Hypercalcemia UCI Internal Medicine – Mini Lecture A diagnostic and treatment approach
advertisement

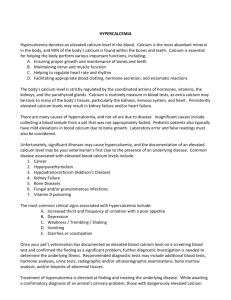
Hypercalcemia A diagnostic and treatment approach UCI Internal Medicine – Mini Lecture Hypercalcemia objectives • Identify true hypercalcemia • Understand basic calcium regulation • Understand the most common etiologies • Have a clear diagnostic and workup plan • Understand acute management Initial evaluation • A 68 year-old female with no PMH or home meds is brought to the ER by family with altered mental status, nausea, and diffuse bony pain. Initial Evaluation • VS unremarkable. A&Ox1, tries to get out of bed and is distracted. Rest of exam normal. Labs are normal except below: 10 139 111 3.8 20 12 1 104 1.4 1.8 Albumin= 1.0 Corrected Calcium = (0.8 * (Normal Albumin - Pt's Albumin)) + Serum Ca What is patient’s corrected calcium? Calcium regulation: • PTH= increases calcium – Release of bone Ca stores – Increase renal tubular Ca resorption – Increase production of activated Vit D by increased kidney hydroxylase • Vitamin D= increases calcium – Needs to be activated to active form (calcitriol) – Increases calcium absorption in gut • Calcitonin= decreases calcium – Slows down osteoclasts, decreases bone resorption – Increase renal calcium clearance Common causes of hypercalcemica • PTH mediated – Primary hyperparathyroidism • Non-PTH mediated – PTHrp, vitamin D intoxication, granulomatous disorders, osteolytic bone metastases, malignancy • Medications – Thiazide diuretics, lithium • Misc – Hyperthyroid, immobilization, Milk-alkali, etc… Treatment: Mild and Moderate • Mild (<12): No acute tx necessary – Avoid thiazides and lithium, volume depletion – Low calcium diet • Moderate (12-14): May or may not require tx – If mildly symptomatic (constipation), no immediate therapy needed – Treat if severely symptomatic (ie mental status changes) Treatment: Severe Hypercalcemia (>14) • Normal Saline (200cc/hr, adjust for UOP 100150cc/hr) • Calcitonin 4 IU/kg q6-12 hrs (if Ca>14) • Bisphosphonates (Reclast 4mg IV over 15 mins) • Especially for excessive bone resorption/malignancy • Dialysis if above measures fail Monitor with Q8 serum calcium levels Treat Underlying Cause • Multiple Myeloma • Squamous Cell Cancer • Gynecologic Cancer • Sarcoidosis • Tuberculosis • Thyrotoxicosis • Pituitary Adenoma • Multiple Endocrine Neoplasia Back to the case • Admitted to medicine • PTH 77 (normal 11-55) Tc99m-sestamibi demonstrated a single parathyroid adenoma • Referred to surgery for parathyroidectomy Hypercalcemia objectives • Identify true hypercalcemia • Understand basic calcium regulation • Understand the most common etiologies • Have a clear diagnostic and workup plan • Understand acute management Take home points • Remember to correct calcium based on albumin levels • Calcium regulation based on multiple factors including PTH, Vitamin D, Calcitonin • Primary hyperparathyroidism and malignancy are the most common causes Take home points • Check PTH first, if elevated likely primary hyperparathyroidism • If PTH not elevated, check vitamin D (both 25OH and 1,25-OH) • Treat all symptomatic patients with IVF – Calcitonin, bisphosphonates if warranted