EKG Presentation: Cardiac Cycle, Rhythm, and Interpretation
advertisement

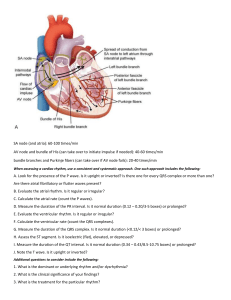
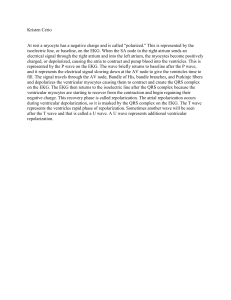
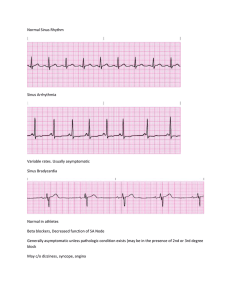
EKG 2018 Michael Weigner, MD, FACEP Learning Objectives • Describe the electrical pathways of the heart as they relate to the cardiac cycle • Describe how an EKG is obtained • Describe the various components of an EKG as it relates to the cardiac cycle • Understand how to determine rate on an EKG • Understand how to read the rhythm on an EKG • Understand all forms of blocks on an EKG • Understand how axis is read on an EKG • Understand how hypertrophy is read on an EKG • Understand how ischemia and infarction are read on an EKG • Describe how an EKG is interpreted in special and miscellaneous circumstances • If it is in Dubin OR on a power point slide OR if I discuss it in lecture it may be tested. • You must read and understand Dubin • All of it • You must listen to and watch my lectures • Being present is best • You must ask questions • You must practice The majority of concepts and images are taken from Dubin What is an EKG • Tracing of the electrical activity of the heart. • Recorded on standard graph paper • Usually 12 tracings (12 lead EKG) • Different but similar to a rhythm strip • Different from a monitor • EKG • Rhythm Strip • Monitor What is an EKG measuring • Electrical activity of the heart • As a cell depolarizes from a negative charge to a positive charge, it contracts • EKGs measure this wave of depolarization • The actual contraction is not directly measured • By placing electrodes around the heart, we can obtain tracings from different directions • As the wave of depolarization moves towards the electrode, it deflects the tracing in a positive direction • If a wave is moving away, it deflects negative • Depolarization is abrupt, causes the contraction • It is a wave of positive (Na+) ions • Repolarization is more gradual • Repolarization is a resetting of the electrical potential • As the electrical waves move through the heart, electrodes record them • The electrical waves move in a predictable way • By placing electrodes strategically we can take advantage of this • By noting differences from normal we can gain valuable insight into heart function and pathology Sinus Node SA Node Sinus-Atrial Node Bundle of His Left Bundle Branch (LBB) Atrial-Ventricular Node AV Node Anterior and Posterior Fascicles not visualized Right Bundle Branch (RBB) Purkinje Fibers Dubin’s schematic, used in the rest of his text • Morphology of a tracing • Must know all these terms • And how they relate to the cardiac cycle • Atrial Depolarization and thus Contraction is recorded at a P wave • It is positive, as it is moving towards electrode • It is slurred, as it advances like ripples in a pond • The AV valves electrically insulate the ventricles from the atria • The only way electricity gets from the atria to the ventricle (usually) is the AV Node and the Bundle of His • The AV node s-l-o-w-s down the wave of depolarization • Thus the pause • This is the PR segment • The wave of depolarization slows in the AV node, but once it reaches the Bundle of His it very rapidly conducts down it and both Bundle Branches and into the terminal Purkinje Fibers • This allows near simultaneous depolarization and thus contraction of both ventricles • This very rapid depolarization causes the QRS complex • It is larger as there is more ventricular mass than atrial mass • The Purkinje Fibers end in the endocardium- thus the wave of depolarization goes from the inside to the outside of the ventricle • ST segment is flat and is the beginning of repolarization • T wave is ventricular repolarization • Atrial repolarization is buried in the QRS complex • Ventricular contraction begins at depolarization (QRS complex) and lasts through repolarization (T wave) • This is the QT interval Moving to Recording • Measured in one millimeter blocks • Horizontal is time • Vertical is both amplitude and direction Positive • Deflection is the direction from the baseline • This is read at positive or negative • Amplitude is the magnitude of deflection • It is an abstract measure of voltage • Read as millimeters Negative • Each heavy black line is 0.2 seconds • Each mm is 0.04 seconds • You can measure the time a portion of the cardiac cycle takes. • This can be manual or the computer can do this for you • The PR interval is 0.16 sec • The QRS is 0.08 sec OK So why 12 leads Chest Leads Horizontal Plane Limb Leads Vertical(Frontal) Plane 3 Limb Leads • By changing the charge of the three electrodes you can get a different angle + Vector • Now, instead of going from negative to positive in two leads, the positive lead is paired with both other leads which are negative • AVF (left foot) is positive, so AVR (right arm) and AVL (left arm) are both negative - - All 3 together AVR is strange, only limb lead that goes to the right 6 Chest Leads • Setting the chest or ‘anterior’ leads up this way allows for a progression of angles and thus morphology of complexes • Lateral Leads • Inferior Leads • Anterior and Septal Leads Rate • Normal is 60-100 • Basically count over time • Pulse and EKG rate not always the same • We usually mean QRS when we talk about rate, but we can also calculate the P wave rate • Computer not always right • Rate is constantly changing • Normal Sinus Rhythm (NSR): • Rate 60-100 • SA node drives rate • P waves all the same morphology • P wave for every QRS • QRS for every P wave • Sinus Bradycardia is when the SA node sets the rate below 60 • Sinus Tachycardia is when the SA node sets the rate above 100 Fast way to determine rate (roughly) QRS Complex Practice • Pick a QRS that falls on a heavy black line • Count 300 150 100 75 60 6 Second Strip Method • Count number of cardiac cycles in 6 seconds • Multiply by 10 Practice • 6 second strip • 4+ cardiac cycles • x10 • HR is just over 40 • Really? Rhythm- Arrhythmias of focal origin • Normal Sinus Rhythm: • P waves all the same morphology • Distance between beats all the same • Rate is 60-100 • P wave with every QRS • QRS with every P wave Sinus Arrhythmia • SA node rate varies with respiration • This is normal • May be pronounced • Sometimes the rate may be set from areas of the heart that are not the SA node • May be in atria or ventricle • May occur in conjunction with the SA or other ectopic foci • The rate alone may provide clues as to the origin of areas of automaticity • Atrial 60-80(100) • AV Junction 40-60 • Ventricles 20-40 • The highest rate will suppress lesser areas of automaticity • Morphology helps with this also Atrial Foci • Each P wave has a QRS • Each QRS has a P wave • Multiple different P waves • COPD • Same as ‘wandering pacemaker’ except rate is over 100 • No P waves • May be normal ventricular rate (Afib with rate control) • May have fast ventricular rate (Afib with RVR or rapid ventricular response) Escape Beats and Escape Rhythm • Escape means there is a pause at the SA node • Then a different area of automaticity takes over • May be atrial, junctional(AV node) or ventricular • Escape beat is one beat then return to sinus • Escape rhythm is continuous with new area of automaticity taking over pacemaking Atrial Escape Beat • Sinus pause • Followed by a single beat that originates from an atrial automaticity focus (P wave looks different) • Followed by return to sinus • Atrial Escape • Abnormal P wave • Rate is 60-80 • QRS is normal Junctional Escape Beat • Sinus pause • Followed by a single beat that originates from a junctional or AV nodal automaticity focus • No P wave • Normal to slightly wide QRS • Followed by return to sinus • Junctional Escape • Rate 40-60 • No P wave • QRS may be wide or look normal Ventricular Escape Beat • Sinus pause • Followed by a single beat that originates from a ventricular automaticity focus • No P wave • Wide QRS • Followed by return to sinus • Ventricular Escape • Rate 20-40 • May have no P waves • May have P waves but don’t conduct • Wide QRS Premature Beats • An irritable focus fires spontaneously • Single stimulus (or it’s a run) • May be rare or frequent • Happens PRIOR to when the next regular beat would occur • Premature Atrial Beat or PAB • Earlier than expected • Has a P wave but it is a different morphology • The ectopic P firing stimulates the SA node also • This resents the SA nodal pacing timing • PAB happens • Usually conduction from the AV node down is normal • Sometimes its not- and the two bundle branches fire separately • Wide QRS • Sometimes the PAB doesn’t conduct past the AV node at all • Dropped (ventricular) beat • Still resets the SA node • Every other beat is a PAB • Every third beat is a PAB • Origin of irritable focus is AV junction • Usually has a partially widened QRS • No P wave prior to QRS • May have bigeminy and trigeminy • The point is MAY cause retrograde atrial contraction • P wave inverted • P wave may be before, during or after QRS PVCs • Premature Ventricular Contraction (PVC) • Large and Wide QRS • Generates a pulse but weaker • Often felt by patients • Pause not due to ‘reset’ of SA node • May actually see an ineffective P wave • The ventricle is refractory for a period of time • Bigeminy and Trigeminy are worrisome • May devolve into Ventricular Tachycardia • Multifocal PVCs are worrisome also • R on T phenomenon • Often leads to Vtach • This is why we synchronize with certain deliveries of electricity Tachy-arrhythmias • Originating from very irritable automaticity foci Paroxysmal (Sudden) Atrial Tachycardia • PAT • Atrial origin • Different foci from SA node- so P waves look different • But… has a P wave • 150-250 • PJT • Slightly wide QRS • Variable retrograde P wave conductionusually buried • Can’t see a P wave • 150-250 • SVT or PSVT • PAT and PJT • 150-250 • Often P waves not appreciated • Really can’t tell if PAT or PJT and implications the same • PVT or VT or V Tach • Very Bad • May have pulseor not • 150-250 • Called VT if sustained • Called a ‘run’ if in and out • Special form of VTach • Atrial rate is different from ventricular rate • Usually both are regular • P waves are regular • ‘sawtooth’ A Flutter • Flutter can be hard to determine • Especially if very fast or 2:1 block • Invert • Vagal • Slow down EKG tracing • Looks like Atrial Fibrillation • Afib and Atrial flutter can look very similar if very fast • Totally unorganized • ‘bag of worms’ • We already talked about Afib • Chaotic atrial foci • No functional atrial ‘kick’ • Ventricular rate is variable and irregular • If ventricular rate is fast, called Afib with RVR (rapid ventricular response) • No organized pumping action of ventricles • No pulse- ever • Coarse VFib • Fine VFib • Asystole Re-entry tachycardia • Accessory pathway Short PR interval • Accessory pathway skips the AV node • Causes short PR interval • Only dangerous when atrial pacing is sped up (A Flutter) Blocks • Sinus Block • A sick SA node drops a beat, then resumes pacing • No P wave • The pause may induce an escape beat • SA node not functional • Lower atrial or junctional foci that would produce escape beats not functional Atrio-Ventricular (AV) Blocks • 1° (First Degree AV Block) • PR > 0.2sec (one large box) • Remains the same beat to beat • Impulse is slowed in the AV node 2° AV Block • Some P waves conduct, and some don’t • 2 Kinds • Wenckebach-AV node • Mobitz-below AV node Wenckebach 2°(Type I) AV Block • AV nodal block • PR progressively lengthens • Until QRS dropped • Cycle repeats • Stable • QRS normal Mobitz 2°(Type II) AV Block • Block below AV node • Regular repeating series • PR interval consistent • Unstable • QRS often partially wide (BBB pattern) Complete or 3° AV Block • Atrial rates and Ventricular rates independent • No atrial impulse makes it past AV node • Automaticity focus in ventricles ‘escape’ • Unstable- bad • Wide QRS • This is not 3° Block as there is no P wave to block • Very bad • May be hyperkalemia Bundle Branch Block (BBB) • Right BBB • RBBB • Left BBB • LBBB • The two bundle branches are out of sync. One transmits the impulse normally and one is slow • Creates a wide QRS (>0.12 sec or 3mm) and two R waves • In RBBB the right bundle is slow • In LBBB the left bundle is slow • Each produces a distinct pattern • The QRS is always wider than 0.12sec RBBB • Wide QRS (>0.12sec) • R R’ in V1 and V2 • ‘Rabbit Ears’ • ‘Buffalo Horns’ • OK, I made that last one up LBBB • Wide QRS (>0.12sec) • R R’ in V5 and V6 • R R’ often hard to appreciate Incomplete (L)BBB • Occasionally you will see an R R’ in an EKG where the QRS is not quite >0.12 sec • “Almost Wide” • May be RBBB or LBBB Hemiblocks • The Left Bundle Branch has an anterior and posterior fascicle • These may be independently blocked • This is call a Left Anterior Hemi-Block (or Left Anterior Fascicular Block • Left Posterior Hemi-Block (or Left Posterior Fascicular Block) • We’ll come back to this after AXIS… AXIS • Represents the direction of electric impulse (Vector) • Begins at endocardium, moves out • Each small vector added together produces a ‘mean vector’ • Always begins at the AV node • Down and to left as the left ventricle is larger • Normal is down and to the left • The mean QRS Vector is described in degrees within a circle drawn on the frontal plane • The Limb Leads define the position of this vector • Called the Axis • If the heart is displaced, so is the mean vector (Axis) • The AV node is always the tail of the vector Right Axis Deviation Left Axis Deviation • Hypertrophy of a ventricle will increase the relative electrical impulse and thus shift the mean vector (Axis) • Can be to left or right • An area of infarct (dead heart- electrically silent) will shift the mean vector (axis) away from the infarcted area • Normal is down and to the left • AV node is always the tail of the vector • We check two leads to check axis I and AVF Lead I • Left arm lead • Measured right through AV node • Positive if vector is to the left (normal) • You’ll remember that the QRS deflects upwards if the wave of positive ions is going towards the electrode • This is normal • If the QRS is upright in lead I, it is normal • If the QRS is downwards in lead I… • If the electrical impulse is going away from lead I (away from the left arm) • The QRS is deflected down • This is Right Axis Deviation Right Axis Deviation • Review AVF • The normal vector in relation to AVF is positive • The QRS is deflected up in AVF in a normal heart • If the vector is (abnormally) pointed upwards • The QRS is deflected down • This is an abnormal axis (usually left axis deviation) • Normal means both lead I and lead AVF are upright • Left Axis Deviation • There is a way to calculate the actual degree of the axis based on the most isoelectric lead • Note that this exists, and that the computer usually does this for you • Don’t need to know how to calculate the exact degree for the test • P wave generally generates an impulse that goes down and to the left • P waves in both I and AVF are therefore positive also • Can calculate axis in the horizontal plane also • V1 and V2 usually downwardly deflected • V5 and V6 usually upwardly deflected • V3 and V4 are isoelectricthis is the transition zone Hemiblocks • Now that that AXIS is understood • Hemiblocks can be discussed • Usually associated with (old) myocardial infarction • Can have more than one block • Moving towards complete heart block • Left Axis Deviation • Normal* QRS • Q1S3 • Q wave in I • S wave in III • This is variable • LAD • Nl QRS • Q1S3 • Right Axis Deviation • Normal QRS • S1Q3 • S wave in I • Q wave in III • variable • RAD • Normal QRS • S1Q3 Hypertrophy • Means thick • Can be seen electrically • V1 directly over atria • V1 best source of information on atrial hypertrophy • P wave is biphasic in V1 if atrial hypertrophy is present • If V1 has a biphasic P wave AND the initial deflection is upwards and larger then right atrial enlargement (hypertrophy) is present • If V1 has a biphasic P wave AND the terminal deflection is downwards and larger then left atrial enlargement (hypertrophy) is present Right Ventricular Hypertrophy • Normal V1 has a large downward deflected S wave RVH • R wave is larger and upward deflection in V1 Left Ventricular Hypertrophy (LVH) • Left ventricular wall thick • Very large QRS complexes • V1 (S wave) is down • V5 (R wave) is up • If S + R = 35mm then LVH • The topics of Acute Coronary Syndrome (clinical presentation, treatment, etc) are discussed in their own lectures • We are limiting ourselves to the EKG implications • Knowing the coronary arteries is important • Knowing the areas of the heart corresponding to the coronary arteries is important • Knowing which EKG lead corresponds to which area of the heart to which coronary artery is important • In general, its all about the Left Ventricle Electrical activity is altered in area of infarct • RCA: inferior and sometimes posterior wall of left ventricle, Right ventricle and Right Atrium including SA and AV nodes • LCx: high lateral and sometimes posterior walls of left ventricle • LAD: anterior wall and some lateral left ventricle, septum, both bundle branches Common Pathway • Hypoxia (decreased oxygen to tissue) • Ischemia (decreased blood flow from thrombus- moving towards injury) • Injury (acute- about to be dead) • Necrosis (dead-stays dead) Ischemia • May be (new) inverted T wave • May be ST segment depression • Both imply very stressed (hypoxic) myocardium Injury • Acute- happening now • ST segment elevation • This is an active myocardial infarction • STEMI • Infarct does not extend through entire thickness of wall • Looks the same as ischemia • Also looks the same as ‘reciprocal changes’examples to follow Necrosis (Dead) • Q Wave means dead tissue • Must be ‘significant’ • May be new or remote • Anterior Leads • Anterior Left Ventricle • LAD- Left Anterior Descending artery • Lateral Leads • Lateral Left Ventricle • Circumflex Artery • Occasionally from LAD V5 and V6 also • Inferior Leads • Inferior Left Ventricle • Right Coronary Artery • Occasionally from LAD Posterior Infarct Normal Vectors EKG Changes for Anterior MI Q wave, ST elevation R Wave and ST Depression in V1 and V2 • Posterior Leads • Or Inverted Anterior Leads • Posterior Left Ventricle • Circumflex or Right Coronary Artery Posterior Leads • V7, V8, V9 • Under left scapula • Purpose is to look at the posterior wall of the left ventricle • Right sided leads • Look at right ventricle Acute MI in Bundle Branch Block • If OLD LBBB, difficult to determine if acute MI • If new LBBB (some say any new BBB), treat as acute MI • There are very complicated criteria for BBB in context of MI Injury (MI) Mimics: • Ventricular aneurysm • Brugada’s syndrome • Pericarditis Ventricular Aneurysm • Anterior ST elevations • Looks like anterior MI • Hx • Old EKG Brugada’s Syndrome • RBBB • ST elevation V1-V3 • Congenital • Not CAD • Sudden death Pericarditis • Pericarditis EKGs are complicated • ST elevations everywhere Miscellaneous EKG Findings Very Dangerous EKGs • ONE: Brugada Syndrome • TWO: Wellens Syndrome • May be biphasic T waves • High LAD lesion • Leads to Massive Anterior MI THREE: Prolonged QT Syndrome • Hereditary- sudden death in athletes • Acquired- many drugs, especially psychiatric drugs • Electrolytes- Ca++ • Rate dependent • There is a mathematical formula to find the QTc (corrected) • The ½ the cardiac cycle eyeball test is a quick screen COPD- Chronic Obstructive Pulmonary Disease • RAD (I down) • Low amplitude • MAT (multifocal atrial tachycardia) PE- Pulmonary Embolism • Classic is S1Q3T3 • S wave in I, Q wave in III, Inverted T wave in III • Tachycardia • Often RAD • Often RBBB • Often inverted T waves in V1-V4 • This is acute right heart strain • Big PE can cause PEA (pulse electrical activity) • S1Q3T3 • RAD • Inverted T waves V1-V4 • Not RBBB • Not Tachycardic Hyper K+ • Peaked T waves • Hyperkalemia • May widen QRS • May cause blocks • May cause PEA Hypo K+ • Hypokalemia • Flat T waves • U wave Calcium PACERs • Multiple different kinds • Will see a pacer spike • Rest of morphology is then not useful for diagnostic purposes • Pacer takes over when needed • and turns off when not needed • Pacer spike before (and causing) P wave • Normal AV conduction • Normal QRS complex • Can use QRS for diagnosis • Normal P wave • No natural AV conduction • Pacer stimulates ventricles • BBB appearance (wide QRS) • Not useful for diagnosis • Atrium and Ventricles have there own pacer leads • QRS has BBB appearance • Wide QRS • QRS not useful for diagnosis • Advantage of this is preserves atrial ‘kick’ AICD • Automated Implantable Cardiac Defibrillator • Can pace, over drive pace, or defibrillate • Native SA node preserved • Transplanted SA node also present • Two P waves Questions?