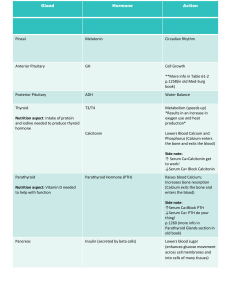
Hypercalcemia Heidi Chamberlain Shea, MD Endocrine Associates of Dallas Goals of Discussion Review Calcium metabolism Differential Diagnosis of Hypercalcemia Treatment options Calcium case presentations Calcium Physiology An essential intracellular and extracellular cation Extracellular calcium is required to maintain normal biological function of nervous system, the musculoskeletal system, and blood coagulation Intracellular calcium is needed for normal activity of many enzymes Preservation of the integrity of cellular membrane Regulation of endocrine and exocrine secretory activities Activation of compliment system Bone metabolism Role of Calcium Bone mineralization Muscle contraction Skeletal Cardiac Smooth muscle Blood clotting Nerve impulse transmission Bone metabolism Parathyroid hormone (PTH) Calcium Phosphorus Vitamin D Calcitonin Calcium 41% combined with plasma proteins 9% combined with anionic substances Not diffusible One gram per deciliter of albumin binds approximately 0.8 mg/dl of calcium Citrate and phosphate Not ionized Diffusible 50% is diffusible and ionized Most important in bodily functions Effects of Calcium Hypocalcemia Increased neuronal membrane permeability to sodium ions facilitates action potentials When calcium levels < 6mg/dl Tetany Chvostek’s sign Trousseau’s sign Calcium <4mg/dl = Death Effects of Hypercalcemia Calcium >12 mg/dl Nervous system depressed Fatigue Depression Constipation Anorexia Polyuria Most common nocturia Parathyroid poisoning Calcium > 17mg/dl Calcium phosphate crystals precipitate Findings with Hypercalcemia Bony tenderness Hyperactive tendon reflexes Tongue fasciculations Hypercalcemia in pregnancy May cause hypocalcemia in the neonate Suppressing the fetal parathyroid Hypercalcemia Small decrease in GFR Hemodynamic effects & hyposthenuria (a loss of renal concentrating abilities) Findings with Hypercalcemia Band Keratopathy Deposition of Calcium Corneal opacities Long standing hypercalcemia Associated with primary hyperparathyroidism Calcium deposition begins near the limbus at the 3 & 9 o’clock position Less friction from the lids near the limbus Tear film is most alkaline in the most exposed area, band running across the cornea from the 3 to 9 o’clock position Complications of Hypercalcemia Sinus bradycardia Increase in the degree of a heart block Cardiac arrhythmia Hypertension Pancreatitis Peptic ulcer disease Nephrolithiasis Accelerated vascular calcification Calcium Homeostasis Hormones PTH Vitamin D Calcitonin Organs Bone Kidney Small intestine 1,25-OH Vitamin D Calcium Physiology Target Organs Small intestine : Kidney : approx. 40% absorbed, 50% of that excreted into bile and other intestinal secretions. So only 20% of the total amount of Ca ingested daily is available to circulate between bone and extracellular fluid. Glomerulus filters out the Ca that is not bound to protein. Proximal tubule - approx. 50% to 70% is reabsorbed, Ca reabsorption mirrors Na reabsorption. Ascending limb of the loop of henle - approx. 30% to 40% reabsorbed Distal nephron - about 10% reabsorbed. PTH and activated Vit D increases Ca absorption during Ca deficient states. Normally kidney excretes approx. 200 mg /day of Ca to maintain homeostasis. During states of severe Ca depletion, the Kidney can decrease urinary excretion to 50mg /day or less. CALCIUM REGULATION PTH _ + _ + 1,25(OH)2 D3 + + GI Tract + CALCITONIN _ ECF Pool of Calcium URINE BONE Parathyroid Four glands located behind the thyroid Length 6 millimeters Width 3 millimeters Thickness 2 millimeters Often accidentally removed Normal function with at least 2 glands Parathyroid Composed Chief cells Oxyphil cells Synthesize, secrete and store PTH ? function Responsible for calcium homeostasis Kidney Bone Parathyroid Actions Increases calcium Regulates intestinal absorption 25-OH vitamin D 1,25-OH vitamin D Renal absorption of calcium/excretion of phosphorus Bone reabsorption Osteolysis Parathyroid and Bone Osteoblasts + Osteocytes = Osteocytic membrane system Osteocytic pumps Pump calcium from bone to ECF To maintain calcium concentration in bone fluid, osteolysis occurs and calcium phosphate is resorbed from bone Fibrous and gel matrix remain intact Parathyroid and Bone PTH stimulates osteocytic pump Increases permeability of osteocytic membrane allowing calcium to diffuse Osteoblasts,cytes and clasts do not have PTH receptors PTH stimulates osteoblasts and cytes, which then activate osteoclasts via “signaling” system PTH indirectly stimulates formation of new osteoclasts Both cell lines are activated but clastic activity > blastic Calcitonin Secreted by Parafollicular (C cells) in the thyroid Temporarily lowers calcium levels Decreases osteoclastic activity Stimulated by high calcium levels Stimulating a distal tubular - mediated calciuresis Calcium Caveats Respiratory alkalosis and elevated pH Decrease in pH has the opposite effect. Increase in the binding of calcium Lowers ionized calcium. As a general rule a shift of 0.1 pH unit produces a change in ionized calcium of 0.04 to 0.05 mmol/L Chelators such as citrate may transiently decrease ionized calcium Blood transfussions Formulas for Correction 0.8 for each gm of Albumin 0.16mg/dl for each gm of globulin. FEca= (uCA x sCR)/(sCA x uCR) FEca <1% - Familial hypocalciuric hypercalcemia, FEca >2% - primary hyperparathyroidism in pH will protein bound Ca by 0.12mg/dl 80-90% of protein bound Ca is bound to Albumin. Increase in serum pH of 0.1 may cause decrease in ionized Ca of 0.16mg/dl Calcium : Protein bound - 40%; Complexed - 13%; Ionized fraction - 47% Etiology of Hypercalcemia Approx. 80% of all cases are caused by Malignancy or Primary Hyperpathyroidism V Vitamins I Immobilization T Thyrotoxicosis A Addison’s disease M Milk-alkali syndrome I Inflammatory disorders N Neoplastic related disease S Sarcoidosis T Thiazide, other drugs - Lithium R Rabdomyolysis A AIDS P Paget’s disease, Parental nutrition, Pheochromocytoma, Parathyroid disease HYPERCALCEMIA SERUM CALCIUM > 10.6 Determine wheather hypercalcemia is real, measure ionized Ca adjust for change in serum albumin level, careful drug hx Li, Vit D or A, Measure PTH PTH high Hyperparathroidism PTH - N or Low Malig- prim. or mets If cause remain unclear measure Vit D Vit high consider Sarcoidosis CXR Consider other *Hyperthyroidism *Milk-alkali syndrome *Familial hypocalciuric hypercalcemia Hyperparathyroidism Stones Bones Groans Moans Normal bone Hyperparathyroid Hyperparathyroidism PTH Calcium normal / Secondary / normal Tertiary Primary Intact PTH PTHrP 1,25 -D Ca++ Prim. HPT PTHrP malignency Non-PTHrP malig Hyperparathyroidism Surgical Management Serum calcium > 12mg/dl Hypercalciuria > 400mg/day Normal <200 mg/day Presence of signs and symptoms Nephrolithiasis Osteitis fibrosa Cystica Neuromuscular symptoms Markedly reduced cortical bone density Most common Long bones Decreased creatinine clearance Patient age < 50 years Markedly reduced cancellous bone density Spine Silverberg et al., JCEM:1996 Hyperparathyroidism Medical Management Alendronate therapy 37 patients >50% female 53 to 80 years Primary Hyperparathyroidism Cross over 24 months Alendronate 12 placebo and 12 treatment Khan et. al., JCEM 2004 Hyperparathyroidism Medical Management Khan et. al., JCEM 2004 Treatment for Hypercalemia Hydration Furosemide Bisphosphonate Calcitonin Mithramycin Gallium nitrate Steroids IV Phosphate Dialysis Others Treatment for Hypercalemia Hydration First step in the management of severe hypercalcemia. --isotonic saline Usually reduces - 1.6-2.4mg/dl Hydration alone rarely leads to normalization in severe hypercalcemia Rate of IV saline based on severity of hypercalcemia and tolerance of volume expansion Treatment for Hypercalemia Loop Diuretics Facilitate urinary excretion of calcium Inhibits calcium reabsorption in the thick ascending limb of the loop of Henle Guard against volume overload Volume expansion must precede the administration of furosemide Drug’s effect depends on delivery of calcium to the ascending limb. Needs frequent measurement of lytes and urine output Treatment for Hypercalemia Calcitonin Not as effective as bisphosphonate, tachyphylaxis quickly occurs and limits therapeutic efficacy Toxic effect limits it’s use, reserved for difficult cases of hypercalcemia that are related to malignancy Gallium Nitrate Need to infuse it over 5 days, nephrotoxity limits it’s use, not used frequently Corticosteroids Mithramycin For myeloma, lymphoma, Sarcoidosis, or vit D toxicity Decreases GI absorption 200-300mg hydrocortisone for up to 5 days Slow response limits it’s use Hemodialysis Zero or low calcium bath, In selected condition, eg-hypercalcemia complicated by renal failure Treatment for Hypercalemia Bisphosphonate Structurally related to pyrophosphate P-C-P bound is a back bone that renders them resistant to phosphates. They bind to hydroxyapatite in bone and inhibit the dissolution of crystals. Their great affinity for bone and their resistance to degradation account for their extremely long half life in bone. Treatment for Hypercalemia Bisphosphonate Poor GI absorption- <10% ETIDRONATE, PAMIDRONATE,CLODRONATE Etidronate- 7.5mg/kg iv over 4 hr for 3-7 days Serum calcium begins to decrease within 2 days after first dose Response better if patient is well hydrated Oral bisphosphonate to prevent recurrent hypercalcemia. Adverse effect-increase creatinine, phosphate Long term use-impair bone formation, osteomalacia Treatment for Hypercalemia Bisphosphonate Pamidronate Inhibits osteoclast function The most potent bisphosphonate 60mg to 90 mg IV over 24hr 70% to 100% of patients Adverse effect Decreased calcium within 24 hr of treatment 2/3rd of this group had normal calcium within 7 days Mild transient increase in temp(<2○ C), transient leukopenia, small reduction in phosphate level Excreted by kidney- dose adjustment Treatment for Hypercalemia Mithramycin An inhibitor of RNA synthesis in osteoclasts IV 25 microgram/kg over 4-6 hr Begins to decrease in 12hr, max in 48-72 hr Duration of normocalcemia ranges from a few days to several weeks Depending on the extent of ongoing bone resorption Adverse effect Nausea- Minimize with slow iv Avoid extravasation-cellulitis Hepatotoxic- in 20% patients Nephrotoxic- increase in creatinine, proteinuria Thrombocytopenia Contraindication-liver, kidney dysfunction, thrombocytopenia, or any coagulopathy Treatment for Hypercalemia Gallium Nitrate Inhibit bone resorption by adsorbing to and reducing the solubility of hydroxyapatite crystals Adverse effect- Nephrotoxity, hypophosphatemia, small reduction in hemoglobin concentration Clinical experience limited Treatment for Hypercalemia GLUCOCORTICOIDS Inhibits the growth of neoplastic lymphoid tissue, counteracting the effects of vitamin D PHOSPHATE Can lower calcium rapidly and profoundly, Restricted to patient with extreme, life threatening hypercalcemia Very dangerous Last resort Contraindications-Hyperphosphatemia and azotemia Treatment for Hypercalemia Choice of Agent Mild (<12mg/dl) Hydration with saline Lasix Saline + Calcitonin + mithramycin Alternatively bisphosphonate, Steroids if sensitive Hypercalcemia secondary to malignancy Moderate (12-14 mg/dl) with symptoms Severe life threatening (>14mg/dl) Bisphosphonate Survival after the appearance of hypercalcemia is very poor Median of 3 months. What Is The Diagnosis? 52 yr old African American female presents with broken hip Poor light exposure Fatigue Constipation Difficulty concentrating History of kidney stones What Is The Diagnosis? Calcium 13mg/dl (9-10.5) Phosphorus 2mg/dl (3-4.5) 25-OH vitamin D 33 ng/ml (20-40) PTH 90 pg/ml (10-80) Diagnosis: Primary Hyperparathyroidism What Is The Diagnosis? 10 day old infant presents to ER with seizures Calcium 5.5mg/dl (9-10.5) Ionized calcium 3 mg/dl (4-5.6) Phosphorus 10 mg/dl (3-4.5) • PTH 5 pg/ml (10-80) Diagnosis: Hypoparathyroidism What Is The Diagnosis? 18 month old African American male Presents with abnormal gait Low sunlight exposure Breast fed as infant with current poor dairy intake Calcium 8 mg/dl (9-10.5) Phosphorus 4mg/dl (3-4.5) • PTH 85 pg/dl (10-80) • 25-OH Vitamin D 10 ng/ml (20-40) Diagnosis Vitamin D deficiency with secondary hyperparathyroidism Tibial and femur bowing Treatment: Ergocalciferol and calcium