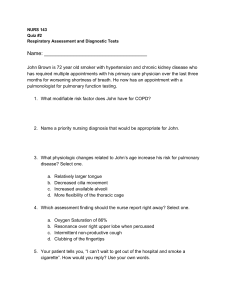
Final Exam Review Pt. 2 CHILD WITH SPECIAL NEEDS 9 questions Black = Lecture Notes Gray = Textbook Notes 1 Red = Fall 2021 Test Questions Orange = Spring 2021 Test Questions Blue = Spring 2021 Quiz Questions Purple = Final Spring 2021 Test Questions Green = Medications/Tx. to Know Family Centered Care o Family functioning, communication, therapeutic relationships, role of culture, shared decision making o Family is the child’s primary source of strength and support o Hospitalization alters the parental role; nurses should be role models and mentors for engaging parents in children’s hospital routines and daily care that benefits the Test Q: What child trend of care allows for a child Trends in Care: to develop social o Normalization: establishing a normal pattern of living skills, sense of Family life, delegation, routines, participation, age-appropriate activities self, etc. Test Q: A child has o Home Care: normalize, lessen family disruption, maximize G&D Mainstreaming established a promotes self-enabled routine when appropriate normal pattern of living with o Mainstreaming: process of integration of the child into the classroom or daycare with routines and agepeers appropriate Quiz Q: how would Develops sense of self, understand and respect themselves and peers, activities? mainstreaming gain acceptance, socialization skills Normalization benefit a child with o Early Intervention: PT, speech therapy, OT, IFSP Down’s Syndrome? Test Q: Parents with a o Managed Care: reduce barriers, quality, training of increased recently diagnosed openness families and communities special needs child are Assisting the Family with Feelings: asking question if the o Shock & Denial child will ever get better. What stage are they in? o Adjustment Shock & Denial o Reintegration & Acknowledgment o Support System Cognitive Impairment = Any Type of Intellectual Disability o Consists of 3 Components: IQ Adaptive Behavior – ability to plan, reason, solve problems, think abstractly, and be able to meet demands for culturally appropriate demands of life Test Q: Which < 18 years old at diagnosis cognitive impairment has genetic ties? Ex. Down’s Syndrome, Fragile X Syndrome Matching. o Etiology = social, familial, environmental, organic, and unknown causes Down’s Syndrome, Chromosomal disorders, prenatal toxin exposure, cerebral palsy, microcephaly, Fragile X infantile spasms o Primary Prevention: Avoid Prenatal Rubella Smoking or Alcohol Use Infection Reduce Head Injuries Genetic Counseling Future Gene Therapy Folic Acid (PKU) o Secondary Prevention: Early identification to avoid damages (hypothyroidism, PKU, galactosemia) o Tertiary Prevention: Treatment to minimize long-term consequences Final Exam Review Pt. 2 o Test Q: Which of the following are commonly associated with down’s syndrome? Otitis Media and Septal Defects 2 Development: Delayed Verbal Skills Socialization Promote Independence Sexuality Discipline Play & Exercise o Care of Child with CI: Detailed history with special focus on self-care abilities Questions about abilities, approach positively Assess developmental age Communication with child appropriate to cognitive level Address potential loneliness Developmental Disability = Any significant lag or delay in physical, cognitive, behavioral, emotional or social development Language & cognitive skill delays, fine & gross motor skills delay o Developmental Screening = Early Identification Down’s Syndrome (Trisomy 21) o Most Common Chromosome Abnormality AND Genetic Cause of CI o Risk Factors: (exact cause unknown) maternal age > 35 years old (80%) paternal age > 55 years old (< 5%) genetic predisposition (97%) o Manifestations: Separated Sagittal Excess Skin in Neck Sutures Folds Palpebral Fissures (slant Hyperflexible eyes) Hypotonia/Muscle Transverse Palmar Weakness Crease Hearing and Visual Small Nose/Flat Bridge, Losses Small Ears Hypotonicity Short Rib Cage, Large Protruding Tongue Wide Variations of IQ: mild moderate Initial development normal; strength in sociability Social development may be 2-3 years ahead of mental age Hypersensitive to Touch & Sound o Congenital Anomalies: Heart Defects – Septal Defects Congenital Heart Disease – AV CANAL! Hirschsprung Tracheoesophageal Fistula Otitis Media Altered Immune Function Test Q: Most common Musculoskeletal – Atlantoaxial Instability comorbidity associated Sexual Development/Growth with down’s syndrome o Comorbidities = CONGENNITAL HEART DISEASE is: o Treatment & Prognosis: congenital heart disease Atlantoaxial Instability: urgent if s/s of spinal compression Final Exam Review Pt. 2 Test Q: Which tests would be accurate in prenatal diagnosis of down’s syndrome? CVS, Amniocentesis, AlphaFetoprotein Test Q: Why is Fragile X most common in males? X-Linked Recessive, males have nonfunctioning X 3 Avoid activities stressful to head & neck May require surgical intervention Life Expectancy: majority live to be 60+ Remains lower than general population Help Family Prevent Physical Problems – positioning, feeding, attachment, URIs, ear infections, etc. o Prenatal Diagnosis + Genetic Counseling: Offer to pregnant women of advanced maternal age or with family history Chromosomal Villus Sampling Amniocentesis Alpha-Fetoprotein o Early Intervention: Address developmental delays and help child achieve full potential Test Q: What should the nurse Therapy, exercises, activities promote when Begin ASAP educating o Education: parents of a child Teach patients & caregiver importance of independence; ways to with down’s syndrome? improve child’s independence ways to Promote Optimal Development improve child’s Guidance for establishing acceptable social behavior, personal independence feelings of self-worth, esteem, and security Fragile X Syndrome o Most Common Inherited CI; 2nd Most Common Genetic Cause (after down’s) o Males = nonfunctioning X; Females = one functioning X, one nonfunctioning X o Etiology – X-linked Recessive; DNA Testing o o Classic Physical Appearance: Large Head Circumference, Long Face & Ears, Palpebral Fissures, Strabismus Palate (high-arched) Macroorchidism (enlarged gonads) Hyperflexible Finger Joints Palmar Crease Flat Feet Classic Behavioral Features: Mild Severe CI normal IQ with learning difficulties Delated Speech & Language Hyperactivity, Aggression Autistic-Like Behaviors Hearing Impairment o Slight Profound Slight Moderately Severe: residual hearing sufficient to process linguistic information; generally, with hearing aid slight (16-25 dbs.), mild to moderate (26-55 dbs.), moderate to severe (56-70 dbs.) Final Exam Review Pt. 2 Quiz Q: Why is a child’s risk of hearing loss higher if they were in the NICU for long periods of time? continuous humming noises from equipment 4 Severe Profound: precludes processing of linguistic information with or without hearing aid severe (71-90 dbs.), profound (>91 dbs.) o Etiology: family history, anatomic malformation, low birth weight, ototoxic drugs (gentamycin), chronic ear infections (OM), perinatal asphyxia or infection, prenatal substance abuse, cerebral palsy Sensorineural Hearing Loss in NICU babies with continuous equipment humming noises o Pathology: Conductive Hearing Loss: middle ear [OM, foreign bodies, medications, cerumen impaction] Sensorineural Hearing Loss: auditory nerve or inner ear Mixed Conductive-Sensorineural Loss: may follow recurrent OM with complications Central Auditory Interception: organic or functional o Therapeutic Interventions: Conductive Defects Medication/Antibiotics Test Q: What hearing defects are hearing aids Hearing Aids not beneficial for Sensorineural treatment? Hearing Aids NOT Beneficial Sensorineural Cochlear Implant o Assessment: Lack of Startle Reflex Absence of Babbling by 7 Months Final Q: What is General Indifference to Sounds indicative of hearing ID before 3 months; no later than 6 months loss in infants? Language & Educational Development, Hearing/Speech Development lack of startle reflex o Lip reading, sign language, picture books Parental Concerns: refer for hearing evaluation o LISTEN TO PARENTAL CONCERNS o Prevention: Treatment & Management of OM Reoccurrence Prenatal Preventive Measures Avoid Exposure to Noise Pollution Visual Impairment o Partially Sighted: 20/70 – 20/200 o Legal Blindness: 20/200 or less o Etiology – perinatal or postnatal infections (gonorrhea, chlamydia, rubella, syphilis), retinopathy of prematurity, perinatal/postnatal trauma, other disorders and visual problems, unknown causes o Visual Impairment: Myopia: nearsighted Amospmetropia Hyperopia: farsighted Amblyopia: lazy eye Strabismus: misaligned Cataracts Astigmatism: uneven Glaucoma curvatures in vision Final Exam Review Pt. 2 o 5 Assessment & Promotion: Infants – expect binocularity by age 6 months (depth perception) Response to light, pupillary response, visual evoked response, ability to follow a target Childhood – Visual Acuity Testing Headaches, rubbing eyes, vertigo, poor school performance, tilting head to one side, closing one eye to see Promoting Optimal Development – play and socialization, independence, education, braille, audiobooks, safe environment, reassurance, orient child to surroundings, consistency of team members Plan of Care: Safe environment, orient to surroundings, encourage independence, consistency of team members Management: Prenatal Care/Prevention of Prematurity Rubella Immunizations FOR ALL CHILDREN!! Periodic Screening Final Q: What is the Safety Counseling historic cause of hearing Education on Glasses/Contacts – involve optometry PRN and visual impairments Refer to Support Groups in children? Rubella Historic Cause of Hearing and Visual Impairments in Children = Rubella!! Communication Impairment (emotional & social deprivation) o Inability to receive, process, transmit, or represent symbol systems o Delayed Language & Speech – most common developmental delay Speech problems are more prevalent than language disorders Both types decline as children grow older o M-CHAT – modified checklist for autism in toddlers o Nursing Care: Primary Intervention = Prevention Understanding normal speech & language development Assessment, Referral, Education Autistic Spectrum Disorders (ASD) o Complex brain dysfunction accompanied by broad range and severity of intellectual and behavioral deficits. Reassure parents NOT RELATED TO MMR VACCINE – diagnoses at same time as vaccine Encompasses: Autistic Disorder, Asperger Syndrome, and Pervasive Test Q: What is the Developmental Disorder best plan of care for a o Etiology: child with Autism? Unknown, Genetic Basis highly structured Appears 18-36 months of age; 4x more common in males routines and intensive behavior modification o Nursing Considerations: programs No cure; most promising results in highly structured routines and intensive behavior modification programs, importance of family counseling o Nursing Care: Primary Intervention = Prevention Understanding normal speech & language development Assessment, Referral, Education Final Exam Review Pt. 2 6 Premature and “At-Risk” Infants of CI o Classifications: Birth Weight LBW = < 2500g Test Q: What is the best indicator of high-risk VLBW = < 1500g infants for CIs? ELBW = < 1000g Gestational Age Gestational Age (best indicator) Pathophysiologic Problems Congenital Anomalies o Nursing Care: Developmental Support – assessments, NICU Controlled Environment – auditory/noise control, cluster care Special Handling – kangaroo care, gentle touch, facilitative tucking Assessments – APGAR, GA, Skin Assessments, Vital Signs, Temperature Maintain thermoneutrality (overhead warmer PRN) Fluid & Electrolyte Balance IV Fluids Nutritional Needs o Gavage Nipple Breastfeeding o Tolerance, Success, Resistance to Feeding Medication Administration Potential for drug toxicity and adverse drug reactions Parent-Infant Relationships Initial Shock and Denial Adjustments to Environment Parental Support – family support systems, parent care skills o Apnea of Prematurity Decreased Age = Increased Incidence Origins: Central, Obstructive, Mixed Monitoring: at home or in the hospital Treatment: Stimulate, Resuscitate, Document Pharmacologic Interventions: o Caffeine (most widely used) o Theophylline or Aminophylline (CNS Stimulants) monitor drug toxicity vs. therapeutic levels o Respiratory Distress Syndrome (RDS) Pathophysiology: lack of surfactant in the lungs contributes to alveolar collapse affected lungs become stiffer and require more pressure to achieve expansion, increased transudate of fluid is produced and further impairs gas exchange Clinical Manifestations/Diagnostics: Retractions – Substernal, Subcostal, Intercostal Nasal Flaring Grunting – with stethoscope or naked ear Therapeutic Management: Ventilatory Support, Conventional Ventilation Final Exam Review Pt. 2 o o o o o 7 Bronchopulmonary Dysplasia (BPD) & Chronic Lung Disease (CLD) O2 Requirements or Mechanical Ventilation >36 weeks of age May be marker of long-term pulmonary and neurologic outcome 15-40% of preterm infants – inversely rated to BW and GA Meconium Aspiration Syndrome Fetal Stress = Asphyxia Primary Asphyxia: gasping aspirations o In utero = meconium aspiration Infections (Neonatal & Maternal) Neonatal Infections – Neonatal Sepsis o Early Onset (3 days post-birth): acquired during perinatal period o Late Onset (1-3 weeks post): Nosocomial or Health-Care Associated Infection (HAI) o Diagnostics: Cultures of Blood, Urine, CSF CBC, HgB, Hct o Therapeutic Management: Antibiotic Therapy (2, 10, 14 days) Oxygen, Fluids PRBC Transfusion Maternal Infections – During early gestation can result in fetal loss or malformations because of the ability of the fetus to handle infectious organisms is limited and the fetal immunologic system in unable to prevent the dissemination of infectious organisms to various tissues Mother is tested for TORCHES Complex: o Toxoplasmosis, Other (Hep. B, Parvo, HIV, Varicella, Measles, Mumps), Rubella, Cytomegalovirus, Herpes Simplex, Syphilis Retinopathy of Prematurity A disease of preterm infants that affects the blood vessels of developing retina Severe Cases Results In: Retinal Detachment, Severe Visual Impairment, and Blindness Risk Factors: BW, GA, Hypoxemia/hypercarbia, Excessive O2 Neurological Problems: Hypoxic-Ischemic Brain Injury Most common cause of neurological impairment, results from asphyxia before, during, or after delivery o Ischemia and Hypoxia – simultaneously, or not Intra-Ventricular Hemorrhage (IVH) Most often in infants less than 32 weeks of gestation May Result in CNS/Motor Problems Cerebral Palsy (CP), or Seizures Causes: o Birth Trauma o Hypoxic Insult o Increased ICP or Intrathoracic Pressure o Hypertension Final Exam Review Pt. 2 8 o o Volpe Classification: o Catastrophic Deterioration – rapid deterioration to coma or deep stupor Respiratory Abnormalities, Cardiac Arrhythmias Fixed Pupils, Decerebrate Posturing, Generalized Tonic Seizures, Flaccid o Saltatory Deterioration – subtler, signs may stop altogether then reappear Altered LOC, Hypotonia, Subtle Abnormal Eye Position Decreased spontaneous or abnormal movements and an abnormally tight popliteal angle o Clinically Silent Deterioration – often overlooked clinically Sudden, unexplained decrease in hematocrit may be the only clinical sign of IVH Grading and Prognosis: o Higher Number = Poorer Outcome I III o Neurological Consequences, Unpredictability o Focus on Prevention of IVH Hypoglycemia Signs: Irritability, Jitteriness Eye Rolling, Poor Feeding Seizures, Hypotonia Cyanosis, Apnea Management: Bolus of IV Glucose – if unable to immediately feed o If using D-15 or D-25 – must infuse via central catheter (UAC/UVC) Drug Exposed Infants S/S of Withdrawal in Neonates: Irritability, Tremors, Shrill Cry Hypertonic Muscles Poor feeding, Vomiting, Diarrhea Seizures Sleep Disturbances, Fever Diaphoresis Nasal Stuffiness, Sneezing Tachypnea, Hyperactivity o NALOXONE = Avoid if Infant is Suspected of Drug Exposure May precipitate neonatal WD symptoms Opiate Exposure Cocaine Exposure: unlikely to show NAS Toxicology Screening Neonatal/Pediatric Effects – following intrauterine exposure Marijuana Exposure Methamphetamine Exposure: appear to be dose related Final Exam Review Pt. 2 9 Test Q: T/F – Fetal Alcohol Syndrome is 100% preventable. TRUE o Higher incidence in cleft lip/palate, cardiac defects, preterm delivery, and placental abruption Small Head Circumferences and Low Birth Weights Newborn Brady/Tachycardia Delays in Gross and Fine Motor Coordination Behavioral Changes – decreased arousal, increased stress, alterations in movement Alcohol Exposure Fetal Alcohol Syndrome (FAS): leading cause of cognitive impairment o Cognitive & Motor Delays Microcephaly, Poor Coordination, Hypotonia o Hearing Disorders o Facial Dysmorphia Short palpebral fissures, smooth philtrum, thin upper lip, short upturned nose o Irritable, Hyperactive Tobacco Exposure Polydrug Exposure ADHD Complete/Thorough Multidisciplinary Evaluation Behavior Checklist/Assessment Tools – IQ, Hand-Eye Coordination, Visual & Auditory Perception, Comprehension & Memory Therapeutic Management: Behavioral Therapy, Classroom Structures Family Education/Counseling, Environmental Manipulation Medication – not all children benefit o Stimulants: Dexedrine, Amphetamine, Adderall, Ritalin Side Effects: insomnia, anorexia, hypertension Long-Term Use Suppressed Growth Psychotherapy, Psychologic, Social Therapies Special Needs Children Reaction to Hospitalizations minimize loss of control o Infants to Preschool: separation anxiety, protest, despair, detachment/denial Test Q: A 1-year old o Early Childhood: separation anxiety greatest reaction of protest – goal-directed child’s reaction to hospitalization will o Childhood to Adolescence: loneliness, fear, anger, sadness, stress/regression, be what? cooperation, sleep disturbances Separation o Families: Anxiety Parents – stressed, angry, guilt Siblings – lonely, left out, stressed Minimizing Loss of Control: o Promote freedom of movement, parent/child contact o Prevent fear of bodily injury, maintain routine & independence of child o Patient-family-centered care nursing Pediatric Nursing & Consent o Informed Consent = age of majority/competence o Assent = process of obtaining informed consent < 18 years old Final Exam Review Pt. 2 10 Child is informed and willing, developmentally appropriate awareness, patient educated on expectations, understanding assessed, soliciting expression of child’s willingness o Emancipated Minor = legally underage, recognized to have legal capacity of adult Pregnancy, marriage, high school graduation, independent living, military o Treatment NOT Requiring Consent – STIs, mental health, alcohol/drug dependencies, pregnancy, contraceptive advice (exception – sterilization) Temperature Regulation in Children o Set Point, Fever, Hyperthermia Treatment = DANTROLENE (1st line treatment of malignant hyperthermia) o Febrile Seizure Antipyretics, Anticonvulsants – little evidence; Antipyretics = increase comfort Infection Control: o Standard – all contact with any bodily secretion o Airborne – mask, gown, gloves (N95/Hood) o Droplet – mask, gown, gloves o Contact – gown, gloves Restraining Methods: o Behavioral Restraints – antianxiety medications, relaxation techniques o Positioning for Procedures = swaddle (analgesia, sedation) o Physical Restraints – therapeutic hugging, jacket restraints, Test Q: On what mummy/swaddle, limb restraints group are physical Alternative Feeding Techniques: restraints used on o Gavage Feedings (NG/OG/NJ) most? Gavage = gravity; bolus o G-Tube/J-Tubes Pumps – continuous or intermittent feedings o Totally Parenteral Nutrition (TPN) Used when GI feeding is not possible – central line vs. peripheral line; intralipid infusion o Use pacifier during alternative feedings – nonnutritive suckling improves digestion Final Exam Review Pt. 2 11 CARDIOVASCULAR DYFUNCTION 9 questions Congenital Heart Disease (CHD) – abnormal anatomical defect that results in abnormal cardiac function (CHF/Hypoxemia) and is present at birth Final Q: Matching: CHD o results in altered hemodynamics, flow, and pressure and AHD. 2 Categories – CHD: results in CHF: defects that result in left-to-right shunting CHF/Hypoxemia AHD: seen in in normal Hypoxemia: defects that result in decreased pulmonary heart or CHD blood flow cause cyanosis Maternal Risk Factors for CHD – Rubella in Pregnancy, Fetal Drug Exposure, Increased Maternal Age, Maternal Metabolic Disorders, Genetic Factors, Environment, etc. Genetic Association with CHD – Familial Tendency; Unknown Genetic Reason CHD Presentation – Cardiac Failure, Cyanosis, Poor Feeding Left-to-Right Shunt, Altered Pulmonary Blood Flow Acquired Heart Disease – disease process that occur after birth; seen in normal heart or CHD o Result of: infection, autoimmune response, disease process, environmental factors, familial tendencies Embryology/Fetal Circulation: o Development begins at 4 weeks and is complete by 8 weeks’ gestation (note: lungs nonessential in utero) – heart beats on day 28 Test Q: Structural Defects: can be ID’d by 18-20 weeks something about o Structures: fetal structures of DA and PO Foramen Ovale (opening between atria) Ductus Arteriosus (opening between great vessels – aorta & pulmonary aa.) Conduction Tissue – maintains orderly and effective pumping action (SA Node = Pacemaker) o VSD = Damage to Conduction Tissues Bypass may need to be done, pacemaker for permanent damage ECG review: o Evaluates Conductive Tissue & Records Electrical Activity P Wave – atrial depolarization n PR Interval – delay AV node filling ventricles QRS Complex – depolarization of ventricles main pumping action T Wave – ventricular repolarization QT Interval – time taken for ventricular depolarization n& repolarization n ST Segment – ventricular repolarization begins (flat) o 3-lead: right – white, left - smoke (black) over fire (red) o 5-lead: right – white over green, left – black over read, brown in middle o 12 -lead: diagnostic & selectively identifies – 6 second strip to compare Cardiac Output = HR x SV o Preload – volume of blood returning to the heart (filling of the valves during diastole); circulating blood volume Starling’s Law = an increase in ventricular end-diastolic (caused by increased preload) increases stroke volume Final Exam Review Pt. 2 Test Q: Best indicator to measure CO of a pt. with a low preload? I&Os, Pedal Pulses o o 12 Direct Measurements: circulating blood volume using CVP Indirect Measurements: balance of I&Os, pedal pulses (best indicator) Reduce Preload By: diuretics, restrict/give fluids, I&Os, daily weights Afterload – resistance the heart (LV) has to work against for ventricular ejection Increased when conditions make it hard to pump blood into circulation Indirect Measurements: Blood Pressure (higher = increased afterload) Direct Measurements: central line or SWAN (direct pressure inside heart), SVR, PVR Can reduce afterload with ABCs – ace inhibitors, beta blockers, CCBs Improve tone after afterload – DA, EPI, NE Contractility – ability/efficiency of heart muscles to shorten and contract (Ca+) Assessed by: urine output & peripheral tissue perfusion Give: Digoxin to increase contractility Pulses, extremity warmth, capillary refill Normal Heart Pressures o Fetal Circulation – Placenta supplies blood via umbilical veins Blood enters 1) portal and hepatic circulation of liver or 2) directly to IVC via ductus venous Test Q: Which is true right atrium foramen ovale left atrium about fetal circulation? aorta head & upper extremities SVC pulmonary artery is shunted through the right atrium tricuspid valve right ventricle ductus arteriosus to the pulmonary artery shunted through ductus descending aorta arteriosus descending aorta returned to placenta from descending aorta through umbilical arteries o Neonate Vascular Changes – Before Birth: high PVR due to collapsed fetal lung = greater pressures in the right side. Free-flowing placenta circulation & ductus arteriosus = Low SVR Normal Heart Pressure – left side of heart is greater than pulmonary vascular resistance Birth: umbilical cord clamp lungs expand postnatal circulation Cardiac Assessment: o Pediatric Indicators of Cardiac Dysfunction – Poor Feeding, FTT Developmental Delays – d/t activity intolerance Difficulty with Air Exchange & Tissue Oxygenation Tachypnea/Tachycardia o History – maternal/prenatal, neonatal, birth, and family histories o Physical Exam General Appearance: Skin, Respirations, Chest Deformities Vital Signs: Pulse & BP Heart Auscultation: Check for Murmurs! Palpate for Liver Enlargement Fluid Status Activity & Behavior Final Exam Review Pt. 2 Test Q: Complication of Cardiac Catheterization? Aneurysms or Bleeding Test Q: What is a reason to cancel a cardiac catheterization? Severe Diaper Rash Test Q: What is the priority for the nurse when caring for a pt. who is pot-op cardiac catheterization? tissue perfusion; NV check of 6 P’s 13 Testing Cardiac Function – Pulse Oximetry Chest X-Ray: certain defects seen (Tetralogy of Fallot, AV canal, Transposition); can be diagnostic EKG: if strips inconsistent – order 12-lead; can detect cardiomegaly Echo: detects cardiac dysfunction; ultra-high-frequency waves shows heart structure Cardiac Catheterization – effective but invasive; high risk o Invasive procedure where a catheter is inserted through a peripheral blood vessel (femoral vein) into the heart. Usually combined with angiography (contrast material injected into circulation). Must obtain allergies before performing with dye. Gives oxygen saturation and pressure changes of blood within the chambers and great vessels, cardiac output or stroke volume, & anatomic abnormalities o Purpose: Palliation (Balloon Atrial Septostomy), Valvular Balloon Dilation, Diagnosis, and for Pressures & Oxygenation o Complications: Aneurysms or bleeding d/t invasive procedure through great arteries and veins o Preprocedural Care: Test Q: What Assessment: ASSESS PEDAL PULSES – assess and mark locations, clearly should the document; Accurate height & weight nurse be sure of before cardiac Severe Diaper Rash – cancel procedure if femoral access is required catheterization? Child is usually NPO before procedure good pedal Polycythemia Infants & Children: IV Fluids prevent dehydration pulses, child is Neonates: Dextrose Solution up to 2 hours to prevent hypoglycemia NPO o Postprocedural Care: Vital Signs, Neurovascular Checks (6 P’s), Assess Catheterization Site Apical Pulse 1 FULL MINUTE; Vital Signs q 15min. x 1hr q 30min. x 1hr pulse distal to site may be week for first few hours, but Quiz Q: Important extremity should be warm teaching for pt. with Bedrest, Leg Straight for 4-8 hours cardiac cath. Restrict activity 24 hours bedrest, leg I&Os, Encourage Hydration straight for 4-8 Occlusive Waterproof Dressing hours postprocedure; replace o Discharge Teaching: pressure dressing Remove Pressure Dressing Day After Apply Band-Aid (change QID day after and apply for 2 days) band-aid (replace Keep Site Clean & Dry QID for 2 days) avoid bathtubs (3 days) to prevent clot dislodging Monitor for swelling, drainage, bleeding, leg coolness Monitor entry site for swelling, infection, decreased perfusion Acetaminophen or Ibuprofen Final Exam Review Pt. 2 14 Congenital Heart Disease (CHD) o Major cause of death in 1st year of life, etiology unknown combination of: Maternal viral infections, increased maternal age, metabolic disorders, chromosomal abnormalities, genetic factors, environmental factors, Rubella Results in blood shunting – often hear a murmur Quiz Q: What would o Indicators: may not appear immediately you expect to see in a prenatal history, family history, poor feeding, failure to thrive, child with CHD? developmental delays r/t activity intolerance, tachypnea feeding difficulties and/or tachycardia o USE OF PULSE OX ON UPPER & LOWER EXTREMITIES o Therapeutic Management: minimize dysfunction – evaluate CO determinates Test Q: What is used as improve cardiac function the primary tx. to reduce remove fluid & sodium – decrease preload (diuretics) sodium and fluid in pt. Spironolactone or Lasix: mainstay of therapy to eliminate excess water with CHD? Lasix or Spirolactone and sodium reduce afterload: ACE Inhibitors (Captopril) decrease cardiac demands – cluster care, treat infections, reduce effort of breathing (semi-fowler position), decrease oxygen consumption improve tissue oxygenation Test Q: Why are CHD’s classified no longer identified as acyanotic vs. cyanotic? some that are classified as “acyanotic” can have cyanosis as well Final Exam Review Pt. 2 15 Increased Pulmonary Blood Flow (Acyanotic) o Patent Ductus Arteriosus, Atrial Septal Defect, Ventricular Septal Defect, AV Canal Blood flow to pulmonary vasculature increased, allows blood from high pressure left heart low pressure right heart left to right shunt CHF Symptoms: pink, difficulty with feedings, tachypnea, SOB, increased workload of heart, tachycardia, frequent respiratory infections, murmurs Responsive to Oxygen; has enough RBCs Treatments: digoxin, ace inhibitors, fluid management, diuretics, oxygen untreated = irreversible pulmonary hypertension o Patent Ductus Arteriosus (PDA): failure of ductus arteriosus to close within 1st weeks of life (48 hours); may be caused by problems with fetal circulation (placenta issues) Connection between the pulmonary artery and aorta that has failed to close Clinical Manifestations: FTT, respiratory infection, CHF symptoms, common in preterm infants Final Q: What CHD is Characteristic murmur (past 5-8 days of birth) with widened pulse recognized by pressures and bounding pulses characteristic murmur Causes a left to right shunt causing blood to recirculate to the lungs (pulmonary 5-8 days past birth with widened pulse pressure artery over circulation) and bounding pulses Treatment: (depends on presentation of the patient) Medically – Indomethacin (Indocin), a PgE Inhibitor Cath Lab – percutaneously with occlusion (coils) Surgically – Thoracotomy (1st choice – immediate) o If not symptomatic, percutaneously occlude with contrast dye o Atrial Septal Defect (ASD): failure of the foramen ovale to close resulting in persistent fetal circulation, blood shunts from left atria to right atria not as much force pushing blood to right side of the heart Some are persistent fetal circulation, some are structural defects (hole in filling chambers) May spontaneously close in 4 years of age Symptoms: depend on the size of the defect; (+) for murmur Treatment: Cath Lab – percutaneous patch (small ASDs) Surgically – patch/pericardium to close; bypass machine (large ASDs) o Ventricular Septal Defect (VSD): failure of the septum between pumping chambers to form; hole between pumping chambers present sooner d/t shunts being more increased Most common of heart defects, but frequently associated with other defects Prognosis: depends on location, number of defects, may close on its own in 1st year of life Treatment: Surgical Closure (Percutaneous Transcatheter Device) – large VSDs small ones are followed up with by cardiologist Do NOT use – occlusive d/t clotting stroke (left side) or PE (right side) o Atrioventricular Canal Defect (AV Canal): incomplete fusion of the endocardial cushions low ASD (hole between filling) high VSD (hole between pumping) one common AV valve presents very early Final Exam Review Pt. 2 16 Av Canal Defect: Most common cardiac defect in children with Down’s Treatment: (surgical) Palliative – Pulmonary Artery Band: restricts pulmonary blood flow o Buys time for child to grow – temporary repair o too tight cyanosis & hypoxic spells, too loose HF Corrective – close hole between pumping and filling chambers creating two new valves out of common AV valve o Look for problems with conductive tissue from surgery or valvular problems in patient postoperatively Decreased Pulmonary Blood Flow (Cyanotic) o Tetralogy of Fallot, Tricuspid Atresia, Pulmonary Atresia BF to pulmonary vasculature decreased, results in cyanosis (blue spells); allows deoxygenated blood to shunt right to left blood into systemic circulation without being oxygenated Test Q: What manifestations NOT responsive to oxygen – not enough RBCs to lungs are associated with Hypoxemia (low SaO2), Hypoxia, Cyanosis (deoxygenated Hgb) decreased pulmonary blood Clinical Manifestations: O2 Sats = 50-90%, dusky, mottled/cyanotic, chronic flow heart defects? Select all hypoxemia and appears blue, fatigue, exertional dyspnea, failure to thrive, dusky, mottled, chronic hypoxemia and appears difficult eating and breathing at the same time, clubbing, delayed milestones, blue, bradycardia, poor weight gain, bradycardia, compensatory polycythemia (clotting polycythemia abnormalities) Hypercyanotic or Tet Spells o Infants oxygen requirements exceed the blood supply – usually Test Q: What should the crying after feeding – can result in sudden death nurse’s plan of care be for a o If crying = squat to counteract cyanosis child experiencing a Tet Knee to Chest Position Spell? Final Q: What should the put child in knee-to-chest Palliation – Cardiac Shunts: increases blood flow to lungs nurse monitor with a pt. position who is post-op BT Shunt? Prostaglandins & Cardiac Shunts preload, hydration, o Blalock-Taussing Shunt bleeding r/t Aspirin Atrial Septostomy o Place child on prostaglandins first hole made by cardiac catheter between left & right atria – can diagnose at the same time o Post Op: check preload, hydration, bleeding r/t aspirin o Tetralogy of Fallot: blue babies Final Q: Which of the 4 Characteristics: following are seen in Tetralogy of Fallot? VSD polycythemia, Tet Pulmonary Stenosis spells, blue appearance Overriding Aorta Right Ventricular Hypertrophy Symptoms: Loud Murmur, Tet Spells Sudden Death, Seizures; Clubbing, Heart Appears “Boot-Shaped” Test Q: Complication of Blue blood going to red side Tetralogy of Fallot? Complication: Compensatory Polycythemia Compensatory Polycythemia Treatment: can only correct VSD & Pulmonary Stenosis (redilate pulmonary a.) Complete repair during first year of life; closure of VSD and resection of stenosis; patch placement to enlarge right ventricle outflow tract Test Q: Which cardiac defect is most commonly associated with Down’s Syndrome? AV Canal Defect Final Exam Review Pt. 2 o o 17 Tricuspid Atresia: tricuspid valve fails to develop no communication of right atrium and right ventricle = no blood getting to the lungs Ductal dependent lesion; present when fetal circulation develops S/S: presents when fetal circulation closes – o ashy/dark, poor stats, tachypneic, tachycardia Lots of these patients do not have pulsatile flow = given Sildenafil (Viagra) to lower pulmonary hypertension Immediate intervention @ birth until surgical intervention arranged Balloon Septostomy Prostaglandins E1 – keeps ductus open until surgical intervention Surgical Treatment – STAGED REPAIR Palliative: Central Shunt o SVC/IVC pulmonary artery blood returns to heart without pulsation Pts. without pulsatile flow – give Sildenafil (Viagra) Bidirectional Glenn Shunt o Cavo Pulmonary Anastomosis Modified Fontan Procedure Pulmonary Atresia: pulmonary valves don’t exist Ductal Dependent; Easier to Repair Early Symptoms Children with PA: make single ventricle back to lungs without pulsatile flow = ventricle works Extreme version of Pulmonary Stenosis, total fusion of commissures and no blood flow to the lungs Obstructive Pulmonary Blood Flow (Acyanotic) o Coarctation of Aorta, Aortic Stenosis, Pulmonary Stenosis Impedes Blood Flow Out of Ventricles Obstruction on Left Side = Heart Failure Obstruction on Right Side = Cyanosis Similar to Symptoms of Low CO – o Diminished Pulses, Poor Capillary Refill & Color o Decreased Urinary Output & Flow to GI Tract r/t kidney function decreased & intolerance with feeding & absorption problems o CHF with Pulmonary Edema o Coarctation of the Aorta – narrowing of aorta by arch (ductus); tightness determines severity, makes it hard for LV to pump = left-sided heart failure Presentation: Classic – younger children o BP Discrepancies – higher upper than lower Test Q: Disorder with Causes increased pressure proximal to narrowing, increased blood pressure in upper decreased pressure distal to obstruction (upper vs. lower extremities and body pressures) decreased BP in lower o Pulse Discrepancies Final Q: What heart extremities? Coarctation of Aorta defect is associated with pulse discrepancies? Coarctation of the Aorta Final Exam Review Pt. 2 18 o o Later – Older Children o Hypertension UPPER extremities o Dizziness, headache, fainting, epistaxis o Decreased/Absent Pulses LOWER Extremities o Rib Notching Treatment Cath Lab: Balloon Dilation [increase the diameter] o Treatment of choice for OLDER infants and children Surgical: end-to-end anastomosis, subclavian flap, then patch graft o Treatment of choice for infants younger than 6 months o Post-op: check for bleeding, clotting, distal pulses, BP upper & lower extremities Aortic Stenosis – narrowing of aortic valve causing resistance to blood flow from the left ventricle Left-Sided Heart Failure HF Clinical Manifestations – S/S Decreased CO (faint pulses, hypotension, tachycardia, poor feeding) Exercise Intolerance Chest Pain Dizziness with Standing for Long Periods Characteristic Murmur At Risk For – Infective endocarditis, Coronary Insufficiency, Ventricular Dysfunction Treatment – Cath Lab: Balloon Dilation o First-Line Procedure Aortic Valvotomy [Rare] Pulmonary Stenosis – narrowing of the pulmonary valve resistance Right-Sided Heart Failure Clinical Manifestations – May be Asymptomatic Cyanosis, Some Mild HF o Newborns with severe narrowing = cyanotic Characteristic Murmur Cardiomegaly – apparent on chest radiograph At Risk For – Infective Endocarditis Treatment – Cath Lab: Balloon Angioplasty o Need for surgery is rare d/t wide spread balloon techniques o Associated with few complications, highly effective o Treatment of Choice! Surgery = RARE o depending on severity o in some cases, cardiopulmonary bypass may be necessary Final Exam Review Pt. 2 19 Mixed Blood Flow (Cyanotic) o Transposition of the Great Arteries/Vessels, Hypoplastic Left Heart Syndrome Complex cardiac anomalies that requires mixing of blood in postnatal period Combination Defects: more than one defect can compound problems or cancel them out Desaturated blood mixed with saturated blood; no increase or decrease in BF, defects balance them out Hypoxia & Heart Failure can occur together Pulmonary Congestion Occurs, Cardiac Output Decreases Clinical Manifestations – Variable Picture that Combines: Desaturation & Signs of CHF o Cyanosis not always visible Often Requires Multiple Surgical Interventions o Transposition of the Great Arteries/Vessels (TGA) – parallel blood flow; blood goes to pulmonary artery/aorta then back to the heart through the same way Pulmonary Artery = outflow for left ventricle Aorta = outflow for right ventricle Most common defect is patent foramen ovale – life threatening at birth Quiz Q: What does the Clinical Manifestations – nurse know when caring cyanosis at birth that does not improve with oxygenation for baby with TSA? CHF may develop at birth or a couple of days another heart defect “egg on its side” seen on CXR must be present to sustain life abnormal position of the great arteries seen on Echo Treatment – Arterial Switch – Prostaglandin E1 given after birth to maintain PDA Test Q: Post-Op concern until surgery performed following Arterial Switch? o Common Complication = arrhythmias; may need pacemaker EKG to check for o Survival Without Surgery is IMPOSSIBLE! ischemia (Coronary Perfusion) o Post-Op Concerns: Coronary Perfusion EKG for Ischemia (coronary perfusion) enzymes for cardiac muscle death o Hypoplastic Left Heart Syndrome (HLHS) – underdeveloped left side of heart, small left ventricle and aorta Clinical Manifestations – cyanosis noted after birth single heart sound auscultated; no murmur present usually fatal after 1 month with no intervention Therapeutic Management – Prostaglandin E1 given to maintain PDA until surgery (allow mixing of blood); AVOID SUPPLEMENTAL O2 Treatment (4 options): Comfort & Palliative Care Heart Transplant Staged Procedure Hybrid Procedure Final Exam Review Pt. 2 Test Q: What teaching should the nurse prepare for a pt. with HLHS? Staged Norwood Procedure 20 o Staged Procedure: Stage 1 NORWOOD – left side is nonfunctional; make one ventricle pump for the whole body, new aorta, blood flow ONLY through shunts (newborn) At risk for clots d/t Aspirin o monitor for Reye’s Syndrome Viagra for pulmonary vascular reduction Stage 1 HYBRID – do not need bypass machine; done in Cath lab If candidate, put on PgE1 Cath lab atrial septostomy (stent in ductus arteriosus to keep open) brought in later for Norwood & begin stages Stage 2 Bidirectional Glenn Shunt – SVC hooked to pulmonary artery to create passive flow, not pulsatile Give lots of Viagra Stage 3 Modified Fontan – SVC & IVC both passively flowing in the great arteries Post-Op Cardiac Patient: o Monitor chest tube for bleeding and/or tamponade – record hourly drainage o Catheter to Indicate CO; Continuous VS [heart pressures & changes] Intracardiac & Intraarterial Monitoring o Intubated overnight; extubate next day Care After Heart Surgery: o Monitor and Prevent Infection & Bleeding o Respiratory Complications: pneumothorax, pleural effusion, muscle fatigue, atelectasis Final Q: What is a o Pain Management; Manage Fluids & Nutrition; Elevate HOB common complication post Feed pt. as soon as bowel sounds present op heart surgery o Neutral Thermal Environment that the nurse o Avoid Picking Up from Under the Arms should be aware of? o Prevent Thromboembolism – those at risk, administer aspirin, maintain hydration Cardiac o Quiet Games/Activities Tamponade o Continuous Monitoring For: arrhythmias, cardiac tamponade, cardiac output/perfusion, bacterial endocarditis, HF & pulmonary HTN, pharmacological support Pharmacological Support – Enhance CO: o Furosemide (Lasix): Adverse Effects = Hypokalemia Spironolactone: decreases preload Adverse Effects = Hyperkalemia Test Q: Select all o Digoxin (Lanoxin) – increases contractility; decreases HR the medications Apical Pulse 1 Minute do not give if HR is low that can be given to Dig Toxicity Monitoring – bradycardia, vomiting (early), enhance CO. nausea/anorexia, neurological symptoms, visual disturbances Final Q: What would o Captopril/Enalapril – decrease afterload the nurse expect to Prevent Pulmonary HTN: Sildenafil (Viagra) give to decrease afterload? Captopril Final Exam Review Pt. 2 Super Ventricular Tachycardia – dysrhythmia; can be lethal, unchanged high HR o Starts with SA node; symptoms determine treatment Treatment (depending on condition) – Valsalva Maneuver: blow through straw or splash cold water on face Adenosine: time out [asystole], restart the heart; very rapid IV push (short ½ life) Synchronize Cardio Version: low energy shock with peak of QRS ACQUIRED HEART DISEASES o Bacterial Endocarditis, Infective Endocarditis, or Subacute Bacterial Endocarditis Infection of the inner lining of the heart (endocardium), involving the valves Causes – Streptococci, Staphylococci, Fungal Infections Pathophysiology – Organisms in bloodstream from any site of localized infection o May occur from routine activities (brushing teeth), catheters Altered BF & Turbulence Damage to Valvular Endothelium – form vegetation on endocardium Lesions may infect adjacent tissues [valves and myocardium] May break off and embolize [spleen, kidney, CNS] Clinical Manifestations – Malaise, Low-Grade Fever New Murmur/Change in Previous Murmur S/S of HF may present Signs d/t Embolus Formation Elsewhere – o Splenomegaly o Osler Nodes [red, painful nodes on pads of fingers] o Janeway’s Lesions [painless spots on palms & soles] o Splinter Hemorrhages [think, black lines] Major Criteria – Blood Cultures IE Diagnosed If: Echocardiographic Evidence 2 Major Criteria Minor Criteria – 1 Major + 3 Minor Criteria Fever 5 Minor Criteria Predisposing Risk Factors [central line, IV drug use] Vascular and Immunologic Findings Therapeutic Management – High-Dose IV Antibiotics [2-8 weeks] o Evaluate Effectiveness with Repeat Blood Cultures Little to No Change = Surgical Approach [remove vegetation, valve replacement] Prevention of IE – Prophylactic Antibiotics: ONLY for highest risk of CHD pts. o Take before dental work, invasive respiratory treatment, or procedures on soft tissue infections Meticulous Dental Hygiene [prevent infection] 21 Final Exam Review Pt. 2 o 22 Kawasaki Disease (Mucocutaneous Lymph Node Syndrome) – acute systemic vasculitis of unknown cause; self-limiting (6-8 weeks) – peak in toddlers, seasonal variations Damage to coronary arteries & heart muscle can occur – coronary dilation Test Q: Complication associated with (ECTASIA), coronary artery aneurysms (ischemia, tamponade, clotting, MIs) Kawasaki Disease? Acute – abrupt high fever unresponsive to antibiotics & antipyretics – Coronary Artery hospitalized Aneurysm o Conjunctivitis without drainage, strawberry tongue, edema in hands and feet, extreme irritability, periungual desquamation, arthritis, non-blistering rash, bilateral joint pain, enlarged Test Q: Pt. presents with lymph, cervical lymphadenopathy, decreased left vent function, strawberry tongue, high fever, pericardial effusion, mitral regurgitation and is inconsolable. What Subacute – resolution of fever until all outward clinical signs disappear would the nurse assume? Kawasaki Disease o Still irritable, peeling of skin nails/palms, temporary arthritis Convalescent – no manifestations except on labs Test Q: What o Erythrocyte & CRP Increased; back to normal 6-8 weeks cardiac Cardiac Involvement of KWD – involvement is seen in Kawasaki particularly the coronaries Disease? Serious Complication – POTENTIAL MI potential for Final Q: What is the Treatment – MI; particularly in appropriate treatment IV Immune Globulin (IVIG): stop autoimmune from occurring the coronaries for Kawasaki Disease? Aspirin: prevents clotting, sent home IV Immune Globulin Nursing Care – (IVIG) & Aspirin Early Diagnosis & Treatment, Prevention of CV Complications Monitor I&Os Symptomatic Relief, Address Symptoms & Pt. Irritability Discharge Teaching: continue aspirin through course of subacute phase HEMATOLOGICAL DISORDERS o Sickle Cell Anemia Autosomal Recessive hereditary Hemoglobinopathy Ethnicity/Malaria: 1 in 12 African Americans are Carriers Diagnosis – cord blood in newborns tested genetic testing sickle turbidity test for children older than 6 months Assessment of Hematologic Function – CBC (normal life = 120 days; sickle cell hemolysis = 40 days) History & Assess. [fatigue, SOB on exertion, joint pain, neonatal screen] Energy & Activity Level Growth Patterns o Sickle Cell Disease Autosomal Recessive Disorder, Chronic Disease, primarily African American Causes of Crisis – Decreased Oxygen Tension Hgb S to Sickle o Hypoxia Occurs and Causes Sickling o Infection, Fever, Trauma o Dehydration, Acidosis o Hypoxia Final Exam Review Pt. 2 23 High Temperatures: exposure to cold High Altitudes Physical/Emotional Stress (puberty) o Sickle Cell Crisis Vaso-Occlusive Crisis: painful episode/pain crisis; sickled Hgb increases risk for CVA and vital organ infarction Monitor for good perfusion; large tissue infarctions occur Increased RBC destruction > RBC production Sequestration Crisis: splenic sequestration – sickled cells become fragile an easily hemolyzed in the spleen pooling of blood & infarction of splenic vessels Clinical Signs: profound anemia, hypovolemia, shock May require splenectomy @ early age; results in decreased immunity Chest Syndrome: overwhelming pneumonia r/t inability of spleen to filter s/s – chest pain, fever, cough, dyspnea Overwhelming Infarction Cerebrovascular Accident – transcranial doppler annually 2-16 years old Test Q: which of the o Nursing & Care Management = Supportive following should Hydration & Electrolyte Replacement the nurse question Pain Management DO NOT GIVE DEMEROL (Morphine, Dilaudid ok) before administering to a Promote Tissue Oxygenation, Prevent Infection (PCN) pt. with sickle cell? Prevent Sickling Episodes, Early ID of Crisis Demerol Careful Monitoring of SHOCK Education: splenomegaly, dehydration, no contact sports, avoid heat & low O2 o Prognosis: no cure (possible bone marrow transplants), frequent bacterial infections r/t immunocompromised bacterial infection = leading cause of death DEFECTS IN HEMOSTASIS o Hemophilia: group of hereditary bleeding disorders that result from deficiencies of specific clotting factors; x-linked disorder Diagnosis – amniocentesis, genetic testing for carriers Clinical Manifestations – bleeding tendencies (mild severe), hemarthrosis, ecchymosis, internal bleeding, hematuria, epistaxis, bleeding post procedures (minor trauma, tooth extraction, minor surgeries, hemorrhages, bleeding compromising airway) Hemophilia A most common, factor VIII (8) deficiency Hemophilia B deficiency of factor IX (9) Mild: bleeding with severe trauma or surgery Moderate: bleeding with trauma Severe: spontaneous bleeding without trauma Clinical Therapy: prevent bleeding, amniocentesis diagnosis, genetic testing, labs, history, and exam diagnosis Treatment: recognize & control bleeding o Final Exam Review Pt. 2 24 Test Q: What should nurse implement for hemarthrosis? RICE Institute factor replacement therapy DDAVP (IV) – Desmopressin: help production of components that help with clotting (mild) Prevent crippling effects of bleeding RICE for Hemarthrosis Prognosis: near normal lives; gene therapy for future Education: First aid for small cuts/abrasions o Clean Cut = apply pressure & band-aid o Severe = give factor VIII Promote Independence: regular school o avoid contact sports; may swim or golf Home Care: venipuncture & factor VIII admin If complaining of joint pain, send immediately to school nurse Final Exam Review Pt. 2 25 GI DYSFUNCTION/TRANSFER OF NUTRIENTS 8 questions Review o Nutrition – Healthy Newborn: 108 kcal/kg/day Infant Nutritional Care – o Solid Foods 6 months; introduced 1 at a time, every 4-7 days o Cow’s Milk 1 years old d/t deficient source of Vitamin C, iron, or zinc o 2% Whole Milk NOT UNTIL 2 YEARS! Limiting milk sources can decrease risk of anemia Toddlers: 102 kcal/kg/day; Preschoolers: 90 kcal/kg/day Toddler & Preschool Nutritional Concerns – o Physiologic Anorexia (12-18 months): growth slows down, finicky eaters Reassure parents this is normal, give healthy snacks child enjoys o Non-Nutritive Function: pleasure/comfort food, social activity Discourage food becoming a reward o Parental Guidance: calm eating environment, stress free & fun, varieties of choices, cut food into small pieces School Age: 1200-1800 kcal/day Test Q: When Family eating habits remain large influence; peer influences @ lunch teaching a parent Increased independence in food choice – remind stop eating when full about their child’s nutrition, what Midafternoon snacks = common; healthy (no midmorning snack) would the nurse o MyPlate: shows parents a good way to form a child’s plate suggest? Insufficient Dairy Intake; Vitamin D Deficiency MyPlate Adolescents: 1800-2200 kcal/day Females need 2200 kcal/day to support growth spurt; males need 25002900 kcal/day – these decrease after growth spurt Test Q: What is o 4 servings of dairy for growth spurt important Test Q: While nutritional Preparing own food & eating with friends – still need adult guidance teaching an obesity education for Vitamin D deficient prevention class, parents of an which is NOT correct? o Exercise – adolescent? 20 min of exercise All well visits include nutritional/exercise screen, desirable BMI 5th – 84th % still needs daily is sufficient for adult guidance Healthy Heart Activity Levels = prevention 1 hour/day moderate to vigorous activity Vigorous activity 3 days/week Test Q: Eating PICA: eating disorder of compulsive & excessive ingestion of food & nonfood substances at disorder that involves least once a month eating Starvation – nonfood o Severe Acute Malnutrition: caused from poor feeding & sanitary conditions substances 3rd world countries PICA o Kwashiorkor: deficient protein with adequate calories; diet of starch & potatoes Thin, wasted extremities with protuberant abdomen general edema masks atrophy Final Exam Review Pt. 2 26 o Test Q: Test to diagnose diabetes? A1C Marasmus: general malnutrition of calories & protein; decreased subcutaneous tissue Extreme thinness Obesity – Final Q: Parent are concerned about dark lines on child’s neck. o Hypertension: BP screening @ 3 years of age What should nurse respond? o Type II Diabetes: Acanthosis Nigricans (dark line indicators) Acanthosis Nigricans d/t o Hyperlipidemia: increased lipid levels increased levels of insulin which th th o BMI > 85 to 95 = overweight could possibly indicate T2DM above 95th = obese Obesity Complications – o Type II Diabetes, Syndrome X, Fatty Liver, Pulmonary Dysfunction, Growth Acceleration o Depression, Low Self-Esteem, Bullying Obesity Diagnostics/Treatment – o Labs: lipid panel, A1C, liver enzymes, sleep studies o PREVENTION IS KEY; behavior modifications, family interventions, surgical interventions (18+), exercise, diet, etc. Must be ready to make a change DISORDERS OF MOTILITY o Hirschsprung Disease (Congenital Aganglionic Megacolon): congenital abnormality from inadequate motility causing mechanical obstruction; absence of ganglion cells; no Test Q: Matching GI evacuation of stool [matching test question] Disorder. Absence of Symptoms – ganglion cells and the Newborn: failure to pass meconium, vomits bile, refusal to eat, failure to pass meconium in abdominal distention newborn. Hirschsprung Disease Infant: FTT, constipation, vomiting, diarrhea Child: undernourished, anemic, abdominal distention, visible peristalsis, palpable fecal mass, constipation, foul-smelling ribbon like stool Final Q: Absence of ganglion Diagnosis – cells, failure to pass Test Q: What would Rectal Biopsy: shows no ganglion cells meconium, foul-smelling, the nurse prepare ribbon-like stools. Diet – for a pt. pre-op Hirschsprung Hirschberg surgery? High Calorie, High Protein, Low Fiber Barium Enema Treatment – Surgical removal of aganglionic portion, possible colostomy Test Q: How is Hirschsprung o Pre-Procedure: assess for adequate nutrition, bowel emptying, Disease diagnosed? rectal biopsy shows no and abdominal distention ganglion cells o Post Procedure: educate parents on enterocolitis, Final Q: What should fecal incontinence & obstruction, ostomy care child with Hirschsprung be prepared for? Complications – possible colostomy Enterocolitis: inflammation of the digestive tract d/t infection o Antibiotics before surgery to decrease bacterial flora Final Exam Review Pt. 2 27 o Gastroesophageal Reflux (GER): transfer of gastric contents into esophagus; occurs more after meals and at night Risk Factors – prematurity, BPD, neurological impairments, asthma, CF, CP, scoliosis Test Q: What should the usually resolves by 1 year of age nurse tell the mother of a GER becomes a disease when complications such as FTT, resp. 4-month-old with GER? may resolve by 1 year problems, or dysphagia develop GERD of age Symptoms – Infants: o sitting up/forceful vomiting, irritability, excessive crying, blood in vomit, arching of back, FTT, apnea Children: o heartburn, abdominal pain, difficulty swallowing, chronic cough, noncardiac chest pain Diagnosis – 24 upper pH probe study: gold standard upper GI endoscopy: can exclude other disorders such as Chron’s Care – Final Q: Which of the following small, frequent meals; thicken infant formula with rice cereal shows understanding of the o constant NG feedings may be needed with severe reflux and FTT teaching for a child with GER? until surgery can be performed “I will thicken my infant’s formula with rice cereal” avoid caffeine, citrus, peppermint, spicy/fried foods assist in weight control elevate HOB after meals o no prone position o Quiz Q: Child with GERD is at risk for? Aspiration Gastroesophageal Reflux Disease (GERD): Test Q: What is the symptoms/tissue damage from GER disease process that Causes – results from tissue o FTT, respiratory issues, or dysphagia damage d/t GER? o At Risk For: Aspiration GERD Nursing Interventions – o same as GER o + proton pump inhibitor (omeprazole or pantoprazole) o H2 receptor (ranitidine, cimetidine, famotidine) Treatment – o Nissen Fundoplication: takes gastric fundus & wraps around esophagus Post-Op: gastric decompression by an NG tube or gastrostomy to avoid distention in immediate post-op period Should not be replaced by the nurse if Test Q: What procedure accidentally removed because of risk of injury would the nurse prepare to the operative site to educate a patient with GERD on? Nissen Fundoplication Final Exam Review Pt. 2 28 INFLAMMATORY CONDITIONS o Acute Appendicitis: Inflammation of the vermiform appendix; most common emergency in children Clinical Manifestations – Periumbilical Pain RLQ; Rebound Tenderness o McBurney’s Point: most common point of tenderness N/V, Fever, Diarrhea or Constipation Test Q: Child with Tachycardia, Lethargy, Poor Feeding abdominal pain, fever, and Decreased/Absent Bowel Sounds vomiting. What would treatment would the nurse Diagnosis – prepare for? CT Scan, Ultrasound Antibiotics, IV Fluids, NG CBC, UA, CRP (WBC >10,000/mm3) Suction Management – Final Q: What would the Appendectomy (before rupture/perforation) nurse prepare for when a child has appendicitis and has Antibiotics, IV Fluids, NG suction (ruptured) not yet ruptured? Complications – Appendectomy perforation, peritonitis, abscess, phlegmon, fistula, partial bowel obstruction o Meckel’s Diverticulum: Failure of the omphalomesenteric duct to fuse during embryonic development when placenta replaces yolk sac fistula, umbilical cyst, and Meckel’s diverticulum Symptoms – painless rectal bleeding abdominal pain, distention, n/v bloody mucus stools causes: fistula, umbilical cysts Rule of 2’s Diagnosis – Radionucleotide Scan (Meckel’s scan) OBSTRUCTIVE DISORDERS o Hypertrophic Pyloric Stenosis: Circular muscle of pylorus thickens so pyloric canal narrows; lumen becomes Test Q: A child is irritable, hungry, partially obstructed worsening hypertrophy and vomits 30 minutes after each Clinical Manifestations – feeding. An olive-shaped mass is o Vomiting occurs 30-60 min. after feeding seen in abdomen. o Irritable, hungry, dehydrated, decreased weight, FTT Hypertrophic Pyloric Stenosis o Olive-Shaped Mass – upper abdomen o Gastric peristalsis visible Final Q: What can be seen Management – in Hypertrophic Pyloric o Pyloromyotomy (good prognosis) Stenosis? Pre-Op: Correct Metabolic Alkalosis with IV Fluids & Olive-Shaped Mass Electrolytes, NPO Post-Op: may need NG tube if vomiting continues; 4-6 hours start feeding, formula after 24 hours; small, frequent feeds Test Q: What should be pre-op procedure for pt. with Hypertrophic Pyloric Stenosis? NPO, IV Fluids, Prep for Surgery Final Exam Review Pt. 2 29 o Intussusception: Proximal segment of bowel telescopes into distal segment, pulling mesentery; mesentery = angled & compressed lymphatic/venous obstruction Ischemia occurs mucus pours into intestine JELLY STOOLS Clinical Manifestations – o Sudden, acute abdominal pain screaming, drawing knees to chest Final Q: A child with intermittent severe abdominal o Comfortable between episodes pain is screaming, drawing o Vomiting knees to chest; and o Red, currant JELLY LIKE STOOLS comfortable between episodes. o Sausage Shaped Mass in URQ He has red, currant, jelly-like o Most common in ileocecal valve (3-6 months of life) stools. Intussusception Treatment – o Hydrostatic Enema (gas enema) o IV Fluids, NG Decompression, Antibiotic Therapy o Surgery if Needed (possible bowel resection) MALABSORPTION SYNDROMES o Celiac Disease (Gluten-Sensitive Enteropathy): autoimmune disorder triggered by ingestion of glutens; damages villi in small intestine = malabsorption Food Intolerances: protein present in wheat, barley, and rye Test Q: What foods would a o Beans, pasta, beer, etc. pt. with celiac Disease be usually appears around 1-5 years of age able to eat: waffles, bacon, Test Q: Education for Clinical Manifestations – toast, low-fat milk, bananas? adolescent with bacon, low-fat milk, celiac disease: intestinal symptoms, FTT, chronic diarrhea bananas gluten in beer aphthous ulcers canker sores abdominal distention & pain fatigue, muscle wasting untreated = lactose intolerance o Short-Bowel Syndrome: Decreased mucosal surface area d/t small intestine resection decreased area for absorption of fluids, electrolytes, & nutrients o NEED FOR TPN NUTRITION! (glucose, sucrose, etc. needed) Initial Phase: PN as primary source of nutrition Test Q: What nutritional support does a patient with 2nd Phase: introduce eternal feeing after surgery short bowel syndrome need? Formulas containing glucose, sucrose, proteins, TPN as primary source, and triglycerides facilitate absorption (NG/G introduce eternal feeding Tube) after surgery Test Q: What is needed As enteral feeds are advanced, PN solutions is with TPN in post-op pts. decreased in terms of calories, amount of fluid, with SBS? and totally hours of infusion per day. glucose, proteins, If enteral feeds are tolerated, oral feedings sucrose, triglycerides should be attempted to preserve oral skills. Final Exam Review Pt. 2 o 30 Causes – multiple atresia, gastroschisis, necrotizing volvulus, meconium peritonitis, chron disease, trauma Management – preserve length of bowel as much as possible maintain optimum nutrition, growth, and development stimulate intestinal adaption with enteral feeding (TPN) minimize complications Complications – most deaths r/t sepsis d/t poor care of central line Necrotizing Enterocolitis (NEC): Acute inflammatory disease of the bowel where mucosal wall is damaged and gas-forming bacteria invade; most common in preterm Potential Cause: decreased BF to intestines Test Question: Matching GI Disorders. Inflammatory disease Pneumatosis: air in the submucosal & subserosal surfaces of the bowel of bowel, mucosal wall damaged, Clinical Manifestations – bacteria invasion of damaged o Distended Abdomen, Blood in Stools areas. o Gastric Residuals: check NG/G tube every feed (increased – red NEC flag) o Poor Feeding, Lethargy, Hypotension, Apnea, Vomiting Bile, Test Q: Major risk factor Decreased Urine Output, Hypothermia for NEC? Diagnosis – Prematurity o Sausage-Shaped Dilated Intestine, “soap suds” or bubbly o Free air in abdomen perforation n o Labs: anemia, leukopenia, leukocytosis, metabolic acidosis, Test Q: Disorder with free electrolyte imbalance air in the abdomen with Management – “soapsuds” seen in scan. o Hold Feeds for 24-48 hours if Asphyxiated at Birth NEC o Breast Milk Preferred (enteral feeds) – IgA passive immunity o Minimal Feeds – Trophic in VLBW (wake up gut slowly) o Probiotics: in 1st 7 days; 14 days in preterm/VLBW infants o Confirmed NEC: Discontinue all oral feeds IV Antibiotics NGT – decompression TPN – nutrition o Sequelae in surviving infants include short bowel syndrome 2/2 intestinal dysfunction o Nursing Management: Key Factor = Prompt Recognition Test Q: What is associated Monitor VS for s/s of Bowel Perforation, Septicemia, or with NEC? CV Shock Short Bowel Syndrome Prevent Possible Transmissions Strict handwashing, isolation of confirmed cases Leave infant UNDIAPERED and in SUPINE or ON SIDE Final Exam Review Pt. 2 31 Oral feedings reinstituted ~7-10 days after treatment Biliary Atresia: Inflammatory process that causes intrahepatic and extrahepatic bile duct fibrosis ductal obstruction Test Q: Matching GI Disorders. Inflammatory process that o occurs late in gestation, manifests a few weeks after birth causes intrahepatic and Clinical Manifestations – extrahepatic bile duct fibrosis Complete obliteration of extrahepatic biliary tree & ducts leading to ductal obstruction. Jaundice >2 Weeks of Birth, Hepatomegaly Biliary Atresia Dark Urine Test Q: How is Biliary Atresia confirmed for Gray, Alcoholic Stools diagnosis? Test Q: Biliary Increased Serum Bilirubin Liver Biopsy Atresia Diagnosis – manifestations? Liver Biopsy = Best Select all. Jaundice, H&P, Lab Findings Alcoholic Stools, o CBC, Bilirubin, Liver Function Tests Increased Bili o Alpha-antitrypsin, TORCH titers, other intrauterine infections Management of BA – Aggressive Nutritional Support – Enteral or TPN Feedings (Low in Na) Test Q: What would the nurse educate the parents on if their Supplement Fat Soluble Vitamins (A, D, E, K) child has Biliary Atresia? Phenobarbital: stimulate bile flow Supplementation of Fat Ursodeoxycholic Acid (Ursodiol): decrease cholestasis, itching, jaundice Soluble Vitamins (A, D, E, K) Surgery: Hepatic Portoenterostomy (KASAI Procedure) o Prognosis: death by 3 years old if untreated; 20% survival with KASAI Procedure; liver transplant o o Esophageal Atresia & Tracheoesophageal Fistula: Esophagus fails to develop as continuous passage; trachea and esophagus fail to separate (rare) Cardiac Anomalies Occur Clinical Manifestations – o Frothy, Saliva Nose & Mouth, Drooling, Choking, Coughing o Cyanotic, Apneic, Respiratory Distress Aspiration of breastmilk or saliva o Stomach Distended by Air, Gastric Contents Regurgitated Broad-Spectrum Antibiotics if there is concern for aspiration of gastric contents Test Q: What is o Polyhydramnios: amniotic fluid swallowed by fetus is unable to polyhydramnios seen in? reach GI tract to be absorbed and excreted by kidneys EA & TEF Result = Abnormal Accumulation of Amniotic Fluid, or Polyhydramnios Treatment – o Maintain Airway, Prevent Pneumonia Test Q: What is the o Gastric or Blind Pouch Decompression infant with EA & TEF o Supportive Therapy at risk for? Select all. When suspected, discontinue all oral intake, initiate IV Tracheomalacia Aspiration fluids, position to facilitate drainage r/t aspiration of TPN Feeding Final Exam Review Pt. 2 32 secretions. Double lumen catheter on intermittent or continuous low suction. Give Abx. if concerned for gastric content aspiration o Surgical Repair Depends on early diagnosis before complications occur and the presence of severity of associated anomalies and illness factors, including PTB. Pre-Op: Carefully suction, position for drainage Blind pouch kept empty by suction G-Tube and Irrigations with Fluids CONTRAINDICATED before surgery in infant with distal TEF Post-Op: Thermoregulation, Tracheal Suctioning Catheter on Low-Suction or Gravity Drainage Test Q: What nutritional TPN Provided support will an infant o Gastrostomy Tube Gravity until need post-op TEF feedings are tolerated repair? TPN Pain Management Observe Initial Oral Feedings o Sterile Water Frequent, Small Feeding of Breastmilk/Formula o May need to supplement by bolus or continuous feeds o Discharge when tolerated Complications – o Tracheomalacia: weakening of tracheal wall r/t dilated proximal pouch compressing the trachea in early fetal life S/S: barking cough, stridor, wheezing, recurrent respiratory infections, cyanosis, apnea Nursing Care Management – o Major Concern: Patent Airway, Prevention of Respiratory Compromise o OG feeding Tube ABDOMINAL WALL DEFECTS o Gastroschisis: Bowel herniates through defect in abdominal wall on right side of umbilicus; intestines outside of body in utero, peritoneal sac NOT present Test Q: Match Gastroschisis and Complications – Omphalocele. o simple or complicated; bowel atresia, perforation, ischemia, Herniation is to the right of the necrosis umbilicus; peritoneal sac is not Management – present. Cover exposed bowel with bag/transparent gauze (SILO BAG): reduced Gastroschisis Abdominal contents herniate over days to weeks depending on damage through umbilical ring, with intact IV Fluids & IV Antibiotics Test Q: What is the nurse’s priority peritoneal sac. Double Lumen NG Tube: Decompression when a neonate is born with Omphalocele gastroschisis? cover exposed bowel with transparent or moist sterile gauze (silo bag) Final Exam Review Pt. 2 33 Test Q: Nutritional education for post-op gastroschisis repair? prolonged TPN until normal bowel function, could be days to weeks o Test Q: Matching GI Disorders. Failure of lateral folding of abdominal wall; covering liver, bowel, and intestines Test Q: GI Matching. Hernia o that cannot be reduced manually, fusion of umbilical cord incomplete. Umbilical Hernia o 2-3x Maintenance Fluids: Replacement THERMOREGULATION Simple = Surgery Immediately o Post-Op: Mechanical Ventilation (abdominal pressure) Pain Management: Morphine, Fentanyl Prolonged TPN Days Weeks for Normal Bowel Function Omphalocele: True failure of embryonic development; failure of lateral folding of abdominal wall @ 3rd week gestation; covered by translucent sac Includes bowel, maybe liver o associated with other anomalies Test Q: What should the nurse prepare for with a Management of Omphalocele – pt. post-op omphalocele Nonadherent Dressing Over Defect repair surgery? IV Fluids & Antibiotics TPN, Mechanical Double lumen NG/OG: decompression Ventilation Sac Resected/Reduced o Post-Op: May Need Mechanical Ventilation & TPN Feedings Resumed: once bowel function resumes Umbilical Hernias: Common, affects premature babies and low birth weight newborns Rarely a constricted hernia that cannot be reduced manually; occurs when fusion of the umbilical ring is incomplete at the point where the umbilical vessels exit the abdominal wall Affects premies and LBW newborns, usually resolves by 3-5 years Elective Surgery if not resolved Nursing Management – Appearance may be disconcerting to parents, reassure that the defect is usually not harmful Taping or strapping the abdomen to flatten the protrusion does NOT aid in resolution and can produce skin irritation; educate parents Observe for Hematoma or Infection Child may resume normal diet and activity post-op o Strenuous Activity Restricted 2-3 Weeks Inguinal Hernia: Peritoneum precedes testicles into scrotum in boys; round ligament into labia in girls (80% of Childhood Hernias – Boys 6:1) Usually asymptomatic unless the abdominal contents are forced into the patent sac, most often associated with painless inguinal swelling If herniated loop becomes obstructed, symptoms may include: irritability, tenderness, anorexia, abdominal distention, and difficulty defecating Emergency Surgery for Incarcerated (constricted); elective otherwise o Post-Op: keep incision dry and clean, remove wet diapers ASAP Final Exam Review Pt. 2 34 o No restrictions placed on infants or toddlers, but older children should be advised against lifting, pushing, wrestling, bike riding, and sporting events for 2-3 weeks. If surgery is postponed, parents should be educated on s/s of incarcerated hernia, simple measures to reduce it (warm bath, avoid sitting in upright position, comfort measures to reduce crying) and when to call for assistance. Cleft Lip & Cleft Palate: o Incomplete fusion of the oral cavity or palates in utero d/t genetic or environmental factors (alcohol, drugs, smoking, anticonvulsants, steroids, retinoids) Folic Acid = PREVENTION Cleft Lip: failure of the maxillary process to fuse with nasal elevations which occurs in the 6th week of gestation correction at 2-3 months old; must be free from infection Cleft Palate: midline defect that may vary in severity, from the soft palate to the Test Q: Why is Cleft Palate hard palate. Occurs from failed fusion of secondary plate, which takes place corrected at 6-12 months of age? between 7-12 weeks of gestation. early repair restricts skeletal growth and delayed repair correct from 6-12 months old results in speech disorders o early repair restricts skeletal growth and delayed repair increases speech disorders Post-Op: Test Q: What is the main Monitor Integrity (Infection) – Protect Operative Site focus of post-op care of Test Q: What would the o Elbow Restraints cleft palate repair? nurse identify as a need Position Upright/On Back Protect Operative Site for further education Clean Incision: NS, water, or diluted hydrogen peroxide following surgical repair of CP? IV Fluids & Clear Liquids 24 Hours “my child must use a No Straw, Tongue Depressor, or Sippy Cups straw to drink liquids” Test Q: Pain management Observe for Airway Obstruction & Hemorrhage for pt. in immediate post-op o Observe Vitals & O2 following CP repair? Pain Management: Opiates (1st 24 hours) Opiates 1st 24 hours o Acetaminophen Antibiotic Ointments: 3 Days on Suture Line Management – additional surgeries, ortho, speech therapy, audiology, social work, etc. o Encourage Breastfeeding Position Upright, Burp Frequently, Special Bottle (oneway valve, special nipple), Syringe Feed if Necessary o Weekly Weight Checks o Require Cheek Support Squeeze checks together o NOISY FEEDERS; Assure parents this is normal Indication the infant needs to stop feeding for a brief moment: facial signal, elevated eyebrow, wrinkled forehead, watery eyes Final Exam Review Pt. 2 Feedings – o NG/OG Tubes: through nose or mouth, left in place or removed after feed Gavage, Continuous, or Medication Administration Check Placement X-Ray then pH Test (<5.5) o NGT Tubes: placed through nose or mouth to the jejunum/duodenum High Risk Aspiration or Regurgitation Must X-Ray Before Use ONLY Continuous Feeds o Gastrostomy Tubes: if tube unable to pass mouth, pharynx, esophagus, or cardiac sphincter; long term tube feeding through abdominal wall to stomach General/Local Anesthesia Clean with Soap & Water Daily No Check for Placement o Parenteral Nutrition (TPN): provides total nutritional needs; filtered to remove particulate matter IV Infusion of Highly Concentrated Protein, Glucose, Nutrients Central Line if Dextrose >13% Test Q: Considerations with Peripheral Line if Dextrose <13% TPN? Give Dextrose >13% in Management – Central Line, and Dextrose New Bag/Tubing q24 hours <13% in Peripheral Line 2 Nurses Sign Off High Risk for IV Infection 35 Test Q: What should be assessed in a pt. who is receiving TPN? IV Site and Glucose Final Exam Review Pt. 2 Final Exam Question 36 ACES & MALTREATMENT 9 questions with Social & Culture ACEs: Adverse Childhood Experiences caused by toxic stress (constant production of cortisol) and has long term health effects into adulthood o Persons who have experienced ACES had 4 to 12-fold increased health risks for alcoholism, drug abuse, depression, and suicided. Increased risks for smoking, poor selfrelated health, increased sexual partners, STIs, physical inactivity, severe obesity. o Women and Minorities = Highest Risk for ACEs Categories – o Abuse: emotional, physical, sexual o Neglect: emotional, physical o Household Challenges: mother treated violently, substance abuse, mental illness, etc. o Other: peer victimization, dating violence, loss of parent, community violence, trauma, war, poverty Risk Factors – o Family/Individual: low income, low education, high parenting/economic stress, inconsistence discipline, negative communication styles, acceptance of violence o Community: High rates of violence, high unemployment, high poverty, low community involvement, food insecurity, unstable housing Protective Factors – o Family/Individual: families with safe/nurturing relationships, good performance in school, positive peer relationships, positive adult role models outside of the family, basic needs met, engaging in fun family activities, o Community: safe/stable housing, good daycares & preschools, violence not tolerated, community involvement Preventing ACEs – Test Q: True or False – o Strengthen Economic Support to Families promoting social norms to o Promote Social Norms to Protect Against Violence/Adversity protect against o Ensure Strong Start for Children violence/adversity is a factor of o Teach Skills preventing ACEs. True o Connect Youth to Caring Adults/Activities o Intervene to Lessen Immediate & Long-Term Harm Raising Awareness of ACEs – Final Q: What is considered o CHANGE How People Think About Causes and Preventions maltreatment? o SHIFT Focuses from Individual Responsibility to Community Solutions emotional, o REDUCE Stigma Around Seeking Help physical, and o PROMOTE Safe and Nurturing Relationship & Environments sexual abused emotional, Maltreatment of Infants & Children – physical neglect o Maltreatment = physical, sexual, emotional, physical neglect, emotional neglect o Risk Factors – Caregiver: young/uneducated, unrelated partner of child, low income, social isolation, low self-esteem, lack of parenting knowledge, history of abuse Final Exam Review Pt. 2 37 Child: less than 1 years old, unwanted, hyperactive, disabilities, premature Environment: chronic stress, substance abuse, divorce, unemployment, substitute caregivers o Warning Signs – Test Q: Which scenario would make physical evidence Test Q: Which are indications the nurse suspect vague/changing history of parental anger? maltreatment? other injuries parents who are vague/changing delay in seeking care, inappropriate responses unreactive to child’s injuries story of injury o Findings of Maltreatment – Physical Neglect: FTT, lack of hygiene, frequent injuries, delay in seeking healthcare, dull affect, school absences, self-stimulating activities Emotional Neglect + Abuse: FTT, eating disorder, enuresis, sleep disturbances, Test Q: A child has come in self-stimulating behaviors, withdrawal, developmental delay, suicide for CHD. Which of the Test Q: Which of the attempts following would indicate following would be child abuse? Physical Abuse: bruises in various stages of healing or nonmobile most indicative of unexplained burns to the child abuse? child, multiple fractures in different stages, burns, lacerations, fear of neck and back Bruises in various parents, lack of emotional response stages of healing Sexual Abuse: bruises, lacerations, bleeding of genitalia, anus, or mouth; STDs, UTIs, difficulty walking/standing, regressive behavior, withdrawal, sexually explicit language inappropriate for age or development, unusual body odor, bloody/torn underwear Caregiver Behaviors with Emotional Neglect/Abuse – o Rejection, Terrorizing Child o Ignoring Child, Verbally Assaulting o Pressuring Excessively Shaken Baby Syndrome – Infant Abuse o Forcibly shaken from excessive crying; blow to head, fist or object May not be seen until severe o Findings – Early Normal Exam Vomiting, Poor Feeing, Respiratory Distress, Retinal Hemorrhages, Seizures, Posturing, Alterations in LOC, Apnea/Bradycardia, Blindness, Unresponsiveness o Nursing Care – Full Assessment for Other Injuries, NOTIFY AUTHORITIES Remove Child from Care of Abuser Make Clear/Objective Notes About Physical Findings Honest, Direct, and Professional Provide Support for Child & Parent Post-Traumatic Stress Disorder (PTSD): children with ACE’s & maltreatment are high risk; caused by traumatic incident, repeated trauma, disorder, natural disaster, sexual abuse, etc. o Initial Response: few min. to 2 hrs; increase in stress hormones (fight/flight), psychosis o Second Phase: lasts about 2 weeks, period of calm (numbness, denial), defense mechanisms decrease o Third Phase: extended about 2-3 months, get worse; depression, phobias, anxiety, conversation reactions, repetitive movements, flashbacks/obsessions o Nursing Care – Referral to appropriate services, monitor behavioral changes, assist family with coping, allow expression of feelings, prevent long term effects Final Exam Review Pt. 2 38 SOCIAL, CULTURAL, RELIGIOUS, & FAMILY INFLUENCES 9 questions with ACEs Family System Theory o Family System: a change in one, affects entire family dynamic – can initiate and react to change; too much or too little change can cause dysfunction o Rapid Periods of Growth/Changes Periods of Stability Test Q: Define Strengths: works for normal family, family with dysfunction or pathology, Family System families of varying structure or stages of lifestyle Limitations: more difficult to determine cause & effect Applications: mate selection, courtship, family communication, boundary maintenance, power & control o Family Stress: family cope with and responds to stressors with wide range of responses and effectiveness Strengths: predict family behaviors and develop interventions, focuses on positive contributions, used by many disciplines Limitations: not certain if combo of resources and coping are applicable for all Applications: transitions in family Developmental Theory – o Stage 1: marriage & independent home; couple identity, realign relationships with extended family, parenthood decisions o Stage 2: families with infants; integrate into family, new parenting/grandparent roles, maintain martial bond o Stage 3: families with preschoolers; socialize children, adjust to separation o Stage 4: families with school children; develops peer relationships, parents adjust to peer and school influences on child o Stage 5: families with teenagers; autonomy, midlife marital/career issues, parents shift concern to older generation o Stage 6: families as launching centers; independent identities, renegotiate marriage o Stage 7: middle aged families; reinvest in couple identity, disabilities/death of grandparents o Stage 8: aging families; from work role to leisure and retirement, maintain couple and individual functioning and adapt to aging process Family Structure – o Traditional: married couple with ONLY biological children Test Q: Child lives with o Nuclear: 2 parents [don’t have to be married] & their children her mother, 2 biological o Blended: at least one step parent, step sibling, or half-sibling siblings, and step-father. o Extended: at least one parent, one or more children, or one or more members; other What family structure is than a parent or sibling this? Final Q: Child lives with her Blended o Binuclear: parents continue role while ending spouse role grandmother, biological o Polygamous: multiple wives brother, and her mother. What is the family structure? o Communal: cult Extended o LBGTQ: same sex parents Parenting Styles – o Authoritarian: try to control child with unquestioned mandates o Permissive: exerts little or no control over child, rarely punishes o Democratic/Authoritative: combo of authoritarian & permissive. Discuss reasons for rules and negatively reinforce deviations. Rely on guilt & shame. o Passive: parent uninvolved with discipline at all; child in control Final Exam Review Pt. 2 39 Parenting & Divorce o Process: Acute: decision to separate; several months to more than a year; family stress and chaotic atmosphere Transitional: family assumes unfamiliar riles with new family structure; larger share of economic burden and altered parent-child relationships. Test Q: What age child Stabilizing: post-divorce family reestablishes a stable, functioning family would most likely blame o Impact: themselves for their Infancy (0-2): eating, sleeping, elimination disturbances & parental attachment parent’s divorce? Early PreK (2-3): blames self, fear of abandonment, regressive behaviors 3-year-old Later PreK (3-5): fear of abandonment, responsible for divorce and interpret as punishment, increased aggression, fantasy Test Q: Children may feel they Early School Age (5-6): depression, immature behavior, sleep disturbances, loss are responsible for their parents’ of appetite, anxiety, may be able to verbalize feelings divorce and interpret the Middle School Age (6-8): panic reactions, deprivation, sadness, depression, fear, separation as punishment. At what age is this most likely to insecurity, fear of abandonment, desire for reconciliation, impaired capacity to occur? enjoy playing, altered peer relationships, decline in school 4 years Later School (9-12): more realistic, intense anger, decline in school, revenge, loneliness, rejection and abandonment, loyalties, aberrant activities Adolescence (12-18): able to disengage from conflict, profound sense of loss of family/childhood, anxiety, withdrawal Types of Discipline to Minimize Misbehaviors – o Reasoning: Older Children o Scolding: Shame & Criticism o Behavior Modification: Reward Good Behavior, Ignoring Negative Behavior o Time Out Test Q: Which of the following o Corporal: Physical Punishment (after family) is most likely to have not effective long term the greatest influence on providing continuity between generations? Forces to Use When Implementing Discipline – Schools o consistency, timing, commitment, unity, flexibility o planning, behavior orientation, privacy, termination Sociocultural Influence of Families – Final Q: Which surrounding o Surrounding Environment environment is an School Connectedness: important site of health promotion important site for Peer Culture health promotion in Social Roles Influenced by Community children? Test Q: Parents of School o Local Community Influences dying child are anxious o Social Determinants Test Q: Most violence, & upset because they substance abuse, Race, Ethnicity can’t find a priest for unrealistic body images o Social Class last rights. What is the come from: o Religious & Traditional Influences nursing diagnosis? Mass Media o Mass Media Influences Cultural Traditions for Health – o Physical Aspects of Caring for Body special clothes, food, medicine o Feelings, Attitudes, Rituals, Actions r/t Health o Spiritual Aspects of Health identity, customs, prayers, healing Final Exam Review Pt. 2 Health Beliefs & Practices – o Natural o Supernatural o Imbalance of Forces o Health Protection folk healers’ practices & remedies faith healing religious rituals 40 Test Q: Pt. thinks God will heal their child with no other medical help. Nurse on shift makes a derogatory comment. What should you include in your next statement? something to help the patient cope, promote comfort, respect cultural beliefs