities in adult patients when possible Thoroughly inspect medication and solution containers for particulate matter prior to use Remove all air from lines and syringes Ensure tight connections PE S&S and Treatment S&S Treament Place patient on strict bed rest in semiFowler’s position Check lines for air and close all clamps Cyanosis Notify physician immediately Cough, unexplained Monitor vital signs hemoptysis Administer Oxygen Diaphoresis Tachycardia Assess IV and re-site if needed (for emergency drugs) Low-grade fever Chest pain radiating to neck and shoulders Document in permanent health record Apprehension Pleuritic discomfort Dyspnea, tachypnea Quick Quiz! (1 of 2) When receiving report at change of shift, the nurse is told that the patient’s IV infiltrated earlier in the day and the patient is at grade 2 on the phlebitis scale. What symptoms should the nurse expect to see when assessing this patient’s infiltrated IV site? (Select all that apply.) A. Purulent drainage B. Edema C. Erythema D. Streak formation Copyright © 2020, Elsevier Inc. All rights reserved. . Quick Quiz! (2 of 2) Answer: B. Edema C. Erythema Rationale: Purulent drainage is associated with a grade 4 phlebitis, and streak formation is associated with a grade 3 phlebitis. Copyright © 2020, Elsevier Inc. All rights reserved. . References Arias-Fernandez, L., Suerez-Mier, B., Marinez-Ortega, M., & Lana, A. (2017). Incidence and risk factors of phlebitis associated to peripheral intervenous catheters [figure]. Google Images. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S2445147916300091 British Columbia Institute of Technology (n.d). NSL assessment [Digital image]. Google Images. Retrieved from https://opentextbc.ca/clinicalskills/chapter/8-2-types-of-iv-therapy/ Perry, A., Potter, P., Ostendorf, W., & Cobbett, S. (2019). Canadian clinical nursing skills and techniques (1st ed.). Mosby Canada. Dalmua-Pastor, M. (2021). Anterior view of vein [Digital image]. Google Images. Retrieved from https://www.researchgate.net/figure/Anterior-view-of-the-cubital-fossa-showing-the-super-fi-cial-veinsSurface_fig22_278696184 a- Halozyme (n.d.) Intravenous access: When things go wrong [Digital Image]. Pinterest. Retrieved from https://www.pinterest.ca/pin/497366352580193530/ Graduate Medical Education (2017). Peripheral iv starts super starters [PowerPoint slides]. Retrieved from https://gme.conemaugh.org Rajathurai Jeya, M.S. (n.d). Peripheral intra venous cannula insertion (PowerPoint slides]. Retrieved from https://www.slideshare.net/jeya81/iv-cannula-insertion Raymond, K. (n.d). Intravenous (iv) line access [Image]. Google Images. Retrieved from https://iem- student.org/intravenous-ivline-access/