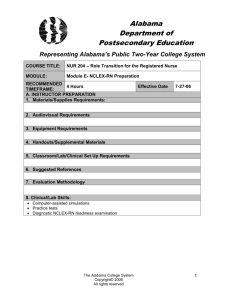
“Becoming a USRN Study guide 2019 Roadmap to NCLEX” 100 m NCLEX-RN study guide Introduction Welcome to RoadMap to NCLEX®. This book is based on the need of Filipino nurses to pass their NCLEX-RN examination and other foreign licensure tests. NCLEX-RN in the United States is a standardized test used to determine competencies for entry level nurses in each state. It is regarded by many as one of the toughest examinations to pass especially for foreign nurses like Filipinos. Working here in the US, I see that one of the reasons behind is that, the exam is not as consistent as what we learned in the Philippines even though we use American references. Simply because we don’t see it in our hospital practice. But in here, it is mostly consistent with what they learn and do. The percentage of passing rate for first time takers, US educated for NCLEX-RN in 2019 is within 86-92% comparing to 47.1% for internationally educated. Filipino nurses are on top of the list for NCLEX-RN takers. Nevertheless, I am driven to bring the gap closer. There is no big difference between me and my co-nurses in the Philippines or elsewhere in terms of passing the NCLEX-RN and be able to practice here in the US, we all can do it. Learning does not stop. It is not as difficult as what you think, just don’t doubt yourself. NCSBN only need an entry level competency to get in. In the Philippines, I am thankful to IPass who has been the instrument of success for many nurses who passed including those who were unsuccessful, “believing” is the key. IPass has been my enabler in making all this possible. The resources from various top of the line review materials such as Saunders, LaCharity, Uworld, online medical information access like Mayoclinic, Medscape, American Heart Association, The Joint Commission, Center for Disease Control, Osmosis and Khan academy videos and the likes, and images from various internet sites. This book is basically a consolidation of these resources put as one, coherent with the trending topics in the NCLEX-RN. In addition, past examinees contributed by gathering information which came out from their exams themselves. These facts are also seen in my workplace as a medical-surgical floor and in other acute hospital settings in general which helped me align NCLEX knowledge into practice. My family, who has been my inspiration all this time. We are family of nurses and educators as well. We believe in the value of education. We survive with persistence, as the saying goes “The river cuts through a rock not because of its power, but its persistence” (James Watkins). Lastly, I believe in blessings and not by luck. God gives us all this blessings, may be in a form of hardships or prosperity. At the end of the day, his plans are greater and he made it beautiful. 1 NCLEX-RN study guide 100 m 7 routes of success 1. Know the NCLEX 7. Destination RN 2. Your Goal 4. Strategies 6. The Day 3. Your Abilities 5. Mastering the “Trends” 2 NCLEX-RN study guide 100 m 1 Know the NCLEX NCLEX is an adaptive testing system. As you answer a question, the computer determines your competency based on the answer you selected. If you selected a correct answer, the computer scans the question bank and selects a more difficult question. If you selected an incorrect answer, the computer scans the question bank and selects an easier question until you meet the PASSING standard or otherwise a failing mark. There are 75 – 265 number of questions and as long as 6 hours to complete the exam. The computer assesses at 75th item, it’s either satisfied or not. If not, then it will continue until 6 hours or 265 whichever comes first. It may stop at any time after 75th item as long as the computer already determines your competency. If you completed the 265 items, last item must be correct otherwise you fail the exam. On the other hand, if you ran out of time, the average of the last 60 items will be assumed as your competency level. It must be at least in line with the minimum competency. 3 NCLEX-RN study guide 100 m The Test Plan Type of questions The NCSBN provides specific directions for you to follow with all question types to guide you in your process of testing. Be sure to read these directions as they appear on the computer screen before you start answering the graded exam. 1. Multiple choice 2. Ordered Response (Place the sequence in order) 3. Select all that apply (SATA) – in SATA you can answer one up to all choices as long as you think it’s the right answer(s) 4. Fill in the blank (usually computations) 5. Drag and drop 6. Hotspot (place the cursor over the area on the diagram that does the selected action) 7. Chart/Exhibit – your answer is based on the chart or exhibit given 8. Graphic Option – showing you pictures or images where you can base your answers 9. Audio – For example lung or heart sounds 4 NCLEX-RN study guide 100 m 2 Your Goal Remember: Pass with 75 questions as much as possible. To pass with 75 questions you will most likely need to answer more difficult and multiple response questions correctly like the BEAST “Select All That Apply.” The key to slay this is to be a master of the content! Don’t panic if you exceeded the minimum 75 item. The goal is to pass the exam, so take a break and relax before you answer the next succeeding questions. In 2012, the average number of items (questions) administered per candidate was around 119 on the NCLEX-RN and 117 on the NCLEX-PN. 3 Your abilities Remember: It’s important to know your strong and weak concepts for you to focus on. It is not good to hope that your weak points would not come out during exam, the secret is focus on your weakness and maximize your strengths. NCLEX® knows how to target weak points by throwing more questions until you hit their standards. 5 NCLEX-RN study guide 100 m 4 ❖ ❖ ❖ ❖ ❖ ❖ ❖ ❖ ❖ ❖ ❖ ❖ Strategies Don’t start being anxious and especially don’t panic! You don’t need to read extra meaning to the question. Look for keywords and phrases to help you understand. Interpret the question correctly first before reading into the choices. Read the stem correctly and notice, is it asking for the best response or the initial response Understand what the question is asking before considering the distracter. Rephrasing technique translates the question into your own words. Isolate choice that is relevant from what is not. Judge all four alternative choices/options against the stem and not against one another. Use the process of elimination, cross out those variables that are incorrect. When you come across a difficult question and you cannot immediately identify the answer, go back to your body of knowledge and draw all the information that you do know about the condition. Even though you do not know exactly what to do, you might know what not to do If one is the exact opposite of another (e.g. complete bed rest is different from activity as tolerated; both cannot be correct since they are of opposites), choose the one that seems to be most logical. 6 100 m NCLEX-RN study guide ❖ If you cannot choose an alternative, use your intuition. Let yourself feel which alternative might be right. Remember, it’s better to choose one answer than none at all. o Do we depend on this “hunch?”(Intuition). Current studies support that hunches are often correct, for they are based on rapid subconscious connections in the brain. ❖ So, if you have an initial hunch, go with it! Do not change the answer if and only if, upon reflection, it just doesn’t seem right. (If you are taking NCLEX®, you can take time as you want, but do not dwell too much.) ❖ Remember, this is a nursing test and questions are designed to test your nursing competency and safety. ❖ It is unlikely that a question would require a medical action for the correct answer; it may, however offer these actions as distracter. ❖ Beware of answers that contain specific qualifiers, such as “always’ and “never,” they rarely fit within a logical framework. ❖ Content is King: “Select all that Apply” (SATA) format questions are very much like a “T & F” quiz you may have taken during nursing school. Unfortunately, there is no short cut to preparing for the SATA questions, a candidate just has to have enough content. 7 NCLEX-RN study guide 100 m 5 Mastering the “Trends” 8 NCLEX-RN study guide 100 m 1 Prioritization and Delegation Considerations in Prioritizing: Remember: Registered Nurses (RN) use “higher clinical judgement skills”. Delegate task that does not use much of your clinical judgment. Do not misuse prioritization approaches for example, CAB (Compression, Airway, Breathing). This is used for basic CPR guidelines. 1. ABCs 1. Airway/Breathing 2. Circulation/CV status 3. Infection/Sepsis 4. Pain/Injury 5. Nutrition/Elimination 6. Knowledge deficit/Anxiety & Fear 7. Other psychosocial prob 2. Acute patients before Chronic ❖ Acute patients will have unexpected symptoms, chronic has expected manifestations and are predictable. 3. Unstable patients before stable ones. Delegate task 4. Consider high vulnerable patients: <2 YO, >65-70 YO, pregnant women, consciously sedated patients. 5. Changing Condition/Deteriorating Ex: Chronic can become acute at any time – Prioritize 9 100 m NCLEX-RN study guide Question: An emergency department nurse is assigned to triage. Which client should the nurse assess first? 1. Five-year-old with a superficial leg laceration 2. Lethargic 3-month-old with diarrhea for the past 12 hours 3. Seven-year-old with an elevated temperature of 101 F (38.3 C) and hematuria 4. Seventeen-year-old with severe, acute abdominal pain Answer: 2 Rationale: 1. Five-year-old with a superficial leg laceration Bleeding/circulation problem but only superficial. Age is 5 YO (non-vulnerable) 2. Lethargic 3-month-old with diarrhea for the past 12 hours Vulnerable patient @ <2 YO, circulation problem, acute and can deteriorate at any time, cannot be delegated, RNs judgment is needed 3. Seven-year-old with an elevated temperature of 101 F (38.3 C) and hematuria Infection is not a priority, age is not vulnerable, stable and can be delegated 4. Seventeen-year-old with severe, acute abdominal pain 2nd priority – could be appendicitis, or ectopic pregnancy that can deteriorate at any time, however the age is not vulnerable. Unless otherwise the patient develops sudden respiratory distress – AIRWAY is a priority. 10 NCLEX-RN study guide 100 m Delegation: General Tasks RN LPN/LVN UAP Assessment Initial/admission Acute/Unstable Patient Stable Patients Follow-up Assessment Special assessment: Lung sounds, Bowel sounds etc. Stable Patients Monitor VS, I/O, Height and weight Care Planning Yes Assist only No Evaluation Yes No No Education Initial & Discharge Reinforce only Reinforce only Documentation Yes Yes Yes Medication All Except IV No Sterile Procedure Yes Yes – Routine Only No Remember: 5 Rights of delegation ▪ right task ▪ right person ▪ right circumstances ▪ right communication/direction ▪ right supervision/evaluation Blood Transfusion: Initial assessment (15 mins) done by RN, Then delegate to UAP. Delegate positioning to UAP: Unless with cervical injury in which RNs must assess respiratory status. Delegate feeding to UAP: CVA patient: first 24-48° should be RN (Risk for Aspiration) PEG tube feeding: LPN/LVN (stoma care is indicated) Remember: RNs and LVNs have professional license. Higher accountability and responsibility is implicated. 11 NCLEX-RN study guide 100 m 2 Nursing Issues Transcultural Nursing Latino Americans ▪ May view illness as a sign of weakness, punishment for evil doing; ▪ May consult with a curandero or voodoo priest ▪ Family members are typically involved in all aspects of decision making such as terminal illness ▪ May see no reason to submit to mammograms or vaccinations. • African Americans ▪ May believe that illness is caused by supernatural causes and seek advice and remedies from faith healers ▪ Family oriented; ▪ Higher incidence of HPN and obesity; ▪ High incidence of lactose intolerance Arab Americans Asian Americans ▪ May value ability to endure pain and grief with silent stoicism; ▪ Typically family oriented; extended family should be involved in care of dying patient; ▪ Believes in “hot-cold” yin/yang often involved ▪ Sodium intake is generally high because of salted and dried foods; ▪ May believe prolonged eye contact is rude and an invasion of privacy; ▪ May prefer to maintain a comfortable physical distance between the patient and the health care provider. ▪ May remain silent about health problems such as STIs, substance abuse, and mental illness ▪ A devout Muslim may interpret illness as the will of Allah, a test of faith; ▪ May rely on ritual cures or alternative therapies before seeking help from health care provider ▪ After death, the family may want to prepare the body by washing and wrapping the body in unsewn white cloth ▪ Postmortem examinations are discouraged unless required by law. ▪ People suffering from chronic illnesses, pregnant women, breastfeeding, or menstruating don’t fast. ▪ Females avoid eye contact with males ▪ Use same-sex family members as interpreters. 12 NCLEX-RN study guide 100 m Native Americans ▪ May turn to a medicine man to determine the true cause of an illness; ▪ May value the ability to endure pain or grief with silent stoicism; ▪ Diet may be deficient in vitamin D and calcium because many suffer from lactose intolerance or don’t drink milk; ▪ Obesity and diabetes are major health concerns; ▪ May divert eyes to the floor when they are praying or paying attention. Western Culture ▪ May value technology almost exclusively in the struggle to conquer diseases; ▪ Health is understood to be the absence, minimization, or control of disease process; ▪ Eating utensils usually consists of knife, fork, and spoon; ▪ Three daily meals is typical. 13 NCLEX-RN study guide 100 m What is HIPAA? HIPAA is the acronym for the Health Insurance Portability and Accountability Act that was passed by Congress in 1996. HIPAA does the following: 1. Provides the ability to transfer and continue health insurance coverage for workers and their families when they change or lose their jobs; 2. Reduces health care fraud and abuse; 3. Mandates standards for health care information on electronic billing and other processes; and 4. Requires the protection and confidential handling of protected health information (PHI) “Under HIPAA, a client's information regarding medical treatment is private and cannot be released without the client's permission. Nurses need to try to reasonably limit use of, disclosure of, and requests for PHI in any given situation.” Remember: Information should be provided only on a "need-to-know" basis. The United States is serious about HIPAA and the citizens know this law very much. Ethical Principles: Autonomy: Patient’s right to decide (consent/refuse) Nonmaleficence: Do no harm to patients Beneficence: To act in the best interest of patient Justice: Fairness/equality of treatment regardless of status Veracity: Truthfulness to patients Fidelity: Loyalty to profession 14 100 m NCLEX-RN study guide Informed Consent and Informed Refusal: Must consist of the following: 1. The HCP MUST clearly explain to the patient Diagnosis Procedure/Surgery Complications involved Prognosis Alternatives 2. The client has indicated understanding of the information. 3. The client is giving voluntary, legal consent for the procedure. Question 1: The health care provider gives the preoperative nurse a signed consent form and walks away rapidly. The client turns to the nurse and states, "I don't know what is going on. Why do I need surgery?" What is the most appropriate action? 1. Call the nursing supervisor 2. Call the operating room scheduler and cancel the surgery 3. Page the health care provider and request clarification on behalf of the client 4. Report the incident to hospital administration Answer: 3 Rationale: Informed consent requires that the health care provider performing the procedure explain everything to the client's satisfaction. Remember: Consent or refusal, patient must be INFORMED and aware. Waiting until the client is awake to obtain consent for a procedure already performed is illegal and would warrant charges of assault and battery. 15 100 m NCLEX-RN study guide Assault: An unlawful act that places another person, without that person's consent, in fear of immediate bodily harm. (Threatening the patient) Battery: A completed assault is a battery Slander: oral defamation False imprisonment: Limiting patient to move (illegal detention) Emancipated Minor: "mature minor" who can give consent. Criteria: ▪ Marriage ▪ In the armed forces, ▪ living apart from one's parents ▪ Financial independence ▪ Pregnancy/parenthood ▪ A court decision Question: The nurse is caring for a 4-year-old child in the emergency department who has a 104 F (40 C) temperature, is obtunded, and has a positive Kernig's sign. The parents are refusing antibiotics and any treatment. The parents state that their religious belief is to trust in just prayer and believe the child will receive divine healing. What action does the nurse anticipate? 1. Assisting the parents in signing Against Medical Advice (AMA) papers 2. Discharging the child if parents have power of attorney papers 3. Notifying the hospital administration about the situation 4. Reassuring the parents that their decision will be respected under the principle of autonomy. 16 NCLEX-RN study guide 100 m Answer: 3 Rationale: Hospital administration will obtain legal protective custody of a minor child if the parents are deciding against life-saving measures for their child or when there is child abuse/neglect. Paternalism - A type of medical decision making in which health care professionals assume over an incapacitated parent of a child with life threatening condition Ethical Dilemma Occurs when there is a conflict between 2 or more ethical principles. Negligence: Is a failure to exercise the care that a reasonably prudent person would exercise. Malpractice: Is a type of negligence, also known as “Professional Negligence” unbecoming of a Professional Nurse. Negligence can be: Commission is care rendered but wrong Omission is never rendered at all Ordinary Negligence: unintentional Gross Negligence: Intentional 17 NCLEX-RN study guide 100 m Patient Abandonment The American Nurse’s Association’s definition of patient abandonment is “a unilateral severance of the established nurse-patient relationship without giving reasonable notice to the appropriate person so that arrangements can be made for continuation of nursing care by others” Criteria: 1. Have first ACCEPTED the client assignment, establishing a nurse client relationship; 2. DISENGAGED the nurse client relationship without giving reasonable notice to the qualified person (supervisor, colleague, etc.) What is Self – Determination Act? A law that indicates clients must be provided with information about their rights to identify written directions about the care that they wish to receive in the event that they become incapacitated and are unable to make health care decisions. Advance Directives Include a living will, which states the medical care that you do and do not want at the end of life, and a health care power of attorney (by proxy), which designates a health care agent to make decisions on your behalf if you are incapacitated. 18 NCLEX-RN study guide 100 m Five Wishes Combining a living will and health care power of attorney in addition to addressing matters of comfort care and spirituality. Wishes 1 and 2: are both legal documents. Once signed, they meet the legal requirements for an advance directive Signed: POA for Proxy: By lawyer(Notary) Living Will: By patient only Lateral Violence Lateral violence (also known as horizontal violence) can be defined as acts of aggression carried out by a co-worker against another coworker and designed to control, diminish, or devalue a colleague. These behaviors usually take the form of verbal abuse such as namecalling, unwarranted criticism, intimidation, and blaming. Remember: Refusing to help someone, sabotage, exclusion, and unfair assignments, also fall under the category of lateral violence. Actions to Take: 1. Confront the bully 2. Validate/Support the colleague 3. Report 4. Document 19 100 m NCLEX-RN study guide Good Samaritan Act Good Samaritan laws protect caregivers from prosecution for medical mistakes, as long as the caregivers are acting in a voluntary manner without any expectation of reward. Remember: Being a rescuer means accountability Most states DO NOT cover acts of “gross negligence” or “willful misconduct”. Gross negligence is generally taken to mean a reckless action that is taken without regard for the safety of others while willfull misconduct is generally considered to be an action that is reasonably likely to cause an injury to another person. For instance, you are rescuing the severely bleeding patient from an injury to his/her hand and you did not apply a direct pressure from a near artery. This is an obvious negligence on the part of the rescuer. 20 NCLEX-RN study guide 100 m 3 Patient Safety Patient Safety Goals The purpose of the National Patient Safety Goals is to improve patient safety. The goals focus on problems in health care safety and how to solve them. 1 Identify patients correctly Use at least two ways to identify patients. Ex: Identifiers ▪ Patient’s Full Name, ▪ Date of Birth ▪ Medical Record Number (most distinct) 2 Improve Effective Communication A. SBAR S: B: A: R: Situation Background Assessment Recommendation/read-back An established reporting format used to communicate with the health care provider (HCP). Use of SBAR ensures that the HCP receives the necessary information to make a clinical judgment regarding treatment or need for immediate assessment. 21 NCLEX-RN study guide 100 m Ex: Place the following report information in the correct order according to the SBAR format. 1. “He is restless and anxious: temperature is 100.3° F (38° C); pulse is 110 beats/min; respiratory rate is 24 breaths/min; blood pressure is 140/90 mm Hg. Abdomen is rigid and tender to touch with hypoactive bowel sounds.” 2. “He had abdominal surgery yesterday. He is on PCA morphine, but he says the pain is getting progressively worse.” 3. “I have tried to make him comfortable and he is willing to wait until the next scheduled dose of pain medication, but I think his pain warrants evaluation.” 4. “Would you like to give me an order for any laboratory tests or additional therapies at this time?” 5. “Dr. S, this is Nurse J. I’m calling about Mr. D, who is reporting severe abdominal pain.” Answer: : 5, 2, 1, 3, 4 5. “Dr. S, this is Nurse J. I’m calling about Mr. D, who is reporting severe abdominal pain.” 2. “He had abdominal surgery yesterday. He is on PCA morphine, but he says the pain is getting progressively worse.” 1. “He is restless and anxious: temperature is 100.3° F (38° C); pulse is 110 beats/min; respiratory rate is 24 breaths/min; blood pressure is 140/90 mm Hg. Abdomen is rigid and tender to touch with hypoactive bowel sounds.” 3. “I have tried to make him comfortable and he is willing to wait until the next scheduled dose of pain medication, but I think his pain warrants evaluation.” 4. “Would you like to give me an order for any laboratory tests or additional therapies at this time?” B. Verbal & Telephone Orders Verbal Order is order received through face to face interaction during emergency situation. 22 100 m NCLEX-RN study guide Telephone Order is taken when physician is not present & communication is over the telephone. Remember: The nurse “writes down and reads back “ the information to confirm the telephone order. Verbal order must be “repeated/read back” to the ordering physician before proceeding. C. Approved and Unapproved Abbreviation 23 100 m NCLEX-RN study guide Question: Which medication order for a client with a pulmonary embolism is most important to clarify with the prescribing physician before administration? 1. Warfarin (Coumadin) 1.0 mg by mouth (PO) 2. Morphine sulfate 2 to 4 mg IV 3. Cephalexin (Keflex) 250 mg PO 4. Heparin infusion at 900 units/hr Answer: : 1 Remember: Use of “Trailing Zero” e.g. 1.0 mg might be misinterpreted as 10 mg. Use of “Preceding Zero” is allowed, e.g. 0.1 mg. Whereas writing .1 can be interpreted as 1 or 11. D. Report critical results of tests and diagnostic procedures on a timely basis. Critical results of any tests and diagnostic procedures fall significantly outside the normal range and may indicate a life threatening situation. The objective is to provide the responsible licensed caregiver these results within an established time frame so that the patient can be promptly treated. Remember: Most institution requires 30 minute timeline from communicating until treatment. 24 NCLEX-RN study guide 100 m 3 2 Use Medicines Safely A. High Alert Medications (HAM) Drugs that bear a heightened risk of causing significant patient harm when they are used in error. How to reduce errors: ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ Standardizing the ordering Storage Preparation and administration Improving access to information about these drugs Limiting access to high alert medications; Using auxiliary labels Employing clinical decision support and automated alerts Using redundancies such as automated or independent double checks when necessary. Example in drug calculations, “I check, you check separately, then compare answers”. Memorize at least this mnemonic! PINCH P: Potassium Chloride I: Insulin N: Narcotics, Neuromuscular blocking agents (muscle relaxants) C: Concentrated electrolytes (>0.9% NaCl) H: Heparin and other anticoagulants, thrombolytics Remember: All forms of insulin, subcutaneous and IV, are considered a class of high-alert medications. Insulin U-500 has been singled out for special emphasis to bring attention to the need for distinct strategies to prevent the types of errors that occur with this concentrated form of insulin. 25 NCLEX-RN study guide 100 m 4 2 Use Alarms Safely Remember: Make improvements to ensure that alarms on medical equipment are heard and responded to on time. 5 2 Prevent Infection A. STANDARD PRECAUTION Standard Precautions include a group of infection prevention practices that apply to all patients, regardless of suspected or confirmed infection status, in any setting in which healthcare is delivered. 1. Hand hygiene 2. Use of personal protective equipment (e.g., gloves, masks, eyewear) 3. Respiratory hygiene / cough etiquette 4. Sharps safety 5. Safe injection practices 6. Ensure appropriate patient placement 7. Handle textiles and laundry carefully 8. Clean and disinfected, instruments, devices and environmental surfaces Hand Hygiene Remember: Handwashing: When hands are visibly soiled, use soap and water for 40-60 seconds Hand rubbing: When hands are not visibly soiled, use alcohol based hand rub for 20-30 seconds 26 100 m NCLEX-RN study guide Moments of Hand Hygiene Personal Protective Equipment PPE: Gloves, masks, eyewear/goggles, gown PPE Donning 1. 2. 3. 4. Hand hygiene Gown Mask or respirator Goggles/face shield 5. Gloves 27 NCLEX-RN study guide 100 m PPE Removal 1. 2. 3. 4. 5. Gloves Goggles/face shield Gown Mask or respirator Hand hygiene Respiratory hygiene/cough etiquette Measures to contain respiratory secretions: Recommended for all individuals with signs and symptoms of a respiratory infection. 1. Cover your mouth and nose with a tissue when coughing or sneezing; 2. Use in the nearest waste receptacle to dispose of the tissue after use; 3. Perform hand hygiene Healthcare facilities should ensure the availability of materials for adhering to Respiratory Hygiene/Cough Etiquette in waiting areas for patients and visitors. 1. Provide tissues and no-touch receptacles for used tissue disposal. 2. Provide conveniently located dispensers of alcohol-based hand rub; where sinks are available, ensure that supplies for hand washing (e.g. soap, disposable towels) are consistently available. 28 NCLEX-RN study guide 100 m Sharps safety Remember: ▪ Fish hook technique ▪ No bending of needles ▪ Dispose container at ½ or 2/3 full Needlestick injury: Things to do 1. Remove gloves 2. Wash area with soap and water 3. Notify the nurse's supervisor 4. Go to employee health clinic 5. Take post-exposure prophylaxis Disinfection Hospital-approved antiseptics: ▪ ≥ 0.5% chlorhexidine with alcohol (most effective) ▪ 70% alcohol pads ▪ ≥10% povidone-iodine Catheter Ports: The nurse should scrub the Foley collection port with alcohol or chlorhexidine solution for 15 seconds before withdrawing a specimen Invasive Lines: The nurse should "scrub the hub" with alcohol or chlorhexidine/alcohol for 1015 seconds. This should be done before flushing, drawing blood, or administering medication. Chlorhexidine is preferred over povidone-iodine: It achieves an antimicrobial effect within 30 seconds whereas povidone-iodine takes ≥2 minutes. 29 NCLEX-RN study guide 100 m B. TRANSMISSION BASED PRECAUTION Transmission-Based Precautions are the second tier of basic infection control and are to be used in addition to Standard Precautions for patients who may be infected or colonized with certain infectious agents for which additional precautions are needed to prevent infection transmission. Contact Precautions for patients with known or suspected infections that represent an increased risk for contact transmission Droplet Precautions for patients known or suspected to be infected with pathogens transmitted by respiratory droplets that are generated by a patient who is coughing, sneezing, or talking Airborne Precautions for patients known or suspected to be infected with pathogens transmitted by the airborne route (e.g., tuberculosis, measles, chickenpox, disseminated herpes zoster) 30 NCLEX-RN study guide 100 m CONTACT precaution guidelines: Ensure appropriate patient placement. Acute care hospitals - single patient room if available Use personal protective equipment (PPE) appropriately Gloves and Gown - Wear a gown and gloves for all interactions that may involve contact with the patient or the patient’s environment. Limit transport and movement of patients. When transport or movement is necessary, cover or contain the infected or colonized areas of the patient’s body. Use disposable or dedicated patient-care equipment (e.g., blood pressure cuffs). If common use of equipment for multiple patients is unavoidable, clean and disinfect such equipment before use on another patient. Prioritize cleaning and disinfection of the rooms at least daily or prior to use by another patient if outpatient setting focusing on frequently-touched surfaces and equipment in the immediate vicinity of the patient. Remember: Mnemonic is Mrs. Wee M – Multi drug Resistant Organisms: ▪ MRSA (Methicillin resistant staph. aureus) ▪ VRSA (Vancomycin resistant staph. aureus) ▪ VRE (Vancomycin resistant enterococcus) ▪ ESBL (Extended spectrum beta lactamase) ▪ KPC (Klebsiella Pneumoniae Carbapenemase) 31 NCLEX-RN study guide 100 m R – Respiratory Infections: ▪ RSV (Respiratory syncytial virus – Viral Croup in children or bronchiolitis) Contact and droplet S – Skin Infections: ▪ Skin diphtheria ▪ Herpes simplex disseminated type ▪ Herpes zoster (shingles) disseminated type & Chicken Pox (varicella zoster) Contact and airborne ▪ Impetigo ▪ Lice/Pediculosis (Head only) ▪ Scabies ▪ Small Pox (Variola) Contact and airborne W – Wound Infections: ▪ Major Staphylococcal disease (S. aureus) Skin, wound, or burn Major Draining abscess E – Enteric Infections: ▪ Clostridium difficile ▪ Norovirus ▪ Rota Virus ▪ Hepatitis A (Diapered or incontinent patients) E – Eye Infections: ▪ Conjunctivitis Acute viral (acute hemorrhagic) DROPLET precaution guidelines: Source control: put a mask on the patient. Ensure appropriate patient placement Acute care hospitals: in a single room if possible. Use personal protective equipment (PPE) appropriately. Don mask upon entry into the patient room or patient space. 32 NCLEX-RN study guide 100 m Limit transport and movement of patients outside of the room to medically-necessary purposes. If transport or movement outside of the room is necessary, instruct patient to wear a mask and follow Respiratory Hygiene/Cough Etiquette. Droplets are large and travel less distance (3 feet and then fall) Keep a distance of 3 – 6 feet when possible (3 – 6 ft rule) Patient’s door can stay open. No special ventilation is required. Remember: Mnemonic is SPIDERMAN S - Scarlet Fever/Streptococcal pharyngitis, Streptococcal Pneumonia P - Parvovirus B19 (5th Disease/Erythema Infectiosum), Pertussis, Pneumonic Plague (Yersinia pestis) I - Influenza D- Diphtheria (pharyngeal) E - Epiglottitis (Hemophilus Influenza Type B – HIB/Bacterial Croup) R - Rubella (German Measles), Rhinovirus, RSV (Respiratory syncytial virus aka Viral Croup in children or bronchiolitis Contact and droplet M - Mumps, Meningitis (Bacterial), Mycoplasmal Pneumonia An - Adenovirus Pneumonia Contact & droplet AIRBORNE precaution guidelines: Source control: put a mask on the patient. 33 100 m NCLEX-RN study guide Ensure appropriate patient placement in an airborne infection isolation room (AIIR) Restrict susceptible healthcare personnel from entering the room of patients known or suspected to have measles, chickenpox, disseminated zoster, or smallpox if other immune healthcare personnel are available. Use personal protective equipment (PPE) appropriately: fit-tested NIOSH-approved N95 or higher level respirator for healthcare personnel. Limit transport and movement of patients outside of the room to medically-necessary purposes. If transport or movement outside an AIIR is necessary, instruct patients to wear a surgical mask, if possible, and observe Respiratory Hygiene/Cough Etiquette. Healthcare personnel transporting patients who are on Airborne Precautions “do not need to wear a mask or respirator during transport” if the patient is wearing a mask and infectious skin lesions are covered. Single room (negative pressure room), with suction effect. The room will have 6-12 air changes an hour to decrease infectious particles in the room. Keep room door closed at ALL TIMES! Remember: Mnemonic is MTV M - Measles (Rubeola) T - Tuberculosis V- Varicella Zoster (Chicken Pox), Herpes Zoster (Shingles - disseminated type) Airborne and Contact 34 NCLEX-RN study guide 100 m Others: Severe acute respiratory syndrome (SARS): Airborne, Droplet and Contact Smallpox (variola): Airborne, Droplet and Contact Middle east respiratory syndrome -Corona Virus (MERS-COV): Airborne, Droplet and Contact Healthcare Associated Infections (HCAIs): Bundles of Care Ventilator associated pneumonia (VAP) ▪ Keep the head of the patient’s bed raised between 30 and 45 degrees unless other medical conditions do not allow this to occur. ▪ Assessment of readiness to extubate ▪ Hand hygiene before and after touching the patient or the ventilator. ▪ Oral care - chlorhexidine (minimizes microaspiration) ▪ Peptic ulcer prophylaxis - PPIs (minimizes complications and length of stay) ▪ Venous Thromboembolism (VTE) prevention (minimizes complications and length of stay) 35 NCLEX-RN study guide 100 m Central line associated blood stream infections(CLABSI) • Comply hand hygiene religiously • Avoid femoral site in obese adult patients. • Prepare the insertion site with >0.5% chlorhexidine with alcohol. • Immediately replace dressings that are wet, soiled, or dislodged – NO WET DRESSING • If blood or blood products or fat emulsions are administered change tubing every 24 hours. • Promptly remove unnecessary central lines • Perform daily audits to assess whether each central line is still needed Catheter associated urinary tract infections(CAUTI) • CATHETERIZE patient only when necessary • Perform daily assessment of the need for catheter • Secure catheter properly • Ensure that urine bag is below bladder, not touching the floor • Perform catheter care daily • Empty drainage regularly 6 2 Identify patient safety risks Find out which patients are most likely to try to commit suicide. 36 NCLEX-RN study guide 100 m Suicide Assessment SAD PERSONS (1 point for each positive answer on the above) S A D P E R S O N S Sex. Men are more likely to commit suicide Age. 15-24 YO / >40 YO Depression Prior History of suicide Ethanol/alcohol and drug abuse. Rational thinking loss, Psychosis Separated divorced or widowed Organized Plan. Having a method in mind No Significant Other Sickness. Terminal illness Score Risk 0-2: No real problems, keep watch 3-4 : Send home, but check frequently 5-6: Consider hospitalization involuntary or voluntary, depending on your level of assurance patient with return for another therapy 7-10: Definitely hospitalize involuntarily or voluntarily 7 2 Prevent mistakes in surgery Remember: ▪ Make sure that the correct surgery is done on the correct patient and at the correct site on the patient’s body. ▪ “Surgical Site Marking”: Mark the correct place on the patient’s body where the surgery is to be done ▪ “Team Time-out”: Pause before the surgery to make sure that a mistake is not being made 37 100 m NCLEX-RN study guide Facility Safety Fire When a fire occurs in a health care agency, the nurse should use the mnemonic RACE to remember the priority steps. The mnemonic PASS is often used to help people remember the steps used in operating a fire extinguisher: R: Rescue any clients in danger and move them to safety A: Alarm-sound the alarm and activate the agency's fire response C: Confine the fire by closing all doors to all rooms E: Extinguish the fire, if possible, with a fire extinguisher P: Pull the pin on the handle to release the extinguisher's lock A: Aim the spray at the base of the fire S: Squeeze the handle to release the contents S: Sweep the spray from side to side until the fire is extinguished 38 100 m NCLEX-RN study guide Child Safety ▪ The safest place for all children to ride, regardless of age, is in the back seat of the car. ▪ Lock the car doors; 4-door cars should be equipped with child safety locks on the back doors. ▪ Do not leave the infant unattended in the bath. Check for water temperature. ▪ Do not hold the infant near hot liquids or items. ▪ Use cool vaporizers instead of steam should if needed, to prevent burn injuries. ▪ Prevent choking by avoiding round shaped food or similar to the size of the airway. ▪ Toys must have no small parts. ▪ Toys hanging over the crib should be out of reach, to prevent strangulation. ▪ Avoid placing large toys in the crib because an older infant may use them as steps to climb. ▪ Cribs should be positioned away from curtains ▪ Cover electrical outlets. ▪ Remove chemicals such as cleaning or other household products, medications, poisons, and plants from the infant’s reach. ▪ Toddlers need to be supervised at play to ensure safety. ▪ Keep all medicines, poisons, household plants, and toxic products in high areas and locked out of reach. ▪ Teach a preschooler and school-age child to leave an area immediately if a gun is visible and to tell an adult. ▪ Children should always wear a helmet when riding a bike or using in-line skates or skateboards. ▪ Teach the child water safety rules. 39 100 m NCLEX-RN study guide Remember: CDC recommendation Up to age 2 YO: Rear facing seat or per state requirement >2 – 5 YO: Forward facing seat or per state requirement >5 up: Booster seat until seat belt fits properly (no booster seats) ≥12 YO: Can seat on a front or per state requirement 40 NCLEX-RN study guide 100 m 4 Nursing Fundamentals Common Drag and Drop: Fall Incident 1. Assess for presence of adequate pulse 2. Inspect the client for injuries 3. Get help and move the client to the bed 4. Notify the client's health care provider (HCP) 5. Complete an incident report Fire Incident: RACE protocol 1. Rescue/remove any clients in immediate danger 2. Pull the fire alarm / activate Code system 3. Close the door to the area of fire 4. Attempt to put out the fire with a fire extinguisher – evacuate as needed 5. Discourage visitors from using the elevators Volume Oriented Incentive Spirometer 1. Exhale normally and place the mouthpiece in the mouth 2. Seal lips tightly on mouthpiece 3. Inhale deeply, until piston is elevated to predetermined level 4. Hold breath for at least 2-3 seconds 5. Exhale slowly around the mouthpiece 41 100 m NCLEX-RN study guide Measuring peak expiratory flow: peak flow meter 1. Slide the indicator to the 0 or lowest level and instruct the client to sit upright 2. Instruct the client to inhale deeply, place the mouthpiece in the mouth, and tightly seal using the lips 3. Instruct the client to exhale as quickly and forcibly as possible, note the reading on the numbered scale 4. Repeat the procedure 2 more times with a 5– 10-second rest period between exhalations 5. Record the highest reading (personal best) Metered Dose Inhaler (MDI) 1. Shake canister well for 3-5 seconds 2. Tilt head back and exhale slowly for 3-5 seconds 3. Place mouthpiece between teeth and wrap lips around mouthpiece 4. Compress canister while inhaling slowly through the mouth for 3-5 seconds 5. Hold breath for 10 seconds before exhaling 6. Wait at least 1-2 minutes before taking a second puff as prescribed Metered Dose Inhaler (MDI) With Spacer 1. Shake the medicine 2. Insert the mouthpiece of the inhaler to the end of the spacer 3. Exhale all air out of your lungs. Then put the spacer into mouth between teeth. Make a tight seal around the mouth piece with your lips. 4. Press the metered dose inhaler down the medicine. The medicine will be trapped in the spacer. Breathe in slowly and deeply. 5. Hold your breath for at least 5-10 seconds. Breathe out slowly. 42 100 m NCLEX-RN study guide Huff Coughing: to decrease lung secretion 1. Position upright 2. Inhale through the nose using abdominal breathing and through pursed lips for 3 breaths (prolong exhalation) 3. Hold breath for 2–3 seconds following an inhalation while keeping the throat open, then exhale 4. Deeply inhale and, while leaning forward, force the breath out gently using the abdominal muscles while making a "ha" sound (huff cough); repeat 2x Tracheostomy Care / Dressing: 1. Gather supplies and position client 2. Don mask, goggles, and clean gloves 3. Remove soiled dressing 4. Don sterile gloves; remove dispose old cannula and replace with a new one 5. Clean around stoma with sterile water or saline; dry and replace sterile gauze pad Lumbar Puncture (Prep): 1. Check consent 2. Gather the lumbar puncture tray and supplies 3. Have the patient empty the bladder 4. Assist the patient into the side-lying position with the knees drawn up 5. Label specimen vials as they are collected 6. Place a bandage on the insertion site 43 100 m NCLEX-RN study guide Central line tubing change (client suddenly begins gasping for air and writhing): 1. Clamp the catheter tubing 2. Place the client in Trendelenburg position on the left side 3. Administer oxygen as needed 4. Notify the health care provider (HCP) 5. Stay with the client and provide reassurance Z-Track technique: IM Injection: 1. Pull the skin 1-1 ½" (2.5-3.5 cm) laterally and away from the injection site 2. Hold the skin taut with non-dominant hand and insert needle at a 90-degree angle 3. Inject medication slowly with dominant hand while maintaining traction 4. Wait 10 seconds after injecting the medication and withdraw the needle 5. Release the hold on the skin, allowing the layers to slide back to their original position 6. Apply gentle pressure at the injection site but do not massage Administration of nasal sprays: 1. Assume a high Fowler's position with head tilted forward 2. Insert the nasal spray nozzle into nostril, occluding the other nostril with a finger 3. Point the nasal spray tip toward the side and away from the center (septum) 4. Spray the medication while inhaling deeply 5. Remove the nozzle and breathe through the mouth 6. Repeat the above steps for the other nostril 44 100 m NCLEX-RN study guide Ear Irrigation (Adult): 1. Assess the patient for ear infection, or tympanic membrane injury 2. Place the client in a sitting position with the head tilted toward the affected ear 3. Place a towel and an emesis basin under the ear 4. Straighten the ear canal by pulling the pinna up and back (down & back - ≤ 3YO) 5. Gently irrigate the ear canal with a slow, steady flow of solution Administration of suppositories: 1. Apply clean gloves and position the client (infant: supine with raised legs, Adult: left side lying with knees flexed) 2. Lubricate the tip of the suppository with water-soluble jelly. 3. Insert the suppository past the internal sphincter using the fifth finger (<3 YO). 4. Hold the buttocks together for several minutes, or until the urge to defecate has passed, to prevent immediate expulsion Inserting NGT 1. Assess and select nares 2. Measure, mark, and lubricate tube 3. Instruct client to extend neck back slightly 4. Gently insert tube just past nasopharynx 5. Ask client to flex head forward and swallow 6. Advance tube to the marked point 7. Verify tube placement and anchor 45 100 m NCLEX-RN study guide Inserting Urinary Catheter: 1. Perform hand hygiene 2. Apply sterile gloves 3. Use non-dominant hand to spread the labia 4. Cleanse labial fold with antiseptic swab 5. Wipe meatus with antiseptic swab 6. Insert catheter until urine is seen Bowel Irrigation: 1. Fill the irrigation container with 500-1000 mL of lukewarm water, flush irrigation tubing, and re-clamp and hung. 2. Instruct the client to sit on the toilet, place the irrigation sleeve over the stoma, extend the sleeve into the toilet. 3. Place the irrigation container approximately 18-24 inches above the stoma 4. Lubricate cone-tipped irrigator, insert cone and attached catheter gently into the stoma. 5. Slowly open the roller clamp, allowing irrigation solution to flow for 5-10 minutes. Clamp the tubing if cramping occurs, until it subsides 6. Once the desired amount of solution is instilled allow feces is allowed to drain through the toilet Guaiac Fecal Occult blood test: 1. Obtain supplies, wash hands, and apply nonsterile gloves. 2. Open the slide's flap and apply 2 separate stool samples to the boxes on the slide. 3. Open the back of the slide and apply 2 drops of developing solution to each box. 4. Wait 30-60 seconds. 5. Document the results 46 100 m NCLEX-RN study guide BSE: Breast Self-examination 1. Place arm behind the head and lie down 2. Use the left hand to palpate the right breast and right hand for the left breast. 3. Palpate the breast with the use of finger pads of the three middle fingers 4. Using circular motion, palpate the breast tissue progressing from light, medium and firm pressure 5. Palpate each breast from top to bottom and then by going across the breast from side to side Anaphylactic shock due to IV medications (e.g. Antibiotics) 1. Stop the infusion and call for help 2. Assess airway and place client on oxygen supplement 3. Give IM epinephrine and start IV normal saline 4. Administer diphenhydramine IV 5. Monitor vital signs for changes Blood Transfusion Administration 1. Always verify blood products, type and crossmatch results, and client identifiers with another nurse prior to transfusion. 2. Obtain vital signs before, during, and after blood administration. 3. Use Y tubing primed with NS and an IV pump for administration. 4. Watch for transfusion reaction 5. Stop the transfusion immediately if a reaction occurs. Blood Transfusion Reaction 1. Stop the blood transfusion 2. Using new tubing, infuse normal saline into the vein 3. Administer prescribed vasopressor 4. Collect urine specimen 5. Document the incident 47 NCLEX-RN study guide 100 m 5 Pain Management Pain Assessment: Severity: Mild (1-3) Moderate (4-6) Severe (7-10) 1. 2. 3. 4. Verbal Scale (Conscious/Awake ≥9 YO) Faces (Wong-Baker) (Conscious/Awake <9 YO) “Can also be used for conscious/awake ≥9 YO, to support verbal scale” FRAAC Scale (unconscious, confused, demented ≥9 YO) Faces, Respiration, Activity, Audibility, Consolability FLACC Scale (unconscious <9 YO) Face, Legs, Activity, Cry, Consolability Pain Ladder: WHO Pain ladder (aka analgesic ladder): By World Health Organization (WHO) Is a guideline for the use of drugs in the management of pain. Originally published in 1986 for the management of cancer pain, it is now widely used in all types of pain. The principle is to start with first step drugs, and then to climb the ladder if pain is still present. One of the purpose is to limit tolerance and dependence to opioid analgesics 48 NCLEX-RN study guide 100 m Mild Pain (1-3) NSAIDS/Non Opioid: Acetaminophen, Aspirin, Ibuprofen, Ketorolac Adjuvant: Steroids, antidepressants (amitriptyline, nortriptyline, venlafaxine, duloxetine) Antiseizures (pregabalin, gabapentin), anticholinergics (Oxybutynin) Moderate Pain (4-6) Weak Opioids: Tramadol, Codeine Hydrocodone, Oxycodone +/- NSAIDS/Non Opioid +/- Adjuvant Severe Pain (7-10) Strong Opioids: Morphine, Hydromorphone, Fentanyl +/- NSAIDS/Non Opioid +/- Adjuvant Facts: ▪ Meperidine – High risk for seizure due to neurotoxic effects ▪ Hydromorphone (Dilaudid) – Fast acting opioid, potent narcotic that has 5-10 times the strength of morphine, typical maximum dose is 2 mg ▪ Hydromorphone IV push, given undiluted or diluted with 5 mL of sterile water or normal saline, should be administered slowly over 2-3 minutes; rapid infusion increases the risk of opioid-induced adverse reactions (e.g. nausea, itching). ▪ Undiluted morphine IV push should be administered slowly over 4-5 minutes; rapid infusion increases the risk of opioidinduced adverse reactions (e.g., hypotension, flushing). ▪ Most commonly abused narcotics in the US: heroin, morphine, codeine 49 100 m NCLEX-RN study guide ▪ Morphine can be used for pancreatitis; worsening pancreatitis due to increase in sphincter of Oddi pressure “has not been proven in studies”. ▪ Fentanyl (IV): Strongest narcotic 100x stronger than morphine Patch: Less potent (not given in post-op pain) due to slower effect (17 hours to achieve full effect) The patch provides continuous analgesia for up to 72 hours. Remember: There is still some drug remaining on the patch when it is removed after the 72 hours. This can be harmful if children, pets, or caregivers are exposed. The patch must be contained and immediately disposed of (flushed down the toilet, discarded deep into the trash). ▪ Common side effects of opioid analgesics: Short term: Pruritus, nausea and vomiting (vomiting 3X or more is reportable), urine incontinence. Long term: constipation ▪ A neonate born to an opioid-dependent mother: is at high risk for neonatal abstinence syndrome, an opioid withdrawal typically within 24-48 hours after birth. Clinical manifestations: irritability, jitteriness, high pitched cry, sneezing, diarrhea, vomiting, poor feeding ▪ Naloxone: Drug of choice for opioid intoxication ▪ Methadone: Drug of choice for opioid withdrawal (longer half-life of up to 60 hours) Stages of drug addiction: 1. Experimentation (controlled) – use without legal consequence “for fun only” 2. Regular Use (controlled) – use with legal consequence “driving under influence” 3. Risky use/abuse (uncontrolled) – craving , depression, anxiety 4. Dependence (uncontrolled) – withdrawal, compulsion, psychiatric implications 50 100 m NCLEX-RN study guide Question 1: Client with cancer pain is prescribed oxycodone. Which teaching is most essential to help prevent long-term complications? 1. Teach the client how to assess blood pressure daily 2. Teach the client how to prevent constipation 3. Teach the client how to prevent itching 4. Teach the client how to prevent nausea Answer: 2 Rationale: Constipation is an expected long-term side effect of opioid use; clients will not develop tolerance to this side effect. It is important to teach aggressive preventive measures (e.g. defecate when the urge is felt, drink 23 L of fluid/day, high-fiber diet, exercise) and simultaneous use of a stool softener and a stimulant. Question 2: A post-surgical client is unresponsive to painful stimuli and is given naloxone. Within 5 minutes, the client is arousable and responds to verbal commands. One hour later, the client is again difficult to arouse, with minimal response to physical stimuli. Which actions should the nurse take? Select all that apply. 1. Administer oxygen 2. Assess respiratory rate 3. Initiate rapid response or code team 4. Notify the health care provider 5. Prepare a second dose of naloxone Answer: 1,2,4,5 Rationale: Naloxone (Narcan) is usually prescribed as needed for post-surgical clients for over-sedation related to opioid use. The nurse should continue to monitor clients who are given naloxone with the understanding that the opioid antagonist has a shorter half-life (1-2hours) than most of the opioids it is meant to counteract. As a result, a second dose of naloxone may be necessary 51 NCLEX-RN study guide 100 m 6 Cardiovascular Anatomy 4 chambers: ▪ Atria (2) ▪ Ventricle (2) 4 Valves: ▪ Semilunar: Aortic, pulmonic ▪ Atrioventricular: Tricuspid, Bicuspid/Mitral Remember: Stenosis – is a narrowing of valves Regurgitation – is the process (backflow of blood) Murmur – is the symptom (assessment) 52 100 m NCLEX-RN study guide Coverings (epicardium): Pericardium ▪ Fibrous ▪ Serous (parietal, pericardial cavity, visceral) Myocardium Endocardium Major Veins ▪ Inferior & Superior Vena Cava (unoxygenated) ▪ 4 Pulmonary Veins (oxygenated) Major Arteries ▪ Pulmonary arteries (unoxygenated) ▪ Aorta (oxygenated) 53 100 m NCLEX-RN study guide Physiology Action - Potential: the potential of a tissue to produce an effect (ex: contraction) Resting - Potential: the potential of a tissue not to cause an effect (ex: relaxation) Electrolytes: determine action potential in the cell membrane Sodium (Na+) Extracellular Potassium (K+) Intracellular Calcium (Ca++) Extracellular Remember: Action – Potential: occurs in 3 types of tissues 1. Heart 2. Nerve 3. Muscles (smooth and skeletal) Heart Action-Potential: 2 types 1. Electrolytes: Ca++, Na+: Contract K+: Relax 2. Conduction System SA, AV nodes, Bundle of His, Purkinje Fibers (propagation of heart rate) Phase 0: Na+ in beginning of action-potential (contraction) Remember: Na+ is extracellular, if it goes inside the cell it causes contraction together with Ca++ Phase 1: K+ out after rapid influx of Na+ inside the cell Remember: Active Na+ K+ pump is ongoing Phase 2: Ca++ in, K+ out Phase 3: K+ out Phase 4: beginning of resting – potential (relaxation) 54 100 m NCLEX-RN study guide Conduction System: Propagation of heart rate Remember: Action potential vs Conduction system ▪ Action potential is for contraction and relaxation ▪ Conduction system is for heart rate propagation Remember: Autonomic Nervous System influences conduction system through ▪ Sympathetic/Adrenergic Nerves: Increase heart rate ▪ Vagus Nerve/Cholinergic: decrease heart rate How? Sympathetic Nerves: Binding of catecholamines (e.g. epinephrine, epinephrine) to adrenergic receptors in the heart (Beta 1, alpha 1) Vagus Nerve: Binding of acetylcholine to muscarinic/cholinergic receptors in the heart (M2) 55 NCLEX-RN study guide 100 m Conduction system Remember: EKG is the reflection of Conduction System (See in EKG interpretation) Cardiac Output Cardiac output (CO) is the amount of blood the heart pumps in 1 minute, and it is dependent on the heart rate, contractility, preload, and afterload. Normal CO: 4-8 liters per minute, depending on the persons size. Basically, total blood volume circulates to heart in 1 full minute as a cardiac output (CO) Remember: Cardiac output Cardiac Output is just simply what you want from heart to produce in order to nourish nutrients and O2 in each body system. Persistent decrease CO means abnormal heart and subsequent problem to brain, kidneys, heart, liver tissues, etc. 56 100 m NCLEX-RN study guide Cardiac CO: Heart Rate (HR) x Stroke Volume Heart Rate (HR): Heart rate is the speed of the heartbeat measured by the number of contractions (beats) of the heart per minute (bpm) propagated by conduction system. Stroke Volume (SV): Volume of blood pumped by the ventricles with each heartbeat. Approximately 70 ml. Preload: aka “Filling Pressure”. Is the pressure that stretches the right or left ventricle during relaxation or before it contracts to produce cardiac output. Afterload: is a pressure against which the heart must overcome to eject blood during contraction. Ex: aortic pressure Summary: As mentioned cardiac output is simply the most important component of cardiac physiology. In a normal circumstance, body systems received sufficient CO to perform their functions including the heart itself via patent coronary arteries. Decrease CO means 57 NCLEX-RN study guide 100 m decrease volume and decrease blood pressure. Hence, in every heart conditions, it is very important to check the patient’s BP to determine severity. Cardiac output explained: Ex: Cardiac Tamponade (sudden accumulation of fluid in the pericardial sac leading to compression). Increase HR results from compensatory mechanisms. However, increase HR does not necessarily mean increase in CO. For this instance, the ability of the heart to produce a sufficient CO is also determined by the volume of blood during the process of contraction/relaxation. Compression of the heart decreases stroke volume. Becks Triad: Hypotension/narrowed pulse pressure Narrowed PP (difference between SBP and DBP – normal is 40– 60 mmhg) Hypotension causes narrowed PP. This is caused by alterations in CO due to compression. Jugular venous distention Limits the ability of the heart to expand due to pressure build up affecting preload and afterload, subsequently the CO. Muffled heart sounds/Distant heart sounds Inaudible heart sounds due to fluid build-up in the pericardium Inotropic is a cardiac drug that affects cardiac contraction. Chronotropic is a cardiac drug that affects heart rate. Dromotropic is a cardiac drug that affects conducting tissues of the heart. Sample medication: DIGOXIN: (+) Inotropic (-) Chronotropic, (-) Dromotropic DOPAMINE, EPI, NE: (+) Inotropic (+) Chronotropic, (+) Dromotropic 58 100 m NCLEX-RN study guide Question: A client has developed atrial fibrillation, with a ventricular rate of 150 beats/minute. The nurse should assess the client for which associated signs/symptoms? 1. Flat neck veins 2. Nausea and vomiting 3. Hypotension and dizziness 4. Hypertension and headache Answer: 3 Rationale: The client with uncontrolled atrial fibrillation with a ventricular rate more than 100 beats/minute is at risk for low cardiac output because of loss of atrial kick. The nurse assesses the client for palpitations, chest pain or discomfort, hypotension, pulse deficit, fatigue, weakness, dizziness, syncope, shortness of breath, and distended neck veins. Test strategy, most likely the answer is between the two opposing answers (3. Hypotension, 4. Hypertension) 59 100 m NCLEX-RN study guide EKG interpretation: Steps 1. Identify PQRST Must know what are PQRST represents. Don’t mind the gridlines initially. Remember EKG takes an analysis, step by step process is applied. P wave: Atrial contraction/depolarization PR Interval: Atrial relaxation/repolarization QRS complexes: Ventricular contraction/depolarization T wave: Ventricular relaxation/repolarization Remember: Isoelectric line An imaginary line to determine ST segment deviation. (dotted lines on the image) Depression: ischemia Elevation: infarction Remember: Possible implications to abnormalities in PQRST P wave – Atrial arrhythmias (missing, aberrant) PR Interval – AV Block (prolonged) QRS complexes – Ventricular arrhythmias (widened, bizarre) T wave – Hypo/hyperkalemia, Pulmonary embolism, Digoxin, AMI (inversion, peaked) ST segment – AMI (elevation, depression) QT Interval – Hypomagnesemia (prolonged) 60 100 m NCLEX-RN study guide 2. Determine PR Interval, QRS Complex (time) Since you identified PQRST. This time, EKG gridlines are considered to measure PR interval and QRS complex. Measuring PR interval is basically determining the relationship of atria and ventricles. Deviation from this interval (prolonged) simply means an atrioventricular concern (ex: AV Block). In addition, measuring QRS complex is identifying ventricular activity (contraction) which is the most important component of heart electrophysiological activity in relation to producing sufficient CO. This means that a ventricular arrhythmia is more life threatening if not treated promptly. In fact, the most common cause of death among AMI patients. 61 100 m NCLEX-RN study guide Normal values: PR Interval: 0.12-0.20 secs Abnormal: ≥ 0.24 secs QRS comp: 0.6-0.12 secs Abnormal: > 0.12 secs 3. Check rhythm. What is a regular rhythm? A regular rhythm means the same distance between PRQST complexes by measuring R-R intervals. What is irregular rhythm? An irregular rhythm simply means abnormal distances between R-R intervals. Remember: Checking rhythms is important in counting the heart rate. One cycle of PQRST represents the other in a regular rhythm. In contrast, one cycle may not represent the other in an irregular rhythm. 62 NCLEX-RN study guide 100 m Regular rhythm: Same distances between R – R Irregular rhythm: Different distances between R - R Common regular rhythm (R-R Intervals): ▪ Sinus Rhythm ▪ Sinus Tachycardia ▪ Sinus Bradycardia ▪ Supraventricular Tachycardia(SVT) ▪ Atrial Flutter (variable) ▪ 3rd degree AV block (CHB) Common irregular rhythm (R-R Intervals): ▪ Premature Atrial Contractions ▪ (PACs) ▪ Premature Ventricular Contractions (PVCs) ▪ Atrial Fibrillation ▪ 2nd degree AV block (Type 1) 63 100 m NCLEX-RN study guide 4. Determine the heart rate. A normal resting heart rate is 60 to 100 beats per minute per EKG reading. In a normally paced heart, SA node (pacemaker) produce 60-100 bpm enough to influence a sufficient cardiac output with a normal preload and afterload physiology. On the other hand, a non-pacemaker such as AV node may not produce enough rate at 40-60 bpm. If you have arrhythmias such as ventricular ectopy (PVCs), as the word says ectopy which means “out of place”, the conduction must not be coming from the SA node. This causes alteration in a normal rate and rhythm which subsequently affects normal cardiac output. Six (6) seconds strip method: Applicable for both regular and irregular rhythm. Count the number of QRS complexes over a 6 second interval. Multiply by 10 to determine heart rate. 10 R waves or QRS complexes in a 6 second strip in a regular rhythm multiply by 10 is 100 bpm. 10 QRS X 10 = 100 bpm 5 R waves or QRS complexes in a 6 second strip in an irregular rhythm multiply by 10 is 50 bpm. 5 QRS X 10 = 50 bpm 64 100 m NCLEX-RN study guide 1,500 method: Applicable ONLY for regular rhythm. Since R-R intervals are all the same or constant in all cycles, one R-R represents the other. Determine the heart rate by counting the number of smallest boxes between R-R. (Most accurate in calculating HR) Smallest boxes: 1500 mm/min ÷ 15 = 100 bpm Note: 1mm = 1 smallest box 1 sec = 25 smallest boxes 60 sec (1 min) = 1,500 smallest boxes (1,500 mm) 65 100 m NCLEX-RN study guide Application: 1. Identify PQRST Notable Question: Is there distinct P wave? Yes, P wave is positively deflected (upward) Is there QRS? Yes, QRS complex is present, (Q: negative deflection, R: positive deflection, S: negative deflection) Is there T? Yes, T wave present with positive deflection and is slightly higher than the P wave. Is there ST depression or elevation? No Is there peaked or inverted T wave? No Findings: This is a normal morphology of a PQRST. 66 100 m NCLEX-RN study guide 2. Determine PR Interval, QRS Complex (time) Notable Question: Since there distinct P wave and a QRS complex, what is the PR interval? 0.16 secs (4 smallest squares x 0.04 secs) Is it within normal limits? Yes What is the QRS complex? 0.06 secs (1½ smallest squares x 0.4 sec) Is it within normal limits? Yes Findings: This is a normal morphology of a PQRST with normal PR (normal relationship between atria and ventricles) and normal QRS (normal ventricular contraction) Remember: QRS complex identifies ventricular activity (contraction), the most important component of heart electrophysiological activity to produce sufficient CO. Ventricular arrhythmia such as PVC is significant. 67 NCLEX-RN study guide 100 m 68 3. Check rhythm. Notable Question: Is the rhythm regular or irregular? Regular (same distances on R-R) Findings: Normal morphology of a PQRST with normal PR and QRS time limits on a regular rhythm 4. Determine the heart rate. Notable Question: Which method will be used to get the HR? Either six (6) second strip or 1,500 method (more accurate). Six (6) seconds strip method: 8 R or QRS comp x 10 = 80 bpm 1 2 3 4 5 6 7 8 100 m NCLEX-RN study guide 1,500 method: 1,500 ÷ 19 smallest boxes = 79 bpm Findings: Normal morphology of a PQRST with normal PR and QRS time limits on a regular rhythm and heart rate within 60-100 bpm. Interpretation: Normal Sinus Rhythm 69 NCLEX-RN study guide 100 m Common Arrhythmias I. Sinus Bradycardia PQRST P wave: Normal PR Interval: Normal QRS complex: Normal Rhythm: Regular Rate: <60 bpm Remember: The only abnormality in this rhythm is the heart rate which is below 60 bpm. In determining the HR, you can use either 1,500 or 6 second strip method. In this example, the HR is 40 bpm using six second strip (4 QRS x 10 = 40 bpm). If bradycardia doesn't cause symptoms, it usually isn't treated. Management: (follow ACLS bradycardia algorithm) It takes 1 question to decide which type of management is necessary. Is the bradycardia causing symptoms? Hypotension, altered mental status, ischemic chest discomfort, signs of acute heart failure (short of breath) 70 NCLEX-RN study guide 100 m If not: Monitor and observe If symptomatic: Emergency management 1. Consider administering atropine 0.5 mg IV if IV access is available. This may be repeated every 3 to 5 minutes up to 3 mg or 6 doses. 2. Prepare for transcutaneous pacing. If no IV is present pacing can be first. Note: If the atropine is ineffective, begin transcutaneous pacing. Consider epinephrine or dopamine while waiting for the pacer or if pacing is ineffective. Epinephrine 2 to 10 µg/min Dopamine 2 to 20 µg/kg per minute Consider expert consultation for Transvenous Pacing if efforts are ineffective. Transcutaneous Pacing (TCP) is a temporary means of pacing a patient’s heart during an emergency and stabilizing the patient until a more permanent means of pacing is achieved. 71 NCLEX-RN study guide 100 m Transvenous pacing is also a temporary means of treating symptomatic bradycardias that do not respond to transcutaneous pacing or to drug therapy. Transvenous pacing is achieved by threading a pacing electrode through a vein into the right atrium, right ventricle, or both. II. Sinus Tachycardia PQRST P wave: Normal PR Interval: Normal QRS complex: Normal Rhythm: Regular Rate: >100 bpm 72 NCLEX-RN study guide 100 m Remember: The only abnormality in this rhythm is the heart rate which is above 100 bpm. In determining the HR, you can use either 1,500 or 6 second strip method. In this example, the HR is 130 bpm using six second strip (13 QRS x 10 = 130 bpm). If tachycardia doesn't cause symptoms, it usually isn't treated. Management: Is the tachycardia ≥ 150 bpm? If not: Monitor and observe. Underlying causes are treated if present. Causes: Pain, Fever, Anxiety, Dehydration, Anemia Hyperthyroidism, Sepsis, Pulmonary embolism Intake of stimulants such as caffeine, theophylline, nicotine, cocaine, or amphetamines If ≥ 150 bpm: Evaluate the rhythm. This might be one of the several tachycardia rhythms Supraventricular tachycardia (SVT) Atrial fibrillation Atrial flutter Ventricular tachycardia Note: Management discussed in specific tachycardias 73 NCLEX-RN study guide 100 m III. Atrial arrhythmias Remember that this abnormal rhythm originates from the atria which is reflected on the P waves (Atrial contraction) in the EKG. P wave abnormality is expected. 1. Atrial Fibrillation PQRST P wave: Absent, Fibrillatory PR Interval: Non existent QRS complex: Normal Rhythm: Irregular Rate: Slow - rapid Remember: The two (2) main characteristics of Atrial fibrillation are absence of P waves and irregular rhythm. It is classified according to its HR as follows: Atrial fibrillation with slow ventricular response (SVR): HR below 60 bpm. Atrial fibrillation with moderate ventricular response (MVR): HR within 60 – 100 bpm. Atrial fibrillation with rapid ventricular response (RVR): HR above 100 bpm. Ventricular rate control is a priority in clients with atrial fibrillation 74 NCLEX-RN study guide 100 m Management: Acronym is ABCD A: Anticoagulants (warfarin, dabigatran, rivaroxaban, apixaban) Patients with A-fib greater risk for forming clots due to abnormal atrial activity. Blood stasis in atria influences clot formation. B: Beta Blockers (metoprolol) blocks beta adrenergic cells stimulation. C: Calcium Blockers (diltiazem, verapamil) Catheter Ablation – Heating or freezing the area to destroy tissues that causes fibrillatory waves D: Digitalis (Digoxin) E: Electrocardioversion 2. Atrial Flutter PQRST P wave: Flutter waves (sawtooth) PR Interval: Not applicable QRS complex: Normal Rhythm: Regular/irregular Rate: Rapid (atrial/P Waves) Remember: Less common than atrial fibrillation. The main characteristic of atrial flutter is “sawtooth” formation of P waves. 75 100 m NCLEX-RN study guide Management: (same with A-fib) Acronym is ABCD A: Anticoagulants (warfarin, dabigatran, rivaroxaban, apixaban) Patients with A-fib greater risk for forming clots due to abnormal atrial activity. Blood stasis in atria influences clot formation. B: Beta Blockers (metoprolol) Blocks beta adrenergic cells stimulation. C: Calcium Blockers (diltiazem, verapamil) Catheter Ablation – Heating or freezing the area to destroy tissues that causes fibrillatory waves D: Digitalis (Digoxin) E: Electrocardioversion 3. Premature Atrial Contraction/Complex (PAC) PAC PQRST P wave: Present (if not: Premature Junctional Comp./PJC) PR Interval: Normal QRS complex: Normal Rhythm: Irregular (the premature complex makes it irregular) Rate: Variable 76 NCLEX-RN study guide 100 m Remember: The above is an example of a single, isolated PAC. The heart rate in this example is 80 bpm using the six second method (8 QRS x 10 = 80) as the rhythm is irregular. The first five cycles are normal, but the sixth beat occurs prematurely that are not generated by the SA node. You can see the P wave right after the T wave of the previous beat. PACs generally have very little medical significance. However, in some cases PACs are triggers of life threatening arrhythmias such as A-fib. Management: PACs are often benign, requiring no treatment. However, it is important to monitor patients with co-morbidities such as hypertension, hyperlipidemia as it leads to more serious arrhythmias. 4. Supraventricular Tachycardia (SVT) PQRST P wave: Frequently buried on preceding T waves PR Interval: N/A QRS complex: Normal (usually narrow complex, rarely wide) Rhythm: Regular Rate: 150 – 250 bpm Remember: SVT is one of the most common tachycardias that originates form the atria (above the ventricles). Between 77 NCLEX-RN study guide 100 m SVT and ST, the former has a higher HR at 150 or higher. On the other hand, ST has a visible P-waves. As for SVT, Pwaves will be entirely buried making it impossible to describe their morphology and measure the PR interval. It is also important to determine A-Fib with rapid ventricular response, though both SVT and rapid A-fib has narrow QRS complexes and no visible P-waves, SVT has a regular R-R interval (regular rhythm) contrary to A-fib. The distinction between regular and irregular rhythm (SVT vs. Rapid A-fib) is fundamental since they are treated differently. For instance, adenosine (drug of choice for SVT) cannot be given to a patient with A-fib because it causes further fatal arrhythmias. Management: Remember, the key to managing a patient with any tachycardia is to check if pulses are present, decide if the patient is stable or unstable and then manage. Low SBP (<90 mmhg) is an implication of a low cardiac output. Measuring BP is a primary assessment. Is the patient stable or unstable? If stable: Vagal Maneuvers The act of "bearing down" as if having a bowel movement (valsalva) is an example of these maneuvers and may need to be attempted more than once. (increases intra-thoracic pressure and stimulates vagus nerve) Other: Coughing, gagging, carotid massage (may be performed by physician) If not effective: Give medication Adenosine is the first-line drug of choice for SVT. 78 100 m NCLEX-RN study guide The half-life is <5 seconds, so adenosine should be administered rapidly as a 6-mg bolus IV over 1-2 seconds followed by a 20-mL saline flush. Repeat boluses of 12 mg may be given twice if the SVT persists. (6mg – 12 mg – 12mg). Remember: Brief period of asystole is due to adenosine slowing impulse conduction through AV node. In addition, monitor for flushing, dizziness, chest pain, or palpitations during and after administration If Adenosine not effective: Consider other medications P: Procainamide Decreases myocardial excitability by blocking myocardial Na+ channels. It also depresses myocardial excitability and conductivity A: Amiodarone (anti-arrhythmic) Prolongs Phase 3 of cardiac action-potential (repolarization) by preventing potassium to leave the cells. B: Beta Blockers (metoprolol, sotalol) Blocks beta adrenergic cells stimulation. C: Calcium Blockers (diltiazem, verapamil) Catheter Ablation – Heating or freezing the area to destroy tissues that causes the arrhythmia If unstable or medications are not effective: Synchronized Cardioversion Remember: Cardioversion rules for SVT QRS narrow and regular (SVT, Atrial flutter): 79 NCLEX-RN study guide 100 m 50 - 100 joules QRS narrow and irregular (A-fib with RVR): 100 - 200 joules Cardioversion Defibrillation Synchronized to R wave/QRS Unsynchronized Elective Emergent Conscious/Awake Unconscious Needs sedation No sedation Low energy/joules High energy/Joules Question: The telemetry nurse reports the cardiac monitor rhythms of 4 clients to the medical unit nurse assigned to care for them. The nurse should assess the client with which rhythm first? 1. Atrial fibrillation with a pulse of 76/min in a client prescribed rivaroxaban 2. Bradycardia in a client with a demand pacemaker set at 70/min 3. First-degree atrioventricular block in a client prescribed atenolol 4. Sinus tachycardia in a client with gastroenteritis and dehydration Answer: 2. Bradycardia in a client with a demand pacemaker set at 70/min Rationale: A demand electronic pacemaker should deliver an impulse when it senses an intrinsic pacemaker drop below a predetermined rate. Bradycardia with failure to capture (pacer spike with no QRS complex) indicates malfunction and requires immediate notification of the health care provider. On the other hand, Clients with atrial fibrillation are USUALLY prescribed an anticoagulant, such as rivaroxaban (Xarelto), due to increased risk for blood clots that can lead to stroke. This client's ventricular response is moderate (A-fib in MVR), so there is no urgency. Unless otherwise rapid ventricular response which requires immediate intervention. First-degree atrioventricular (AV) block can be associated with beta adrenergic blockers. Tachycardia is an expected mechanism to increase the cardiac output associated with hypotension. 80 100 m NCLEX-RN study guide Test strategy: prioritization. Obviously there are no airway problems in the given choices. Do not also choose expected findings that does not require immediate intervention. IV. Ventricular arrhythmias Remember that this abnormal rhythm originates from the ventricles which is reflected on the QRS complex (ventricular contraction) in the EKG. QRS abnormality is expected. More importantly, ventricular arrhythmias are associated with increase mortalities. 1. Premature Ventricular Contraction/Complex (PVC) PVC PQRST P wave: Absent: associated with premature beat PR Interval: N/A QRS complex: Widened, Bizarre “weird” Rhythm: Irregular (the premature complex makes it irregular) Rate: Variable Remember: The above is an example of a single, isolated PVC. The heart rate in this example is 90 bpm using the six second method (9 QRS x 10 = 90) as the rhythm is irregular. The first six cycles are normal, but the seventh beat occurs prematurely that are not generated by the SA node. This abnormal rhythm is life threatening as it involves the ventricles. An isolated PVC can lead into a more serious ventricular arrhythmias such as ventricular tachycardia 81 NCLEX-RN study guide 100 m and ventricular fibrillation if not treated promptly. In addition, an isolated PVC can lead into the following patterns presented as follows: PVCs in QUADRIgeminy: (1 single PVC and 3 normal cycles) 1 3 2 1 2 3 4. PVC 4. PVC PVCs in TRIgeminy: (1 single PVC and 2 normal cycles) 1 2 1 1 2 3. PVC 2 3. PVC 3. PVC PVCs in BIgeminy: (1 single PVC and 1 normal cycle) 1 1 2. PVC 1 1 2. PVC 2. PVC 2. PVC 82 NCLEX-RN study guide 100 m VCs in Couplets: (2 consecutive PVCs) Note: 3 consecutive PVCs or PVCs in triplets is considered ventricular tachycardia Couplets PVCs according to morphology: Unifocal/Monomorphic PVC: (PVCs in identical forms ) Multifocal/Polymorphic PVC: (PVCs in non-identical forms ) 83 NCLEX-RN study guide 100 m Management: For patients with occasional PVCs with no other symptoms and no underlying heart disease or structural problems, no treatment is necessary. For persistent and recurrent ventricular arrhythmias such as PVCs, management are as follows: Acronym: ABC - PALS A: Amiodarone (anti-arrhythmic) Prolongs Phase 3 of cardiac action-potential (repolarization) by preventing potassium to leave the cells. B: Beta Blockers (metoprolol, sotalol) blocks beta adrenergic cells stimulation. C: Calcium Blockers (diltiazem, verapamil) Catheter Ablation – Heating or freezing the area to destroy tissues that causes the arrhythmia OR P: Procainamide Decreases myocardial excitability by blocking myocardial Na+ channels. It also depresses myocardial excitability and conductivity A: Amiodarone L: Lidocaine Shortens cardiac-action potential by blocking myocardial Na+ channels S: Sotalol (beta-blocker) 84 100 m NCLEX-RN study guide 2. Ventricular Tachycardia Note: Ventricular tachycardia can be non-sustained (NSVT) or sustained. Non-sustained is referred as 3 or more consecutive v-tach that stops by itself within 30 seconds. On the other hand, the patient can be pulseless (unstable) or with pulse (stable), which will be the basis of management. PQRST P wave: Absent PR Interval: N/A QRS complex: Widened, Bizarre “weird” Rhythm: Variable Rate: Rapid (Ventricular) Remember: Ventricular tachycardia is simply untreated PVCs Monomorphic Ventricular Tachycardia: (identical QRS forms) Polymorphic Ventricular Tachycardia: (non-identical QRS forms) 85 NCLEX-RN study guide 100 m Torsades de Pointes (TdP): Is a specific form of polymorphic ventricular tachycardia occurring in a patient with QT prolongation (normal: 0.36 to 0.44 sec/9-11 boxes) , these may combine to produce TdP. QT prolongation may occur secondary to hypokalemia or hypomagnesemia. It has a characteristic morphology in which the QRS complexes “twist” around the isoelectric line. Management: Aims to either terminating an episode of the abnormal heart rhythm or to reduce the risk of another V-tach episode. Treatment also depends on the patient’s stability Pulseless/Unstable or With Pulse/Stable) as well as the underlying cause (e.g. Torsades de Pointes – Mg, Potassium replacement). Remember, the key to managing a patient with any tachycardia is to check if pulses are present, decide if the patient is stable or unstable and then manage. Low SBP (<90 mmhg) is an implication of a low cardiac output. Measuring BP is a primary assessment. A. With Pulse/Stable Synchronized Cardioversion - If the waveform is monomorphic synchronize to QRS to avoid ventricular fibrillation or worst asystole. An initial energy of 100J is recommended. If the 86 NCLEX-RN study guide 100 m waveform is polymorphic, then higher energies and an unsynchronized shock should be provided (aka. Defibrillation) Cardioversion Defibrillation Synchronized to R wave/QRS Unsynchronized Elective Emergent Conscious/Awake Unconscious Needs sedation No sedation Low energy/joules High energy/Joules Acronym: ABC - PALS A: Amiodarone (anti-arrhythmic) Prolongs Phase 3 of cardiac action-potential (repolarization) by preventing potassium to leave the cells. B: Beta Blockers (metoprolol, sotalol) Blocks beta adrenergic cells stimulation. C: Calcium Blockers (diltiazem, verapamil) Catheter Ablation – Heating or freezing the area to destroy tissues that causes the arrhythmia Cardioversion Cardioverter/Defibrillator (Implantable) or Implantable Cardioverter Defibrillator) Implanted to chest wall and more effective than drug therapy in recurrent V-tach. OR P: Procainamide Decreases myocardial excitability by blocking myocardial Na+ channels. It also depresses myocardial excitability and conductivity A: Amiodarone L: Lidocaine Shortens cardiac-action potential by blocking myocardial Na+ channels S: Sotalol (beta-blocker) 87 NCLEX-RN study guide 100 m Implantable Cardioverter Defibrillator (ICD): Is an automated device implantable inside the body, that detects abnormal impulses and if necessary, perform cardioversion, defibrillation, and pacing of the heart. B. Pulseless/Unstable When dealing with pulseless ventricular tachycardia is the same way with ventricular fibrillation. The primary management includes cycles of CPR, defibrillation and medication. Using advanced algorithm is the best method of restoring spontaneous circulation. (ACLS algorithm as discussed in the next succeeding topics) 88 100 m NCLEX-RN study guide Emergency management in ORDER: Acronym CDEA C: Cardiopulmonary Resuscitation (CPR) Provide supplemental oxygen. If bag-mask ventilation is adequate, providers may defer insertion of an advanced airway. Begin 5 cycles of CPR (approximately 2 minutes). Each cycle contains 30 chest compressions followed by 2 breaths. Interrupt chest compressions only for ventilation, rhythm checks, and actual shock delivery. CPR should never be interrupted for more than 10 seconds. Push hard (> 2 inches) & fast (100-120/min) D: Defibrillation ▪ Attach defibrillator pads, ▪ Continue CPR while the defibrillator is charging. ▪ Clear the patient for shock . ▪ Deliver the shock. ▪ Resume CPR immediately after shock, 5 cycles. E: Epinephrine If IV is available, administer epinephrine 1mg IV during the CPR cycle. Lidocaine or amiodarone can also be given. A: Advanced airway The value of securing the airway must be balanced against the need to minimize the interruption in perfusion in the early steps of resuscitation (CPR). Includes LMA (Laryngeal mask airway), laryngeal tube, and ET tube (endotracheal tube) Note: In a WITNESSED arrest with V-tach or V-Fib In the context of a witnessed arrest by a trained first responder or bystander who has an AED or manual defibrillator, the importance of early defibrillation is irrefutable. Remember: DCEA (Defibrillation, CPR, Epinephrine, Advanced airway) 89 NCLEX-RN study guide 100 m Medications Note: These are medications that are given generally for Ventricular Arrhythmias A: Amiodarone (anti-arrhythmic) Prolongs Phase 3 of cardiac action-potential (repolarization) by preventing potassium to leave the cells. B: Beta Blockers (metoprolol, sotalol) Blocks beta adrenergic cells stimulation. C: Calcium Blockers (diltiazem, verapamil) OR P: Procainamide Decreases myocardial excitability by blocking myocardial Na+ channels. It also depresses myocardial excitability and conductivity A: Amiodarone L: Lidocaine Shortens cardiac-action potential by blocking myocardial Na+ channels S: Sotalol (beta-blocker) 3. Ventricular Fibrillation Note: V-fib is a lethal dysrhythmia characterized by varying shapes and amplitude on the EKG. Mechanically, the ventricle is just "quivering" with no effective contraction or cardiac output. V-fib results in a pulseless, unresponsive, apneic state. 90 NCLEX-RN study guide 100 m PQRST P wave: Absent PR Interval: N/A QRS complex: Fibrillatory, Bizarre “weird” Rhythm: Extremely irregular Rate: Extremely rapid (ventricular) Remember: Ventricular Fibrillation is simply untreated ventricular arrhythmias. However, patient might have V-tach or V-fib with no preceding PVCs that requires immediate management. Patient is absolutely unconscious and unstable. Course Ventricular Fibrillation Fine Ventricular Fibrillation Management: Same management with ventricular tachycardia (pulseless/unstable) 91 100 m NCLEX-RN study guide Question: The nurse is preparing to defibrillate a client who suddenly went into ventricular fibrillation. Which steps are essential prior to delivering a shock? Select all that apply. 1. Apply defibrillator pads 2. Call out and look around to ensure that everyone is "all clear" 3. Continue chest compressions until ready to deliver shock 4. Ensure adequate IV sedation has been given 5. Ensure that the synchronization button is turned on Answer: 1,2, 3 Rationale: Defibrillation is indicated in clients with ventricular fibrillation (V-fib) and pulseless ventricular tachycardia. Cardiopulmonary resuscitation (CPR) should be initiated and compressions continued until the shock is ready to be delivered Certain pulseless rhythms (asystole and pulseless electrical activity) do not need defibrillation. Steps to perform defibrillation are as follows: 1. Turn on the defibrillator 2. Place defibrillator pads on the client's chest 3. Charge defibrillator. Chest compressions should continue until defibrillator has charged and is ready to deliver the shock. 4. Before delivering the shock, ensure that the area is "all clear." Confirm that no personnel are touching the client, bed, or any equipment attached to the client 5. Deliver the shock 6. Immediately resume chest compressions IV sedation is not necessary for defibrillation as the client is already unconscious. It is often given prior to elective synchronized cardioversion to ease anxiety and decrease pain. Synchronized cardioversion delivers a shock on the R wave of the QRS complex and would not be appropriate for a client in V-fib (no identifiable QRS complexes). Rhythms that are ideal for synchronized cardioversion are supraventricular tachycardia, ventricular tachycardia with a pulse, and atrial fibrillation with rapid ventricular response. If the defibrillator is not synchronized with the R wave in a client with a pulse, the shock may be delivered on the T wave and can cause V-fib or asystole. 92 NCLEX-RN study guide 100 m V. Atrioventricular Blocks Atrioventricular block (AV block) is an impaired conduction between the atria and ventricles. Remember that Sinoatrial node (SA node) is the Pacemaker, and impulses travel down to the ventricles. In an AV block, this impulses are impaired. Hence, it is imperative to determine PR interval which represents relationship between atria and ventricles. Abnormal PR ≥ 0.24 secs is AV Block. 1. First degree AV block (1° AV Block) 0.48 secs 0.48 secs 0.48 secs 0.48 secs 0.48 secs PQRST P wave: Present (1P:1QRS) PR Interval: ≥ 0.24 (consistent/same with each cycles) QRS complex: Usually normal Rhythm: Regular Rate: Variable (slow-fast) Remember: 1. All types of AVB are with PR ≥ 0.24 secs 2. PR intervals are consistent or the same with each cycles 3. Ratio: 1 P-wave is to 1 QRS complex 93 NCLEX-RN study guide 100 m 2. Second degree AV block/2° AVB (Type 1)/Mobitz 1/Wenckebach Irregular rhythm (R-R) 0.24 secs 0.32 secs 0.40 secs P-wave: No QRS 0.24 secs 0.32 secs PQRST P wave: Present (some P-waves are not followed by QRS) PR Interval: ≥ 0.24 (inconsistent/different with each cycles) QRS complex: Usually normal Rhythm: Irregular Rate: Variable (slow-normal) Remember: 1. All types of AVB are with PR ≥ 0.24 secs 2. PR intervals are inconsistent or different with each cycles (increasingly prolonged). Can have normal PR intervals. 3. Rhythm: Irregular 3. Second degree AV block/2° AVB (Type 2)/Mobitz 2 P-wave: No QRS 0.24 secs 0.24 secs 0.24 secs P-wave: No QRS 0.24 secs PQRST P wave: Present (≥2P:1QRS) PR Interval: ≥ 0.24 (consistent/same with each cycles) QRS complex: Usually normal Rhythm: Regular/irregular 94 NCLEX-RN study guide 100 m Rate: Variable (slow-normal) Remember: 1. All types of AVB are with PR ≥ 0.24 secs 2. PR intervals are consistent or the same with each cycles 3. Ratio: ≥2 P-waves is to 1 QRS complex 4. Third degree AV block/3° AVB/Complete heart block (CHB) Regular rhythm (R-R) 0.40 secs 0.52 secs 0.60 secs P-wave: No QRS 0.20 secs P-wave: No QRS PQRST P wave: Present (predominantly not associated with QRS) PR Interval: ≥ 0.24 (inconsistent/different with each cycles) P-waves not associated with QRS QRS complex: Normal/wide Rhythm: Regular Rate: Usually slow Remember: 1. All types of AVB are with PR ≥ 0.24 secs 2. PR intervals are inconsistent or different with each cycles Atria is completely independent from ventricles. There are P-waves with no QRS 3. Rhythm: Regular 95 NCLEX-RN study guide 100 m How to distinguish types of AVB? PR ≥ 0.24 secs Consistent PR Inconsistent PR 1° AVB 2° AVB (II) 2° AVB (I) 3° AVB 1P:1QRS ≥2P:1QRS Irregular Rhythm Regular Rhythm Management: See ACLS bradycardia algorithm Chronic heart blocks are treated with permanent pacemakers: 96 100 m NCLEX-RN study guide Question: Which client should the nurse assess first? 1. Client with atrial fibrillation with a new prescription for warfarin 2. Client with chronic obstructive pulmonary disease with an oxygen saturation of 91% 3. Client with postoperative pain rated 8 out of 10 4. Client with third-degree heart block with a pulse of 42/min Answer: 4 Rationale: Clients with third-degree atrioventricular (AV) block should be assessed immediately due to the potential for life-threatening consequences (e.g. shock, syncope, asystole) caused by decreased cardiac output and severe bradycardia. The client with third-degree AV block requires a permanent pacemaker. 97 NCLEX-RN study guide 100 m Common Cardiovascular Disorders Acute Coronary Syndrome (ACS) Acute coronary syndrome (ACS) encompasses a range of cardiac events, including unstable angina & acute myocardial infarction (with or without ST segment elevation). Clients with ACS require immediate treatment. ACS Stable Angina ▪ Relieved by rest ▪ Monitor Unstable Angina AMI (NSTEMI) AMI (STEMI) (-) EKG (-) Cardiac Markers Pain Mgt: ▪ Nitrates ▪ Morphine (-) ST Elevation, can have ST depression, T-wave inversion (+) Cardiac Markers Pain Mgt: ▪ Nitrates ▪ Morphine (+) ST Elevation (+) Cardiac Markers Pain Mgt: ▪ Nitrates ▪ Morphine Goal: Prevent further clot formation ▪ Antiplatelet ▪ Anticoagulant Goal: Prevent further clot formation and break down clots ▪ Antiplatelet ▪ Anticoagulant ▪ Fibrinolytics/ Thrombolytics/ TPA (window period: 30 mins-1 hr. from the start of S/S) (Proceed with PCI if >1 hour has past) 98 100 m NCLEX-RN study guide Cardiac Markers In order rising: Myoglobin: 0 - 85 ng/ml Troponin: < 0.6 ng/ml (most specific and most sensitive) CPK: 12 - 70 U/ML (m) 10 - 55 U/ml (f) AST: 10 - 50 IU/L LDH: 100 - 190 U/L EKG Changes: Common Anticoagulants and Antiplatelet: 99 NCLEX-RN study guide 100 m Anticoagulation Therapy: Heparin: antidote is Protamine sulfate aPTT: 30-40 sec (more sensitive) (1.5 – 2X is therapeutic) Risk for Bleeding: > 80 secs PTT: 25 – 35 sec (less sensitive) (1.5 – 2X is therapeutic) Risk for Bleeding: > 70 secs Warfarin (Coumadin): antidote is Vitamin K PT: 10—12 sec (1.5 – 2X is therapeutic) Risk for Bleeding: > 24 secs INR: 0.9—1.18 (up to 3X is therapeutic) Risk for Bleeding: > 3.5 secs Thrombolytics/Fibrinolytic/Tissue Plasminogen Activator (TPA): Thrombolytic therapy is aimed at stopping the infarction process, dissolving the thrombus in the coronary artery, and reperfusion of the myocardium. This treatment is used in facilities without an interventional cardiac catheterization laboratory or when one is too far away to transfer the client safely. Window period: (30 mins-1 hr. from start of s/s) Example: Alteplase, Tenecteplase, Reteplase, Streptokinase 100 NCLEX-RN study guide 100 m Contraindications: ▪ Prior intracranial hemorrhage ▪ Arteriovenous malformation (AVM): aneurysms ▪ Ischemic CVA within 3 mos. ▪ Suspected aortic dissection ▪ Active bleeding ▪ Significant head trauma within 3 mos. Percutaneous Coronary Intervention (PCI)/ Balloon angioplasty: Inflation of a balloon within the coronary artery to crush the plaque into the walls of the artery. Angioplasty is often combined with the permanent placement of a small wire mesh tube called a stent to help prop the artery open and decrease its chance of narrowing again. Preparation: ▪ Check dye allergy ▪ Check for intake of Metformin ▪ Check for intake of antiplatelets ▪ Check BUN, creatinine ▪ NPO 6-8 hours Risk: ▪ Re-narrowing of artery ▪ Blood clots ▪ Bleeding ▪ Heart attack ▪ Coronary artery damage. ▪ Acute Kidney Disease ▪ Stroke ▪ Arrhythmias Remember: Antiplatelet agents should be stopped at least 5-7 days prior to the surgery to reduce the chance of intraoperative and postoperative bleeding. 101 NCLEX-RN study guide 100 m Remember: Check BUN, creatinine and intake of metformin (anti diabetic) to patients receiving contrast dye. Kidney primarily excretes this materials Metformin: (withheld until 48 hrs. after procedure). Induces toxic accumulation of lactic acid. Aggravates renal failure 102 100 m NCLEX-RN study guide Question: The client is scheduled to have a cardiac catheterization. Which findings will cause the nurse to question the safety of the test proceeding? Select all that apply. 1. Allergy to shellfish 2. Elevated C-reactive protein 3. Prolonged PR interval on electrocardiogram 4. Serum creatinine of 2.5 mg/dL (221 µmol/L) 5. Took metformin today for type 2 diabetes Answer: 1, 4, 5 Rationale: Cardiac catheterization uses iodinated contrast to assess for artery obstruction. Contrast should be avoided in clients who have allergies to iodine or shellfish, have taken metformin within 24 hours of the procedure, or have kidney disease. Complications of IV contrast use include the following: Contrast nephropathy: Contrast that contains iodine can cause kidney injury, although this risk can be reduced with adequate hydration. However, clients with existing renal impairment (e.g. elevated serum creatinine >1.3 mg/dL [115 µmol/L]) should not receive IV contrast unless necessary for a life-saving procedure Lactic acidosis: Metformin (Glucophage) given with large-dose IV iodine contrast can increase the risk for lactic acidosis. As a result, most clinicians discontinue metformin 24-48 hours prior to IV iodine contrast exposure (regardless of baseline creatinine) and restart the drug at least 48 hours later. 103 NCLEX-RN study guide 100 m Common disorders: Infective Endocarditis Risk: Preexistent disorders ▪ ▪ ▪ ▪ Prosthetic valves Cong. heart defects Rheumatic heart disease Intravenous drug use Remember: Inflammatory type of Endocarditis is called Libman Sacks Endocarditis: related to SLE. Causative Agents: ▪ Streptococcus viridans (most common but not virulent) ▪ Staph aureus (common and virulent) ▪ Staph epidermidis Remember: High risk groups with prosthetic valves for example should have antibiotics before dental procedures. 104 NCLEX-RN study guide 100 m Splinter hemorrhages: Thin, red to reddish-brown lines of blood under the nails due to product of Ag-Ab complexes forming emboli. It runs in the direction of nail growth. Janeway lesion: non-tender, small erythematous or hemorrhagic macular lesions indicative of infective endocarditis also due to AgAb complexes. Osler’s nodes: Painful, red, raised lesions on the hands and feet caused by immune deposition from Ag-Ab complexes. Roth spots: Retinal hemorrhages with white or pale centers due dysfunction of the retinal capillaries from Ag-Ab complexes or inflammatory reactions. 105 100 m Common disorders: Myocarditis Causative Agents: ▪ Coxackie virus ▪ Parasitic/protozoal (Trypanoma cruzi): Severe case “Chagas disease” needs heart transplant NCLEX-RN study guide 106 NCLEX-RN study guide 100 m Common disorders: Pericarditis Remember: Anatomy Pericardial cavity: < 50 ml fluid: normal > 50 ml fluid: abnormal (pericardial effusion) > 150 ml fluid: cardiac tamponade Causes: ▪ Idiopathic ▪ Coxackie virus ▪ Dressler’s syndrome (Post AMI) ▪ Uremia (Urea irritates pericardium) 107 NCLEX-RN study guide 100 m Classic sign: ▪ Chest pain on lying (relieved by sitting up) ▪ Pericardial friction rub Treatment of choice: ▪ Pericardiocentesis Complication: Cardiac Tamponade Beck’s Triad ▪ Narrowed pulse pressure (Hypotension) ▪ Muffled/distant heart sound ▪ Distended neck veins 108 100 m NCLEX-RN study guide Common disorders: Rheumatic Heart Disease (RHD) Rheumatic fever: An inflammatory disease (autoimmune) that can involve the heart, joints, skin or brain. These diseases are closely associated with one another. (e.g. Rheumatoid arthritis, rheumatic heart disease, scarlet fever, impetigo, pharyngitis) and are usually triggered by Streptococcal infections (group A beta-hemolytic streptococcus, aka GABHS) Remember: Diagnostic criteria ▪ Acronym JONES (major criteria) CAFÉ PAL (minor criteria) ▪ Throat cultures for (+) GABHS, elevate Anti- streptolysin titer Remember: Autoimmune diseases are chronic condition that are triggered by infections and environmental factors causing over-activation of immune cells. Symptoms arise from this mechanism. 109 NCLEX-RN study guide 100 m Erythema marginatum: is a type of erythema (redness of the skin or mucous membranes) involving pink rings on the torso and inner surfaces of the limbs which come and go for as long as several months. Sydenham chorea: Characterized especially by involuntary movements of the face, arms, legs, and trunk (dance like movements) Root word: “Choreography” Subcutaneous nodules: Painless, small (0.5-2 cm), mobile lumps seen beneath the skin overlying the bony prominences, particularly of the hands, feet, elbows and occiput. It is a delayed manifestation of RF. 110 NCLEX-RN study guide 100 m Common disorders: Kawasaki disease (Mucocutaneous lymph node syndrome) Kawasaki disease (KD): Is a systemic vasculitis of childhood that presents with ≥5 days of fever, nonexudative conjunctivitis, lymphadenopathy, mucositis, hand and foot swelling, and a rash. Treatment: IV Immunoglobulin along with aspirin is the recommended initial treatment for Kawasaki disease, with the primary goal of coronary disease prevention. Diagnosis: CRASH & Burn 4/5 of the given criteria + Fever ≥5 days Remember: Aspirin is given to prevent coronary complication. It outweighs the risk of having Reye syndrome in children having KD. Remember: IVIG creates high plasma oncotic pressure, and signs of fluid overload and pulmonary edema develop if it is given in large quantities. Therefore, the child should be monitored for symptoms of CHF 111 100 m NCLEX-RN study guide Review of cardiopulmonary circulation Right Side of the Heart 1. Un-oxygenated blood enters the heart through the SUPERIOR & INFERIOR VENA CAVA. 2. RIGHT ATRIUM 3. Then it is squeezed through the TRICUSPID VALVE 4. RIGHT VENTRICLE 5. Then it is squeezed into the PULMONIC VALVE then to 6. PULMONARY ARTERY and enters into the lungs for oxygenation Left Side of the Heart 7. Oxygenated blood to PULMONARY VEIN 8. LEFT ATRIUM 9. Down through the BICUSPID VALVE (mitral valve) 10. Then blood is squeezed into the LEFT VENTRICLE 11. Up through the AORTIC VALVE 12. Lastly the AORTA for multi system distribution. 112 NCLEX-RN study guide 100 m Common disorders: Congenital heart defects (CHD) Acyanotic: Left-Right shunt Pressure on the left side of the heart is normally greater than right. It just simply means left – right shunt (acyanotic type) directs blood towards pulmonary artery and towards lungs for oxygenation. Cyanotic: Right-Left shunt Right – left shunt forces blood towards the aorta. Less chances of blood going to pulmonary artery for oxygenation due to defect. Left-Right shunt: Acyanotic An atrial septal defect (ASD) is a hole in the wall between the two upper chambers of your heart (atria). Blood goes back to right side because of the pressure and goes into lungs for oxygenation A ventricular septal defect (VSD) is a defect in the septum between the right and left ventricle. Blood goes back to right side because of the pressure and goes into lungs for oxygenation 113 100 m NCLEX-RN study guide Remember: Ductus arteriosus Connects the pulmonary artery with the aorta in fetal life. Closes when the newborn infant starts to breath. Prostaglandin keep the DA open. Aorta (left-higher pressure) pushes blood to pulmonary artery for oxygenation. DOC for PDA: Indomethacin (Prostaglandin inhibitor) Classic sign: continuous machinery-like murmur Coarctation of Aorta: "Coarctation" means narrowing of the aorta Classic sign: Hypertension in the arms with low blood pressure and weak pulses in the lower extremities. This due to deficient blood flow prior to coarctation. This directs more blood flow to subclavian, brachiocephalic, carotid arteries. Acyanotic type general S/S: ▪ Shortness of breath ▪ Tachycardia ▪ Tachypnea ▪ Diaphoresis ▪ Fatigue ▪ Frequent respiratory infections May not have symptoms depending on the size of the defect. Remember: Heart failure is a complication of any congenital heart defects The early signs of HF include tachycardia, tachypnea, profuse scalp or eyebrow sweating, fatigue and irritability, sudden weight gain, and respiratory distress. 114 NCLEX-RN study guide 100 m Right-Left shunt: Cyanotic Tetralogy of Fallot (TOF): TOF is made up of 4 main defects. Narrowing of the pulmonary valve (pulmonic stenosis) prevents blood from flowing to lungs for oxygenation causing the cyanosis. Multiple defect favors R-L shunting as blood backflows to right side of the heart such as overriding of aorta, VSD and right ventricular hypertrophy. Transposition of the great arteries: The two main arteries (Aorta and pulmonary artery) leaving the heart is reversed or transposed. Unoxygenated blood coming from the right side goes directly to the aorta without a chance of oxygenation Tricuspid Atresia: Complete absence of the tricuspid valve. Associated with other defects such as: ASD, PDA, VSD. Classic sign is holosystolic murmur d/t the VSD. DOC for TA: Prostaglandin (To maintain PDA). Directs blood from aorta to lungs for oxygenation 115 100 m NCLEX-RN study guide Truncus arteriosus: Occurs when the 2 major vessels (Pulmonary artery & Aorta) fails to separate completely during development, leaving a connection between them. Usually associated with VSD. Question: A nurse is assisting a new mother as she is breastfeeding her infant. The infant has been diagnosed with tetralogy of Fallot (TOF). During feeding, the infant becomes cyanotic and is having difficulty breathing. What should be the nurse's first action? 1. Administer morphine to the infant 2. Administer oxygen via mask 3. Assess infant's vital signs and pulse oximetry 4. Place the infant in the knee-chest position Answer: 4 Rationale: This infant is experiencing a hyper-cyanotic episode, or "TET SPELL," which is an exacerbation of tetralogy of Fallot that can happen when a child cries, becomes upset, or is feeding. The child should first be placed in a knee-to-chest position. Flexion of the legs provides relief of dyspnea by increasing the abdominal pressure forcing the blood back to aorta for left-right shunting via VSD. 116 NCLEX-RN study guide 100 m Common disorders: Congestive Heart Failure (CHF) Remember: Anatomy and physiology is the key Right sided: Resistance to right side d/t failure causes backflow to both large veins (vena cavas). Excess fluids pool in GI tract, liver, extremities (U/L) Left sided: Resistance to left side d/t failure causes backflow to lungs through pulmonary veins. Excess fluids causes pulmonary edema. 117 NCLEX-RN study guide 100 m Question: A client seen in the clinic with shortness of breath and fatigue is being evaluated for a possible diagnosis of heart failure. Which laboratory result will be most useful to monitor? 1. Serum potassium 2. B-type natriuretic peptide (BNP) 3. Blood urea nitrogen 4. Hematocrit Answer: 2 Rationale: B-type natriuretic peptide levels increase in clients with poor left ventricular function and symptomatic heart failure and can be used to differentiate heart failure from other causes of dyspnea and fatigue such as pneumonia. BNP is widely used in the acute care settings nowadays. The other values should also be monitored, but do not indicate whether the client has heart failure. Remember: Diuretics Potassium Sparing (SEAT): ▪ Spironolactone ▪ Eplerenone ▪ Amiloride ▪ Triamterene Potassium Wasting (BF): ▪ Bumetanide ▪ Furosemide Low Na diet: DASH (Diet Approach to Stop HTN) ▪ All foods high in sodium (>400 mg/serving) should be avoided. ▪ Do not add salt or seasonings containing sodium when preparing meals ▪ Do not use table salt ▪ Avoid high-sodium foods (e.g. canned soups, processed meats, cheese, frozen meals) ▪ Limit milk products to 2 cups daily 118 100 m NCLEX-RN study guide Common disorders: Aortic Aneurysms Aortic Aneurysm: Enlargement of the aorta to greater than 1.5 times normal size. It will cause no symptoms except when ruptured. Aortic aneurysm increases your risk of developing an aortic dissection (tearing). Aneurysm: Occurs when part of an artery wall weakens, allowing it to balloon out or widen abnormally. Abdominal aneurysm is more common than thoracic aneurysms (both are aortic aneurysms) Remember: Dysphagia is a sign of enlarging thoracic aneurysm including dull chest, collarbone and back pain Pulsatile lump with abdominal pain are signs of enlarging abdominal aortic aneurysm (AAA). S/S of shock (hypotension, tachycardia tachypnea) are signs of rupture. AAA Management: Surgically repaired when they measure about 6 cm or are causing symptoms. ▪ Femoral percutaneous placement of a stent graft (endovascular aneurysm repair) ▪ Open surgical incision of the aneurysm with synthetic graft placement. 119 100 m NCLEX-RN study guide Remember: Following repair of an abdominal aortic aneurysm, hemodynamic stability is a priority. Prolonged hypotension can lead to graft thrombosis. A falling blood pressure and rising pulse rate can also signify graft leakage. Signs of graft leakage: ▪ pain in back, pelvis, or groin ▪ ecchymosis of the groin scrotum, or penis ▪ tachycardia ▪ weak or absent peripheral pulses ▪ decreasing hematocrit and hemoglobin ▪ increased abdominal girth ▪ decreased urinary output Open vs endovascular: Open repair – A large incision in the abdomen is made to expose the aorta. Once the abdomen is opened, a graft can be used to repair the aneurysm Endovascular repair: A minimally invasive procedure via incision in the femoral artery to the aneurysm. A stent and/or graft is placed to repair the aneurysms. 120 NCLEX-RN study guide 100 m Common disorders: Aortic Dissection Aortic dissection: Occurs when the arterial wall intimal layer tears and allows blood between the inner (intima) and middle (media) layers. Results from high blood pressure that puts stress on weakened areas of the aortic wall causing tearing. Remember: An aortic dissection, which classically has moving, "ripping" back pain, is a medical emergency. Hypertension is the most important contributing factor. Remember: Extending dissection from uncontrolled HTN can cause cardiac tamponade or arterial rupture, which is rapidly fatal. Emergency treatment includes surgery (open or endovascular) and/or lowering the blood pressure. 121 100 m NCLEX-RN study guide Common disorders: Venous thromboembolism (VTE) Deep vein thrombosis vs Pulmonary embolism DVT occurs when a blood clot (thrombus) forms in one or more of the deep veins in your body, usually in your legs. Pulmonary embolism (PE) is a DVT that breaks loose and travels through the bloodstream to the lung vasculature. Death from PE is often attributed to a missed diagnosis. Early identification of risk factors can have a positive effect on client outcome. Risk Factors: Trauma, surgery (especially orthopedic, knee, hip), prolonged immobility/inactivity, oral contraceptives, pregnancy, varicose veins, obesity, smoking, and advanced age. Remember: Virchow’s Triad 1. Venous stasis 2. Vein trauma/Endothelial injury 3. Hypercoagulability 122 100 m NCLEX-RN study guide Duplex ultrasonography is the standard imaging test to diagnose DVT. D-dimer blood test: Measures a substance in the blood that is released when a clot breaks up. Indicated for suspicion of DVT, PE or coagulopathies such as disseminated intravascular coagulation (DIC). Computed tomographic pulmonary angiography (CTPA): A special type of Xray test that includes injection of contrast material (dye) into a vein. This test can provide images of the blood vessels in the lungs. Standard imaging test to diagnose PE. The areas of the tip of the arrowhead are slightly darker than the normal indicating decreased ability for contrast dye to enter pulmonary artery and its branches. This is indicative of PE. Remember: Procedure with contrast dye ▪ Check BUN, Creatinine ▪ Check intake of metformin ▪ Check for allergies to dye 123 100 m NCLEX-RN study guide Ventilation-perfusion (V/Q) scan: A specialized test that uses a radioactive substance to show the parts of the lungs that are getting 02 (ventilation scan) and getting blood flow (perfusion scan). Used when CTPA is not available or when contraindicated. Pulmonary angiography: Special type of X-ray test that requires insertion of a large catheter to femoral vein & into the pulmonary arteries, followed by injection of contrast dye through the catheter. Most accurate test to diagnose PE but invasive. 124 NCLEX-RN study guide 100 m VTE PROPHYLAXIS/ TREATMENT Pharmacologic Mechanical Unfractionated Heparin (IV) Graduated compression stocking/ted hose Low molecular weight heparin (LMWH): given SQ Intermittent pneumatic compression device Vitamin K Antagonist (PO) IVC filter Thrombolytics Thrombectomy/ Embolectomy Unfractionated Heparin Heparin Induced Thrombocytopenia (HIT) HIT occurs over several days. Report a decrease of ≥50% from baseline or a drop below 150,000/mm3. If the client has HIT, all heparin products must be stopped immediately, and a different anticoagulant should be started to prevent thrombosis risk. Remember: High Alert Medication (HAM) Most central lines require IV heparin flushes to maintain patency and prevent clotting by using single-dose vials of 2–3 mL of 10 units/mL or 100 units/ml. A dose of 1000–10,000 units is given for cases of thromboembolism. 125 NCLEX-RN study guide 100 m LMWH Heparin Monitoring: Anticoagulants LMWH (Enoxaparin): Requires monitoring of CBC, (thrombocytopenia) but not coagulation studies. Unfractionated heparin: Requires monitoring with PTT Warfarin: requires PT/INR monitoring. Remember: LMWH (Enoxaparin) Comes in a prefilled syringe. To ensure complete medication delivery, the air bubble should not be expelled prior to injection. ▪ Right or left side of abdomen, 2 inches from umbilicus ▪ Insert the needle at a 90degree angle into a pinchedup area of skin. ▪ Discourage the client from rubbing the site. Vit K antagonist Warfarin (coumadin) Warfarin: Must be taken at the same time daily to reach a therapeutic INR level. A diet high in Vitamin K (e.g. green leafy vegetables) may decrease warfarin's anticoagulant effect, (eat consistent amount). In addition, most antibiotics will increase INR by causing vitamin K deficiency. Intestinal bacteria produce Vitamin K. 126 NCLEX-RN study guide 100 m Heparin Warfarin (Coumadin) aPTT: 30-40 sec (normal range) (1.5-2X therapeutic: 45-80 sec) Risk for Bleeding: > 80 sec PTT: 25-35 sec (normal range) (1.5-2X therapeutic: 45-70 sec) Risk for Bleeding: > 70 sec PT: 10-12 sec (normal range) (1.5-2X therapeutic: 18-24 sec) Risk for Bleeding: > 24 sec Antidote: Protamine Sulfate INR: 0.9-1.18 sec (normal range) (up to 3X therapeutic: <3.5 sec) Risk for Bleeding: ≥ 3.5 sec Antidote: Vitamin K Remember: Normal vs. Therapeutic range Therapeutic range is expectedly higher than the normal range if the patient is taking anticoagulants but with certain limits. Exceeding therapeutic range increases risk for bleeding. For patients not taking anticoagulants, exceeding the normal range is ruling out liver conditions, blood dyscrasias, etc. Thrombolytics Thrombolytic agents: Indicated to resolve acute thrombotic events (e.g., ischemic stroke, myocardial infarction, massive pulmonary embolism). They are recombinant plasminogen activators (RTPA) that activate the blood fibrinolytic system and dissolve thrombi (e.g. alteplase, tenecteplase, reteplase) 127 100 m NCLEX-RN study guide Graduated compression stocking Anti-embolism stockings: Anti-embolism stockings improve blood circulation in the leg veins by applying graduated compression. When fitted properly and worn consistently, the stockings decrease VTE risk. The stockings should not be rolled down, folded down, cut, or altered in any way. If stockings are not fitted and worn correctly, venous return can actually be impeded. Intermittent pneumatic compression device Intermittent pneumatic compression device or sequential compression device (SCD): A mechanical prophylactic treatment to reduce the incidence of VTE by enhancing the blood flow in the deep veins of the legs, thereby reducing venous stasis. SCD utilize sleeves with separated areas or pockets of inflation, which works to squeeze on the appendage in a “milking action.” The most distal areas will initially inflate, and the subsequent pockets will follow in the same manner. 128 NCLEX-RN study guide 100 m IVC filter An inferior vena cava filter: A device that is inserted percutaneously, via the femoral vein. The filter traps blood clots (embolus from DVT) from lower extremity and prevents them from causing PE. Prescribed when clients have recurrent emboli or anticoagulation is contraindicated. Clients should report any metallic implants (e.g. vascular filters/coils) to the health care team prior to radiologic imaging. Thrombectomy/ Embolectomy Surgical or catheter embolectomy: Performed in patients with massive pulmonary embolism. Embolectomy is used for patients with persisting shock despite supportive care and who have an absolute contraindication for thrombolytics Thrombectomy: Involves removal of the clot in a patient with DVT. 129 NCLEX-RN study guide 100 m Question 1: A client with obesity is diagnosed with pulmonary embolism (PE). Which assessment data would the nurse expect to find? Select all that apply. 1. Bradycardia 2. Chest pain 3. Chills and fever 4. Hypoxemia 5. Tachypnea 6. Tracheal deviation Answer: 2,4,5 Rationale: A pulmonary embolus usually originates from the deep veins of the legs (>90%), travels to the pulmonary circulation, and obstructs a pulmonary artery or one of its branches, resulting in decreased perfusion in relation to ventilation and impaired gas exchange (hypoxemia). Clients are at risk for formation of venous thromboembolism (VTE) when the conditions detailed in Virchow's Triad are present (e.g. hypercoagulability, venous stasis, and endothelial damage). Clients at risk for PE include those with prolonged immobilization (e.g. during hospitalization if not ambulatory), obesity, recent surgery, varicose veins, smoking, heart failure, advanced age, or history of VTE. Characteristic of PE include: ▪ Dyspnea (85%) ▪ Pleuritic chest pain (60%) ▪ Tachycardia ▪ Tachypnea ▪ Hypoxemia ▪ Apprehension and anxiety A more atypical presentation can be associated with a larger sized PE, and may include manifestations of cardiopulmonary compromise and hemodynamic instability (e.g. right ventricular dysfunction, pulmonary hypertension, systemic hypotension, syncope, loss of consciousness, distended neck veins). 130 100 m NCLEX-RN study guide Question 2: A client with a diagnosis of atrial fibrillation has just been placed on warfarin therapy. The registered nurse (RN) overhears a student nurse teaching the client about potential food-drug interactions. Which statement made by the student nurse requires an intervention by the RN? 1. "Do you take any nutritional supplements?" 2. "You will need to monitor your intake of foods containing vitamin K." 3. "You will not be able to eat green, leafy vegetables while taking this medication." 4. "Your blood will be tested at regular intervals." Answer: 3 Rationale: Warfarin (Coumadin) works by blocking the availability of vitamin K, which is essential for blood clotting. As a result, the clotting mechanism is disrupted, reducing the risk of a stroke, venous thrombosis, or pulmonary embolism. Sudden increases or decreases in the consumption of vitamin K-rich foods could inversely alter the effectiveness of warfarin. An increase in vitamin K could decrease the effectiveness of warfarin, placing the client at increased risk of blood clot formation; a decrease could increase the effectiveness of warfarin, placing the client at increased risk for bleeding. Keep vitamin K intake consistent from day to day to keep INR/PT stable and within the recommended therapeutic range. Many medications can interfere with warfarin metabolism. Nutritional supplements may contain vitamin K, and so any new medication or nutritional supplement should be approved by the health care provider. Cranberry juice, grapefruit, green tea, and alcohol may also interfere with the effectiveness of warfarin. Rather than avoid vitamin K-rich foods, the client needs to keep vitamin K intake consistent from day to day to keep INR/PT stable and within the recommended therapeutic range. If the client enjoys vitamin K-rich foods (e.g., kale, broccoli, spinach, Brussels sprouts, cabbage, green leafy vegetables), these may be consumed in the same amounts, consistently on a daily basis. There is some evidence that a very low intake of vitamin K could decrease the overall effectiveness of warfarin. 131 NCLEX-RN study guide 100 m Common disorders: Arterial insufficiency vs Venous insufficiency Signs/Symptoms Arterial insufficiency Cause Arteriosclerosis, Atherosclerosis Incompetent valves Pain Intermittent claudication: Bilateral legs (pain relieved by rest) Pain may signify DVT; Unilateral (not relieved by rest) Color Cold Warm Swelling No Yes Hair loss Yes No Temperature Cold Warm Ulcers Circular, small and deep Location: Toes Irregular, large, superficial Location: Ankle Peripheral artery disease (PAD): Previously called peripheral vascular disease refers to arteries that have thickened, have lost elasticity due to calcification of the artery walls, and are narrowed by atherosclerotic plaques (made up of fat and fibrin). Pain (intermittent claudication) d/t decreased blood flow is the most common symptom of PAD. Venous insufficiency Chronic venous insufficiency (CVI): Refers to inadequate venous blood return to the heart. Too much venous blood remains in the lower legs, and venous pressure increases. This increased venous pressure inhibits arterial blood flow to the area, resulting in inadequate supply of oxygen and nutrients to area. DVT resulted from a clot from Virchow’s triad mechanism whereas CVI is caused by more specifically to incompetent valves 132 NCLEX-RN study guide 100 m 7 Anatomy and Physiology Respiratory 133 100 m NCLEX-RN study guide Remember: Lung coverings The volume of fluid is small, at around 15-20 ml and normally reabsorbed by lymphatic vessels. Excess fluids lead to pleural effusion. 134 NCLEX-RN study guide 100 m Normal: Bronchial/Tracheal: High pitch an loud Bronchovesicular: Moderate pitch, moderate loudness Vesicular: Low pitch and soft Adventitious: Abnormal Wheeze/rhonchi: whistling/sibilant, musical Stridor: whistling/sibilant, musical Crackles/Rales: cracking/clicking/rattling Common respiratory findings: Mediastinal shift Condition Lung sounds Vibration (tactile fremitus) Normal Bronchial, Bronchovesicu lar, vesicular Normal Resonance No Pneumonia Crackles Normal Dull None Percussion 135 NCLEX-RN study guide 100 m Pleural effusion Decreased or absent Decreased Dullness Yes if large Pneumothorax Decreased or absent Decreased Hyper resonant Yes COPD Wheezing Decreased Hyper resonant No Remember: The lung is filled with 99% air. Hence, percussion gives a resonant sound. This step helps identify areas of lung with fluid which causes dullness and air trapping causes hyperresonance. Percussion sounds in general are composed of dullness (flat organ such as liver), resonance (filled with air such as lung), tympany (filled with fluid and air like stomach). Oxygen administration: Device Flow rate Percentage of O2 (FIO2) Nasal cannula 1-4 liters Up to 40% Simple face mask 4-6 liters 40-60% Non-rebreather 10-15 liters 80-100% Venturi (venti) mask Depending on the color code Up to 60% (depending on the color code) Remember: Drying effect When the O2 flow rate is higher than 4 L/min, the mucous membranes can be dried out. The best treatment is to add humidification to the O2 delivery system. Applying water-soluble jelly to the nares can also help decrease mucosal irritation. 136 NCLEX-RN study guide 100 m Nasal Cannula Simple face mask Nonrebreather mask Remember: COPD Clients with COPD breathe in response to low arterial O2 levels (hypoxemia). If they receive more oxygen than they need to maintain an arterial saturation, the increased level can decrease the drive to breathe. Therefore, supplemental oxygen should be administered in the lowest concentration possible to maintain a pulse oxygen saturation of 90%-93% or PaO2 of 60-70 mm Hg. Non rebreather mask: Nursing care ▪ Monitoring the reservoir bag to assure continual inflation during inhalation ▪ Monitoring the 2 exhalation (flutter) valves that cover the ports on each side of the mask (valves close on inhalation to prevent entry of room air and open on exhalation to prevent re-inhalation of exhaled air. The ports should be occluded when initiating the device to fill the reservoir with oxygen) ▪ Keeping the mask secured to the face by adjusting the tightness of the head strap to minimize leaks 137 NCLEX-RN study guide 100 m Venturi mask Remember: The Venturi mask is best for COPD patients because it provides all the oxygen required in the exact amount because the device controls the mixture of room air. The fraction of inspired oxygen is therefore "guaranteed" and does not vary with changes in the client's respiratory rate, depth, or tidal volume. Positive pressure ventilation: Invasive vs non-invasive Invasive Remember: Positive pressure Positive pressure compresses the vena cavas and increases intrathoracic pressure during inspiration. This leads to less venous return, ventricular preload, and cardiac output, which results in hypotension. The hypotensive effect of PPV is greater in the presence of hypovolemia (e.g. hypovolemic shock) and decreased venous tone (e.g. septic shock, neurogenic shock). 138 NCLEX-RN study guide 100 m Modes Mechanism Mandatory/Assist control (AC mode) ▪ Previously known as Continuous Mandatory ventilation (CMV) ▪ Triggered either by the patient or mechanically by the ventilator. The ventilator is set to deliver a breath according to parameters. ▪ Can ASSIST OR CONTROL ventilation regardless of spontaneous breathing Intermittent Mandatory Ventilation (IMV): Synchronized IMV (SIMV) Spontaneous Ventilation: Pressure Support Ventilation (PSV) ▪ Regular series of breaths are scheduled but the ventilator senses patient effort and reschedules mandatory breaths based on the calculated need of the patient. ▪ Improve weaning from ventilator ▪ Any mode of mechanical ventilation where every breath is spontaneous or triggered by patient. ▪ Ventilator controls O2 amount and pressure ▪ Delivers flow and volume as needed to SUPPORT the patient breathe ▪ e.g. CPAP, BIPAP Settings Function Parameters Respiratory rate Breaths delivered per minute 4-20/minute Tidal volume (VT) Volume of air delivered during ear ventilator breath 5-15 ml/kg FIO2 Amount of O2 delivered 20-100% (to keep PO2 >60% and Saturation >90%) Inspiratory and expiratory ratio (I:E) Positive end expiratory pressure (PEEP) Length of inspiration vs expiration 1:2 or 1:1.5 Amount of pressure during end of expiration to prevent collapse 10-20 cmH20 139 NCLEX-RN study guide 100 m High Low Alarms Non-invasive CPAP vs BIPAP Continuous positive airway pressure (CPAP): Applying continuous pressure to the airways. Same on both inhalation and expiration Bi-level Positive Airway Pressure (BiPAP): Two different pressures, reduce the pressure when exhaled and increases pressure when inhaled. It helps to get more air in and out without much effort. 140 100 m NCLEX-RN study guide Question: A client has chronic obstructive pulmonary disease (COPD) exacerbation. The pulse oximeter shows a saturation of 86% on room air. The nurse assesses diminished lung sounds and low-pitched wheezing posteriorly, shallow respirations, respiratory rate of 32/min, and use of accessory muscles. What is the most appropriate oxygen delivery device for this client? 1. Nasal cannula 2. Non-rebreathing mask 3. Oxymizer 4. Venturi mask Answer: 4 Rationale: The Venturi mask is a high-flow device that delivers a guaranteed oxygen concentration regardless of the client's respiratory rate, depth, or tidal volume (TV). The adaptor or barrel can be set to deliver 24%–60% (varies with manufacturer) oxygen concentration. In the presence of tachypnea, shallow breathing with decreased TV, hypercarbia, and hypoxemia, it is the most appropriate oxygen delivery device for this client as rapid changes in inspired oxygen concentration can blunt the hypoxemic drive to breathe in clients with COPD. 141 NCLEX-RN study guide 100 m Arterial blood gas analysis (ABG) Normal Values 1. Determine if the deviation/problem is Acidosis or Alkalosis Note: Use 7.40 (mean) instead of the range (7.35-7.45) <7.40 – Acidosis >7.40 - Alkalosis 2. Identify which is responsible for the deviation. PCO2: Respiratory (Respiratory System) <35 – Alkalosis >45 - Acidosis HCO3: Metabolic (Renal System) <22 – Acidosis >26 – Alkalosis 3. After identifying, you need to know if there is compensation. Remember, ABG is about buffer system. If there is deviation then the other one must compensate. How do you know if it is COMPENSATED? If the other value opposes and attempts to neutralize (buffer): Compensated If not: Uncompensated 4. If compensated, determine if full or partial. Note: This time, refer to the range (7.35-7.45) If within 7.35 – 7.45: FULL If not within 7.35 – 7.45: PARTIAL 142 NCLEX-RN study guide 100 m Application Example: pH 7.39 PCO2 49 mmHg HCO3 28 meqs/L 1. Determine if the deviation/problem is Acidosis or Alkalosis Note: Use 7.40 (mean) instead of the range (7.35-7.45) <7.40 – Acidosis >7.40 - Alkalosis Ex: pH 7.39: ACIDOSIS (<7.40 – Acidosis) 2. Identify which is responsible for the deviation. PCO2 – Respiratory (Respiratory System) <35: Alkalosis >45: Acidosis HCO3 – Metabolic (Renal System) <22: Acidosis >26: Alkalosis PCO2 49 mmHg (ACIDOSIS): RESPIRATORY HCO3 28 meqs/L (ALKALOSIS): METABOLIC Problem: RESPIRATORY ACIDOSIS 3. After identifying, you need to know if there is compensation. Remember, ABG is about buffer system. If there is deviation then the other one must compensate. How do you know if it is COMPENSATED? 143 NCLEX-RN study guide 100 m ▪ If the other value opposes and attempts to neutralize (buffer): Compensated ▪ If not: Uncompensated HCO3 28 meqs/L (ALKALOSIS) OPPOSES? YES: COMPENSATED Problem: RESPIRATORY ACIDOSIS COMPENSATED 4. If compensated, determine if full or partial. Note: This time, refer to the range (7.35-7.45) If within 7.35 – 7.45: FULL If not within 7.35 – 7.45: PARTIAL pH 7.39 Within normal range? Yes Problem: RESPIRATORY ACIDOSIS (FULLY COMPENSATED) 144 100 m NCLEX-RN study guide Chest tube Remember: 3 aspects of chest tube drainage system Collection chamber: measures the collected fluid and also allows passage of air to the water seal. Water seal: prevents any entry of air into the thorax and measures any air exiting the system in the air leak portion of the water seal. Suction chamber: The amount of negative pressure it exert to promote suction effect (-10 to -20 cmH20) Water Seal Fluctuation is normal, continuous bubbling is air leak, absence of fluctuation can be a sign of a lung fully inflated. Suction Chamber Continuous bubbling is normal, Intermittent bubbling (check gauge), no bubbling (check connection) Remember: Chest tube drainage (50-500 mL for the first 24 hours) is expected to be sanguineous (bright red) for several hours and then change to serosanguineous (pink) followed by serous (yellow) over a period of a few days. Notify HCP: >100 mL/hour 145 NCLEX-RN study guide 100 m Remember: “Milking” Is generally contraindicated as it can cause tissue damage from highly increased pressure changes in the pleural space. It is only done if ordered and a clot/obstruction is suspected. Emergency bedside equipment: ▪ 2 chest tube clamps, ▪ 250 mL bottle of sterile H2O or NS and antiseptic wipes Remember: Clamping Chest tubes should not be clamped during transport of a client. A clamped chest tube may cause a tension pneumothorax. The chest tube is clamped only a few hours prior to removal to check for an air leak, or if the drainage system needs to be changed. Remember: Disconnection If a chest tube disconnects from the chest drainage system and cannot be reattached quickly, or if a chest drainage unit cracks or malfunctions, submerge the distal end of the chest tube 1-2 in (2-4 cm) below the surface of a 250 mL bottle of sterile H2O or saline solution. Question: The client has a chest tube for a pneumothorax. While repositioning the client for an x-ray, the technician steps on the tubing and accidently pulls the chest tube out. The client's oxygen saturation drops and the pulse is 132/min; the nurse hears air leaking from the insertion site. What is the nurse's immediate action? 1. Apply an occlusive sterile dressing secured on 3 sides 2. Apply an occlusive sterile dressing secured on 4 sides 3. Assess lung sounds 4. Notify the health care provider (HCP) 146 100 m NCLEX-RN study guide Answer: 1 Rationale: If a chest tube is dislodged from the client and the nurse hears air leaking from the site, the immediate action should be to apply an occlusive sterile dressing taped on 3 sides. This action decreases the risk for a tension pneumothorax by inhibiting air intake on inspiration and allowing air to escape on expiration 147 NCLEX-RN study guide 100 m 148 Common Respiratory Disorders Obstructive lung diseases: Asthma Asthma: Characterized by airway hyperreactivity and chronic inflammation, resulting in bronchial muscle spasm, mucosal edema, and hypersecretion of mucus. The airways narrow, resulting in increased airway resistance, air trapping, and lung hyperinflation. Remember: Asthma is a chronic disorder. It is not the most priority unless it becomes acute/ exacerbated. Expiratory wheezing is expected. However, if it says inspiratory wheezing and/or diminished lungs sounds, it’s a sign of worsening condition. Common characteristic: ▪ Use of accessory muscle ▪ Chest tightness related to air trapping ▪ Diminished breath sounds related to hyperinflation ▪ High-pitched, sibilant wheezing on expiration ▪ Tachypnea (alkalosis initially) ▪ Cough from inflamed airways ▪ Increased secretions Common asthma triggers: Allergens: Dander (e.g., cat, dog), dust mites, pollen Drugs: Beta blockers; NSAIDS (Ibuprofen, ASA) Environmental: Chemicals, sawdust, soaps/detergents Infectious: Upper RTI Intrinsic: Emotional stress, GERD Irritants: Aerosols/perfumes, cigarette smoke (including secondhand smoke), dry/polluted air. Acute exacerbation management 1. Oxygen to maintain saturation >90% 2. High-dose inhaled short-acting beta agonist (SABA) Albuterol (Ventolin) & anticholinergic agent ipratropium (Atrovent) nebulizer treatments every 20 minutes 3. Systemic corticosteroids Methylprednisolone (Solu-Medrol) Preventive management: leukotriene receptor blocker (bronchodilator, anti-inflammatory) Montelukast (Singulair) Zafirlukast (Accolate) Long-term mgt: Long acting beta-agonist (LABA) Salmeterol (Serevent) 100 m NCLEX-RN study guide Diagnosis: PEF measures severity of asthma The peak flow meter is used to measure PEFR and is most helpful for clients with moderate to severe asthma. A reading is obtained by exhaling as quickly and forcibly as possible through the mouthpiece of the device. Measuring peak expiratory flow: peak flow meter 1. Slide the indicator to the 0 or lowest level and instruct the client to sit as upright 2. Instruct the client to breathe in deeply, place the mouthpiece in the mouth, and tightly seal using the lips 3. Instruct the client to exhale as quickly and forcibly as possible, note the reading on the numbered scale 4. Repeat the procedure 2 more times with a 5–10-second rest period between exhalations 5. Record the highest reading or personal best Green Zone: 80 to 100 % of your usual or "normal" peak flow rate signals all clear. A reading in this zone means that your asthma is under reasonably good control. ▪ Continue management Yellow Zone: 50 to 80% of your usual or "normal" peak flow rate signals caution. ▪ May require extra treatment. ▪ Your symptoms can get better or worse. Contact HCP for changes in medications or management plan. Red Zone: <50 % of your usual or "normal" peak flow rate signals a Medical Alert. Severe airway narrowing may be occurring. ▪ Take your rescue medications immediately ▪ Contact HCP immediately and follow the plan they have given you for red zone readings. 149 NCLEX-RN study guide 100 m Obstructive lung diseases: Chronic Obstructive Pulmonary Disease (COPD) Emphysema Chronic bronchitis Causes ▪ Smoking (active or passive) ▪ Chemical exposure (CO, fuel, coal) ▪ Air pollution ▪ Genetics (alpha 1 antitrypsin deficiency Diagnosis Pathological: Permanent enlargement and damage to air spaces. Hyperinflated lungs with flattened diaphragm (X-ray) Clinical: Chronic productive cough that lasts for ≥ 3 months out of the year (usually winter months) and occurs in 2 consecutive years. Mechanism Damages the alveoli. These air sacs lose their elasticity, swell and some even burst. Damages the airways. Typically produces cough d/t to its effects on the mucus producing cells in the linings of the airways. Classic appearance ▪ Pink puffers (no cyanosis and does pursed lip breathing) ▪ Barrel chest (air trapping) Lung sounds Usually quiet ▪ Smoking (active or passive) ▪ Chemical exposure (CO, fuel, coal) ▪ Air pollution Blue bloaters (blue and obese) Rhonchi and wheezing Chronic obstructive pulmonary disease (COPD): Generally refers to 2 conditions, emphysema and chronic bronchitis. A combination of the 2 is common. It is the 3rd leading cause of death in the US. It occurs commonly in the age 70s. COPD is categorized by slowly progressive, persistent airflow obstruction that is closely associated with chronic airway inflammation. 150 100 m NCLEX-RN study guide Emphysema Typically called PINK PUFFERS because the normal compensatory mechanism of the patient to support breathing is to expire air in a longer period by “pursed lip”. Prolonged expiration helps expire “trapped air” Air-trapping is hallmark of airway diseases which causes build-up of CO2 Barrel Chest: d/t air trapping Normal chest A/P diameter: 2:1 (Posterior is half the dm of anterior). Emphysema 1:1 (same dm). Barrel chest, and assumption of a sitting position leaning over the nightstand are common in patients with chronic emphysema. 151 100 m NCLEX-RN study guide Chronic Bronchitis Typically called BLUE BLOATERS because patients tend to be obese and cyanotic. The chronic complication is pulmonary HTN d/t reactive vasoconstriction from hypoxemia leading to right sided CHF (fluid retention). Other complication: Polycythemia (elevated RBC) d/t chronic hypoxemia (compensatory) Chronic bronchitis vs. Acute bronchitis Chronic Bronchitis: Chronic productive cough that lasts for ≥ 3 months out of the year (usually winter months) and occurs in 2 consecutive years. Acute Bronchitis: AKA “chest cold”, is short-term bronchitis. 90% of cases are caused by viral infection, some cases are by air pollution or bacteria. Recurrence lead to chronic bronchitis COPD: Management ▪ Reduce risk factors, prevent & treat acute exacerbations, manage associated illnesses. ▪ SMOKING CESSATION ▪ Prevent infection: Influenza, pneumococcal vaccines ▪ Bronchodilators: SABA, LABA ▪ Systemic corticosteroids: Methylprednisolone ▪ Antibiotics: Macrolides (“mycins”) ▪ Mucolytics: Acetylcysteine ▪ Oxygen therapy: Noninvasive (BIPAP, CPAP) ▪ Pulmonary rehabilitation: Exercise, pursed lip breathing, “huff cough” ▪ Comfort: Morphine (improves SOB) Remember: Contraindication Codeine is a narcotic analgesic used for acute pain or as a cough suppressant. Depressing the cough reflex can cause an accumulation of secretions in COPD, leading to respiratory difficulty. Remember: Theophylline Generally cause more harm than benefit and thus are usually not recommended. But can be used as second line of treatment. Theophylline has narrow therapeutic index causing seizures and SVT. 152 NCLEX-RN study guide 100 m Remember: Use of Incentive spirometry (IS) vs “huff” cough In COPD, the pathophysiology involves structural changes and permanent airflow limitations, “AIR TRAPPING” The client needs help to expel the air, not get more air into the lungs. IS is not generally used for COPD. The low-pressure "huff" cough, which uses a series of minicoughs, is more effective in mobilizing and expectorating secretions in clients with COPD. Ladder of management: COPD 153 100 m NCLEX-RN study guide Obstructive lung diseases: Cystic Fibrosis (CF)/Mucoviscidosis Cystic Fibrosis (CF): Autosomal recessive disorder that results in a mutation of a gene that impairs chloride transport and sodium absorption, resulting in thickened secretions (dehydrated secretions) that blocks major ducts in the body. 154 100 m NCLEX-RN study guide Salty Skin: Diagnosed through sweat chloride test (SC) in the skin. > 60 mEq/L is CF. (Remember SC “senior citizen” is 60) Persistent Cough: d/t recurrent sinus & pulmonary infections-the thickened mucus inhibits normal ciliary action and cough clearance. The resulting airway obstruction can lead to frequent infections and eventual bronchiectasis. Respiratory failure is the leading cause of mortality. Bronchiectasis – recurrent infection related to CF characterized by thick secretions “layered sputum”. Most commonly associated with pseudomonas infection. Normal: moist mucus with healthy cilia CF: Thick dry mucus Bronchiectasis: layered sputum 155 100 m Foul smelling fatty (steatorrhea): d/t pancreatic insufficiency-mucus plugs in the pancreas obstruct the release of pancreatic enzymes, leading to malabsorption of nutrients (CHO, protein, fats) and fat-soluble vitamins (A,D,E, K). Bowel obstruction (meconium ileus): Often the first sign of CF in NB (inability to pass stool in 24 hrs.) d/t tenacious mucus preventing passage in the colon. Failure to thrive (FTT): d/t malabsorption and an increased metabolic rate associated with frequent infection, children with CF have difficulty maintaining adequate weight & growth Infertility: -d/t conngenital absence of vas deferens in male clients, resulting in low sperm levels and infertility. Female clients have thick cervical secretions that can obstruct sperm entry. NCLEX-RN study guide Management: ▪ Antibiotics: Aminoglycoside (tobramycin) ▪ Pancreatic enzyme supp. ▪ Diet: High in calories, fat, and protein. ▪ Chest physiotherapy ▪ Genetic testing/counseling Remember: Pancreatic enzyme Are supplements used to aid the absorption of nutrients in a child with CF. They are taken with or just before every meal (not as needed); should be swallowed whole or sprinkled on an acidic food; and should not be crushed or chewed. They should not be taken with milk. Remember: When addressing the multiple needs of a client with cystic fibrosis, airway is the priority. 156 NCLEX-RN study guide 100 m Obstructive lung diseases: Obstructive sleep apnea (OSA) Obstructive sleep apnea (OSA): Characterized by partial or complete airway obstruction during sleep that occurs from relaxation of the pharyngeal muscles. The result is repeated episodes of apnea (≥10 seconds) and hypopnea (≤50% normal ventilation), which cause hypoxemia and hypercarbia. S/S: ▪ loud snoring ▪ witnessed apnea episodes (waking with gasping or a choking sensation) ▪ morning headaches irritability ▪ excessive sleepiness Management: ▪ CPAP/BIPAP at night to keep the structures of the pharynx and tongue from collapsing backward ▪ Limiting alcohol intake at bedtime as it can cause muscles of the oral airway to relax and lead to airway obstruction ▪ Lifestyle changes: Weight loss because obesity contributes to the development of OSA, and exercise can reduce snoring. Smoking cessation ▪ Avoiding sedatives(eg, benzodiazepines, antidepressants, antihistamines, opiates) as they may exacerbate OSA and worsen daytime sleepiness 157 100 m NCLEX-RN study guide Restrictive lung diseases: Pleural effusion Pleural Effusion: Abnormal collection of fluid (>15-20 mL) in the pleural space between the parietal and visceral pleura that prevents the lung from expanding fully. This results in decreased lung volume, atelectasis, and ineffective gas exchange. Common s/s: ▪ Pain (pleurisy) ▪ SOB on exertion ▪ non-productive cough ▪ diminished breath sounds ▪ dullness to percussion ▪ decreased tactile fremitus ▪ trachea (mediastinum) deviation Common causes: ▪ Infection - Pneumonia ▪ Trauma ▪ Malignancy Management: ▪ Diuretics ▪ Chest tube thoracotomy ▪ Thoracentesis Mechanism: Fluid or air outside the lung interrupts the transmission of sound, resulting in decreased fremitus in pleural effusion and pneumothorax. Breath sounds are diminished or absent over a pleural effusion or pneumothorax. 158 NCLEX-RN study guide 100 m A thoracentesis involves the insertion of a largebore needle through an intercostal space to remove excess fluid. Thoracentesis Complications: Iatrogenic pneumothorax, hemothorax, pulmonary edema, and infection. If any abnormalities are noted, a post-procedure chest x-ray is obtained. Indications: ▪ Diagnostic: analysis of fluid including cytology, and culture to diagnose infection, malignancy, heart failure ▪ Therapeutic: removal of excess fluid (>1 L) improves dyspnea and client comfort Pulmonary edema Involved mechanisms Pulmonary edema ▪ Oncotic pressure ▪ Hydrostatic pressure ▪ Capillary permeability Cardiogenic Non-cardiogenic AKA: ARDS Acute Respiratory Distress Syndrome 159 NCLEX-RN study guide 100 m Capillary permeability: Capacity of a blood vessel wall to allow for the flow of small molecules (drugs, nutrients, water, ion, leukocytes in and out of the vessel. In an event of an inflammation, blood vessels become leaky. PUSHING PRESSURE PULLING PRESSURE Capillary hydrostatic pressure: PUSHING force that is exerted by a fluid against the capillary wall. It helps in the movement of fluid between capillaries and the interstitial fluid. Oncotic pressure: (AKA colloidal osmotic pressure) A form of osmotic pressure exerted by albumin, in a blood vessel's plasma (blood/liquid) that PULL water into the circulatory system. Hydrostatic pressure exerts more pushing force in arterial end at 35mm. Osmotic pressure at 25mm (net pressure 10mm) on the left side. Contrary to venous end (right side), osmotic pressure exerts more pulling force with constant net pressure at 10mm. The movement of fluids are controlled within the capillaries by this pressure gradients necessary to nourish tissues. In an event of conditions eg. hypoalbuminemia (albumin-maintaining gradient to oncotic pressure), pressure changes in the capillaries. The capillaries become leaky and promotes movement of fluid to interstitium (edema). In addition, arterial HTN pushes more fluid to interstitium causing the same effect. 160 NCLEX-RN study guide 100 m Cardiogenic Type Causes: ▪ Left sided CHF: promotes backflow of blood back to the lungs ▪ Hypertension ▪ Valvular disease ▪ AMI ▪ Cardiomyopathy S/S: ▪ Acute-onset DOB ▪ Tachypnea ▪ Pink, frothy sputum ▪ Diffused crackles ▪ Anxiety, restlessness Non-Cardiogenic/ARDS Causes: ▪ Sepsis: most commonly from pneumonia ▪ Acute pancreatitis ▪ Aspiration, near drowning ▪ Chest injuries ▪ Nephrotic syndrome (Hypoalbuminemia) S/S: Refractory hypoxemia: Hallmark of acute ARDS, a progressive form of acute respiratory failure that has a high mortality rate. ARDS: Massive inflammatory response that causes the lung tissue to release inflammatory mediators (leukotrienes, proteases) that cause damage to the alveolar-capillary (A-C) membrane. As a result of the damage, the A-C membrane becomes more permeable, and intravascular fluid then leaks into the alveolar space, resulting in a noncardiogenic pulmonary edema. Management: Treat the cause and relieve symptoms The priority of care is to improve oxygenation (Mechanical ventilation, O2 supplementation) or by reducing pulmonary pressure and congestion. IV Diuretics (e.g. furosemide) are prescribed to remove excess fluids. Antibiotics for sepsis are given. 161 NCLEX-RN study guide 100 m Acute respiratory failure (ARF) ARF Type I Type II Oxygenation Example: ▪ ARDS ▪ Pulmonary edema ▪ Pulmonary emboli ▪ Pneumonia ▪ Shock Ventilatory Example: ▪ COPD ▪ MG, GBS, ALS ▪ flail chest ▪ OSA ▪ Drug overdose Impaired O2 transfer Impaired CO2 elimination Impaired gas exchange (ABG) Respiratory failure: Occurs when oxygenation is inadequate (hypoxemic failure) and/or when ventilation is inadequate (hypercapnic failure). Arterial blood gas (ABG) analysis provides objective data about the efficiency of gas exchange in the lungs. Management: ▪ Treat underlying cause ▪ Mechanical ventilation ▪ Antidotes (naloxone, flumazenil) 162 100 m NCLEX-RN study guide Other diseases: Superior vena cava syndrome: An obstruction of blood flow through the superior vena cava (SVC). SVC is a medical emergency and most often manifests in patients with a malignant disease process within the thorax compressing SVC. Blockage of blood flow to the venous system of the head resulting in facial edema is a classic sign of SVC syndrome. Remember: Carbon monoxide (CO) has a much stronger bond to Hgb than oxygen does. Consequently, CO displaces oxygen from Hgb. The priority is to administer 100% oxygen using a nonrebreather mask to treat or reverse hypoxia and help eliminate CO. Levels: 10 to 20% (Headache) > 20 % (Generalized weakness) > 30% (Chest Pain) > 40% (Seizure, unconsciousness) > 60% (Coma - Death) 163 NCLEX-RN study guide 100 m Other diseases: Respiratory infections in children Condition Classic signs Nasopharyngitis “common colds” Nasal congestion with discharges, cough, sore throat, sneezing Rhinovirus, corona virus, influenza virus Epiglottitis (bacterial croup) 4 Ds: dysphonia (muffled voice), dysphagia (difficulty swallowing), drooling, and distressed respiration. Hemophilus influenzae Laryngotracheitis (viral croup) URTI symptoms, hoarseness, barking cough, stridor, respiratory distress Parainfluenza virus Bronchiolitis (viral croup) URTI symptoms, wheezing, cough, respiratory distress Respiratory syncytial virus Tripod position and epiglottitis Causative agent Remember: Epiglottitis An inflammation by bacteria of the tissues surrounding the epiglottis, a long, narrow structure that closes off the glottis during swallowing. Edema can develop rapidly (as quickly as a few minutes) and obstruct the airway by occluding the trachea. There has been a 10-fold decrease in its incidence due to the widespread use of the Hib (H. influenzae type B) vaccine. The classic symptoms: ▪ High-grade fever, severe sore throat, and the 4 Ds-dysphonia (muffled voice), dysphagia (difficulty swallowing), drooling, and distressed respiration. ▪ Tripod position opens the airway. The child should be allowed to assume a position of comfort in response to PROTECT AIRWAY. 164 NCLEX-RN study guide 100 m 8 Neurology Anatomy and Physiology CNS: Brain and Spinal cord Remember: Knowing the anatomical site and its function is vital in ruling out s/s related to certain disorders. Decussation: crossing of the corticospinal tract Describes the point where the nerves cross from one side of the brain to the other. If the tract is interrupted in the cerebrum or at any level above the pyramids of the medulla, the manifestation is contralateral side of the body (e.g. hemiplegia). 165 100 m NCLEX-RN study guide Broca’s vs Wernicke’s Illustration: language processing If a person is asking your name. 1. Wernicke’s area RECEIVES and UNDERSTANDS the information thru auditory function. (Receptive/Sensory) 2. Broca’s area generates the language so that the person can SPEAK fluently. (Expressive/Motor) 3. Motor cortex initiates the complex muscle MOVEMENTS necessary for speech. 4. Verbal output Aphasia: language deficit ▪ Receptive/sensory aphasia Unable to receive or understand the information. Lesion to Wernicke’s ▪ Expressive/motor aphasia Unable to speak fluently. Lesion to Broca’s. ▪ Global/mixed aphasia Lesion to both Wernicke’s and Broca’s 166 NCLEX-RN study guide 100 m Meninges Blood-brain barrier (BBB) Remember: Brain tissues are unique from the rest. It is made up of glial type of cells (glial-“glue”) that protects the integrity of neurons from having harmful substances. BBB is one protective mechanism which has HIGHLY SELECTIVE semipermeable border that separates the circulating blood from the brain and extracellular fluid in the CNS. Significance: The brain tissues are very sensitive to any toxic substances. If a there is a sudden change in mental status in a certain condition, there must be a break in the BBB. Remember, brain tissues are very dependent to glucose and O2 to function adequately. It is a major challenge in terms of giving medications to treat most brain disorders due to BBBs neuroprotective role. In addition, BBB functions to hinder the delivery of many potentially important diagnostic and therapeutic agents to the brain. Therapeutic molecules and antibodies that might otherwise be effective in diagnosis and therapy do not cross the BBB in adequate amounts such as treating multiple sclerosis. 167 NCLEX-RN study guide 100 m Cranial nerves Bell's palsy: is peripheral, unilateral facial paralysis characterized by inflammation of the facial nerve (CN VII) in the absence of a stroke or other causative agent/disease. Paralysis of the motor fibers innervating the facial muscles results in flaccidity on the affected side. Trigeminal neuralgia (Tic douloureux): is sudden, sharp pain along the distribution of the trigeminal nerve (CN VII). The symptoms are usually unilateral and primarily in the maxillary and mandibular branches. Clients may experience chronic pain with periods of less severe pain, or "cluster attacks" of pain between long periods without pain. 168 NCLEX-RN study guide 100 m Bell’s palsy vs Trigeminal neuralgia Bell’s palsy: S/S (sensory and motor function) ▪ Inability to completely close the eye on the affected side ▪ Flattening of the nasolabial fold on the side of the paralysis ▪ Inability to smile or frown symmetrically. ▪ Decreased tearing with extreme dryness/excessive tearing due to lower eyelid muscle weakness ▪ loss of taste on the anterior 2/3 of the tongue. Eye care: Use glasses during the day; wear a patch (or tape the eyelids) at night to protect the exposed eye. Use artificial tears during the day as needed to prevent excess drying of the cornea Oral care: Chew on the unaffected side to prevent food trapping; a soft diet is recommended. Maintain good oral hygiene after every meal to prevent problems from accumulated residual food (eg, parotitis, dental caries) 169 NCLEX-RN study guide 100 m Trigeminal neuralgia S/S (sensory and motor function): ▪ Severe, intense, burning, or electric shock-like pain depending on the zones affected Triggers: ▪ Washing the face ▪ Chewing food ▪ Brushing teeth ▪ Yawning ▪ Talking DOC: Carbamazepine (seizure medication but is highly effective for neuropathic pain). Report fever or sore throat (agranulocytosis) Care: Use a small, soft-bristled toothbrush or a warm mouth wash Use lukewarm water; avoid beverages or food that are too hot or cold. Room should be kept at an even and moderate temperature Avoid rubbing or facial massage. Use cotton pads to wash the face if necessary. High calorie soft diet; avoid foods that are difficult to chew. Chew on the unaffected side of the mouth. 170 NCLEX-RN study guide 100 m PNS: Autonomic nervous system Sympathetic NS (SNS) vs. Parasympathetic NS (PNS) ANS SNS PNS Adrenergic/dopaminergic fiber: from the prefix itself “adreno” “dopamine”, it is where adrenalines and dopamine function is involved. Sympathetic fibers are structures that transmit information to a target organ Cholinergic fiber: from the prefix itself “choline” , it is where acetylcholine is involved. Parasympathetic fibers are structures that transmit information to a target organ Catecholamines; Adrenalines (epi, norepinephrine) Dopamine: Are group of excitatory chemicals that bind to specific receptor sites in a target organ. Acetylcholine (ACH): A neurotransmitter (chemical message) released by nerve cells to send signals to target organs by binding to specific receptors sites. Adrenergic receptors: Are sites where adrenalines bind to produce a certain effect or reaction. Alpha receptors Beta receptors Cholinergic receptor: Are sites where ACH bind to produce a certain effect or reaction. Nicotinic receptors Muscarinic receptors Example: Alpha 1 & 2- smooth muscle contraction, mydriasis (pupil dilation) Beta 1 – heart muscle contraction (inotropic); increased HR (chronotropic); Increased conductivity (dromotropic) Beta 2 – smooth muscle relaxation, bronchodilation in the lungs Example: Nicotinic receptors (N) – excitation on skeletal muscle by opening Na+ channel and Na+ ions flow into the cell membrane (contraction) Muscarinic receptors (M) smooth muscle contraction (increased peristalsis) bronchoconstriction in the lungs, bradycardia, miosis (pupil constriction) FIGHT or FLIGHT (generally increased activity in response to stress) REST and REPAIR/DIGEST (generally decreased activity in response to stress) 171 NCLEX-RN study guide 100 m Organ system Eyes Salivary gland Heart Blood vessels SNS Dilation (mydriasis) Decrease production PNS Significance Constriction (Miosis) Tear production (lacrimation) Beta-adrenergic antagonists (miotic): This helps reducing the production of aqueous humor in glaucoma, e.g. TimOLOL Increase production (salivation) Pyridostigmine (Mestinon): DOC for myasthenia crisis. An anticholinesterase medication to increase ACH production. Common s/e in increase salivation. Atropine is the opposite, given to patient with cholinergic crisis (inhibit PNS effect/anticholinergic) ▪ Increase force (Inotropic) ▪ Decrease force (-) Inotropic ▪ Increase HR (chronotropic) ▪ Decrease HR (-) chronotropic ▪ Increase conductivity (dromotropic) ▪ Decrease conductivity (-) dromotropic ▪ Peripheral vasoconstriction (Increase BP) ▪ Coronary vasodilation ▪ Vasodilation to vessels of skeletal muscles (muscle contraction) ▪ Vasodilation to blood vessel in GI tract: Increase peristalsis (digestion) ▪ Vasodilation to blood vessel in penis, clitoris (erection and arousal) Anticholinergic: Atropine DOC for symptomatic bradycardia to inhibit PNS effect. Adrenergic agonist: Epinephrine, Norepinephrine, dopamine to increase SNS activity in cardiac arrest. Increase CO, HR Beta-adrenergic blocker: Decreases cardiac workload, HR, BP, conductivity Selective: antagonizes only beta 1(does not cause bronchoconstriction) e.g. metoprOLOL Non-selective: antagonizes both beta 1 & 2 (causes bronchoconstriction) e.g. propranOLOL: contraindicated in asthma Adrenergic agonist: Epinephrine, Norepinephrine, dopamine to increase SNS activity in cardiac arrest. Increase CO, HR Beta-adrenergic blocker: Decreases cardiac workload, HR, BP, conductivity 172 NCLEX-RN study guide 100 m Respiratory GI tract Genitourinary Bronchodilation (improve O2) Bronchoconstriction (decrease O2) Anticholinergic: Ipratropium (Atrovent) is a short-acting anticholinergic used as a rescue medication for COPD and asthma Short-acting beta agonist (SABA): Albuterol (Ventolin), Adrenergic agonist: Epinephrine, Norepinephrine, used to relax bronchial muscles (bronchodilation) ▪ Decrease peristalsis, HCL acid (constipation) ▪ Decrease pancreatic secretions (digestive enzymes) ▪ Decrease bile secretions ▪ Glucose production (hyperglycemia) ▪ Increase peristalsis, HCL acid (diarrhea) ▪ Increase pancreatic secretions (digestive enzymes) ▪ Increase bile secretions (digestion) Dopamine antagonist/Antiemetic: Metoclopramide (Reglan): A serious adverse effect r/t long term use of metoclopramide is tardive dyskinesia (TD) which can cause unusual uncontrollable movements. ▪ Bladder relaxation (urinary retention) ▪ Stimulates orgasm (ejaculation) ▪ Bladder contraction (urination) ▪ Vasodilation of vessels causes erection and clitoris arousal Anticholinergic: antispasmodic Oxybutynin (Ditropan): used for bladder spasms, an expected complication of the TURP procedure. They also decrease urinary urgency and frequency. The most common anticholinergic s/e are (e.g. dry mouth, constipation) 173 100 m NCLEX-RN study guide PNS: Somatic nervous system Muscle contraction: Calcium triggers release of ACH (action-potential). ACH binds to nicotinic receptors (cholinergic receptors) in the muscle cells to cause contraction. Equilibrium/balance: Acetylcholinesterase is an enzyme that degrades (breaking down) ACH to promote balance. Remember: In myasthenia gravis, ACH is unable to bind with its receptors d/t auto immune antibodies (autoimmunity) present. Increase ACH causes more acetylcholinesterase which promotes more degradation to ACH. 174 NCLEX-RN study guide 100 m Injury related disorders: Traumatic brain injury (TBI), Spinal cord injury (SCI) Traumatic brain injury (TBI) Extra-axial Intra-axial Diffuse axonal injury Meninges Brain tissues Brain tissues Epidural Arterial bleed Subdural Venous bleed Subarachnoid Arterial bleed Intracerebral Microhemorrhage Intracerebral Shearing of axons & dendrites (white matter tract) Remember: Lucid interval The client may regain consciousness quickly and feels well for some time after the injury. This transient period of well being is called a “lucid interval”, particularly in epidural hematoma. It is followed by a quick decline in mental function that can progress into coma and death 175 100 m NCLEX-RN study guide Remember: Basilar fracture An NGT must not be inserted when a basilar skull fracture is suspected. CSF leakage is an indication of this and can be evidenced by a positive halo/ring test of the blood-tinged nasal drainage (coagulated blood surrounded by CSF). Other s/s: Otorrhea, racoon’s eye, postauricular ecchymosis (battle’s sign) Remember: Clients in a coma (GCS score≤7) or with aphasia may need an advance directive to make treatment decisions because they cannot directly express their wishes. 176 NCLEX-RN study guide 100 m Autonomic dysreflexia vs spinal shock vs neurogenic shock Autonomic dysreflexia Spinal shock Neurogenic shock Mechanism Hyperreflexia: Overreaction of SNS where PNS cannot overcome. CNS is unable to control resulting to incoordination PNS: above level of injury (e.g. bradycardia) SNS: below level of injury (e.g. HTN) Hypo/Hyperreflexia (Variable): Peripheral neurons become unresponsive to stimuli. AKA “False shock” because it does not lose its sympathetic tone or to cause circulatory collapse. Loss of vasomotor tone (blood vessel tone): Loses its ability to activate the SNS and cannot trigger compensatory mechanisms. Only parasympathetic tone remains. “True shock” because it causes circulatory collapse. Level of injury T6 or above Variable T6 or above Trigger Bladder distention bowel impaction pressure ulcer Injury itself Injury itself Time Within 24 hours after injury Within 24 hours after injury Within 24 hours after injury Urgency Emergent Urgent/self-limiting Emergent BP Hypertension (≥ SBP 300 mmhg) Hyper/hypotension Hypotension HR Bradycardia Tachy/bradycardia Bradycardia RR Tachypnea Tachypnea Tachypnea Temperature Hyperthermia Hypothermia Hypothermia Other S/S ▪ ▪ ▪ ▪ ▪ ▪ ▪ Loss of reflexes below level of injury ▪ Paralysis ▪ Loss of sensation ▪ Bladder/bowel problems S/S Circulatory collapse: ▪ Decreased LOC ▪ Cold clammy skin ▪ Diaphoresis ▪ Low urine output ▪ Generalized weakness Flushing Restlessness Headache (initial) Diaphoresis Piloerection “Feeling of doom” 177 100 m Goal of treatment NCLEX-RN study guide ▪ Prevent trigger Treat the spinal cord ▪ Treat HTN (may injury (SCI) lead to AMI, CVA) ▪ Prevent organ failure (inotropes, IV fluids, ▪ Respiratory support Summary: Spinal shock is the temporary reduction or loss of reflexes following a spinal cord injury (SCI). Keep in mind that spinal shock is to SCI like fever are to infections. It means, spinal shock is merely a symptom of an underlying problem, not a disease itself. Furthermore, If the injury is T6 or above it may lead to a severe form called Neurogenic shock or Autonomic dysreflexia. To distinguish both of these severe forms, Neurogenic shock involves circulatory collapse and massive vasodilation while Autonomic dysreflexia involves massive dysfunction to ANS. 178 NCLEX-RN study guide 100 m Common neurologic disorders: Cerebrovascular accident (CVA/Stroke) CVA Etiology: Ischemic HTN, Hyperlipidemia Heart disease (CAD, Atrial fibrillation) Diabetes Sickle cell disease (SCD) (common cause of CVA in children) Etiology: Hemorrhagic HTN Ruptured aneurysm Arteriovenous malformation (AVM)/Ruptured aneurysm (Subarachnoid hemorrhages) 179 NCLEX-RN study guide 100 m Ischemic CVA Ischemic penumbra: A zone of reversible ischemia around core of irreversible infarction. Salvageable in first few hours after onset of ischemic CVA. Window period : Saving the penumbra ▪ Give thrombolytics (tissue plasminogen activator TPA) as long as within the time frame or window period IV: <3-4.5 hours Intraarterial: 6 hours Contraindications to thrombolytics: ▪ Prior intracranial hemorrhage ▪ A/V malformation (AVM) aneurysms ▪ Ischemic CVA within 3 mos. ▪ Suspected aortic dissection ▪ Active bleeding ▪ Significant head trauma within 3 mos. Remember: Permissive hypertension Maintain SBP ≥170 mmHg to ensure adequate cerebral perfusion. Usually autocorrects within 24-48 hours and does not require treatment unless the HTN is extreme (SBP >220 mm Hg or DBP >120 mm Hg) or contraindicated d/t the presence of another illness requiring strict blood pressure control (e.g., active ischemic coronary disease, heart failure, aortic dissection) Remember: Time is brain in ischemic CVA “Save the PENUMBRA” 180 NCLEX-RN study guide 100 m Hemorrhagic CVA Increase ICP in hemorrhagic CVA: An increase in intracranial pressure is considered to be a serious and life-threatening medical emergency. Primarily caused by an intracranial or subarachnoid hemorrhage (ruptured aneurysm) Normal ICP: 0 - 10 mmHg Remember: Monro-Kellie hypothesis Because of limited space in the skull, an increase in any of the component, brain tissue, blood & CSF will cause a change in the volume of the others. With disease or injury, ICP may increase. Increase ICP eventually causes decreases cerebral perfusion causes ischemia and cell death, and further cerebral edema. Early signs/symptoms: ▪ Decrease LOC (restlessness, agitation, irritability, confusion) ▪ Headache ▪ Projectile vomiting without nausea ▪ Slowed speech ▪ Pupillary changes (sluggish reaction) ▪ Temperature changes Late signs/symptoms: Deteriorating VS Cushing’s triad ▪ Irregular respiration ▪ Bradycardia ▪ Widened pulse pressure (systolic HTN) e.g.: 200/80 mmhg Rationale: The heart increases its force during contractions in response to decreased O2 in the brain. In this response, longer relaxation is needed resulting to low DBP. 181 100 m NCLEX-RN study guide Manage ICP: Other management: ▪ Pharmacologic: Mannitol and ▪ Frequent neuro assessments corticosteroids (decrease inflammation) ▪ Keep the client NPO ▪ Reduce stimulation (structured care) ▪ Seizure precautions ▪ Maintain a quiet and dimly lit environment ▪ Prevent further bleeding ▪ Limit visitors ▪ (eg. Anticoagulants, ▪ Administer stool softeners thrombolytics) ▪ Reduce exertion ▪ Ensure adequate O2 ▪ Maintain strict bed rest ▪ Assist with ADLs ▪ Maintain head in midline position Mannitol: ▪ (improve jugular venous return to the Mannitol is an osmotic diuretic heart) that can help reduce cerebral ▪ Hyperventilate and preoxygenate the edema and ICP through use of client for brief periods such as before a hyperosmolar solution to suctioning to help reduce ICP draw water from the brain ▪ Manage pain well without sedating the tissues and extracellular fluid, client too much ▪ Treat fever aggressively (cool sponges) but allowing excretion in a form of diuresis. avoid having the client shiver or shake Neuromuscular disorders: Myasthenia gravis (MG) Muscle contraction: Calcium triggers release of ACH (action-potential). ACH binds to nicotinic receptors (cholinergic receptors) in the muscle cells to cause contraction. Equilibrium/balance: Acetylcholinesterase is an enzyme that degrades (breaking down) ACH to promote balance. Remember: In myasthenia gravis, ACH is unable to bind with its receptors d/t auto immune antibodies (autoimmunity) present. Increase ACH causes more acetylcholinesterase which promotes more degradation to ACH. 182 100 m NCLEX-RN study guide Myasthenia gravis: An autoimmune disease involving a decreased number of acetylcholine (ACH) receptors at the neuromuscular junction. As a result, there is fluctuating weakness of skeletal muscles, most often presented as: ▪ Ptosis/diplopia ▪ Bulbar signs (difficulty speaking or swallowing) ▪ Difficulty breathing. Muscles are stronger in the morning and become weaker with the day's activity as the supply of available acetylcholine is depleted. Remember: Airway and breathing are the priority in neuromuscular disorders. It is also important to know the anatomy and physiology of neurologic system to determine the symptoms related to the condition. (e.g. GBS affects Autonomic NS, MG affects Somatic NS) Remember: Bulbar muscles Are muscles involving speaking and swallowing. These are the main problems in MG and ALS occurring with the mouth, tongue and swallowing muscles. In a descending manner, it affects the respiratory muscles. Remember: Dysphagia (difficulty swallowing) and Dysarthria (difficulty of speaking) are signs of impending respiratory failure DOC: Pyridostigmine (Mestinon) given before meals so that the client's ability to swallow is strongest during the meal. Tensilon test: Edrophonium HCL Done by injecting the drug Tensilon into a vein and observing for rapid improvement of strength, usually of eye muscles. Improvement in strength of speech may also be considered a positive test. Primarily because Tensilon is an anticholinesterase. 183 NCLEX-RN study guide 100 m Myasthenic crisis Cause/mechanism Signs/symptoms Drug of choice Cholinergic crisis ▪ Undermedication ▪ Disease exacerbation Disease process: ↑ acetylcholinesterase ↓ acetylcholine ▪ Overmedication ▪ ↓ acetylcholinesterase ▪ ↑ acetylcholine ▪ Severe muscle weakness ▪ Dysarthria ▪ Dysphagia ▪ Tachycardia Respiratory failure ▪ ▪ ▪ ▪ ▪ ▪ ▪ Pyridostigmine (Mestinon): anticholinesterase Intubation Atropine sulfate: anticholinergic Intubation Muscle weakness Bradycardia Hypotension Constricted pupils Sweating Abdominal pain Respiratory failure Amyotrophic lateral sclerosis (ALS)/ Lou Gehrig disease Amyotrophic lateral sclerosis (ALS)/ Lou Gehrig disease: Is a debilitating, progressive neurodegenerative disease with no cure and death usually occurs within 5 years of diagnosis.. Characterized by the progressive loss of motor neurons in the brainstem and SC. Clients have spasticity, muscle weakness, and atrophy. Neurons involved in swallowing and respiratory function are eventually impaired, leading to aspiration, respiratory failure, and death. Care of clients with ALS focuses on maintaining respiratory function, adequate nutrition, and quality of life. 184 100 m NCLEX-RN study guide Symptoms : ▪ Fatigue ▪ Progressive muscle weakness ▪ Twitching and muscle spasms ▪ Bulbar signs ▪ (Dysphagia, dysarthria) Respiratory failure DOC: Riluzole (Rilutek) slows the progression of ALS by slowing glutamate production. The only medication approved for ALS treatment. Thought to slow neuron degeneration by decreasing the production and activity of the neurotransmitter glutamate in the brain and SC. Management: ▪ Respiratory support with noninvasive positive pressure BiPAP or CPAP or invasive mechanical ventilation (eg. via tracheostomy) ▪ Feeding tube for enteral nutrition ▪ Medications to decrease symptoms (eg. spasms, uncontrolled secretions, dyspnea) ▪ Mobility assistive devices (eg. walker, wheelchair) ▪ Communication assistive devices (eg. alphabet boards, specialized computers) 185 100 m NCLEX-RN study guide Multiple Sclerosis (MS) Symptoms: ▪ Diplopia, Optic neuritis, Muscle weakness, Spasticity, Paresthesia, Incoordination, Loss of balance, Fatigue, Impaired mobility ▪ Lhermitte’s sign ▪ Respiratory failure Charcot’s Triad: ▪ Intentional tremors ▪ Nystagmus ▪ Scanning speech (staccato speech) Management: ▪ Steroids (Immune suppression) ▪ Plasmapheresis ▪ Prevent exacerbation Multiple sclerosis (MS): Is a chronic relapsing and remitting nerve disorder caused by patchy demyelination of nerve fibers in the brain and spinal cord causing a variety of symptoms. MS is thought by many medical researchers to be an autoimmune disease. In MS, attacks are against the fatty myelin coating that surrounds and insulates nerve cells (a process called demyelination), resulting in lesions. The immune response can be triggered by infection to Epstein barr virus. Remember: MS affects the entire nervous system, which means the manifestations is a variety. Lhermitte’s sign: Is a physical exam maneuver that is considered to have a positive result when a patient experiences an electric-like shooting pain that radiates from the back of the neck down the back when the neck is bent forward. 186 NCLEX-RN study guide 100 m Guillain-Barre Syndrome (GBS) Management: Measurement of forced vital capacity (FVC) is the gold standard for assessing ventilation; a decline in FVC indicates impending respiratory arrest requiring endotracheal intubation. Others: Plasmapheresis, IV immunoglobulins Guillain-Barre Syndrome (GBS): Is an acute, immune-mediated polyneuropathy (autoimmune) that is most often accompanied by ascending muscle paralysis and absence of reflexes. Lower-extremity weakness progresses over hours to days to involve the thorax, arms, and cranial nerves (CNs). Neuromuscular respiratory failure is the most life threatening complication. In its most severe form GBS is a medical emergency. The exact cause is unknown. But it is often preceded by an infectious illness such as a respiratory or stomach infection (Campylobacter jejuni) Remember: GBS affects the peripheral nervous system (PNS), which distinguishes the condition from MS, which affects the entire nervous system. However, both can cause demyelination. Symptoms: ▪ Prickling, pins and needles sensations in your fingers, toes, ankles or wrists ▪ Weakness, Unsteady gait ▪ Difficulty with eye or facial movements, Dysarthria, Dysphagia, Severe pain (cramp like and may be worse at night) ▪ Impaired bladder/bowel control ▪ Tachycardia ▪ Hypo/hypertension ▪ Respiratory failure Early signs of impending respiratory failure include: ▪ Inability to cough ▪ Shallow respirations ▪ Dyspnea and hypoxia ▪ Inability to lift the head or eye brows 187 NCLEX-RN study guide 100 m Myasthenia Gravis (MG) Amyotrophic Lateral Sclerosis (ALS) Multiple Sclerosis (MS) Guillain-Barre Syndrome (GBS) Autoimmune Triggers: GI infections (C. jejuni) Respiratory Infections Autoimmune Thymoma Genetic (active T-cells) Unknown ↑ A-cholinesterase ↑ Glutamate ↓ ACH Autoimmune Triggers: Somatic NS Voluntary muscles Somatic NS Voluntary muscles Entire nervous system ▪ Muscle weakness ▪ Ptosis/diplopia ▪ Bulbar signs: dysarthria, dysphagia ▪ Muscle weakness ▪ Diplopia, Optic neuritis, Muscle weakness, Spasticity, ▪ Muscle Paresthesia, weakness with Incoordination, atrophy Fatigue ▪ Progressive Loss of balance, muscle Fatigue, weakness Impaired ▪ Twitching & mobility muscle spasms ▪ Mental deficit ▪ Bulbar signs: ▪ Depression dysarthria, Lhermitte’s sign dysphagia Respiratory failure Charcot’s Triad: ▪ Intent. tremors ▪ Nystagmus ▪ Scanning speech Complication Respiratory failure Myasthenic & Cholinergic crisis Respiratory failure Respiratory failure Respiratory failure Tests Tensilon test: Edrophonium HCL Electromyography MRI, CSF studies Electromyography Etiology/ Mechanism NS affected Signs/symptoms Epstein Barr Demyelination Demyelination (ascending) Peripheral NS (ANS, Somatic NS) ▪ Muscle weakness ▪ Severe pain Prickling sensation ▪ Unsteady gait ▪ Difficulty with eye or facial movements ▪ Bulbar signs: dysarthria, dysphagia ▪ Impaired bladder/bowel control ▪ Tachycardia ▪ Hypo/HTN 188 NCLEX-RN study guide 100 m Management ▪ Pyridostigmine (Mestinon) ▪ O2 Support for exacerbation ▪ Supportive management ▪ Riluzole (Rilutek) ▪ Respiratory support ▪ Supportive management ▪ Steroids (Immune ▪ Measurement of suppression) FVC ▪ Plasmapheresis ▪ Plasmapheresis (removing (removing autoimmune autoimmune cells) cells) IVIG ▪ Prevent ▪ Prevent exacerbation infections ▪ Stress mgt 189 NCLEX-RN study guide 100 m 9 ACLS algorithms: 1. Bradycardia Remember: H’s and T’s ▪ Hypovolemia ▪ Hypoxia or Hypoxemia ▪ Hydrogen Ion (Acidosis) ▪ Hypo/Hyperkalemia ▪ Hypothermia ▪ ▪ ▪ ▪ ▪ Tamponade (Cardiac) Toxins (overdose) Tension Pneumothorax Thrombosis (Pulmonary) Thrombosis (Coronary) Transvenous Pacing Critical care Remember: H’s and T’s The H’s and T’s of ACLS is a mnemonic used to help recall the major contributing factors to pulseless arrest including PEA, Asystole, Ventricular Fibrillation, and Ventricular Tachycardia. Most commonly associated with PEA, but they will help direct your search for underlying potentially reversible causes to any of arrhythmias associated with ACLS. 190 NCLEX-RN study guide 100 m 2. Tachycardia Remember: This algorithm is for HR ≥ 150 bpm. This might be one of the several tachycardia rhythms: SVT, Atrial fibrillation, Atrial flutter, V-tach (with pulse). Remember: The distinction between regular and irregular rhythm (SVT vs. Rapid A-fib) is fundamental since they are treated differently. For instance, adenosine (drug of choice for SVT) cannot be given to a patient with A-fib because it causes further fatal arrhythmias. Atrial Flutter SVT Atrial Fibrillation V-tach (with pulse) Torsades da pointes V-fib 191 NCLEX-RN study guide 100 m 3. Ventricular tachycardia (pulseless) Ventricular fibrillation Remember: Basic airway management involves head tilt, chin lift technique. On the other hand, advanced airway involves invasiveness using LMA, laryngeal tube, and ET tube with special techniques and training. D C Remember: CPR & defibrillation are highest priority over advanced airway The value of securing the advanced airway (LMA, laryngeal tube, and ET tube), must be balanced against the need to minimize the interruption in perfusion in the early steps of resuscitation. E A ROSC is resumption cardiac perfusion with significant respiratory effort after cardiac arrest. Signs of ROSC include breathing, coughing, or movement and a palpable pulse or a measurable BP 192 Remember: CDEA vs DCEA CDEA: UNWITNESSED arrest DCEA: The importance of early defibrillation is irrefutable in a WITNESSED arrest (sudden change in patients status to pulseless v-tach and v-fib). NCLEX-RN study guide 100 m 4. Pulseless electrical activity (PEA) Asystole Remember: PEA PEA occurs when you see a rhythm on the monitor that would normally be associated with a pulse, however the patient is pulseless. The rhythm can be anything, at any heart rate Remember: PEA is most commonly associated with H’s and T’s ▪ Hypovolemia ▪ Hypoxia or Hypoxemia ▪ Hydrogen Ion (Acidosis) ▪ Hypo/Hyperkalemia ▪ Hypothermia ▪ ▪ ▪ ▪ ▪ Tamponade (Cardiac) Toxins (overdose) Tension Pneumothorax Thrombosis (Pulmonary) Thrombosis (Coronary) 193 NCLEX-RN study guide 100 m Sepsis: A leading cause of mortality in critical care Mild 1. SIRS (at least 2/4 criteria) T: ≥100.4 F [38 C]) or ≤96.8 F [36 C]) HR: ≥90/min RR: ≥20/min or alkalosis (PaCO2 ≤32 mm Hg WBC: ≥12,000/mm3 or ≤4,000/mm3 or ≥10% immature neutrophils (bands cells) normal is 3.5% 2. Sepsis SIRS + Identified causative agent (eg. Pneumonia, UTI) 3. Septic shock SIRS + Sepsis + Hypotension (SBP ≤ 90 mmhg) 4. MODS SIRS + Sepsis + Septic shock + Multi organ system dysfunction Severe Sepsis continuum SIRS: Systemic inflammatory response syndrome (SIRS) occurs when the body undergoes a major insult (eg. trauma, infection, burns, hemorrhage, multiple transfusions). Stimulation of the immune response leads to activation of WBCs, release of inflammatory mediators, increased capillary permeability, and inflammation of organs. Sepsis: Sepsis is an exaggerated systemic inflammatory response associated with a documented or suspected infection. Septic shock: Sepsis-induced hypotension despite fluid resuscitation (30 mL/kg) or 2L bolus is defined as "septic shock." In addition, inadequate tissue perfusion (ie. ↑serum lactate) despite fluid resuscitation and decreased CVP and pulmonary artery wedge pressure also indicate the presence of septic shock. Stages of septic shock: 1: Reversible (aerobic to anaerobic) 2: Compensatory (homeostasis) sympathetic response 3: Failed compensation 4: Irreversible (beginning organ damage) MODS: Multi Organ Dysfunction Syndrome is the failure of 2 or more body organs (e.g. acute kidney injury, ARDS). MODS occurs in related to decreased perfusion is the end point of the sepsis continuum. It is important for the nurse to recognize manifestations of SIRS to promote early recognition, prevention, & treatment of infection and to limit its progression to MODS. Sepsis continuum 194 NCLEX-RN study guide 100 m Central lines: Central venous catheter CVC vs. Arterial line (A-line) Central lines Central venous lines Common sites: Subclavian (SC) Intrajugular (IJ) Purpose: ▪ Medications ▪ Parenteral nutrition, ▪ Chemotherapy ▪ Plasmapheresis ▪ Dialysis ▪ Blood draws ▪ Need for IV therapy when peripheral venous access is impossible ▪ Blood transfusion ▪ CVP monitoring Arterial lines Common sites: Radial arteries Femoral arteries Purpose: ▪ Monitor BP directly in real-time ▪ Obtain ABG sample Arterial lines are generally not used to administer medication, since many injectable drugs may lead to serious tissue damage. Golden rule (Allen’s Test): there has to be collateral circulation to the area affected by the chosen artery, so that peripheral circulation is maintained. 195 100 m Nursing care for CVC: ▪ A 10 mL syringe is generally preferred for administering medications through a CVC. ▪ CVCs require IV heparin flushes to maintain patency and prevent clotting. (Single-dose vials of 2–3 mL of 10 units/mL or 100 units/mL) Remember: A dose of 1000–10,000 units is given for cases of VTE. ▪ Prime tubing before insertion to prevent air embolism ▪ Dressing changes (7 days) using tegaderm transparent dressing and PRN ▪ Use mask when dressing changes Preventing air embolism when discontinuing a CVC: ▪ Instruct the client to lie in a supine position. This will increase the CVP and decrease the possibility of air getting into the vessel ▪ Instruct the client to bear down or exhale. The client should never inhale during removal of the line; inhalation will suck more air into the blood vessel via negative suction pressure ▪ Apply an air-occlusive dressing (usually gauze with a Tegaderm dressing) to help prevent a delayed air embolism. If possible, the nurse should attempt to cover the site with the occlusive dressing while pulling out the line (Option 1). ▪ Pull the line cautiously and never pull harder if there is resistance. Doing so could cause the catheter to break or become dislodged in the client's vessel NCLEX-RN study guide Nursing care for central lines: Preventing CLABSI ▪ Comply hand hygiene religiously ▪ Avoid femoral site in obese adult patients. ▪ Prepare the insertion site with >0.5% chlorhexidine with alcohol. ▪ Immediately replace dressings that are wet, soiled, or dislodged – NO WET DRESSING ▪ If blood or blood products or fat emulsions are administered change tubing every 24 hours. ▪ Promptly remove unnecessary central lines ▪ Perform daily audits to assess whether each central line is still needed Allen’s Test before arterial line insertion: The patency of the ulnar artery must be confirmed by performing a modified Allen's test to assure adequate circulation to the hand before proceeding with the radial arterial insertion 1. Instruct the client to make a tight fist (if possible) 2. Occlude the radial and ulnar arteries using firm pressure 3. Instruct the client to open the fist; the palm will be white if both arteries are sufficiently occluded 4. Release the pressure on the ulnar artery; the palm should turn pink within 15 secs as circulation is restored to the hand, indicating patency of the ulnar artery (positive Allen's test) If the Allen's test is positive, the arterial insertion can be done; if negative and the palm does not return to a pink color, an alternate site (eg. brachial artery, femoral artery) must be used. Summary: It is important to distinguish central lines in critical care. Central venous catheter (CVC) uses the venous system to provide direct access to the heart with the indications mentioned above. On the other hand, arterial line provides access to the heart through arteries using shorter catheter contrary to CVC. Arterial lines are short to prevent unnecessary obstruction to arterial circulation. In terms of monitoring hemodynamics, both of these central lines use the same set-up. 196 NCLEX-RN study guide 100 m Hemodynamic monitoring: Set-up for CVC and Arterial line Monitor: Shows the pressure reading Fast-flush (aka) Square wave test: Perform a dynamic response test (square wave test) using the fast flush valve every 8-12 hours, when the system is opened to air or when accuracy of measurements is questioned. This test helps to verify if the arterial line is functioning correctly. Square wave because when flushing the line, the wave forms turn into square in the monitor. Pressure bag: Inflating the pressure bag to 300 mm Hg regularly helps prevent backflow of blood to transducer Saline: Fluid inside the pressure bag which maintains patency of the line Transducer: Reads fluctuations of pressure from the heart. Zeroing: Leveling or positioning the transducer to baseline or to phlebostatic axis. Phlebostatic axis: At the 4th ICS, at the midway point of the AP diameter (½ AP)of the chest wall. Zeroing stopcock of the transducer system must be placed at the phlebostatic axis If the transducer is placed too low, the reading will be falsely high; if placed too high, the reading will be falsely low. This concept is similar to the positioning of the arm in relation to the level of the heart when measuring blood pressure indirectly using a sphygmomanometer or noninvasive blood pressure monitoring device. The upper arm should be at the level of the phlebostatic axis 197 NCLEX-RN study guide 100 m Hemodynamic monitoring: Pulmonary artery catheter (Swan-Ganz) Pulmonary artery catheterization (Swan-Ganz): AKA right heart catheterization, is the insertion of a catheter into a pulmonary artery. Its purpose is diagnostic; detects CHF etc. The PAC allows direct, simultaneous measurement of pressures in the right atrium, right ventricle, pulmonary artery, and the filling pressure ("wedge" pressure) of the left atrium. Remember: Right heart catheterization is PAC (venous approach). Whereas, left heart catheterization (arterial approach) refers to conventional cardiac catheterization used to diagnose and treat blockages (e.g. AMI, CAD) Technique: The catheter is introduced through a large vein (IJ, SC, femoral). The passage of the catheter is monitored by dynamic pressure readings from the catheter tip. Readings will show in the monitor depending on the site of the catheter tip as it advances to right atrium, the right ventricle, and subsequently into the pulmonary artery. The balloon, when inflated causes the catheter to "wedge" (force into a narrow space) in a small pulmonary blood vessel. Ideally, this measures CHF by measuring left ventricular function and ventricular preload. CVP/RAP: 2–8 mmHg RVP: 15–25 mmHg (systolic) PCWP: 8-13 mmHg PAP: 20-30 mmHg 198 NCLEX-RN study guide 100 m Pulmonary artery catheter Balloon: Should be inflated for only 10-15 seconds and then allowed to deflate passively. A balloon that is inflated for a long period may cause PA rupture. Locking the balloon port of the PA catheter will prevent the balloon from being accidentally inflated. Thermistor port: Connected to the cardiac output computer. Measures core blood temperature. Balloon port: Cannot be connected to a pressure monitoring system. Used to inflate the balloon at the tip of the PA catheter, allowing for the measurement of PA wedge pressures. Special syringe is used (1-3 ml). Always lock the balloon port. Proximal port: Connected to a pressure monitoring system to measure CVP because its lumen exits into the right atrium. Distal port: Connected to a pressure monitoring system to measure PA pressure because its lumen exits into the PA. Remember: PA catheterization Conventionally, PAC is utilized 3-5 days. Its usage is limited due to its controversy in the recent times due to risk of injury (eg. PA rupture). There is growing evidence the use of PAC does not necessarily lead to improved outcome in ICU because there are available test measuring heart function. Hospital based catheter infections clearly limits the usage of this type of invasive ICU procedure. 199 100 m NCLEX-RN study guide 200 Peripherally inserted central line (PICC): Commonly used for long term antibiotic administration, chemotherapy, and total parenteral nutrition (TPN). PICC lines can be left in for weeks or months. Complications related to the PICC are occlusion of the catheter, phlebitis, air embolism, and infection due to bacterial contamination. Care approach is similar to central lines. PICC vs Midline Catheter: Midline catheter are not central lines. It is considered as a peripheral line. However, both has lower incidences of infections Chest Ports: Port-a-cath or Mediport: Consists of a reservoir compartment (portal) that has a silicone bubble for needle insertion (septum), with an attached plastic tube (catheter). Surgically inserted under the skin in the upper chest or in the arm and appears as a bump under the skin. Ideally, the catheter terminates in the superior vena cava or the right atrium. Most commonly used for chemotherapy, antibiotics, BT, blood draws. Permacath: Double lumen dialysis catheter placed in the jugular vein. It is tunneled under the skin along the upper chest under collar bone and the end of the catheter will come out about 4 inches (10cms). Permacath is temporarily used for hemodialysis until a permanent access has time to "mature" AV graft or AV fistula. Although it can last up to 12 months. Trialysis catheter has its 3rd lumen used for CVP monitoring, blood draws ,medication & contrast administration 100 m NCLEX-RN study guide Question: The nurse working in an intensive care unit receives a prescription from the primary health care provider to discontinue a triple-lumen subclavian central venous catheter. Which interventions will help prevent air embolism on removal? Select all that apply. 1. Applying an air-occlusive dressing 2. Instructing the client to bear down 3. Instructing the client to lie in a supine position 4. Pulling the line harder if there is resistance 5. Pulling the line out when the client is inhaling Answer: 1, 2, 3 Rationale: To prevent air embolism when discontinuing a central venous catheter, it is important for the nurse to pull the line cautiously, have the client in a supine position to increase the CVP and decrease the possibility of air getting into the vessel, have the client bear down or exhale (inhalation will suck more air into the blood vessel via negative suction pressure), and apply an air-occlusive dressing while pulling out the line. 201 NCLEX-RN study guide 100 m 10 Renal Anatomy and Physiology Cardiac output: Renal system The renal system receives blood about 20-25% (1L) of the total CO. About 10% (100 ml) is subject for filtration and cleared in a form of urine AKA glomerular filtration rate (GFR). Creatinine clearance is basically GFR. The main function of kidneys is to excrete waste which is more specific to creatinine. This means that elevated creatinine is a specific sign of a failing renal system. Ureter: Is a tube that carries urine from the kidney to the urinary bladder. Bladder: A hollow and elastic organ which stores the urine produced by the kidneys. Residual amounts >100 mL should be reported (urinary retention) Urethra: A duct that transmits urine from the bladder to the exterior of the body during urination. Creatinine clearance: GFR Normal is approximately 100 ml/min. There is 1 ml of creatine cleared in 1 ml of blood filtered (1:1). In kidney injury, there is decreasing creatinine clearance (e.g. 50 ml/min). If the kidneys are expected to clear 100 ml/min of creatinine, where is the other 50 ml/min? It went back to serum which subsequently increases the serum or blood creatinine levels. <GFR is <creatine clearance = kidney injury 202 100 m NCLEX-RN study guide Functions: 1. Acid – base balance 2. Fluid and electrolyte balance (Regulation of osmolality) 3. Hormones & enzyme secretions Erythropoietin (RBC production) Calcitriol (Calcium absorption) Renin (BP regulation) 4. Excretion of waste Formation of urine Acid-base balance: The lungs contribute to acid-base homeostasis by regulating carbon dioxide (CO2) concentration. Mixed with H20 to form carbonic acid (H2CO3). It dissociates to form Hydrogen ions (H+) and bicarbonate (HCO3). Kidneys reabsorb and regenerate HCO3 from urine to neutralize blood, and to excrete H+ ions to prevent blood from become acidic. Osmolality: Concentration An increase in osmolality causes the posterior pituitary gland to secrete antidiuretic hormone (ADH), resulting in water reabsorption by the kidney and an increase in urine concentration. Remember: Water is a diluent. The two factors work together to return the plasma osmolality to its normal levels. Implications: In a presence of disease, the kidneys are not able to excrete H+ ions making the blood acidic. H+ ions are powerful acidifying agents (power of hydrogens: pH). Acidosis is hyperkalemia: To reduce the acidity of your blood, H+ ions move from your circulation into your cells in exchange for K+. Movement of K+ from cells causes hyperkalemia. Remember: Human cells are irritated with acids. Hyperkalemia causes serious arrhythmias. Dialysis is indicated. Implications: In a presence of disease, the kidneys are not able regulate blood osmolality. Fluid volume overload is the subsequent symptom that may eventually cause pulmonary edema. Fluid volume overload contributes to elevated BP found in chronic kidney disease (CKD). 203 NCLEX-RN study guide 100 m Secretion of hormones: Erythropoietin: Stimulates erythropoiesis (production of RBC) in the bone marrow. Calcitriol: Activated form of vitamin D, promotes intestinal absorption of calcium and renal phosphate reabsorption. Renin: An enzyme which regulates angiotensin and aldosterone levels (RAA System) which regulates blood pressure. Implications: In CKD, erythropoietin synthesis is decreased causing anemia. Hypocalcemia is due to decrease secretion of calcitriol. In addition, elevated BP is due to abnormal regulation of ADH and abnormal renin-angiotensin-aldosterone mechanism causing retention or reabsorption of sodium and water. Patient is at risk for developing CHF. Renin – angiotensin – aldosterone system: Elevating blood pressure in response to dehydration, renin is produced by kidneys. Angiotensin 1 is not a potent vasoconstrictor so angiotensin converting enzyme (ACE) is needed to convert angiotensin 1 to angiotensin 2 (potent vasoconstrictor) causing BP elevation. Aldosterone promotes H20 and Na+ retention (close relationship of Na+ and H20) causing hypernatremia and elevated BP. K+ and H+ are excreted by kidneys causing hypokalemia and alkalosis. This also explains the inverse proportion of sodium and potassium. 204 100 m NCLEX-RN study guide Urine formation: Excretion of waste through the nephrons (functional units of kidneys) 1. Filtration: The process by which cells and LARGE PROTEINS are retained while small materials pass through glomerulus and eventually becomes urine. Waste products must be excreted to urine. Hydrostatic pressure pushes fluids and materials through the capillary networks of the glomerulus. Remember: Damaged glomerulus are not able to filter waste products well and retains them to the circulation (↑Crea, BUN etc.) Large proteins are excreted in the urine causing proteinuria and hypoalbuminemia consequently. which causes interstitial edema, a common manifestation in kidney disorder (albumin maintains fluid in the serum). 205 100 m 2. Reabsorption: The transport of molecules that passed through glomerular membrane back into the peritubular capillary. H2O is 55% reabsorbed in the proximal tubule. Glucose and amino acids are reabsorbed in the proximal tubule. Reabsorption happens in proximal tubule, descending & ascending loop of Henle, distal convoluted tubule, collecting tubules. Remember: Loop diuretics (Furosemide, Bumetanide, Torsemide) act in the loop of Henle to inhibit Na+, Ch- and K+ reabsorption thereby causing diuresis/excretion (wasting K+). However, K+ sparing diuretics (Spironolactone) antagonizes aldosterone effects, preventing Na+ reabsorption and preventing K+ excretion. 3. Secretion: The reverse of reabsorption in which molecules are transported from the peritubular capillary through the interstitial fluid. This is the process of cleaning the blood by moving the harmful molecules (ammonium, some K+, H+ ions) back to tubules to for excretion making urine acidic. 4. Excretion: The last step in forming the urine is excretion. Waste is excreted in the form of a clear pale yellowish-colored urine. Remember: All waste products are acidic. Retention of these products due to abnormal regulation of the kidneys results to metabolic acidosis. Hence, it causes harm to most human cells. Any form of acidosis is way more harmful than alkalosis. NCLEX-RN study guide 206 100 m NCLEX-RN study guide 207 Common renal disorders: Acute kidney injury (AKI) Acute kidney injury (AKI): Previously known as Acute renal failure (ARF) Is sudden damage to the kidneys (< 3 months) characterized by rapid reduction in kidney function, based on serum BUN, creatinine, or based on a rapid reduction in urine output, oliguria (less than 400 ml/24 hours). It can range from minor loss of kidney function to complete kidney failure. The cause is before the kidneys: ↓ blood flow ↓ blood filtered Absolute fluid loss: Hypovolemic shock ▪ Major hemorrhage ▪ Dehydration (diarrhea, persistent n/v) ▪ Burns Relative fluid loss: Distributive shock ▪ Septic shock ▪ Neurogenic shock ▪ Anaphylactic shock CHF Renal artery stenosis, embolus The cause is within the kidneys: damage the kidney itself Acute tubular necrosis: Nephrotoxins Aminoglycosides “mycins” Myoglobin (Rhabdomyolysis) Contrast dye Uric acid Glomerulonephritis Nephrotic, nephritic syndrome Acute interstitial nephritis NSAIDs, penicillins, diuretics Pyelonephritis The cause is after the kidneys: Obstruction to outflow Compression: Abdominal tumors Benign prostatic hyperplasia Blockage: Kidney stones (ureter, urinary bladder) Manifestations: Associated with the underlying cause. The symptoms of AKI are related to the various kidney functions. Accumulation of BUN and creatinine (azotemia) lead to fatigue, loss of appetite, headache, nausea and vomiting etc. Metabolic acidosis for instance is a life threatening condition that can lead to CNS depression. Hyperkalemia can also lead to fatal arrhythmias. Furthermore, fluid balance affects blood pressure regulation which leads to heart failure and pulmonary edema. Management: The management of AKI is the treatment of the underlying cause and preventing complications such as metabolic acidosis, hyperkalemia and pulmonary edema. Remember, AKI is reversible because the underlying causes are treatable. However, serious complications may occur if not treated promptly. Dialysis maybe indicated. 100 m NCLEX-RN study guide Common renal disorders: Chronic kidney disease (CKD) Chronic kidney disease (CKD): Characterized by gradual loss of kidney function over a period of months or years (>3 months + GFR < 60 ml/min). Remember that chronic diseases are irreversible. Such causes of CKD includes, hypertension and DM which makes CKD as an irreversible condition contrary to AKI. Both HTN and DM cause sclerosis of glomerulus overtime. Causes: Hypertension Causes: Diabetes Mellitus The sticking of glucose to proteins in the vessel walls Other Causes: ▪ SLE ▪ Rheumatoid arthritis ▪ HIV ▪ NSAIDs (chronic use) ▪ Tobacco 208 100 m NCLEX-RN study guide Azotemia: Abnormally high levels of nitrogencontaining compounds (BUN, creatinine). Azotemia leads to uremia (urine in blood). Remember: Brain cells are very sensitive to waste products (waste products are acids). Monitor alteration in level on consciousness. Patient safety is a priority. Hypocalcemia: Due to low production of calcitriol which causes less absorption of calcium. Inversely, it can cause ↓Phosphorus Hyperkalemia and metabolic acidosis: Results from retention of K+ and less excretion in the urine. This is also in response to H+ ion acidosis (body’s response is to eliminate H+ ions) in exchange of K+ thereby causing ↑K+. Remember: ↑K+ is acidosis. A very important indicator to initiate dialysis Hypertension: Low cardiac output to kidney is the effect of HTN. This causes activation of RAA system increasing risk of HTN and CHF. This creates a cycle since HTN is a significant cause of CKD. Remember: ACE inhibitor “prils” or angiotensin II receptor blocker “sartans” are commonly given to treat CKD with HTN. Hyperkalemia is a common adverse effects. 209 NCLEX-RN study guide 100 m Anemia: Due to abnormal synthesis of erythropoietin causing anemia. Remember: Anemia in CKD is treated with recombinant human erythropoietin (Epogen, epoetin). Target HgB is 10-11.5 g/dL (100-115 g/L) Epogen: to ↑ RBC Neupogen: to ↑ WBC Oprelvekin: to ↑ platelet Stage Severity GFR Stage 1 Diminished function/compensatory ≥90 ml/min Stage 2 Mild CKI 60–89 ml/min Stage 3 Moderate CKI 30–59 ml/min Stage 4 Severe CKI 15–29 ml/min Stage 5 End-stage kidney disease (ESRD) <15 ml/min AKI vs. CKD AKI CKD Definition ▪ Sudden damage to kidneys < 3 months ▪ ↑BUN, creatinine ▪ oliguria (<400 ml/24 hours) ▪ Gradual loss of kidney function over a period of months or years (>3 months + GFR < 60 ml/min Causes Prerenal, Intrinsic, Post-renal HTN, DM SLE, RA, HIV, NSAIDs (chronic use), Tobacco S/S ▪ Depending on the underlying ▪ Depending on the cause underlying cause: HTN, DM ▪ Related to ↑BUN, creatinine: ▪ Azotemia, uremia 210 NCLEX-RN study guide 100 m Diagnosis Management Hypocalcemia Hyperphosphatemia Hyperkalemia Metabolic acidosis Hypertension Anemia fatigue, loss of appetite, headache, n/v, acute confusion, seizures, coma ▪ Hyperkalemia ▪ Metabolic acidosis ▪ CHF, pulmonary edema ▪ ▪ ▪ ▪ ▪ ▪ Clinical exam, GFR, BUN, Creatinine (sudden ↑ within several days -weeks) Clinical exam, GFR, BUN, Creatinine (over several months or years) Supportive/ Treat symptoms: Anemia: Erythropoietin Hyperkalemia: 1. IV 50% dextrose + regular insulin (glucose transports K+ out from serum) 2. Calcium gluconate (if + arrhythmia) 3. Sodium polystyrene sulfonate (Kayexalate) administered PO or enema (removes K+ from the body by exchanging Na+ for K+ ions in GIT; K+ excreted in feces) Last priority d/t delayed onset. 4. Dialysis – last resort Hypocalcemia/Hyperphosphat emia: Calcium supplements Metabolic acidosis: NaHCO3 Hypertension: ACEIs “prils” or ARBs “sartans” Renal replacement therapy: Hemodialysis, Peritoneal dialysis, Kidney transplant Treat underlying cause Prevent complications by treating the symptoms: Hyperkalemia CHF, pulmonary edema Metabolic acidosis Renal replacement therapy Hemodialysis Peritoneal dialysis Avoid nephrotoxins: NSAIDs, contrast dye, aminoglycosides Diet: Low protein, low sodium and potassium, low phosphate, fluid-restricted Diet: Low protein, low sodium and potassium, low phosphate, fluid-restricted Prognosis Reversible but can lead to CKD if not treated promptly Irreversible 211 100 m NCLEX-RN study guide Question: A client with advanced kidney disease has serum potassium of 7.1 mEq/L (7.1 mmol/L) and creatinine of 4.5 mg/dL. What is the priority prescribed intervention? 1. Administer IV 50% dextrose and regular insulin 2. Administer IV furosemide 3. Administer oral sodium polystyrene sulfonate 4. Prepare the client for hemodialysis catheter placement Answer: 1 Rationale: Severe hyperkalemia (potassium >7.0 mEq/L [7.0 mmol/L]) requires urgent treatment because cardiac muscle cannot tolerate very high potassium levels. Severe hyperkalemia increases the risk ventricular tachycardia and fibrillation, asystole. 50 mL 50% dextrose + 10 units of regular insulin is the priority intervention as it is most effective in reducing the potassium level quickly. Glucose is a transporter of potassium from the extracellular fluid back into the intracellular fluid. Insulin is added in the presence of concentrated dextrose (50%) . If the client has ECG changes (e.g. tall peaked T waves), calcium gluconate should be given before insulin/dextrose. This will stabilize the cardiac muscle until the potassium level can be reduced with insulin/dextrose. Furosemide (Lasix) increases the renal excretion of potassium and is usually prescribed for clients with fluid overload. However, administration of furosemide would take time to be effective and is not the priority. Sodium polystyrene sulfonate (Kayexalate) is administered by mouth or enema to remove potassium from the body by exchanging sodium for potassium ions in the intestines; these are then excreted in feces. This is not the priority due to the delayed onset of potassium removal. Placement of hemodialysis catheter will delay treatment. 212 NCLEX-RN study guide 100 m Dialysis: Hemodialysis Arteriovenous Access (A/V) Internal A/V shunt External A/V shunt A/V Fistula Matures 6-8 weeks Permacath (2 lumen-tunneled) Last up to 12 mos. A/V Graft Matures 2 weeks External A/V shunts can be used immediately while waiting for internal shunts to mature Trialysis (3 lumen) 3rd lumen used for CVP monitoring, blood draws ,medication & contrast administration Hemodialysis is used as a temporary measure in either AKI or in CKD - ESRD as a permanent measure where transplant is not possible. The principle is the same as other methods of dialysis (e.g. peritoneal dialysis); it involves diffusion of solutes across a semipermeable membrane (dialyzer) HD is usually done 3X/week for about 3-4 hours/therapy. The dialyzer is composed of bundles of hollow fibers, whose walls are made of semipermeable membrane. Pressure gradients are applied into the dialyzer to move fluid. Remember to monitor patient’s BP during this process. 213 100 m NCLEX-RN study guide Dialysis disequilibrium syndrome (DDS): A rare but potentially lifethreatening complication during the initial stages HD; related rapid rate of HD Rationale: During HD, solutes are removed more quickly from the blood than the brain and CSF due to blood and brain barrier (BBB) mechanism, creating a concentration gradient that can lead to excess fluid in the brain. Manifestations are r/t ↑ICP (cerebral edema): n/v, headache, restlessness, confusion and seizure Thrill : Palpable vibration at the A/V site caused by arterial pressure through the walls of the vessels. Bruit: A blowing or swooshing sound caused by turbulent blood flow assessed through auscultation. Remember: Absence of the thrill or bruit can indicate potential clot formation in the A/V site. Other complications: Hypotension: hold BNP meds before HD Muscle cramps: electrolyte replacement A/V access occlusion: ▪ check bruit and thrill (AVF) ▪ check thrill (AV graft) Bleeding d/t heparin: monitor coagulation studies A/V access infection (CLABSI): Strict bundle of care implementation 214 NCLEX-RN study guide 100 m Dialysis: Peritoneal dialysis Peritoneal dialysis (PD): Uses the peritoneum as a semipermeable membrane to dialyze a blood. A catheter is placed into the peritoneal cavity, and dialysate solution (hypertonic) is infused. The tubing is clamped to allow the fluid to remain in the cavity (dwelling). Finally, the fluid is drained. Remember: There are 2 basic compartments in the human body, intravascular (serum/blood) and extravascular (interstitial, intracellular). PD solution is a hypertonic solution which attracts fluid from low concentration of solutes to higher concentration. Waste products are drawn to peritoneum. Remember: Peritonitis is a major complication. Signs of peritonitis are low to high grade fever, tachycardia and cloudy outflow Insufficient outflow: ▪ Monitor bowel movements Administer stool softeners ▪ Check tubing for kinks or clots ▪ Keep drainage bag below the abdomen; ▪ Place patient on a side-lying position or assist with ambulation. 215 NCLEX-RN study guide 100 m Common renal disorders: Alport syndrome vs Glomerulonephritis (nephrotic & nephritic syndrome) Alport syndrome Etiology Mechanism Genetic mutation Mutation to the collagen containing membrane in eyes, cochlea & kidneys This genetic changes lead to abnormal structure of glomerular basement membrane (kidneys) promoting leakage of large molecules to urine (protein, RBC). Manifestations are also associated with eyes and ear disorders. Classic sign ▪ Hematuria (Tea colored) ▪ Proteinuria ▪ ↓ serum albumin ▪ ▪ ▪ ▪ ▪ Other S/S Periorbital edema Peripheral edema Anasarca Hypertension Eye changes: thinning of cornea, Hearing loss Remember: Albumin controls fluid in the serum. ↓ serum albumin promotes leakage of fluids to extravascular compartment (edema) Glomerulonephritis Nephrotic syndrome Idiopathic (unknown) Nephritic syndrome Post streptococcal: glomerulonephritis Inflammation as well as Immune-complexformation of a crystalline mediated mechanism material within (delayed hypersensitivity) glomerular cells allows that is develop after large molecule proteins Group A beta hemolytic such as albumin, streptococcus (GABHS) antithrombin or the infection GBM is damage immunoglobulins to pass d/t inflammation through the glomerular Impetigo (post 6 weeks) basement membrane Pharyngitis (1-2 weeks). (GBM) towards urine. Noninflammatory Inflammatory ▪ Proteinuria ▪ ↓ serum albumin ▪ ↑ serum lipids ▪ ↓ anti-thrombin ▪ Hematuria (Tea colored) ▪ Proteinuria ▪ ↓ serum albumin ▪ Periorbital edema ▪ Peripheral edema ▪ Anasarca ▪ Hypertension Complication: ▪ Infection (d/t ↓Ig) ▪ DVT/PE (d/t ↓antithrombin) ▪ Hyperlipidemia (d/t compensatory response to ↓ serum albumin) ▪ ▪ ▪ ▪ Periorbital edema Peripheral edema Anasarca Hypertension Infection: Fever, tachycardia, headache, malaise, anorexia, nausea Diagnosis Physical exam, biopsy Genetic testing Physical exam, biopsy Physical exam, Culture & sensitivity Treatment Goal: ↓ BP (ACE inhibitor) Dialysis (kidney failure) Goal: ↓ BP (ACE inhibitor) ↓ edema (diuretics), Prevent infection Goal: Treat infection (Penicillin)↓ BP (ACE inhibitor), diuretics 216 100 m NCLEX-RN study guide Common renal disorders: Kidney stones (urolithiasis) Calcium stones Ca oxalate: Acidic Ca Phosphate: Alkaline Uric stones Acidic Remember: Kidney stones can be elsewhere in the Kidneys: nephrolithiasis Ureter: ureterolithiasis Bladder: cystolithiasis/ vesicolithiasis 217 100 m NCLEX-RN study guide Struvite stones Alkaline Cystine stones Acidic Classic sign: ▪ Flank pain (mid-lower back) ▪ Renal colic (constant sharp pain) Diagnosis: History and physical exam X-ray, CT scan, USD Urinalysis - Hematuria 218 100 m NCLEX-RN study guide Treatment: Hydration – to reverse stone precipitation Medication: Pain – NSAIDS Reduce stone – K+ citrate Pass stone – Alpha adrenergic blocker, Calcium channel blocker (reduce spasms) Shockwave lithotripsy Stent placement Nephrectomy/nephrolithotom y Remember: Extracorporeal shock wave (large stones) lithotripsy (ESWL) A noninvasive procedure used to break up kidney stones. It is typically done on an outpatient, although the client will require local or general anesthesia. The shock waves break up the stone(s) into a fine sand that can then be excreted in the urine. Bruising on the back or abdomen after the procedure is normal. Hematuria is concerning if the urine remains bright red over a prolonged period (>24 hr.). Ureteral stents: Often placed after the procedure to help with the passage of the broken stone and prevent buildup within the ureter. The stents are removed within 1-2 weeks. Nursing care: ▪ Encourage fluid intake ▪ Prevent infection ▪ Administer analgesics (pain can be severe) 219 NCLEX-RN study guide 100 m Alkaline ash diet: Indicated for acidic stones Acidic stones: Uric acid, Calcium oxalate, cystine Consisting mainly of fruits, vegetables, and milk when catabolized leaves an alkaline residue to be excreted in the urine. Acid ash diet: Indicated for alkaline stones Alkaline stones: Struvite (infection stones), Calcium phosphate VS Remember: patient can still have meat, fish, eggs (acid) but in minimal amount Consisting mainly of eggs, meat, fish when catabolized leaves an acidic residue to be excreted in the urine. Remember: patient can still have fruits, vegetables, and milk (alkaline) but in minimal amount. Common renal disorders: Urinary tract infection (UTI) Lower UTI Upper UTI Definition Infection to bladder (cystitis) and urethra (urethritis) Infection to ureter (ureteritis) is rare. It usually affects kidneys (pyelonephritis) Causes E. coli (most common) Klebsiella, Enterobacter, Proteus, Staphylococcus (2nd most common) Same Risk factors ▪ Sexual intercourse “honeymoon cystitis” ▪ Female – short urethra ▪ Post-menopausal - ↓estrogen (loss of protective vaginal flora ▪ Urinary catheter – CAUTI ▪ Diabetes - ↑ blood sugar inhibits phagocytosis ▪ Foreskin (boys) -uncircumcised ▪ Impaired bladder emptying Mechanism Bacteria colonizes the bladder mucosa Remember: Urine is sterile, bacteria cannot thrive in high urea and low pH environment. Bacteria in urinalysis is a significant finding. Same with lower UTI + Vesicoureteral reflux (congenital disorder) which promotes ascending infections Bacteria adheres to renal interstitium. Typically spares blood and glomerulus Ascending infection: recurrent lower UTI Descending infection (rare): from blood stream, consequence of septicemia 220 NCLEX-RN study guide 100 m S/S Diagnosis ▪ Suprapubic pain ▪ Dysuria ▪ Frequent urination ▪ Urgency Infants: poor feeding, fussy, fever Elderly: fatigue, incontinence, DELIRIUM (safety is the priority – risk for fall) Symptoms not usually present: Fever, nausea and vomiting Flank pain (costovertebral angle tenderness) Suggests upper UTI if present Urinalysis: ▪ Abnormally ↑ WBC (>5/HPF) ▪ Cloudy urine appearance ▪ (+) cast: WBCs in clamps Dipstick test: Leukoesterase (+) – WBCs Nitrites (+) – E. Coli converts nitrates in urine to nitrites Urine culture: >100,000 CFU (colony forming units) (+) <100,000 CFU may still indicate infection ▪ Suprapubic pain ▪ Dysuria ▪ Frequent urination ▪ Urgency Infants: poor feeding, fussy, fever Elderly: fatigue, incontinence, DELIRIUM (safety is the priority – risk for fall) Fever, chills, nausea and vomiting Flank pain (costovertebral angle tenderness) Same with lower UTI + Leukocytosis (↑WBCs) in the blood and systemic symptoms such as fever, n/v, chills helps distinguish upper UTI (+) pyuria (WBC in urine) (-) urine culture: Suggests urethritis (possible chlamydia or gonorrhea – sexually transmitted) Treatment Antibiotics: Penicillin’s, cephalosporins, sulfonamides fluroquinolones Pain medication: NSAIDs Prevention: Hydration (flush out bacteria) Good hygiene Avoid bubble bath in young children (girls) Same with lower UTI + Preventing complications: Chronic pyelonephritis (scarring) Renal abscess (sepsis) 221 NCLEX-RN study guide 100 m Others: Circulatory shock Shock: Is circulatory shock Characterized by widespread insufficient blood flow to the tissues of the body. Contrary to ischemia which pertains to specific organ system. HYPOTENSION: Is a determinant of circulatory shock. Consequently, circulatory shock results to cellular damage. Blood Pressure Resistance to flow Factors: Diameter Length Example: HTN, Peripheral vascular disease (PVD) All forms of shock causes low BP. It is a priority condition because it may cause immediate multi organ failure. Remember: All body tissues are dependent on the CO supplying their O2 and nutrients to sustain life Cardiac output Factors: Heart rate x stroke volume Example: Shock, CHF, Acute coronary syndrome (ACS) 1. Hypovolemic shock: Low volume 2. Cardiogenic shock: Pump failure affects the CO Non hemorrhagic – Dehydration, N/V Hemorrhagic - Bleeding Remember: 20-25% (approx. 1L) of blood loss causes significant hypotension. S/S: “hypo,tachy,tachy” Hypotension, restlessness Rapid, weak and thready pulse (tachycardia) Cold clammy skin, Diaphoresis, Rapid shallow breathing (tachypnea), polydipsia. Other s/s apart from hypotension are compensatory (autonomic response) d/t low tissue perfusion affects CO AMI, Arrhythmias, Cardiomyopathies, Valvular defects, cardiac tamponade S/S: “hypo,tachy,tachy” Hypotension, restlessness Rapid, weak and thready pulse (tachycardia) Cold clammy skin, Diaphoresis, Rapid shallow breathing (tachypnea) Associated S/S: d/t underlying heart condition Arrhythmias Jugular vein distention 222 100 m 3. Distributive shock: Widespread vasodilation affects resistance to flow and CO Remember: It is called distributive shock because there is an abnormal distribution of fluid within the involved compartments (intravascular & extravascular). This is due to massive vasodilation. Vasodilation tends to make blood vessels more “leaky” (permeable). However, in this form of shock there is no absolute loss of fluid unlike hypovolemic shock. NCLEX-RN study guide Types of distributive shock: Septic shock – vasodilation due to widespread inflammatory process Neurogenic shock – vasodilation due to loss of sympathetic tone from spinal cord injury Anaphylactic shock – vasodilation due to inflammatory process (histamine) Septic shock: S/S “hypo,tachy,tachy” Hypotension, restlessness Rapid, weak and thready pulse (tachycardia) Warm skin, Rapid shallow breathing (tachypnea) + SIRS criteria and Sepsis: Temperature, HR, respiration, WBCs, identified causative agent Neurogenic shock: S/S “hypo,brady,tachy” Hypotension, Warm, flushed skin due to vasodilation and inability to constrict blood vessels, Bradycardia due to loss of sympathetic tone, Rapid shallow breathing (tachypnea) + Priapism (constant painful erection) due to vasodilation Respiratory arrest – if above C4 is affected 223 NCLEX-RN study guide 100 m Anaphylactic shock: S/S “hypo,tachy,tachy” Hypotension, restlessness Itchiness, warm flushing, or swelling (angioedema). Shortness of breath, wheezes, or stridor, Tachypnea (due to bronchoconstriction) , Tachycardia (Sympathetic response), Abdominal pain, N/V (due to gastric acid secretion) Type of shock 1. Hypovolemic: Absolute loss of fluid 2. Cardiogenic: Pump failure Signs/symptoms “hypo, tachy, tachy” ▪ Hypotension ▪ Rapid, weak and thready pulse (tachycardia) ▪ Rapid shallow breathing (tachypnea) ▪ Cold clammy skin ▪ Diaphoresis, polydipsia, restlessness “hypo, tachy, tachy” ▪ Hypotension ▪ Rapid, weak and thready pulse (tachycardia) ▪ Rapid shallow breathing (tachypnea) ▪ Cold clammy skin ▪ Diaphoresis, restlessness arrhythmias, jugular vein distention Treatment Stabilize blood pressure: ▪ Fluids (Normal saline, LR) ▪ Medications (inotropes) Supplemental oxygen Treat the cause: ▪ Blood transfusion ▪ Fluids (Normal saline, LR) Stabilize blood pressure: ▪ Fluids (Normal saline, LR) ▪ Medications (inotropes) Supplemental oxygen Treat the cause: ▪ Antiarrhythmics 3. Distributive: Widespread vasodilation Septic: widespread infection “hypo, tachy, tachy” ▪ Hypotension, restlessness ▪ Rapid, weak and thready pulse (tachycardia) ▪ Rapid shallow breathing Stabilize blood pressure: ▪ Fluids (Normal saline, LR) ▪ Medications (inotropes) Supplemental oxygen Treat the cause: 224 NCLEX-RN study guide 100 m Neurogenic: Spinal cord injury Anaphylactic: Severe allergic reaction Others: Fluids (tachypnea) ▪ Warm skin ▪ SIRS criteria and Sepsis: Temperature, HR, respiration, WBCs, identified causative agent “hypo, brady, tachy” ▪ Hypotension ▪ Bradycardia due to loss of sympathetic tone, ▪ Rapid shallow breathing (tachypnea) ▪ Warm flushed skin ▪ Priapism (constant painful erection) due to vasodilation ▪ Respiratory arrest: if above C4 spine injury is affected “hypo, tachy, tachy” ▪ Hypotension, restlessness ▪ Tachycardia, Abdominal pain, N/V (due to gastric acid secretion) ▪ Tachypnea (due to bronchoconstriction) ▪ Warm flushed skin ▪ Itchiness, , or swelling (angioedema). Shortness of breath, wheezes, or stridor, ▪ Antibiotics (empiric/broad spectrum) Stabilize blood pressure: return of sympathetic tone ▪ Medications (inotropes) ▪ Fluids (Normal saline, LR) Supplemental oxygen Airway protection (above C4 spine injury) Stabilize blood pressure: ▪ Fluids (Normal saline, LR) ▪ Medications (inotropes) Airway management: ▪ Epinephrine (bronchodilation and ↑BP) ▪ Anti-histamines ▪ Immune suppressants (steroids) Osmotic vs Hydrostatic pressures: Hydrostatic pressure is a PUSHING force that is exerted by a fluid against the capillary wall. Osmotic pressure is a PULLING force that attracts water and solute from lower to higher concentration and is dominant in the venous end. Osmotic pressure helps in the movement of fluid between capillaries and the interstitial fluid. Remember: IV fluids are administered intravenously. Tonicity of fluid is consistent with osmotic pressure involved. Normal osmolality of blood : approximately 300 mosmol/L 225 100 m Hypotonic Solution: low solute, high solvent (low osmolality) As it is given intravenously (intravascular), it causes movement of fluids from intravascular to extravascular (interstitial, intracellular) compartment leading to cell swelling. Given to patients with cellular dehydration (shrunken cell) such as DKA. Remember: Elevated glucose in the blood (hypertonicity) attracts fluid from extravascular to intravascular causing cellular dehydration. Example: 0.45% Normal Saline (aka Half Normal Saline, 0.45NaCl) Remember: Less than 0.9% NaCl is considered hypotonic. It is always avoided in patients with burns, trauma, or liver disease because of its tendency to deplete intravascular fluids. NCLEX-RN study guide Isotonic Solution: equal solute and solvent As it is given intravenously (intravascular), it causes no movement of fluids within both the compartments Given to patients with any types CIRCULATORY SHOCK as a fluid replacement. Hypertonic Solution: high solute, low solvent (high osmolality) 5% Dextrose in Water (aka D5 or D5W) – becomes hypotonic once given as the dextrose is metabolized. As it is given intravenously (intravascular), it causes movement of fluids from extravascular (interstitial, intracellular) to intravascular compartment leading to cell shrinkage. Given to patients with cell swelling such as cerebral edema. Remember: Cerebral edema is swelling of brain tissues. Giving a hypertonic solution promotes movement of fluids from the brain tissues to the intravascular compartment. In lieu of homeostasis, kidneys compensate to cause diuresis removing fluids from a hypertonic intravascular space. Remember: LR contains NaCl, potassium chloride, calcium chloride, & sodium lactate in sterile water. It is the most similar to the body’s plasma and serum concentration, and is especially used for burns or hypovolemia due to fluid shifts. It is avoided in patients with liver disease because the liver may not be able to efficiently process the lactate (lactic acidosis) NS is the most common IV fluids for hydration needs due to vomiting, diarrhea, hemorrhage, or shock. The only fluid used in conjunction with blood product administration. Example: D10 W 3% NaCl D5 0.45% NaCl (D5 half saline) D5 0.9% NaCl (D5NS) Remember: More than 0.9% NaCl is hypertonic such as 3% NaCl. 5% or more Dextrose is hypertonic. However in the case of D5W, the 5% dextrose is diluted by water (solvent)making it hypotonic. In contrast, 0.45% and 0.9% NaCl gives more tonicity to Dextrose 5%. D10W, 3% NaCl are high alert medications. Example: Lactated Ringers (aka LR, Ringers Lactate, or RL, or Hartmann's solution ) 9% Normal Saline (aka NS, 0.9NaCl, or NSS) 226 100 m NCLEX-RN study guide Question: The nurse is caring for a 78-year-old client with a urinary tract infection (UTI). Which assessment finding would be most concerning and require immediate follow-up by the nurse? 1. Confusion 2. Presbyopia 3. Temperature 100.2 F (37.8 C) 4. White blood cell (WBC) count 12,000/mm3 Answer: 1 Rationale: Confusion is a common clinical manifestation of UTI in the elderly but still should be cause for concern and requires follow-up to rule out other possible causes. Confusion is not a normal finding in the elderly adult client and compromises patient’s safety. Some causes of confusion in the elderly include dehydration, lack of blood flow to the brain (stroke), decreased ability to metabolize medications (polypharmacy: ≥ 4 medications) and concurrent infections. Presbyopia is the decrease in ability to see objects close up. This is common in clients over age 40. The elderly tend to have a lower body temperature, so 100.2 F (37.8 C) is considered febrile. This elevation is an expected finding. An elevated WBC count would be expected in the presence of a current infection. 227 NCLEX-RN study guide 100 m 11 Endocrine Anatomy and Physiology Hypothalamus: Has a central neuroendocrine function, by its control of the anterior pituitary, which in turn regulates various endocrine glands and organs. Releasing hormones are produced in hypothalamus then transported, stored and released as needed. Hormones released: ▪ Thyrotropin-releasing hormone (TRH) ▪ Corticotropin-releasing hormone (CRH) ▪ Gonadotropin-releasing hormone (GnRH) ▪ Growth hormone–releasing hormone (GHRH) Pituitary gland: Referred to as the 'master gland' because it controls the activity of most other hormone-secreting glands except pancreas, adrenal medulla, and parathyroid. 228 NCLEX-RN study guide 100 m Anterior pituitary Remember: Acronym GTPAL-F (anterior pituitary function) 1. Growth hormone (GH)/ Somatotropin 2. Thyroid-stimulating hormone (TSH) 3. Prolactin (PRL) Hormones Influenced by GHRH by hypothalamus. Stimulates musculoskeletal growth ▪ Influenced by TRH by hypothalamus. Stimulates release of thyroid hormones. Thyroxine (T4) Triiodothyronine (T3) ▪ Increase the body's sensitivity to catecholamines necessary for metabolism. Remember: Epinephrine and norepinephrine are catecholamines that causes stimulation of the sympathetic nervous system (SNS) “fight/flight response” which means manifestations of overproduction of thyroid hormones (hyperthyroidism) correlates with SNS effects. Stimulates mammary gland to PROduce milk (lactose) ▪ Released under the influence of hypothalamic corticotropinreleasing hormone (CRH). Stimulates release of hormones in adrenal cortex. 4. Adrenocorticotropic hormone (ACTH) Remember: Acronym SSS Sugar, Salt & Water, Sex hormones Glucocorticoids (cortisol): Steroid hormone that activates anti-inflammatory and anti-stress effect by promoting glucose production for energy Related condition Overproduction: Gigantism (pediatrics), Acromegaly (adults). Remember: Acro means “tip end” which means the enlarged portion d/t ↑ GH is at the distal end of the extremities. Underproduction: Dwarfism Overproduction: Hyperthyroidism Underproduction: Hypothyroidism Remember: Negative feedback mechanism causes opposite effects to level of TSH. Elevated T3, T4 causes decrease TSH, vice versa. Overproduction: Hyperprolactinemia Underproduction: Hypoprolactinemia Overproduction: ▪ Cushing’s disease (endogenous, d/t tumor) ▪ Cushing’s syndrome (exogenous, d/t chronic use of steroids) ▪ Conn's syndrome (primary hyperaldosteronism) – only involving excess production of aldosterone. Underproduction: ▪ Addison's disease (primary adrenal insufficiency) 229 NCLEX-RN study guide 100 m consumption. It’s called Hydrocortisone if used as a medication. Mineralocorticoids (aldosterone): A steroid hormone that causes reabsorption of sodium and excretion of potassium by the kidney (hypernatremia, hypokalemia), thereby indirectly influencing water retention or loss, blood pressure and blood volume as part of the RAS system. Androgens: A steroid hormone that regulates the development and maintenance of male characteristics. Remember that females also have them, but at lower levels: they function in libido and sexual arousal. Androgens are also the precursors to estrogens in both men and women. Remember: Adrenal medulla hormones (epinephrine, norepinephrine ) are not controlled by pituitary gland just as pancreas and parathyroid gland. 5. Luteinizing hormone (LH) and Folliclestimulating hormone (FSH) ▪ Both released under the influence of GonadotropinReleasing Hormone (GnRH) In females: ovulation, maintaining of corpus luteum and secretion of progesterone. In males: Testosterone secretion Females: Turner’s syndrome: A genetic condition in which a female is partly or completely missing an X chromosome (X0 instead of XX) associated with other congenital disorders. Classic sign, “webbed neck, low set ears, small body structure” Males: Klinefelter syndrome: A genetic condition in which there are 2 or more X chromosomes in males (XXY instead of XY) Classic sign, “testicular atrophy, tall and lanky structure” 230 NCLEX-RN study guide 100 m Posterior pituitary Remember: Acronym OA 1. Oxytocin 2. Antidiuretic Hormone (ADH)/Vasopressin Hormones Related condition Overproduction: Pitocin as a Most of which is released from synthetic oxytocin cause the hypothalamus. Uterine maternal hypotension, and contractions stimulate the fetal distress release of oxytocin (positive Underproduction: Depression, feedback) from the posterior anxiety, social phobia, pituitary, which, in turn, autism, schizophrenia, PTSD increases uterine contractions. anorexia nervosa, This positive feedback borderline personality continues throughout labor. disorder Released in response to intravascular fluid hypertonicity (hyperosmolarity) by reabsorbing water back into the circulation in the kidneys. Remember: Water is a universal solvent that causes low tonicity or osmolarity It also constricts arterioles, which increases peripheral vascular resistance and raises arterial blood pressure. Overproduction: Syndrome of Inappropriate Antidiuretic Hormone secretion (SIADH) Underproduction: Diabetes insipidus (DI) 231 100 m NCLEX-RN study guide Other endocrine organs: Pancreas, Parathyroid gland Function: "endocrine" role (1%), relating to the secretion of insulin and other substances within pancreatic islets and helping control blood sugar levels "exocrine" role (99%), relating to the secretion of enzymes involved in digestion. Endocrine Function: Alpha cells: producing glucagon Beta cells: producing insulin Delta cells: producing somatostatin (suppresses both the exocrine and endocrine function of pancreas) Parathyroid gland: The major function of the parathyroid glands secretes parathyroid hormone (PTH)s to maintain the body's calcium and phosphate levels so that the nervous and muscular systems can function properly. Remember: Calcium level is inversely proportional with phosphate level. It means, s/s of hypercalcemia are the same with hypophosphatemia vice versa. PTH: increases serum calcium level Calcitonin (released by thyroid gland): decreases serum calcium level 232 NCLEX-RN study guide 100 m Common endocrine disorder affecting ADH: Syndrome of inappropriate ADH (SIADH) vs. Diabetes insipidus (DI) Remember: Physiology of ADH is important in understanding DI and SIADH. ADH works in response to intravascular fluid hypertonicity (hyperosmolarity) by reabsorbing water back into the circulation in the kidneys. Water is a universal solvent that causes low tonicity/concentration/osmolarity. In relation to kidney physiology, there are only 2 main areas where water goes, in the urine which affects urine concentration (specific gravity) and in the blood which affects concentration (blood osmolarity). SIADH Diabetes insipidus Acronym: “Use Increased instead of inappropriate” to easily remember Mechanism Etiology Increased ADH causes NO DIURESIS which means water is in the blood/serum and less water in the urine. The result is concentrated urine and diluted blood. Sodium as a solute is diluted causing “dilutional hyponatremia” as a classic mechanism causing manifestations. Elevated ADH means less aldosterone as a compensatory mechanism d/t retained water. Less aldosterone means less ability to excrete potassium into urine, causing hyperkalemia. In summary it causes ↓Na, ↑K. Conditions that dysregulate ADH secretion in the CNS: Tumors that secrete ADH (lung CA), CNS infections (meningitis), drugs that increase ADH secretion (morphine, amitriptyline, carbamazepine) Acronym: DD Decreased ADH: DI Decreased ADH causes DIURESIS. More water to urine makes the blood more concentrated. Diuresis means more waste of potassium in urine. In response, aldosterone is released to retain sodium and H2O. This causes ↑Na, ↓K Nephrogenic: Acquired DI usually caused by lithium toxicity and high blood calcium. Remember: Calcium has a diuretic effect Neurogenic: post cranial surgery, CVA, Tumor 233 NCLEX-RN study guide 100 m Classic S/S Dilutional hyponatremia/ Water intoxication: Causes brain tissue swelling, (cerebral edema) hallucination, confusion, delirium, seizure tremors, headache Diagnostics ▪ High urine specific gravity: High urine concentration ▪ Decreased hematocrit ▪ Hyponatremia ▪ Hyperkalemia Complications Cerebral edema: Increased ICP ▪ Fluid restrictions 500 ml/day Treatment Treatment of choice: Hypertonic saline (3%) Polyuria (2-3L/H) Polydipsia S/S of dehydration: Dry skin and mucus membrane, tachycardia, weak pulses, weakness ▪ Low urine specific gravity: Low urine concentration ▪ Increased hematocrit ▪ Hypernatremia ▪ Hypokalemia Dehydration: Hypovolemia ▪ Increase fluid intake, prevent dehydration Treatment of choice: Synthetic vasopressin: Desmopressin (DDAVP) (Intranasally, IV, IM, SQ) 234 NCLEX-RN study guide 100 m Common endocrine disorder affecting ACTH: Cushing’s vs. Addison’s disease Remember: ACTH has a complex effects to adrenal cortex causing release of involved hormones (cortisol, aldosterone, androgens: The “SSS” hormones). Note that hormones travels to circulation with a systemic effects to many organs. It is also important to know that negative feedback plays a role in the release of these hormones. For instance increase levels of cortisol halts release of cortisol releasing hormones by hypothalamus (CRH), and ACTH in anterior pituitary. This is mechanism is necessary in the diagnosing between cushing ‘s syndrome and cushing’s disease. Cushing’s Mechanism Elevated levels of ACTH, CRH, Adrenal cortex hormones particularly cortisol, aldosterone and androgens Etiology Endogenous: Cushing’s disease (pituitary or adrenal tumor) Exogenous: Cushing’s syndrome (steroids medications) Classic S/S Due to: Glucocorticoids (cortisol) S – Sugar ▪ Hyperglycemia ▪ Truncal obesity: Hyperglycemia increases insulin levels and targets adipose tissues in the center of the body (activates lipid build-up) ▪ Buffalo hump, moon shaped face: cortisol disturbs lipid metabolism (lipodystrophy) ▪ Sleeplessness/irritability (Cortisol plays a role in circadian rhythm) ▪ Mental disturbances: cortisol disturbs brain function (unclear reason) ▪ Risk for infection: cortisol dampens immune response Addison’s disease (primary adrenal insufficiency) Destruction of adrenal gland resulting to low levels particularly of cortisol and aldosterone, and some androgens. It affects the adrenal gland itself the reason why it is called primary insufficiency Autoimmune Due to: Glucocorticoids (cortisol) S – Sugar ▪ Hypoglycemia (weakness, disorientation, lethargy) ▪ Bronze skin (hyperpigmentation): low levels of cortisol stimulates production of ACTH and melanocyte stimulating hormone (negative feedback), high levels of ACTH and MSH stimulates production of melanin. Mineralocorticoids (aldosterone) S – Salt ▪ Hyponatremia (salt craving, seizure, confusion, syncope) ▪ Hyperkalemia (cardiac 235 NCLEX-RN study guide 100 m ▪ Amenorrhea/infertility /impotence: cortisol inhibits gonadotropin releasing hormone in both male and female ▪ Muscle, bone (osteoporosis, hypocalcemia), tissue breakdown, easy bruising, abdominal striae: d/t direct effect of cortisol to tissues Mineralocorticoids (aldosterone) S – Salt ▪ Hypernatremia, hypokalemia ▪ Hypertension: d/t retained sodium and water ▪ Weight gain Androgens S – Sex hormones ▪ Hirsutism, acne, gynecomastia in males arrhythmias, metabolic acidosis) Remember: Hyperkalemia = H+ ion acidosis ▪ Hypercalcemia: enhanced absorption of calcium in GI d/t low hemoconcentration (low levels of water in the blood) ▪ Hypovolemia, Hypotension: d/t inability to reabsorb sodium and water ▪ Weight loss Androgens S – Sex hormones Men: not affected (major source of androgens in men is testes) Women: Loss of pubic, armpit hair, decrease sex drive ▪ 24 hour urine – cortisol level (normal: 80-120 mcg/24hr) ▪ Dexamethasone suppression test: Low dose of dexamethasone is given (exogenous) Diagnostics “Normally if cortisol level is high by giving the exogenous cortisol, ACTH is low d/t negative feedback mechanism” If ACTH remains unchanged: (+) endogenous type – tumor in the pituitary ▪ MRI/CT scan ACTH stimulation test: Low dose of synthetic ACTH is given to stimulate adrenal glands to produce cortisol and aldosterone. Positive (+) if no increase in cortisol and aldosterone. 236 NCLEX-RN study guide 100 m "Addisonian crisis" or "adrenal crisis": Abdominal, back, leg pain, vomiting, diarrhea, severe dehydration, hypovolemia, loss of consciousness Complications ▪ Diabetes ▪ Hypertension ▪ CHF DOC: Lysodren (Mitotane) Treatment ▪ Treat underlying cause: remove tumor ▪ Prevent complications Remember: Addison’s disease is an autoimmune disorder. Generally triggered by stressors (infection, stress, injury). More importantly, as a disorder characterized by low cortisol levels the patient does not respond effectively to stressors. This requires immediate care. DOC: Hydrocortisone ▪ Prevent complications by preventing stress Remember: Stopping medications can lead to Addisonian crisis. In addition, endocrine disorders in general requires lifetime maintenance of medications. 237 NCLEX-RN study guide 100 m Common endocrine disorder affecting thyroid hormones: Hyperthyroidism vs. hypothyroidism Remember: Thyroid hormones T4 once released in the blood is converted to T3 to exert its effect. It increases the body's sensitivity to catecholamines (epinephrine and norepinephrine. Catecholamines binds to sympathetic receptors to cause stimulation of the sympathetic nervous system (SNS) “fight/flight response. It also speeds up cell metabolism to burn more energy (fats and carbohydrates). Overall, increase levels of thyroid hormones indicates increase body activity in hyperthyroidism. Hypothyroidism is the exact opposite. Hyperthyroidism Hypothyroidism Too much thyroid hormones causing hypermetabolic state due to an autoimmune response, genetic mutation, injury or infection Thyroid gland does not produce enough thyroid hormone. Etiology Autoimmune: Grave’s disease (most common cause). B-cells produce thyroid stimulating antibodies that mimics TSH and bind to thyroid receptor sites to stimulate thyroid gland to secrete thyroid hormones Toxic nodular goiter: mutated TSH receptor keeps thyroid gland active Thyroid adenoma: benign tumor producing excessive thyroid hormone Iodine deficiency: most common cause of hypothyroidism and goiter worldwide d/t low supply of iodine Hashimoto's thyroiditis: autoimmune disease characterized by infiltration of the thyroid gland with T-cells and autoantibodies causing low production of thyroid hormones Pituitary tumor (central hypothyroidism): causing low levels of TSH Congenital hypothyroidism in children (cretinism): can be d/t maternal hypothyroidism Classic S/S Exophthalmia (proptosis): d/t sympathetic activity overstimulating eye muscles to contract, d/t immunemediated inflammation by hypermetabolic state causing fat deposit in the retro-orbital (eye socket) pushing the eye ball Weight loss, (in spite of increase appetite), diarrhea, fever, heat intolerance, sweating, moist warm skin, amenorrhea, hirsutism Mechanism Weight gain (in spite of poor appetite), constipation, hypothermia, cold intolerance, dry course skin, menorrhagia (abnormal heavy menstruation), hair loss: d/t low metabolic rate Bradycardia, hypotension, bradypnea, lethargy, fatigue, poor memory and concentration, hypersomnia: d/t less sympathetic activity 238 NCLEX-RN study guide 100 m : d/t body producing more heat, increase metabolic rate Tachycardia, hypertension, palpitations, tachypnea, anxiety, tremors, hyperactivity, insomnia, fatigue, depression: d/t sympathetic activity Increased T3 T4 Decreased TSH: d/t negative feedback mechanism Diagnostics Complications Remember: If TSH is high, it is caused by a pituitary tumor (central hyperthyroidism). If low then it is primary (caused by thyroid condition itself) Radioactive Iodine uptake test and thyroid scan: remember that thyroid is the only organ that synthesizes iodine to produce its hormones. In thyroid tumor for example, it can be visualized easily via scan d/t increase absorption of iodine. Thyroid Storm or thyroid crisis (severe hypermetabolism): triggered by stressors (infection, injury, surgery, stopping treatment) Remember: Thyroid storm is characterized by exaggerated normal s/s of hyperthyroidism (e.g. High fever, SVT) In addition, it is most commonly caused by Grave’s disease in which it can be triggered by any stressors as an autoimmune disorder. Congestive heart failure: d/t overactivity of SNS Decreased T4 Increased TSH: d/t negative feedback mechanism T3: rarely helpful since there is inadequate T4 (Normally T4 is converted to T3 to exert its metabolic effect) Myxedema coma: developed when there is another illness characterized by severe hypothermia without shivering, bradycardia and hypoventilation, mental sluggishness and coma 239 NCLEX-RN study guide 100 m Treat cause: remove tumor DOC: ▪ Tapazole (Methimazole) ▪ Propylthiouracil (PTU) Treatment Remember: Anti thyroid drugs cause agranulocytosis, thrombocytopenia Symptomatic: ▪ Beta blockers “olols” – regulates heart rate and rhythm HYPOTHYROIDSM Prevent complication: prevent triggers Prevention: Iodine supplement to common foods (e.g. iodized salt) in developing countries DOC: ▪ Levothyroxine (L-thyroxine, Synthroid): synthetic longacting form of thyroxine. Remember: Taken 30–60 minutes before breakfast, or 4 hours after food because food and calcium can inhibit the absorption of levothyroxine. Taken at HS because it can cause insomnia. Do not stop giving the medication to pregnant women, stopping the medication may cause HYPERTHYROIDSM congenital hypothyroidism (cretinism). Growing fetus is dependent on thyroid hormones from the mother. Prevent complication: do not stop medications 240 NCLEX-RN study guide 100 m Common endocrine disorders: Diabetes mellitus Remember: To understand diabetes mellitus further, it is important to know the metabolism of nutrients particularly glucose in causing effect to body tissues. Glucose apart from O2 is the primary source of ATP (cell energy) of any living cells to function effectively. For instance, the brain needs approximately 70% of glucose to maintain its function. It simply means, abnormalities to glucose metabolism has an obvious neurologic manifestations. Acidosis, as a complication of DM1 is a life threatening acute condition that is not compatible to cell function. Remember, any form of acidosis (metabolic/respiratory) causes CNS depression and subsequent effects to other organs. Diabetes mellitus 1 Mechanism Etiology Absolute lack of insulin: d/t failure of the pancreas (β-cells) to secrete insulin. Insulin is necessary to facilitate transfer or diffusion of glucose to the cells necessary to form ATP. Since there is absolute lack of insulin, the patient needs insulin administration. ▪ Genetic ▪ Autoimmune: Unknown ▪ Epstein barr virus (EBV): triggers autoimmune response, inflammation to Islets of Langerhans in the pancreas. Diabetes mellitus II Insulin resistance: pancreas produces enough insulin but the cells are just simply resistant to insulin (insulin cannot bind to insulin receptors) thereby leaving the glucose outside the cell (hyperglycemia). Overtime, pancreas produces insulin effectively as a compensation. However, it cannot sustain this mechanism leading to hypoplasia and thereby produces less insulin. Normally, the patient does not need insulin. Insulin resistance syndrome (aka metabolic syndrome): Presence of 3 or more of the following criteria: Increased waist circumference: Men: ≥40 in (102 cm) Women: ≥35 in (89 cm) Blood pressure: (M/F) ≥130 mm Hg systolic or ≥85 mm Hg diastolic or drug treatment for hypertension Triglyceride level: (M/F) >150 mg/dL (1.7 mmol/L) or drug treatment for elevated triglycerides High-density lipoprotein (HDL: Men: <40 mg/dL (1.04 mmol/L) Women: <50 mg/dL (1.3 mmol/L) in women or drug treatment for low HDL 241 NCLEX-RN study guide 100 m Fasting glucose levels: (M/F) ≥100 mg/dL (5.6 mmol/L) or drug treatment for elevated blood glucose Acronym: "We Better Think High Glucose" Classic S/S Polyphagia: d/t cellular starvation (glucose is the primary food for the cell) Polyuria: d/t increase blood concentration (hemoconcentration), normal body’s response is diuresis to lessen blood osmolality caused by hemoconcentration Polydipsia: d/t excessive urination (polyuria) Glucosuria: d/t excessive amounts of glucose in blood (hyperglycemia) Muscle wasting/weight loss: d/t body’s response in the absence of glucose. It uses other sources of nutrients through proteins stored in muscles and fats (lipolysis) stored in adipose tissues. Acute: Diabetic ketoacidosis: d/t lipolysis, breaking down free fatty acids. The liver then converts fatty acids into ketone bodies (acetoacetic, βhydroxybutyric acids) Blood acidity by ketones: S/S Complications ▪ Acetone breath: fruity odor d/t accumulation of ketones ▪ Kussmaul’s respiration: deep labored breathing as an attempt of the body to reduce acidity. ▪ Hyperkalemia: remember acidosis is hyperkalemia. Body’s response to acidosis is to eliminate H+ ions in the blood in exchange of K+ coming from Polyphagia Polyuria Polydipsia Glucosuria (no weight loss due to the fact that the there is no absolute lack of insulin. It does not use other sources such as lipids and protein to cause lipolysis) Acute: Hyperosmolar hyperglycemia state (HHS) – non ketosis: hyperglycemia results in excessive loss of water by polyuria leaving the blood concentrated (hyperosmolarity). Remember, osmolarity works by drawing solutes from lower concentration to higher concentration (cells-serum). This results in severe cellular dehydration as the cycle goes on. Cellular dehydration: S/S ▪ Mental status changes: (Hallucination, confusion, seizure, coma) – d/t loss of circulating fluids to the brain 242 NCLEX-RN study guide 100 m the cells. However, due to excessive diuresis, potassium loss is anticipated (hypokalemia) ▪ Arrhythmias: d/t potassium imbalance. ▪ Mental status changes: d/t severe ketoacidosis (acids causes CNS depression) Chronic: ▪ Neuropathy ▪ Retinopathy ▪ Gastropathy ▪ Nephropathy ▪ Peripheral vascular disease ▪ Erectile dysfunction ▪ Coronary artery diseases/AMI ▪ CVA Diagnostics ▪ Weakness, nausea/vomiting, dry mouth ▪ Hypokalemia: d/t excessive urination ▪ Hypovolemia (Hypotension, tachycardia, tachypnea) Remember: HHS manifestations also happen in type 1 since there is the same hyperglycemic and hyperosmolar mechanism. However, there is only minimal chance of developing acidosis because there is no absolute lack of insulin. Unless if not treated promptly or hyperglycemia is not controlled. Uncontrolled type 2 can also lead to chronic complications in type 1. ▪ Fasting blood glucose <200 mg/dl: normal >100-125 mg/dl: pre-diabetes >125 mg/dl: diabetes ▪ Glucose tolerance test 1. NPO (8hrs) 2. Take 100 g (40z) glucose 3. Take CBG after 2 hrs. 4. If >200 mg/dl: Diabetes Remember: Blood glucose level is stabilized in 2 hours. ▪ HBA1C (glycosylated HgB): Measures 3 month average blood sugar & can be used as Same with type 1 a test for glycemic control in patients with diabetes. Remember: HgB is exposed to glucose in the blood, and they are bound together through the glycation process. Parameters: Patients with diabetes: < 7% Good control > 9% Poor Control > 12% Very Poor Control With no diabetes: 4 - 5.6% normal level 5.7 - 6.4% high chance ≥6.5% Diabetes 243 NCLEX-RN study guide 100 m ▪ Lifestyle modification ▪ Prevent DKA ▪ Insulin administration Treatment DKA Management: ▪ Fluids for dehydration ▪ Aggressive Insulin ▪ Electrolyte replacement ▪ Lifestyle modification (screening for insulin resistance syndrome) ▪ Prevent HHS ▪ Insulin administration (if needed) HHS Management: ▪ Fluids for dehydration ▪ Electrolyte replacement ▪ Insulin (non-aggressive) DKA Blood sugar S/S Blood pH Ketones Management >300 mg/dl (enough to cause an acute complication) Less pronounced altered mentation, more rapid onset of hyperglycemia symptoms, hyperventilation, abdominal pain (d/t acid accumulation) common <7.25 (acid) HCO3 10-18 meqs/l HHS >600 mg/dl More pronounced altered mentation, gradual onset of hyperglycemia symptoms, hyperventilation, abdominal pain (d/t acid accumulation) less common ≥ 7.30 (usually normal) >18 meqs/l HCO3 Positive Minimal Aggressive insulin and dehydration management Aggressive dehydration and non-aggressive insulin administration. Insulin administration: Remember: ▪ Glargine (Lantus) and Detemir (Levemir) cannot be mixed with short acting insulins. ▪ Rapid acting insulins such as Lispro are “see food” insulins. Make sure the patient eat prior to administration. RI insulins are the only insulin that can be given IV. 244 NCLEX-RN study guide 100 m 1 2 3 4 Aspirating insulins: 1. Inject air to NPH (cloudy) insulin 2. Inject air to Regular (clear) insulin 3. Do not remove needle from Regular insulin, aspirate desired amount 4. Aspirate desired amount from NPH. 245 NCLEX-RN study guide 100 m Oral hypoglycemics (OHA): OHA Example Mechanism Common effects ↑ insulin sensitivity ↑ glucose uptake ↓ Glycogenolysis (glycogenolysis: breaking down glycogen to form glucose) GI upset: Weight loss Lactic acidosis Remember: Cannot be given to patient undergoing procedures given with iodine contrast or ↑BUN, ↑creatinine. It may compromise kidney function because kidney’s normal response is to excrete iodine and excessive waste such as lactic acid. Glimepiride, Glipizide, Glyburide Stimulates β-cells to secrete insulin Hypoglycemia Weight gain Pioglitazone ↑ insulin sensitivity Weight gain, edema May cause liver damage, CHF, fracture Nateglinide Repaglinide Stimulates β-cells to secrete insulin Hypoglycemia Weight gain Sodium – glucose transporter inhibitor Canagliflozin Dapagliflozin Prevents reabsorption of glucose in kidneys, promotes excretion of glucose Diuresis, glucosuria Hypotension Weight loss Alpha glucosidase inhibitors Acarbose Miglitol Slows the digestion of carbohydrates and delay glucose absorption GI upset, bloating, diarrhea Weight loss Biguanide “first line Metformin drug” Sulfonylureas “ 3Gs” Thiazolidinediones /Glitazones “TZDs” Glinides Weight loss: Biguanide Sodium–glucose transporter inhibitor Alpha glucosidase inhibitors Weight gain: Sulfonylureas Thiazolidinediones/Glitazones Glinides 246 NCLEX-RN study guide 100 m Acute management: DKA and HHS 1 Fluid management: (24-48 hours: 6-8 L/day) Isotonic (0.9% NaCl): Replaces loss fluids Hypotonic (0.45% NaCl): to reverse cellular dehydration by forcing fluids from intravascular to intracellular space. Insulin management: 2 3 Can be concurrent with fluid management (higher priority). More aggressive in DKA than HHS Potassium management: (Preventing cardiac arrhythmias) The administration of sodium bicarbonate solution to correct acidosis is controversial. There is little evidence that it improves outcomes beyond standard therapy. It may actually lead in certain complications. 1. Fluid bolus 2. If CBG ≤ 250 mg/dl D5W for 8 hours (dextrose containing to prevent sudden hypoglycemia and a hypotonic solution to maintain cellular hydration) 3. If s/s of dehydration are still (+) D5W + NaCl for 12 hours 1. Insulin bolus (0.1 units/kg) 2. Insulin infusion (0.1 units/kg/hr.) If CBG not decreased by 10%: Repeat loading dose (0.1 units/kg) If no response: Double dose (0.2 units/kg) 2. If CBG ≤ 250 mg/dl D5W for 8 hours (dextrose containing to prevent sudden 1. <3.5 meqs/L (mmol/L): hypoglycemia and a hypotonic 20-30 meqs/L solution to maintain cellular hydration) 2. 3.5 5.5dehydration meqs/L (mmol/L): 3. If s/s– of are still (+) 20-30 meqs/L D5W + NaCl for 12 hours 3. ≥5.5 meqs/L (mmol/L): Discontinue potassium 247 100 m NCLEX-RN study guide Other endocrine disorders: Turner vs. Klinefelter syndrome Question: The nurse is caring for an adolescent client diagnosed with type 1 diabetes. The client exhibits hot, dry skin and a glucose level of 350 mg/dL (19.4 mmol/L). Arterial blood gases show a pH of 7.27. STAT serum chemistry labs have been drawn. Cardiac monitoring shows a sinus rhythm with peaked T waves, and the client has minimal urine output. What is the nurse's next priority action? 1. Administer IV regular insulin 2. Administer normal saline infusion 3. Obtain urine for urinalysis 4. Request prescription for potassium infusion 248 100 m NCLEX-RN study guide Answer: 2 Rationale: This client has diabetic ketoacidosis (DKA). All clients with DKA experience dehydration due to osmotic diuresis. Clients with DKA and hyperosmolar hyperglycemic state require IV normal saline as a priority due to severe dehydration. Once fluids are given as a bolus, insulin is initiated. Potassium should never be given until the serum potassium level is known. Peaked T waves indicate hyperkalemia in this client. Potassium repletion is started once the serum potassium levels are normalized or trending low (from elevated levels). 249 NCLEX-RN study guide 100 m 12 Anatomy and Physiology Gastrointestinal 250 NCLEX-RN study guide 100 m Common disorders affecting GI tract: Peptic ulcer disease (PUD) (Gastric vs Duodenal ulcers) Parts of the stomach: Cardia: secretes mucus (water & glycoproteins) by Foveolar cells Fundus and body: contains parietal cells that secretes HCl acid and chief cell’s pepsinogen (digests protein) Antrum: secretes gastrin (also found in duodenum and pancreas) stimulates parietal cells to secrete HCl acid. Remember: With all this acids in the stomach, it can digest the whole of its tissues an duodenum. However, Brunner gland in duodenum secretes mucus that contain bicarbonate to neutralize this acids. Stomach also has a thicker layers than duodenum which is momentarily exposed to acids. Finally, prostaglandin in stomach and duodenum continuously stimulates mucus & bicarbonate secretion, which inhibits acid secretion and stimulates epithelial growth by promoting vasodilation. Gastric ulcer Mechanism Etiology Duodenal ulcer Loss of protective mechanism causing break in the inner lining of the stomach Loss of protective mechanism causing break in the inner lining of the duodenum (first part of the small bowel/intestines) Helicobacter Pylori bacteria (most common cause: Common in low income settings. It releases enzymes (adhesins, proteases) that cause adhesion and damage to mucosal and Foveolar cells (secrets mucus & glycoproteins) NSAIDs: Inhibits prostaglandin synthesis causing less mucus and bicarbonate secretions. Zollinger Ellison syndrome (Gastric tumor): Parietal cells secrete excess HCl acid H. Pylori: causes both gastric and duodenal ulcers NSAIDS: causes both ulcers but mostly gastric Zollinger Ellison: mostly causes gastric ulcer but it can also extend up to the distal end of duodenum. 251 NCLEX-RN study guide 100 m Common site of ulcer Classic S/S Complications Diagnostics Lesser curvature of the antrum ▪ Epigastric pain: aching and burning PAIN WHILE EATING: Relieved by vomiting ▪ Bloating, belching, vomiting ▪ Weight loss: d/t vomiting and less desire to food because of pain upon eating Hemorrhage: d/t untreated deep ulcer that affects the nearby artery Perforation: This allows gastric content into peritoneum. This leads to peritonitis. Remember: Peritoneal space is usually sterile. Peritonitis is a serious condition to any GI disorders that can lead to septic shock. Upper endoscopy with biopsy: biopsy is done to see if there is malignancy or H. Pylori infection Proximal part of duodenum (right after pyloric sphincter) ▪ Epigastric pain: aching and burning. PAIN IF NOT EATING: Relieved by food (eating) ▪ Bloating, belching, vomiting ▪ Weight gain as food intake relieves pain Same Same H. Pylori test: blood, breath, stool Treatment Prevent substances that triggers ulcer: smoking, alcohol, caffeine, NSAIDs Same Triple Therapy (for H. Pylori infection): Amoxicillin + Clarithromycin + PPIs Acronym: ABCP Anti-ulcers A: Antacids (Aluminum, Magnesium) B: Blockers (H2 blockers) “dine” (Ranitidine, Cimetidine) C: Cytoprotective “fate” (Sucralfate) P: Proton pump inhibitors “zole” (Pantoprazole, Omeprazole) Remember: Antiulcer medications cause diarrhea except Aluminum which causes constipation. 252 100 m NCLEX-RN study guide Gastric surgeries: Treatment for stomach cancer, severe PUD Billroth I: (Gastroduodenostomy) - removal of the distal two-thirds of the stomach; the remaining stomach is anastomosed to the duodenum. Billroth II: (Gastrojejunostomy) - removes the distal two-thirds of the stomach, the remaining is anastomosed to jejunum. Roux operations (Roux-en-Ys): Gastric bypass surgeries for many indications such as gastric cancer, treatment of morbid obesity, reconstruction of previous surgeries, etc. Roux-en-Y distal gastrectomy: An end-to-side surgical anastomosis of bowel used to reconstruct the GIT. Typically, it is between stomach and small bowel that is distal (or further down the gastrointestinal tract) from the cut end. Roux-en-Y Gastric bypass: (RYGB) procedure uses a small proximal portion of the stomach to create a gastric pouch that is anastomosed to the Roux limb (the food recipient portion) of the small intestine, bypassing most of the stomach and a portion of the duodenum. 253 100 m NCLEX-RN study guide Common complication (gastric surgery): Dumping syndrome Dumping syndrome: Rapid emptying of hypertonic gastric contents into the duodenum and small intestine. This process leads to fluid shift from the intravascular space to the small intestine. Remember that hypertonic solution attracts fluid from an area of lower concentration to higher concentration. This mechanism leads to hypotension and activation of the sympathetic nervous system. Symptoms include abdominal pain, diarrhea, nausea and vomiting, dizziness, generalized sweating, palpitations and tachycardia. Imagine the feeling after periods of starvation, eating rapidly and dumping volume of food to your stomach and eventually to duodenum for absorption. How much would it feel more for a patient with smaller stomach capacity? Nursing Care: ▪ Delay gastric emptying ▪ Small, frequent meals - reduces the amount of food ▪ High in protein and fat - take longer to digest and will remain in the stomach longer than carbohydrates ▪ Drink fluids between meals (at least 30-60 mins before or after meals) - fluids with meals would promote passage of stomach contents into the jejunum easily and worsen symptoms ▪ Low carbohydrates carbohydrates are broken down into simple sugars easily ▪ High in fiber – delay the emptying of the stomach and prevent rapid absorption of simple sugars ▪ Eat slowly, Low fowler’s (while eating) Avoid sitting up, low fowler’s to flat position (after eating) - gravity increases gastric emptying. Lying down after meals would slow down gastric emptying. 254 NCLEX-RN study guide 100 m Post-operative diet progression: Clear vs. Full liquid vs. Soft Common disorders affecting GI tract: Celiac disease (Gluten enteropathy) Gluten: A group of various proteins found in wheat and in other grains such as barley and rye. Moderate quantities are found in oat (depending on the variety). Contains gliadin that triggers immune response. Celiac disease (Gluten enteropathy): An autoimmune disorder in which chronic inflammation caused by gluten damages the small intestines. The inflammation is mediated by T cells, leads to disruption of the structure and function of the small bowel's mucosal lining and causes malabsorption as it impairs the body's ability to absorb nutrients, minerals, and fatsoluble vitamins A, D, E, and K from food. 255 100 m NCLEX-RN study guide S/S: Malabsorption to: ▪ Water: causes diarrhea ▪ Fat: causes Steatorrhea (malodorous fat in the stool) ▪ Iron: causes microcytic anemia ▪ Vitamin B12: causes macrocytic anemia Other S/S: ▪ Failure to thrive in children ▪ Weight loss Diagnostics: Biopsy, serum antibodies Remember: Inflammatory response usually happens to duodenum because it is the first to get exposed to gluten. Ironically, this is where majority of the absorption process takes place. In fact, celiac disease is one of the most common cause of malabsorption syndrome. Can have: 3 C’s Corn, Cassava, Coconut Cannot have: 4 C’s Cakes, Cereals, Cookies, Crackers Cannot have: 4 P’s Pasta, Pretzel, Pizza, Pastries In general: Avoid BROW B: Barley (high amounts) R: Rye (high amounts) O: Oat (depending on variety) W: Wheat (high amounts) 256 NCLEX-RN study guide 100 m Common disorders affecting GI tract: Inflammatory bowel disease (IBS): Crohn's disease vs. Ulcerative colitis Crohn's disease (Regional enteritis) Mechanism Etiology Classic S/S Complications An inflammatory response that affects anywhere of the GI tract. It is immune related, which means it is triggered by a foreign pathogen in the GI (e.g. Pseudomonas). The inflammatory response is uncontrolled and unregulated that leads to destruction of the cells in the GIT. Characteristics: ▪ It affects all layers (transmural) ▪ Can affect any (mouth-anus) ▪ Most common site is ileum ((RLQ) ▪ Scattered or in patches “patchy” Genetics - familial ▪ Abdominal pain: crampy, RLQ pain associated with ileum site ▪ Diarrhea: d/t malabsorption of water in the colon (3-4 /day) ▪ Bloody stool (porridge like): d/t damaged intestinal tissues ▪ Fever: d/t inflammatory response ▪ Malabsorption: d/t affectation of the small intestine (most commonly ileum) ▪ Weight loss: d/t malabsorption ▪ Abscess to sepsis ▪ Fistula: d/t perforating ulcer ▪ Peritonitis Ulcerative colitis More common than Crohn’s disease. An inflammatory response that affects the colon (large intestines including the rectum). Autoimmune related, which means the body’s own immune cells promotes inflammatory response. It characterized by remission (healing) and flares (exacerbation/new damage). Characteristics: ▪ Affects mucosa and submucosa only ▪ Affects colon only ▪ Most common site is recto/sigmoid (LLQ) ▪ Continuous (from area to another) ▪ Autoimmune ▪ Genetics - familial ▪ Diet and stress ▪ Abdominal pain: crampy, LLQ pain associated with recto/sigmoid ▪ Diarrhea (More severe and painful): d/t malabsorption of water in the colon (10 or more x /day). More severe since it mainly affects colon where water is absorbed. ▪ Bloody stool (mucoid like with pus) ▪ Fever: indicates flares ▪ Malabsorption and weight loss (seldom): because it does not affect small intestines ▪ Dehydration: d/t severe diarrhea ▪ Toxic megacolon: rare but serious d/t severe inflammation causing air trapping in the colon. This leads to enlargement and rupture. 257 NCLEX-RN study guide 100 m Diagnostics Treatment ▪ Upper GI series (barium swallow) ▪ Lower GI series (barium enema) ▪ Colonoscopy with biopsy ▪ ↑ESR, ↑C-reactive protein (CRP): indicates chronic inflammation ▪ CBC: Anemia d/t malabsorption ▪ Colonoscopy with biopsy ▪ Lower GI series (barium enema) ▪ CT scan/MRI ▪ Anti-inflammatory - Prednisone, Infliximab (Remicade) ▪ Antibiotics – Ciprofloxacin, Metronidazole ▪ Prevent flares (healthy lifestyle) ▪ Depends on the severity: Anti-inflammatory: Sulfasalazine, Mesalamine, Prednisone, Cyclosporine, Azathioprine For severe forms: Infliximab Antibiotics: generally not useful Surgery: Colectomy Remember: IBD vs. IBS Inflammatory bowel disorder (IBD) is different from irritable bowel syndrome (IBS). IBD is a chronic incurable inflammatory GI disease whereas IBS is a functional disorder that does not cause permanent damage. IBD is characterized by severe diarrhea while IBS is alternating constipation and diarrhea 258 100 m Colostomies: NCLEX-RN study guide Remember: Clients with a descending or sigmoid colostomy drain stool that is more formed and similar to a normal bowel movement that requires irrigation. Although less common, irrigating this colostomies create a bowel regimen that allows patient to wear a smaller pouch or a dressing over the stoma. Remember: The colostomy stoma should be beefy red in the immediate postoperative period. Any discoloration to the stoma could indicate decreased blood supply to the area; the nurse should notify the HCP. Colostomies can be permanent or temporary by performing colostomy reversal procedure. Stool characteristics: Possible etiologies 259 NCLEX-RN study guide 100 m Common disorders affecting GI tract: Diverticular disease Diverticular disease: ▪ Diverticular disease of the colon occurs when saclike protrusions form in the large intestine (can also happen in small intestine). ▪ When diverticula become infected and inflamed, the client has diverticulitis. ▪ Usually asymptomatic unless inflamed. ▪ Most common site is sigmoid colon (LLQ) (d/t smaller space or diameter=higher pressure “La Place’s law”). ▪ Exaggerated or abnormal smooth muscle contractions d/t chronic constipation mainly causes formation of diverticula. Diagnostics: ▪ CT scan ▪ Colonoscopy and barium enema : contraindicated during acute stage d/t risk of perforation Management: ▪ Prevent constipation: High fiber diet to prevent constipation causing inflammation of the diverticula (diverticulitis) During diverticulitis: Rest bowel ▪ NPO status: severe case ▪ Low-fiber/clear liquid diet: if not severe ▪ IV fluids (when NPO) ▪ IV Pain relief and antibiotics ▪ Preventing increased intraabdominal pressure (avoid straining): to avoid perforation ▪ Avoid laxatives and enemas: prevent perforation Etiology: forming the diverticula ▪ Increase colonic pressure: d/t chronic constipation, low fiber diet ▪ Fatty and red meat intake Cause: Diverticulitis (inflammation) ▪ Lodged fecalith (e.g. seeds as small or smaller than “pencil eraser”) ▪ Erosion from high pressure Classic S/S: Diverticulitis ▪ Painless rectal bleeding: Blood in the stool (hematochezia) d/t rupture of the blood vessels that traverses the muscle layer of the colon (can be both present in diverticulitis and diverticulosis itself) ▪ Pain in the LLQ: associated with sigmoid affectation Remember: Pain that is not in LLQ may be a sign of perforation affecting other portion of the colon Complication: Fistula: connects nearby organ Perforation: leading to peritonitis 260 NCLEX-RN study guide 100 m Common disorders affecting accessory organs of GIT: Liver cirrhosis Liver cirrhosis: Characterized by chronic scarring and damage of liver tissues. This is due to constant processing of alcohol (Laennec’s cirrhosis), exposure to Hepatitis B virus, or any long term or chronic state of hepatocyte destruction such as drugs (hepatotoxicity). At any point, this can cause fibrotic tissues to build up and eventually becomes irreversible. This process is called liver cirrhosis (end stage liver damage) Estrogen metabolism: Inactivates harmful estrogen metabolites Detoxification: Converts ammonia to urea Liver cirrhosis: Gynecomastia, Palmar erythema, Spider nevi, Caput medusae (estrogen promotes vasodilation, and capillary fragility Clotting factors production: Ability to coagulate blood Liver cirrhosis: Easy bruising Bleeding Liver cirrhosis: Encephalopathy Asterixis – flappy tremors Fetor hepaticus – musty breath Bile production: Breaks down fats in the duodenum Albumin : Maintains oncotic pressure Liver cirrhosis: Ascites Edema Liver cirrhosis: Jaundice, pruritus (d/t build-up of bile salts in skin) Clay colored stool and dark urine (d/t bile in the circulation instead of draining to GIT) Glucose metabolism, iron storage: Source of energy, HgB processing Liver cirrhosis: Weakness, Fatigue Weight loss Complication Mechanism Hepatic encephalopathy Ammonia that is not converted to urea travels to circulation and eventually to the CNS. Remember that any form of acids, practically all waste products can cause CNS depression. Other symptoms associated with encephalopathy: Altered mental status (confusion, agitation, lethargy, somnolence), seizure and coma. 261 NCLEX-RN study guide 100 m Portal hypertension Constant fibrosis and scarring leads to increase pressure in the portal circulation affecting the “portal triad” (hepatic artery, hepatic vein, bile duct). Increase pressure causes cascade of manifestations such as ascites when fluid is pushed out of the blood vessels. In addition, portosystemic shunt happens where fluid channels thru a lower pressure towards systemic circulation (inferior vena cava – heart). This abnormal build-up of fluids results into vasoconstriction of the vessels involving kidneys resulting into renal failure aka hepatorenal syndrome. Other manifestations: Splenomegaly, hepatomegaly Congestive heart failure (CHF) Results when the heart compensates due to fluid build-up which resulted from portal hypertension Esophageal varices Results from collateral portal blood flow through vessels in the stomach and esophagus. When these blood vessels become enlarged, they are called varices and are more likely to rupture. Rupture often leads to severe bleeding. Diagnostics: ▪ Gold standard: Liver biopsy ▪ Laboratory findings: Liver enzymes (elevated AST, ALT, alkaline phosphatase) elevated bilirubin, low albumin, Elevated PT/INR, Elevated ammonia, low platelet Treatment: generally irreversible ▪ Prevent liver damage: identify the cause (e.g. stop alcohol, treat hepatitis) ▪ Liver transplant ▪ Supportive treatment: Antipruritic: Cholestyramine (Questran) promotes excretion of bile salts Albumin replacement: to prevent ascites Prevent encephalopathy or elevated ammonia levels: Lactulose - promotes excretion of colonic bacteria (thru feces) as it plays a role in ammonia production. Remember: 3x bowel movement is the goal of lactulose treatment. 262 NCLEX-RN study guide 100 m Spider angioma (spider nevi, telangiectasia) Capput medusae (“medusa” snake hair, jellyfish) 263 NCLEX-RN study guide 100 m Tubes and drains: Remember: Keep scissors at the bedside at all times; monitor for respiratory distress, and if it occurs, cut the tubes to deflate balloons. Double port Linton–Nachlas tube 1. gastric balloon 2. gastric suction Lumen Triple port Sengstaken Blakemore 1. gastric balloon 2. gastric suction 3. esophageal balloon Quadruple port Minnesota Tube 1. gastric balloon 2. gastric suction 3. esophageal balloon 4. esophageal suction Nasogastric Nasointestinal Single Lumen Levine Cantor Double lumen Salem Sump Miller Abbott Remember: Acronym single lumen “single word” Levine and Cantor tubes, double lumen “double word” Salem Sump and Miller Abbott 264 NCLEX-RN study guide 100 m Remember: Continuous suction can be applied to decompress the stomach if a double lumen Salem-sump tube is in place. The larger lumen is attached to suction and the smaller lumen (within the larger one) is open to air as an air vent. The air vent (blue pigtail) must remain open as it provides a continuous flow of atmospheric air through the drainage tube at its distal end (to prevent excessive suction force). This prevents damage to the gastric mucosa. If gastric content refluxes, 10-20 mL of air can be injected into the air vent. However, the air vent is kept above the level of the client's stomach to prevent reflux. Common disorders affecting accessory organs of GIT: Acute pancreatitis, Acute cholecystitis Protecting the pancreas from being auto digested: Pancreas itself continuously produces ZYMOGEN (inactive enzyme) to prevent the enzymes from digesting proteins in the cells in which they are made of or synthesized. Pancreatitis: A condition characterized by inflammation of the pancreas. Functions: ▪ Endocrine (islets of Langerhans): 1% ▪ Exocrine (acinar cells): 99% (production of digestive enzymes for metabolism) Trypsin: protein Amylase: carbohydrates Lipase: Lipid 265 100 m NCLEX-RN study guide Cullen’s Sign Grey Turner’s Sign Hypocalcemia Chvostek’s Sign: facial spasm when touched Trousseau Sign: Carpal (hand) or pedal (foot) spasm once irritated The gallbladder (storage of bile): Digestion of fats When there is fat ingestion, the small intestines produces cholecystokinin (CCK) to stimulate gallbladder to contract and ejects bile through cystic duct (passage ways) to empty in the duodenum to aid in the digestion of fats. Cholecystitis: In gallbladder containing stones (cholelithiasis), during contraction, one of this stones may lodge in the cystic duct. If large enough, this causes backflow of bile to gallbladder and causes inflammatory response. Continuous squeezing (contraction) causes the pain as the classic sign. 266 100 m NCLEX-RN study guide Jaundice: Bile leaks into blood Murphy’s Sign Remember: Pneumoperitoneum Patients who undergone laparoscopic procedure is at risk for accumulation of air in the peritoneum. CO2 is used in insufflating the abdomen during the procedure. If the CO2 is retained, it can irritate the phrenic nerve causing respiratory failure. Patient should be instructed to ambulate asap to eliminate CO2. Turning sideside may also help. 267 NCLEX-RN study guide 100 m Acute pancreatitis Acute cholecystitis Mechanism Autodigestion: The enzymes itself are digesting the pancreas d/t premature activation of zymogen. This causes cascade of mechanisms leading into massive inflammatory response. Inflammatory response: d/t large bile stones (cholelithiasis) blocking the cystic duct. Infection may also occur since E.coli, clostridium etc. are all over the gut. Etiology ▪ Alcohol abuse: alcohol enhances early activation of zymogen. It becomes clogged up in the pancreatic duct (ducts are passageways of enzymes towards the duodenum for digesting food). Subsequently, these contamination of zymogen in the pancreas is activated to become trypsin (digestive enzyme). This cascade also promotes activation of other digestive enzymes. Remember that alcohol has a dehydrating effect, it favors the same mechanism. In addition, alcohol also promotes inflammatory response. ▪ Gallstones: blocking d/t gallstones promotes backflow of pancreatic enzymes, thereby auto digesting the tissues. ▪ Abdominal pain: epigastric radiating to back ▪ Fever ▪ Nausea/Vomiting ▪ Tachycardia ▪ Loss of appetite Classic S/S ▪ Hemorrhagic type: d/to rupture of the small vessels Grey turner’s sign -bluish discoloration of the flanks Cullen’s sign – bluish discoloration of the umbilicus Gallstone: Predisposes the Fs ▪ Fair complexion: more prevalent to Caucasians ▪ Fat: high fat intake ▪ Female, Fertile, Forty (age ≥40: Estrogen are made up of fat cells itself. Estrogen imbalance predisposes fat deposition ▪ Familial Abdominal pain: Mid epigastric to RUQ (radiates to scapula and shoulders). Rebound tenderness when palpated. It is also usually in response to eating high fatty food due to continuous release of CCK. Murphy’s sign: Positive when RUQ is palpated while patient is instructed to inhale and suddenly stops, complains of pain and catches breath. (pain upon inhalation) Jaundice: if the stone lodges further down to common bile duct, the bile from the liver backflows to itself. Increase bile in the bile ducts of the liver causes increase pressure and 268 NCLEX-RN study guide 100 m bile is pushed into the blood vessel. Others S/S: ▪ Fever ▪ Nausea/Vomiting ▪ Tachycardia ▪ Loss of appetite Remember: Acute pancreatitis is a very severe kind of inflammation. It means you expect severe complications. Complications ▪ Hypovolemic shock: d/t hemorrhage ▪ Disseminated intravascular coagulation (DIC): the body used up the coagulation function, in effect, if there is needed coagulation it cannot produce more coagulants, causing bleeding. ▪ Cyst abscess: d/t a massive inflammatory response ▪ Hypocalcemia: necrosis (fat necrosis) d/t massive inflammation consumes a lot of calcium. Peritonitis: d/t rupture or the microorganisms invading the wall of the gallbladder and into the peritoneum. Remember: Pancreatic function depends on the precise flow of calcium within the acinar cells. In short, calcium is a way of life for pancreas ▪ ARDS (non-cardiogenic pulmonary edema): d/t massive inflammatory response that affects the lung tissues. Diagnostics Elevated Lipase(more specific) Elevated Amylase CT scan, USD Endoscopic retrograde cholangiopancreatography (ERCP) ▪ Magnetic resonance cholangiopancreatography (MRCP) ▪ ▪ ▪ ▪ ▪ Elevated alkaline phosphatase: Necrotic ductal cells release these enzymes ▪ CT scan, USD ▪ HIDA scan (Cholescintigraphy): Measures gallbladder bile ejection ▪ Endoscopic retrograde cholangiopancreatography (ERCP) ▪ Magnetic resonance cholangiopancreatography (MRCP) 269 NCLEX-RN study guide 100 m Treatment ▪ REST BOWEL: NPO, NGT if severe vomiting ▪ Nutritional support while NPO: TPN ▪ Pain management: IV Morphine Remember: There is no conclusive study suggests that morphine causes spasm in sphincter of oddi. ▪ Anti-nausea/emetic: Zofran (ondansetron) ▪ Antipyretic ▪ Hydration: IV Fluids, replace electrolyte ▪ Treat complications: Oxygen, Antibiotics ▪ REST BOWEL: NPO, NGT to low intermittent suction (LIS) ▪ Pain management: IV NSAIDs: Ketorolac IV Morphine ▪ Anti-nausea/emetic: ▪ Zofran (ondansetron) ▪ Antipyretic ▪ Hydration: IV Fluids, replace electrolyte ▪ Treat complications: Antibiotics ▪ Surgery: Open cholecystectomy, Laparoscopic cholecystectomy 270 NCLEX-RN study guide 100 m Common GIT disorders: Appendicitis Appendicitis: The appendix is a blind pouch located at the junction of the ileum of the small intestine and the beginning of the large intestine (cecum). When infected or obstructed (foreign body, fecal material, tumor, lymph tissue), the appendix becomes inflamed, causing acute appendicitis. Appendicitis is an acute condition that needs immediate surgical intervention to prevent appendix rupture and subsequent peritonitis and sepsis. Causes: Obstruction ▪ Fecalith: hard fecal matter ▪ Undigested seeds ▪ Pinworm infections: intestinal parasites ▪ Lymphoid hyperplasia: common in children and adolescent when growing, also caused by viral infections. Mechanism: Inflammation The inflammatory process causes increase pressure and eventually migration of E. coli (common gut flora). S/S: ▪ Fever, Elevated WBC: d/t inflammatory process ▪ Nausea/vomiting ▪ RLQ (Mc Burney’s point) pain: d/t inflammation irritating the nearby nerves. Radiates to umbilicus. Complications: Further pressure Compression of the blood vessels leads to ischemia and the appendiceal walls becomes weaker and ruptures. Leakage means peritonitis and eventually septic shock. Management: ▪ REST BOWEL: NPO, NGT if severe vomiting ▪ Pain management: IV Morphine: Nowadays, there are no concerns of masking the symptoms of peritonitis iv giving analgesics ▪ Anti-nausea/emetic ▪ Antipyretic ▪ Hydration: IV Fluids, replace electrolyte ▪ Treat complications: Antibiotics ▪ Surgery: Open, Laparoscopic appendectomy 271 100 m NCLEX-RN study guide Other signs: Appendicitis Psoas Sign Irritation or pain upon Hip Flexion Obturator Sign Irritation or pain on hip flexion and abduction Rouvsing Sign Pain on RLQ upon palpation of the LLQ Flexion 272 100 m NCLEX-RN study guide Blumberg Sign Rebound tenderness on palpation of abdomen (indicates peritonitis) Areas of referred pain in the abdomen: 273 NCLEX-RN study guide 100 m Common GI disorders in children: Pyloric stenosis vs Intussusception vs Hirschsprung’s disease Pyloric stenosis Stenosis of the pyloric sphincter causing backflow of food into stomach and esophagus due to increasing pressure. ▪ Projectile vomiting: d/t increasing pressure in the stomach ▪ Non bilious vomitus: because food is not drained yet to duodenum d/t stenosis ▪ Olive shaped mass: visible swollen stomach Intussusception Hirschsprung’s One part of the intestine prolapses and then telescopes into another part. It is one of the most frequent causes of intestinal obstruction during infancy. Aka Aganglionic megacolon: the segment lacking neurons (aganglionic) becomes constricted, causing the normal, proximal section of bowel to become distended with feces. Aganglionic also means loss of bowel tone or movement leading to fecal impaction ▪ LLQ pain: d/t fecal impaction that usually ▪ RLQ pain (intermittent affects the recto-sigmoid cramping): guarding colon behavior or drawing up legs. ▪ Meconium ileus: unable to It usually affects the terminal pass out stool within 24 hour part of ileum to ascending after birth d/t constricted colon (small-large space) portion. This sign can be ▪ Currant jelly stool: mixed present in cystic fibrosis (d/t mucus and blood d/t dehydrated stool) adhesions ▪ Ribbon like stool: passing ▪ Sausage shaped mass: out stool resulting from a visible mass d/t telescoping constricted portion in the rectum. Complication: dehydration d/t vomiting Complication: dehydration d/t diarrhea, Bowel ischemia (Necrosis) Complication: Toxic megacolon develops due to relative fecal stasis including sepsis Surgical repair: Pylorotomy ▪ Enema to push the telescoping out: Air enema is better than barium d/t relative effects of constipation or fecal impaction ▪ Surgery: for bowel ischemia Surgical resection (removal): colostomy can be done and reversed. 274 NCLEX-RN study guide 100 m Common GI diagnostic procedures : Upper GI series vs Lower GI series, ERCP vs MRCP Procedure Mechanism Nursing care Pre-procedure: ▪ NPO 8 hours before the Radiographic (X-ray) test examination of the Post-procedure: upper gastrointestinal ▪ Expect the passage of (GI) tract. The chalky, white stool until esophagus, stomach, all barium contrast has and duodenum are been expelled made visible on X-ray film ▪ Take a laxative (e.g., Upper gastrointestinal series by a liquid suspension. magnesium This liquid suspension (barium swallow) hydroxide[Milk of may be barium or a Magnesia]) to assist in water-soluble contrast. If expelling the barium. only the pharynx and Retained barium can esophagus are lead to fecal impaction examined with barium, ▪ Drink plenty of fluids to the procedure is called a promote hydration and barium swallow. eat a high-fiber diet to prevent constipation. Pre-procedure: ▪ Take a cathartic (e.g. magnesium citrate, Uses fluoroscopy to polyethylene glycol) to visualize the colon empty stool from the outlined by contrast to colon. detect polyps, ulcers, ▪ Clear liquid diet the tumors, and diverticula. day before the procedure: (avoid red Lower gastrointestinal series Remember: This and purple liquids) procedure is (barium enema) ▪ NPO 8 hours before the contraindicated for clients with acute test diverticulitis as it may Post-procedure: rupture inflamed ▪ Take a laxative (e.g., diverticula and cause magnesium subsequent peritonitis. hydroxide[Milk of Magnesia]) ▪ Drink plenty of fluids 275 100 m NCLEX-RN study guide An invasive procedure in which an endoscope is passed through the mouth into the duodenum to assess the pancreatic and biliary ducts. Using fluoroscopy with contrast media (iodine dye) during the procedure, the ducts can be visualized and treatments including Endoscopic retrograde cholangiopancreatography removal of obstructions, dilation of strictures, and (ERCP) biopsies can be performed. Pre-procedure: ▪ NPO 8 hours before the test ▪ Assess for iodine allergy (dye allergies) ▪ Assess kidney status: BUN creatinine d/t use of contrast dye (nephrotoxicity) Post-procedure: ▪ You will not be allowed to eat or drink anything until your gag reflex has returned. ▪ Instruct patient to report: Fever or chills, abdominal pain, N/V: may indicate pancreatitis ▪ Black, tarry, or bloody stools (perforation) Remember: Perforation or irritation of these areas during the procedure can cause acute pancreatitis, a potentially lifethreatening complication after an ERCP. A noninvasive diagnostic Pre-procedure: test used to visualize the biliary and hepatic ducts ▪ Assess for contraindications prior via MRI. MRCP uses oral to the procedure, or IV gadolinium Magnetic resonance including presence of (noniodine contrast cholangiopancreatography certain metal implants material) and is a safer, (MRCP) (e.g. pacemaker, less invasive alternative aneurysm clip, to ERCP to determine the cochlear implant), cause of cholecystitis, pregnancy. cholelithiasis, or biliary obstruction. 276 NCLEX-RN study guide 100 m 13 Musculoskeletal Anatomy and Physiology How does muscles contract? Skeletal muscles: Neuromuscular junction Calcium triggers release of ACH (action-potential). ACH binds to nicotinic receptors (cholinergic receptors) in the muscle cells to cause contraction. A smooth muscle is excited by external stimuli, which causes contraction. Smooth muscle contractions are involuntary movements triggered by impulses that travel through the autonomic nervous system (ANS) to the smooth muscle tissue. 277 NCLEX-RN study guide 100 m Common disorders: Arthritis Rheumatoid arthritis (RA) Chronic inflammatory (autoimmune): Human leukocyte antigen (HLA), which are present in these individuals are triggered by environmental factors (e.g. smoking, pathogens) to cause inflammatory process. The process involves immune cells (RH ABs, IgM Abs) that attack the synovium (joints). It is also associated with other autoimmune diseases such as SLE, scleroderma etc. Osteoarthritis (OA) Progressive loss of articular cartilage (a connective tissue that allows gliding of joints without friction): This results in significant friction of bones and eventually generates inflammation. The high tensile strength and elasticity of articular cartilage helps weight bearing joints (knees & hips) distribute the weight from one bone to the other. The progressive loss of elasticity in years promotes inflammatory responses to the whole synovium. Gouty arthritis (GA) Hyperuricemia: Levels of uric acid exceeds the level of solubility and excretion through urine. This results into formation of urate crystals (sharp crystals) which usually accumulates in areas with low blood flow. Overtime, this promotes inflammation to joints (chronic gout) 278 NCLEX-RN study guide 100 m ▪ Autoimmune ▪ Genetics ▪ Environment ▪ Symmetrical: affects same joint groups at the same sides of the body ▪ Peripheral to Weight bearing joints (as disease progresses) PAIN: ▪ Cyclical (from AM-PM) ▪ Last in several hours ▪ Not relieved by rest ▪ AM pain last > 1hr ▪ Pain with swelling DEFORMITIES: ▪ Boutonnière deformity ▪ Swan-Neck deformity Others non-specific S/S: Fever, malaise, low appetite ▪ Blood test: Rheumatoid factor (RH Ab) ▪ Imaging: X-rays Low bone density, bone erosions, narrowing of the joint space, soft tissue swelling ▪ ▪ ▪ ▪ Age Joint injury Obesity Mechanical stress: overuse ▪ Asymmetrical: can affect only one knee, hip joints ▪ Weight bearing to peripheral joints (as disease progresses) PAIN: ▪ AM – PM (worst in PM) d/t overuse ▪ Last in few hours, Relieved by rest ▪ AM pain last < 1hr ▪ Pain without swelling DEFORMITIES: ▪ Bouchard’s deformity (proximal interphalangeal) ▪ Heberden’s deformity (distal interphalangeal) ▪ Imaging: X-rays Joint space narrowing, osteophytes (bony projections from outward growth) Primary hyperuricemia: Unknown Secondary hyperuricemia: ▪ Acquired ▪ Diet: increase purine ▪ Obesity ▪ Chemotherapy & radiation (Tumor lysis syndrome) ▪ CKD ▪ Medications: Thiazide diuretics and aspirin ▪ Variable symmetry ▪ Usually affects “big toe” (aka Podagra) PAIN: ▪ AM or anytime of the day precipitated by high purine intake ▪ Podagra: In AM (big toe burning pain) ▪ May last in several hours ▪ May not be relieved by rest ▪ AM pain last > 1hr ▪ Burning pain, tender, swelling DEFORMITIES: ▪ Tophi (uric deposits): d/t repeated gouty attacks ▪ Synovial fluid: definitive (+) urates ▪ Blood test: Elevated uric acid ▪ Imaging: X-rays Bone erosions 279 NCLEX-RN study guide 100 m Disease modifying antirheumatic drugs (DMARDs): Acronym: ELISA + Methotrexate E: Etanercept L: Leflunomide I: Infliximab S: Sulfasalazine A: Anakinra Methotrexate Remember: This medications are aimed to modify the disease by minimizing the symptoms of chronic inflammation and minimize chances of flare-ups as an autoimmune disease. This leads to longer remissions than exacerbations. ▪ Non-pharmacologic: ▪ Weight loss (exercise) ▪ Physical therapy ▪ Pharmacologic: reducing pain and inflammation ▪ NSAIDs ▪ Hyaluronic injections to joints ▪ Surgery: ▪ Hip replacement ▪ Knee replacement ▪ Non-pharmacologic: ▪ Low purine diet ▪ Hydration (promotes solubility of uric acid) ▪ Pharmacologic: reducing pain and inflammation ▪ NSAIDs ▪ Steroids DOC: ▪ Colchicine: Antiinflammatory (acute gout) ▪ Allopurinol: decrease uric acid levels (chronic gout) ▪ Probenecid: increases excretion of uric acid (chronic gout) 280 100 m NCLEX-RN study guide Dietary modifications: ▪ Increasing fluid intake (2 L/day): to help eliminate excess uric acid ▪ Implementing a low-purine diet: particularly avoiding organ meats (e.g. liver, kidney, brain) and certain seafood (e.g. sardines, shellfish) ▪ Limiting alcohol intake, especially beer: alcohol competes with the excretion of uric acid in kidneys ▪ Low-fat diet: as excess dietary fats impair urinary excretion of urates Hip and knee replacement: 281 100 m NCLEX-RN study guide Nursing: Preventing complications ▪ Provide abduction pillow between the legs- to prevent adduction of the affected leg (prosthesis dislocation) ▪ Do not flex the affected hip more than 90 degrees – prevent prosthesis dislocation ▪ Provide elevated toilet seats and chairs that do not recline. ▪ Assess for signs of hip dislocationincluding shortening and internal rotation of the leg. Assess for s/s of complications: DVT or PE, infections, hemorrhage Complications: ▪ Bleeding ▪ Prosthesis dislocation ▪ Deep vein thrombosis (DVT) ▪ Infection Average stay post operatively: 3-5 days (full weight bearing by discharge) 282 NCLEX-RN study guide 100 m Common disorders: Developmental dysplasia of the hip (DDH) aka Congenital hip dysplasia Normal development: ▪ Femoral head stays fitted with the acetabulum ▪ Grow together DDH: ▪ Femoral head dislocates out of acetabulum ▪ Grow out of proportion ▪ Unable to form stable joint S/S: <2-3 months ▪ Extra gluteal or inguinal folds/Asymmetrical folds ▪ Affected leg shorter when flexed together (Galeazzi sign) ▪ Laxity/instability: (+) Barlow and (+) Ortolani maneuvers (done only by physician) Remember: If DDH is not treated, these signs disappear after age 2-3 months d/t the development of muscle contractures. Etiology: ▪ Unknown ▪ Breech position of baby: too much force against fetal thigh ▪ First borns: uterus is not yet stretch-out putting pressure to fetal thigh ▪ Low amniotic fluid: not enough room for fetus’ legs Key management: Maintain abduction ▪ Proper swaddling technique ▪ Choosing infant carriers or car seats with wide bases-infant seats. Avoiding any positioning device, seat, or carrier that causes hip extension with the knees straight and together. ▪ Pavlik harness (1-6 mos. old) ▪ Closed reduction with Spica cast (6-18 mos.) 283 100 m NCLEX-RN study guide Ortolani maneuver: Done after Barlow maneuver. If (+) dislocation is determined (Barlow maneuver), abducting the adducted leg results into a clicking sound, (+) Ortolani. Galeazzi sign: performed by flexing an infant's knees when they are lying down so that the feet touch the surface and the ankles touch the buttocks. If the knees are not level then the test is positive, indicating a potential DDH 284 NCLEX-RN study guide 100 m Pavlik harness: ▪ Regularly assess skin for redness or breakdown under the straps ▪ Dress the child in a shirt and knee socks under the harness to protect the skin ▪ Avoid lotions and powders to prevent irritation and excess moisture ▪ Lightly massage the skin under the straps every day to promote circulation. ▪ Only apply 1 diaper at a time (wearing ≥2 diapers increases risk of incorrect hip placement ▪ Apply diapers underneath the straps to keep harness clean and dry Spica cast: ▪ Keep the cast clean and dry ▪ Check carefully beneath the cast edges for skin impairment (redness, etc.) ▪ If the cast becomes damp, it can be dried by exposing it to air during the child's nap or dryer on a cold setting ▪ Assess for s/s of abdominal pain. This can be a sign of Cast syndrome (superior mesenteric artery syndrome). A rare condition which compresses the SMA (major artery) that leads to GI ischemia and necrosis. Common disorders: Fat embolism 285 100 m NCLEX-RN study guide Medullary cavity: Located in the center of long bones ▪ Red marrow – for blood cell formation ▪ Yellow marrow – contains mainly fats Fat embolism syndrome (FES): A rare, but life-threatening complication that occurs in clients with long bone and pelvis fractures. It can also occur in non-trauma– related conditions, such as pancreatitis and liposuction. It usually develops 24-72 hours following the injury or surgical repair. S/S: The FES triad (Respiratory/Neurological/Petechiae) ▪ Respiratory problems (e.g. dyspnea, tachypnea, hypoxemia) after a fat embolus travels through the pulmonary circulation and lodges in a pulmonary capillary, leading to impaired gas exchange and acute respiratory failure (similar to PE) ▪ Neurologic changes (e.g. AMS, confusion, restlessness) d/t cerebral embolism and hypoxia ▪ Petechial rash (e.g. pin-sized purplish spots that do not blanch with pressure), which appears on the neck, chest, and axilla d/t microvascular occlusion. This is a distinguishing characteristic from PE. Fever : d/t a cerebral embolism leading to hypothalamus dysfunction. Management: Non specific Minimizing movement of a fractured long bone and early stabilization of the injury with surgery reduce the risk for fat emboli. 286 NCLEX-RN study guide 100 m Common disorders: Acute compartment syndrome ACS: Is a serious complication due to neurovascular compromise from swelling and increased pressure in a confined space. This swelling of the soft tissues surrounding the blood vessels compresses the blood and lymphatic vessels further, causing more fluid to enter the extracellular spaces, leading to additional compression. This worsening cycle can eventually lead to tissue ischemia and necrosis. Classic S/S: The 6 Ps Early: Pain: Increasing despite elevation, analgesics, and ice. Pressure: Digits are firm and tense; shiny tight skin Paresthesia: Tingling, numbness, burning sensation, (nerve ischemia) Pallor: Capillary refill is >3 seconds (poor perfusion) Late: Pulselessness Paralysis: Loss of function (e.g. Volkmann paralysis) Diagnosis: ▪ Clinical signs/symptoms (6Ps) ▪ Posterior compartment: Pain upon dorsiflexion ▪ Anterior compartment: pain upon plantar flexion ▪ Blood test: Elevated myoglobin, elevated CK-MB Remember: Elevated amounts of myoglobin overwhelms kidney that leads to kidney failure. This condition is also known as rhabdomyolysis. Management: ▪ Hydration: to eliminate myoglobin thereby preventing kidney failure ▪ Fasciotomy: a large incision to decompress the compartments. It remains exposed for several days (upto 2 weeks). Risk for infection is a priority. ▪ Amputation: if treatment options are ineffective 287 100 m NCLEX-RN study guide Common disorders: Carpal tunnel syndrome Carpal tunnel syndrome (CTS): CTS is caused by compression of a median nerve within the carpal tunnel at the wrist. Any swelling in the canal puts pressure on the nerve and produces pain and paresthesia in the median nerve distribution (first 3½ digits). Symptoms often worse at night when the wrists are flexed during sleep after a day of use. 288 NCLEX-RN study guide 100 m Etiology: ▪ Genetics ▪ Work related: Stress to d/t repetitive tasks (e.g. typing), force, posture, & vibration Associated conditions: ▪ Arthritis ▪ Acromegaly ▪ Obesity ▪ Pregnancy: d/t hormonal changes (fluids retention) Management: ▪ Behavior modification (e.g. wrist support while typing) ▪ Physical therapy: isometric exercise and stretching ▪ Splinting ▪ Steroids ▪ Surgery: relieving pressure in median nerve (Pain and tingling may last several months after surgery which normally subsides gradually) Diagnosis: ▪ Physical symptoms ▪ Phalen’s maneuver: flexing wrist as far as possible for 1 min. (+) tingling or pain ▪ Tinel’s maneuver: tapping the median. (+) tingling or pain ▪ Durkan’s test: manually compressing the median nerve. (+) tingling or pain 289 100 m NCLEX-RN study guide Assistive devices: Crutches and cane 2 point gait: 1. Advance bad leg and crutch on the side of good leg together 2. Advance good leg and crutch on the side of bad leg together. 3 point gait: 1. Advance both crutches 2. Advance bad leg 3. Advance good leg 4 point gait (most stable): 1. Advance crutch on the side of good leg 2. Advance bad leg 3. Advance crutch on the side of bad leg 4. Advance good leg Remember: In assistive devices using cane and crutches, the acronym “good goes to heaven” and “bad goes to hell” applies. It means, good leg first on going up and bad leg first on going down using stairs. In addition, assistive device should always go together with the bad leg, one or the other advances or simultaneously. 290 100 m NCLEX-RN study guide Using stairs: Going up: Modified 3 point gait 1. Advance good leg (goes to heaven) 2. Advance both crutches 3. Advance bad leg Going down: 3 point gait 1. Advance both crutches 2. Advance bad leg (goes to hell) 3. Advance good leg Remember: Acronym “COAL” in holding cane C – Cane held O – Opposite from A – Affected L – Leg 291 100 m Using stairs: Going up: 1. Advance good leg (goes to heaven) 2. Advance cane 3. Advance bad leg Going down: 1. Advance cane 2. Advance bad leg (goes to hell) 3. Advance good leg NCLEX-RN study guide 292 NCLEX-RN study guide 100 m Tractions: Skin vs skeletal traction Principles: ▪ Must produce pulling effect ▪ Counter traction must be maintained ▪ Traction and counter pull/traction must be opposite direction ▪ Ropes must move freely ▪ Precise amount of weight must be applied and must hang freely Purpose: ▪ Relieve spasms/promoting comfort ▪ Promotes alignment ▪ Maintains immobilization Buck’s (skin traction): A type of skin traction used for fracture of the hip and femur. The upper body must be flat on bed to promote counter traction. The affected leg is placed with pillow to prevent swelling and decrease tension. Types: ▪ Skin ▪ Skeletal (uses tong, metal pins and wires) Russel’s (skin traction): A type of skin traction used for fracture of the femur similar to Buck’s traction. However, it uses upward pull as a counter traction in addition to own upper body traction. It can also utilize metal pins and tongs, in this case it is called a skeletal traction. 293 100 m NCLEX-RN study guide 294 Nursing care: Traction Bryant’s (skin traction): A type of skin traction used for fracture of the femur in children age 2 years or under 20-30 lbs. Buttocks should be off the bed and legs at right angle to the body Dunlop’s (skin traction): A type of skin traction used for fracture of the arm (humerus, radius, ulna). Used when closed reduction is difficult or traumatic. Elbow flexed at 45 ° (radial/ulnar fracture as illustrated above), horizontal elbow (humerus fracture). T – Temperature checks for infection d/t applied metal pins and tongs aka pin tract infection (skeletal traction) R – Ropes hanging freely maintaining counter traction A – Analgesia (relieve pain) C – Circulation (check neurovascular status - 6Ps) T – Trapeze bar to assist in mobility (prevents pneumonia) I – Infection (assess for s/s of associated infection e.g. pneumonia, pin tract infection) O – Output and intake (maintain hydration) N – No weights on the floor (must be hanging freely) Cervical (skeletal traction): A type of skeletal traction that uses tongs (e.g. Crutchfield tongs) to promote traction to patients with cervical fractures. Weights are used as counter tractions. 100 m NCLEX-RN study guide Scoliosis: Characterized by lateral curvature and spinal rotation to the spine. Caused by congenital or pathologic conditions, it is most often determined to be idiopathic (unknown cause). Commonly first noticed during periods of rapid growth, particularly during early adolescence in girls. Screening for early detection: Girls (age 10-12) Boys (age 13-14) Braces for scoliosis: A type of skin traction device that uses with the same purposes such in traction. Boston brace, Wilmington brace are thoracolumbosacral orthosis (TLSO) braces. Milwaukee brace is cervical thoracolumbosacral orthosis (CTLSO) Nursing care: ▪ Perform proper skin care ▪ Wear a cotton t-shirt under the brace ▪ Do not use lotion or powder can cause skin irritation beneath the brace. ▪ Most braces are worn for up to 23 hours/day and removed for bathing and exercise ▪ Address psychosocial needs (e.g. body image, socialization) 295 NCLEX-RN study guide 100 m 14 Integumentary Anatomy and Physiology The Skin Function: Protection: an anatomical barrier from pathogens and damage Sensation: contains a variety of nerve endings that react to heat and cold, touch, pressure, vibration, and tissue injury Heat regulation: contains a blood supply greater than its requirements, allows control of energy loss by radiation, convection, conduction. Control of evaporation: provides a relatively dry and semi-impermeable barrier to fluid loss Storage and synthesis: storage center for lipids and H20, and synthesis of vitamin D Excretion: sweat contains urea Skin flora: competes with transient pathogens for nutrients, secreting chemicals against them, or by stimulating the skin's immune system. 296 NCLEX-RN study guide 100 m Common disorders: Burns Burns Classification SUPERFICIAL DEEP Characteristics: ▪ Painful, swelling ▪ Normal capillary refill ▪ Blanchable redness SUPERFICIAL Affects: Dermis ▪ Dry/red (erythema) ▪ Painful Remember: This is not included in TBSA (rule of 9 calculation) EPIDERMIS (1°) Characteristics: ▪ Minimal – No pain ▪ Non blanchable redness SUPERFICIAL Partial Thickness Affects: Parts of dermis ▪ Red and moist with blisters ▪ Very painful DEEP Partial Thickness Affects: All dermis ▪ Pale to red ▪ Minimal pain ▪ Damaged blood vessels ▪ Extravasation DERMIS (2°) Full Thickness Affects: Hypodermis (SQ) ▪ Leathery gray or charred black ▪ No pain d/t damaged nerves HYPODERMIS (3°) Associated Problems: Evaporation: 30-50 ml/hr. evaporation leading to hypovolemia Anemia: d/t destruction of RBC by injury Hyperkalemia: d/t shifting of electrolytes resulting from cellular injury Infection: d/t loss of barrier function Pain: d/t inflammatory process and affecting nerve endings 297 NCLEX-RN study guide 100 m Rule of 9: Total body surface area (TBSA) Remember: Burns needing referral to HCP ▪ ≥ 10% TBSA ▪ Deep thickness (partial or full) ▪ Circumferential/around the area (leads to compartment syndrome) ▪ Inhalation burns ▪ Chemical burns ▪ Electrical burns Remember: Use rule of palm (1%) to each scattered small wounds. Remember: Does not need referral (minor burns) ▪ < 10% TBSA ▪ Superficial burns First aid: ▪ Flush with cool (not ice cold) water ▪ Prevent further burning ▪ Manage pain 298 NCLEX-RN study guide 100 m Burns management: 1 2 Resuscitative/Emergent phase: Burns with ≥ 15% TBSA given 24-48 hrs. Goal: Prevent hypovolemia ▪ Parkland Rule (ml/day) ____% (TBSA) X WT (kg) X 4 ml Isotonic solution: ▪ Hartman Solution/PLR (Preferably d/t added electrolytes & stays longer in the serum) Acute phase: After hemodynamically stable Goal: Prevent infection, Pain management ▪ IV antibiotics (≥60% TBSA) ▪ Wound care ▪ NSAIDs, Morphine Example: Parkland (ml/day) 50 % (TBSA) X 80 kg X 4 ml = 16,000 ml/day 1st 8 hrs. 50% = 8,000 ml 2nd 8 hrs. 25% = 4,000 ml 3rd 8 hrs. 25% = 4,000 ml Total: 16,000 ml/day (24°) Rehabilitative phase: Goal: Return of optimum function 3 ▪ Emotional support ▪ Surgical debridement (if needed) Common disorders: Hospital acquired pressure ulcer (HAPU) HAPU classification Affects: Epidermis Affects: Epidermis to dermis (e.g. blister) 299 NCLEX-RN study guide 100 m Affects: Epidermis to hypodermis (SQ) Unstageable: Mostly covered by slough or necrotic tissue Affects: Epidermis to muscles and bones SDTI: Skin is intact but with purple discoloration d/t possible deep tissue injury Common types of dressing: Transparent dressing: For stage 1 pressure ulcer (protective dressing) Foam dressing: For stage 2 exudative pressure ulcer (absorbent) 300 NCLEX-RN study guide 100 m Duoderm dressing: For stage 2 pressure ulcer (moist wound healing). The wound moist itself promotes debridement. Hydrogel dressing: For stage 3 or 4 pressure ulcer (hydrates and promotes debridement) Question: A client is brought to the emergency department after sustaining thirddegree burns over 50% of the body. Which solution is the best choice for fluid resuscitation in this client? 1. 0.45% normal saline 2. 5% dextrose in 0.9% normal saline (D5NS) 3. 5% dextrose in water (D5W) 4. Lactated Ringer's solution Answer: 4 Rationale: Hypovolemic shock and electrolyte imbalance is a priority in patients with burns. In the emergent/resuscitative phase of burn management, it is critical to establish an airway and replace fluids and electrolytes. LR remains in the intravascular space longer than other solutions, which helps to stabilize blood pressure and avert shock. Hypotonic solutions (e.g. 0.45% normal saline) quickly leave the intravascular space and are not useful in replacing intravascular volume. They may also contribute to peripheral and interstitial edema, which can lead to pulmonary complications. Hypertonic solutions (e.g. D5NS , 3% saline) can cause further electrolyte imbalances in a client with severe burns, resulting in hypernatremia and arrhythmias. Although technically an isotonic solution, D5W once infused and metabolized by liver is a hypotonic solution and free water is released to the tissues rather than remaining in the intravascular space. 301 NCLEX-RN study guide 100 m 15 Visual & Auditory Anatomy and Physiology Eye Important components: ▪ Cornea, the anterior chamber, and lens: Refraction (focusing ability of the eye) ▪ Ciliary body: Accommodation, aqueous humor production and resorption ▪ Aqueous humor: Providing oxygen, nutrients, and metabolic waste removal to the lens and the cornea (which do not have their own blood supply) and provides structural support of the eye (keeping the shape of the eye) Remember: Intraocular pressure depends on the levels of production and resorption of aqueous humor (IOP: 12 -15 mmHg) ▪ ▪ Retina: Translates image into electrical neural impulses to the brain to create visual perception (Rods: Black/white, Cones: Color) Macula: Responsible for the central, highresolution, color vision. 302 NCLEX-RN study guide 100 m Common disorders: Macular degeneration vs Retinal detachment Age related Macular degeneration (AMD) Age related degeneration Mechanism Etiology ▪ Dry AMD (90%): related to decrease blood supply ▪ Wet AMD (10%): Related to abnormal formation of blood vessels ▪ Environmental: Smoking, HTN, Atherosclerosis, Hyperlipidemia, Exposure to UV ▪ Genetics Classic S/S Los of central vision Diagnostics ▪ Amsler grid: Grid of horizontal and vertical lines used to monitor a person's central visual field. ▪ Fundoscopy: aka ophthalmoscopy ▪ Fluorescein angiography: Technique for examining the circulation of the retina and choroid using a dye & a specialized camera. Treatment ▪ Preventive: Lifestyle modification ▪ Laser coagulation: for wet AMD ▪ Stem cell implant Retinal detachment Involves a break or separation in the retina that allows the fluid in the eye to get behind the retina. Can be caused by injury or inflammation of the eye. ▪ Trauma/Injury: Cataract surgeries, high impact sports, glaucoma ▪ DM retinopathy ▪ Painless (d/t absent pain receptors in retina) ▪ Floaters ▪ Curtain sensation ▪ Flashes of light ▪ Clinical S/S ▪ Fundoscopy: aka ophthalmoscopy ▪ Ocular ultrasonography ▪ Laser coagulation ▪ Pneumatic retinopexy: a gas bubble is injected into the eye after which laser or freezing treatment is applied to the retinal hole to push the retinal back. ▪ Scleral buckling: Silicone bands push the wall of the eye inward against the retinal hole 303 NCLEX-RN study guide 100 m Loss of central vision Amsler grid Pneumatic retinopexy Curtain sensation Scleral buckling 304 NCLEX-RN study guide 100 m Common disorders: Glaucoma (COAG vs ACAG) Glaucoma: Characterized by increase IOP (normal: 12-15 mmhg) which results to damage in the optic nerve and cause vision loss. IOP is a function of production of aqueous humor by the ciliary processes of the eye, and its drainage through the trabecular meshwork. Aqueous humor flows from the ciliary processes by the lens posteriorly and anteriorly by the iris. It then flows through the pupil of the iris into the anterior chamber. Furthermore, trabecular meshwork drains aqueous humor via the scleral venous sinus (Schlemm's canal) into scleral plexuses and systemic blood circulation. Any problem to its drainage system causes increase in IOP in a fixed space like the eye. Increase IOP (intraocular hypertension) means at ≥25 mmhg causes symptoms of glaucoma. Chronic open angle glaucoma (COAG) Acute close angle glaucoma (ACAG) Most common: Open angle between cornea and iris. However, the drainage system slowly gets clogged overtime. This results gradual (chronic) increase IOP to optic nerve. ▪ Age ▪ Genetics ▪ Prolonged use of steroids (steroidinduced glaucoma) ▪ DM retinopathy: d/t restricted blood Close (narrow) angle between cornea and iris. This results into backflow of aqueous humor and thereby pushing the lens against the iris. This build-up of fluid is rapid enough to cause acute symptoms. Classic S/S ▪ Does not have acute S/S ▪ Loss of peripheral vision (tunnel vision): d/t atrophy of the outer rim of the optic nerve. Eventually leads to central vison loss. ▪ Eye pain, Headache, Nausea ▪ Blurred vision, Eye redness, ▪ Visual halos, Loss of peripheral – central vision (if not treated promptly) Diagnostics ▪ Tonometry: assess IOP ▪ Visual field testing ▪ Gonioscopy: anterior chamber angle examination ▪ Optical coherence tomography (OCT): To obtain detailed images from within the retina. Same Mechanism Etiology ▪ Trauma ▪ Surgery 305 NCLEX-RN study guide 100 m Goal: Early detection, Decrease IOP Treatment Medication: ▪ Alpha 2 adrenergic agonist: ↓ aqueous humor production & ↑outflow. (e.g. Brimonidine) ▪ Prostaglandin analogs: ↑outflow (e.g. Bimatoprost) ▪ Beta blockers: ↓ aqueous humor production(e.g. Timolol) ▪ Carbonic anhydrase inhibitors:↓ aqueous humor secretion (e.g. acetazolamide) ▪ Laser trabeculoplasty (ALT): Used to treat open-angle glaucoma temporarily (not a cure) ▪ Trabeculectomy: Partial thickness flap is made in the scleral wall and a window opening is made under the flap to remove a portion of the trabecular meshwork Goal: Decrease IOP, preventing further damage ▪ Medication: same with COAG ▪ Trabeculectomy 306 NCLEX-RN study guide 100 m Loss of peripheral vision (tunnel vision) Errors of refraction: Myopia (nearsightedness), Hyperopia (farsightedness), Astigmatism Myopia: Light rays focus in front of the retina d/t irregular shape lens. Correction with biconcave lens (thinner) to reach the retina Hyperopia: Light rays focus behind the retina d/t irregular shape lens. Correction with biconvex lens (thicker) just enough to reach the retina Astigmatism: Light rays focus on more than one point (unequal refraction). Correction with lens depending on the errors. 307 NCLEX-RN study guide 100 m Common disorders affecting external, middle, inner ear Otitis externa (Swimmer’s ear) Mechanism Etiology Alteration in the protective environment of the external ear that results into infection. It can also lead into otitis media. ▪ Swimming ▪ Minor trauma from cleaning ▪ Using hearing aids and ear plugs Pathogens: Pseudomonas, E. Coli, S. Aureus Otitis media Inflammation or infection of the middle ear. The eustachian tubes in infants and young children are short, wide, and fairly horizontal, which results in ineffective draining of respiratory secretions and a potential for recurrent infections. Age group: < 2 YO ▪ Recurring exposure to tobacco smoke ▪ Regular pacifier use, after age 6 months (d/t constant sucking) ▪ Drinking from a bottle while lying down ▪ Lack of immunization Pathogens: S. Pneumoniae, H. influenza (HIB), R. syncytial virus (RSV) Classic S/S ▪ Ear pain ▪ Fever, irritability ▪ Ear pain: upon pulling ▪ Conductive and sensorineural hearing the tragus loss (if not treated) ▪ Ear discharge, itchiness Remember: Sudden ▪ Temporary conductive absence of fever and hearing loss pain is a sign of perforated tympanic membrane. Diagnostics ▪ Clinical S/S ▪ History of URTI ▪ Ear examination: Otoscope (bulging tympanic membrane distinguish OM from otitis externa) ▪ Clinical S/S ▪ Ear examination: Otoscope Meniere’s disease (Endolymphatic hydrops) Endolymphatic hydrops: excessive build-up of the endolymph fluid, which fills the hearing and balance structures of the inner ear. This build-up of fluid may be caused by immune response. ▪ Autoimmune ▪ Genetics Triad: ▪ Vertigo ▪ Ringing in the ears (tinnitus), ▪ Hearing loss (sensorineural) Clinical S/S 308 NCLEX-RN study guide 100 m DOC: Amoxicillin Treatment Prevent further infection DOC: Ciprofloxacin If failed: Myringotomy/tympanos tomy: incision is created in the eardrum (tympanic membrane) to relieve pressure caused by excessive buildup of fluid, or drain pus. Tympanostomy tube (grommet) to keep the middle ear aerated to prevent reaccumulation of fluid. DOC: ▪ Thiazide diuretics ▪ Acetazolamide 309 100 m NCLEX-RN study guide How to distinguish conductive hearing loss (reversible) from sensorineural hearing loss (irreversible)? Conductive hearing loss is temporary and it affects external and middle ear. Sensorineural hearing loss affects inner ear and is irreversible kind of hearing loss. Remember: Weber and Rinne tests are done on an existing hearing loss of an affected ear. This is to distinguish what kind of hearing loss the patient is manifesting. Weber test: Tap a tuning fork and placed on top of the head. Interpretation: Considering the patient complained of a hearing loss in the right ear. ▪ If the patient cannot hear on that right ear, patient is having a sensorineural hearing loss ▪ If the patient hears louder on that affected right ear (lateralization), the patient is experiencing conductive hearing loss. Rinne’s test: 1. Tap a tuning fork and place in front of the affected ear 2. If the patient does not hear anymore sound from the tuning fork, place behind the ear. Interpretation: Considering the patient complained of a hearing loss in the right ear. ▪ After placing the tuning fork (step 2) behind the ear and still hears it: sensorineural hearing loss ▪ If the patient does not hear it otherwise: conductive hearing loss. 310 100 m NCLEX-RN study guide Question: The nurse is planning care for a client experiencing an acute attack of Meniere disease. Which action is a high priority to include in the plan of care? 1. Initiate fall precautions 2. Keep the emesis basin at bedside 3. Provide a quiet environment 4. Start intravenous fluids Answer: 1 Rationale: Clients with Meniere disease (endolymphatic hydrops) can have severe vertigo, tinnitus, hearing loss, and aural fullness. It is a priority for the nurse to institute safety measures, such as fall precautions, for these clients. All other choices are correct but are not priority. 311 NCLEX-RN study guide 100 m 16 Hematology/Oncology Anatomy and Physiology Hematopoiesis Bone marrow (hematopoietic stem cells) Myeloid (Blast cells) Erythrocyte (RBC): Gas exchanges Megakaryocyte (Platelet): Blood coagulation Lymphoid (Blast cells) Monocyte Migrates to tissues and become macrophages (e.g. Alveolar macrophages in the lungs, Kupffer cells in the liver, Microglia in the brain) Granulocyte Basophils: Allergic reaction Eosinophils: Allergic reactions, parasitic infections Neutrophils: Most abundant, bacterial infections Agranulocytes: T-cells and B-cells B-cells: Mature in bone marrow (B) T-cells: Mature in Thymus gland (T) Plasma B-cells: T-cells: Antibody /immunoglobulin (Ig) production IgG – Crosses placental barrier (most abundant) IgA – abundant in secretions, found in breastmilk IgM – First Ig to migrate in the area of infection Cytotoxic (CD8)– destroys virus, tumor cells Suppressor/regula tory: Shuts down immunity T-helper (CD4) – Orchestrates immune response Memory T-cells Specific immunity to previous pathogen IgE – Allergic reaction IgD – Unknown function Memory B-cells: Specific immunity to previous pathogen 312 100 m NCLEX-RN study guide Common disorders affecting RBCs: Anemias Hemoglobin: Heme: iron containing compound where O2 binds. Globin: protein chains where hemes are wedged. Heme and globin are both involved in binding and transport of O2. 2 alpha, 2 beta chains Anemia: Is a decrease in the total amount of RBC or hemoglobin in the blood, or a lowered ability of the blood to carry O2. 313 NCLEX-RN study guide 100 m Anemias Mutations to globin chains Alpha Thalassemia: Major: 4 mutations (hydrops fetalis) Minor: 2 mutations Beta Thalassemia: (Cooley’s anemia) Major: 2 mutations Minor: 1 mutation Sickle cell anemia: Mutation to beta chains Deficiencies Megaloblastic: ▪ Vit B12 (Pernicious anemia) ▪ Vit B9 (Folic acid def. anemia) Iron deficiency Bone marrow suppression Aplastic anemia: (Fanconi’s anemia) (Low RBCs, WBCs, Platelets Pancytopenia) Remember: The 4Fs (Classic S/S of anemia) Fatigue Forgetfulness Fainting Fast heartbeat (tachycardia) Differentiating anemias: Microcytic vs macrocytic Hypochromic vs hyperchromic Remember: There are various types of anemias. In order to distinguish these types, microscopic test is made to determine the size and the color (morphology). On the other hand, a complete blood count test (CBC) is a more convenient test. Mean corpuscular HgB (MCH) for color and mean corpuscular volume (MCV) is for size. A normal sized RBC is normocytic while normochromic pertains to its normal red color. MCV: Determines size Normal: 80-90% Microcytic: <80% Macrocytic: >90% MCH: Determines color Normal: 27-33% Hypochromic: <27% Hyperchromic: >33% 314 NCLEX-RN study guide 100 m Anemias Overview Morphology Alpha thalassemia Major Minor Alpha thalassemia results in decreased alpha-globin production. This leads to a relative excess of beta globin chains. The degree of impairment is based on how many genes are affected. Alpha thalassemia major is associated with hydrops fetalis (e.g. hemolytic disease in newborn) where hemolysis is evident leading to accumulation of water in newborn. Microcytic, Hypochromic Beta Thalassemia: (Cooley’s anemia) Major Minor Characterized by reduced or absent synthesis of the beta chains of hemoglobin that results in severe anemia. In beta thalassemia major, it involves lifelong blood transfusion which later cause iron overload as a complication. Microcytic, Hypochromic Megaloblastic: Vit B12 deficiency (Pernicious anemia) Vit B9 (Folic acid deficiency anemia) Megaloblastic as the name says forms macrocytic type of RBCs. This is a result from abnormal RBC production d/t low vitamin B12 (cyanocobalamin) and vitamin B9 (folic acid), main components to create RBCs. Vit B12 (Pernicious anemia): Characterized by “red beefy tongue”. The deficiency is mainly d/t absence of parietal cells which secretes intrinsic factor necessary in Vit B12 absorption. Can be caused by low dietary intake, PUDs, gastritis, Zollinger Ellison (gastric cancer) Remember: Vitamin B12 is obtained only from animal proteins, so clients who follow a vegan diet are at high risk. Macrocytic, Normo/Hypochromic 315 NCLEX-RN study guide 100 m Vit B9 (FADA): Associated with neural tube defects in infants (spina bifida), chronic alcoholism and gastritis. Remember: Contrary to Vit B12, leafy green vegetables are the best dietary sources of folic acid. Other sources include, fortified grain products (e.g. cereals, bread, pasta) Iron deficiency (IDA) IDA is the most common chronic nutritional disorder in children. Iron-rich foods are leafy green vegetables, red meats, poultry, dried fruit and fortified cereals. It is also important to limit milk intake (16-24 oz/day) in toddlers to ensure a balanced diet. Microcytic, Hypochromic Remember: Over consumption of cow's milk (poor source of available iron) before age 1 year is a common cause. Aplastic anemia: (Fanconi’s anemia) Characterized by bone marrow suppression which leads to pancytopenia. The main cause is unknown. However, heredity, autoimmune response, or exposure to chemicals (benzene: major chemical in gasoline) and radiation can play a role. Normocytic, Normochromic Common disorders affecting RBCs: Sickle cell disease 316 NCLEX-RN study guide 100 m Sickle cell disease/anemia (SCD): Is a hereditary hemoglobinopathy in which normal hemoglobin is replaced with abnormal hemoglobin S in red blood cells (genetic mutation to beta chain). The cells change to a sickle shape with triggers such as dehydration, infection, stress, high altitude and extremes in temperature. In general, this triggers cause greater demand of O2 in the body. The sickling causes occlusion of small blood vessels with ischemia and damage to organs. Another reason is that the mutated beta chain has less affinity (attachment) to O2. Person with SCD survives as long as the environment has good oxygenation. SCD Increase levels of reticulocytes (immature RBCs) A counterregulatory mechanism by bone marrow in response to abnormal levels of RBCs d/t hemolysis. Effects: Hepato/splenomegaly: d/t crowding of the reticulocytes Enlarged cheeks: d/t new bone formation from expanded medullary cavities (overcrowding) Risk for infection: d/t splenomegaly (spleen: role in immune system) DOC: Hydroxyurea - Increases formation of fetal Hgb which has higher affinity to O2. Fetal Hgb is present at birth until 6 months, the primary reason why infants are asymptomatic with SCD. Vasoocclusive crisis Hemolysis Sickled cells stocked in the small capillaries impeding the circulation and causes variety of symptoms Repeated sickling causes premature destruction of RBCs (hemolysis) leading to Effects: Pain crisis: primary symptom of SCD Remember: Generalized pain is a common and a chronic symptom of SCD. Localized pain on the other hand is acute and needs to be addressed immediately. Dactylitis (swollen hands and feet in infants): Initial sign of SCD Splenic sequestration: characterized by severe abdominal pain which is a life threatening symptom. CVA: involving cerebral vessels Renal necrosis: causing hematuria and proteinuria Acute chest syndrome: characterized by chest pain affecting lung vasculature Priapism: prolonged painful erection as it affects vasculature in penis Effects: Anemia Hyperkalemia: as K+ leaks into the serum d/t RBC destruction Elevated bilirubin: biproduct of RBC metabolism is bilirubin Jaundice: d/t elevated bilirubin Gallstone formation: d/t elevated bilirubin Triggers: Promote sickling ▪ ▪ ▪ ▪ ▪ Dehydration Infection Stress High altitude areas Extremes in temperature. Remember: Hypoxia and deoxygenation of the RBCs in general causes the sickling, so administration of oxygen is the priority intervention. 317 100 m NCLEX-RN study guide Management: ▪ Prevent triggers ▪ O2 supplement - to prevent further sickling ▪ Hydration - aggressive intravenous and oral hydration is recommended (to reduce the viscosity of the blood) ▪ Pain control: Often need large doses of narcotics (round the clock) ▪ Infection prevention – age-appropriate vaccination ▪ Diet - the client is encouraged to have a high-protein, high-calorie diet with folic acid and a multivitamin without iron (IDA is uncommon to SCD) ▪ Folic acid - to help in the creation of the new red blood cells needed due to the hemolysis Question: A 32-year-old patient with sickle cell anemia is admitted to the hospital during a sickle cell crisis. Which action prescribed by the health care provider will you implement first? 1. Give morphine sulfate 4 to 8 mg IV every hour as needed. 2. Administer 100% oxygen using a nonrebreather mask. 3. Start a 14-gauge IV line and infuse normal saline at 200 mL/hr. 4. Give pneumococcal and Hemophilus influenzae vaccines. Answer: 2 Rationale: Hypoxia and deoxygenation of the RBCs are the most common cause of sickling, so administration of oxygen is the priority intervention here. Pain control and hydration are also important interventions for this patient and should be accomplished rapidly. Vaccination may help prevent future sickling episodes by decreasing the risk of infection, but it will not help with the current sickling crisis. 318 100 m NCLEX-RN study guide Common disorders affecting platelets: Thrombocytopenia Thrombocytopenia: Disseminated Intravascular coagulation (DIC) “consumption coagulopathy” Mechanism: Hemostasis out of control. Too much platelet is consumed d/t a massive injury in a certain area. As a result, other body parts tend to bleed. Etiology: Trauma, Abruptio placenta, sepsis, leukemia Diagnosis: ▪ Low platelet ▪ Elevated PT/INR, PTT ▪ Elevated D-dimer Management: ▪ Treat cause ▪ Blood transfusion ▪ Prevent bleeding Heparin induced thrombocytopenia (HIT) Mechanism: Due to administration of various forms of heparin. Regardless of its cause, thrombocytopenia usually results in bleeding. However, in HIT this usually leads to paradoxical venous and/or arterial thrombosis and less commonly to bleeding. The mechanism for thrombosis is unclear. The danger of HIT is risk of organ damage from local thrombi and/or embolization, leading to CVA or PE. Remember: Bleeding risk A priority assessment in a client with low platelets is any change in LOC (e.g. disorientation, lethargy, restlessness). This indicates intracranial bleeding and increased ICP. Thrombotic thrombocytopenic purpura (TTP) Mechanism: An immune response characterized by thrombosis in small blood vessels, d/t elevated Von Willebrand factor (clot creator). The platelet are stocked into fibrin (stabilizer) strands made by VWF resulting to low platelet count with hemolysis of the RBCs. Elevated VWF is d/t deficiency of ADAMTS enzyme (clot buster) Etiology: Autoimmune Remember: FAT RN F - Fever: immune response A – Anemia: hemolysis T – Thrombosis: ↑ VWF R – Renal: AKD d/t massive hemolysis N – Neuro: thrombotic CVA Diagnosis: ▪ Normal platelet ▪ Normal PT/INR, PTT ▪ Elevated Von Willebrand factor (VWF) Management: ▪ No platelet transfusion (worsens the problem) ▪ Plasmapheresis (adding ADAMTS enzyme) Idiopathic/Immune thrombocytopenic purpura (ITP) (Werlhof's Disease) Mechanism: An autoimmune disease with antibodies against several platelets. Primary ITP is unknown (idiopathic) while secondary ITP is d/t SLE. Platelets with Ig are rendered to spleen and phagocytized by splenic macrophages, Etiology: Idiopathic, autoimmune Diagnosis: ▪ Low platelet ▪ Normal PT/INR, PTT Management: ▪ Blood transfusion ▪ Prevent bleeding ▪ Steroids ▪ IV Immunoglobulins ▪ Splenectomy Remember: HIT Platelets <150,000 /mm3: continue treatment Platelet <40,000/mm3: Discontinue treatment (risk for bleeding) 319 NCLEX-RN study guide 100 m Common disorders affecting WBCs: Leukemia Myeloid/Myelocytic Affects the myeloid line of blood cells. The monocytes, erythrocytes (RBCs), megakaryocyte (platelets) and ,granulocytes (basophils, neutrophils, eosinophils) Chronic leukemia Characterized by partially immature cells. Gradually spills out and still causes crowding but in a slow progression. This mechanism also causes pancytopenia Acute leukemia The fully immature cells are >20% which more likely crowds abruptly. Crowding affects the production of other blood cells, RBCs, platelets and other WBCs regardless of the line originally affected Lymphoid/lymphocytic Affects the lymphoid line of blood cells. The agranulocytes (B-cells and T-cells) Acute Myeloid/Myelocytic leukemia (AML) Rare type which usually affects elders/adults. Rapidly progresses as an acute leukemia Chronic Lymphoid/lymphocytic leukemia (CLL) Usually affects elders >70 YO. Only affects the B-cells of the lymphoid line. Acute Lymphoid/lymphocytic leukemia (ALL) B-cell leukemia affects children and T-cell type usually affects teenagers. A very rare type of leukemia which progresses rapidly. Chronic Myeloid/Myelocytic leukemia (CML) Rare type which usually affects elders/adults. Characterized by mutation of the chromosome 22 (Philadelphia chromosome). Leukemia: Is a group of blood malignancies (cancer) that usually begin in the bone marrow and result in elevated count of abnormal and immature white blood cells. Classification is according to progression and the hematopoietic blood line affected. These blood cells are not fully developed and are called leukemia cells. Treatment involved are chemotherapy, radiation bone marrow transplant and supportive care. 320 NCLEX-RN study guide 100 m Remember: Acute myelodysplastic syndrome is not AML of leukemic origin. This is characterized by <20% blast cells of myeloid blood lines but it does progress rapidly causing the same symptoms such of AML. Common disorders affecting WBCs: Hodgkin’s vs Non-Hodgkin’s lymphoma Lymphoma Hodgkin’s lymphoma (+) Reed Sternberg cells on biopsy Lymphadenopathy usually in neck and chest Good Good prognosis A group of blood malignancies (cancers) that affects the lymphocytes. Most commonly B-cells. Mechanism: Migration to lymphoid tissues causing painless firm and movable lymphadenopathy (classic symptom). Other manifestations include: fever, night sweats (drenching type which rule out PTB), weight loss, loss of appetite. Treatment is usually chemotherapy, radiation and surgery. In addition, Burkitt’s lymphoma (severe form) causes rapid deterioration or death Non-Hodgkin’s lymphoma (-) Reed Sternberg cells on biopsy Lymphadenopathy usually affects upper and lower extremities Good Poor prognosis 321 NCLEX-RN study guide 100 m Common disorders affecting WBCs: Multiple myeloma Multiple myeloma Is a malignancy of plasma cells that produces antibodies, particularly affecting the IgG. The usual onset is 70 YO. Older patients are often experiencing other serious diseases, which affect survival. Diagnosis: ▪ BUN, creatinine ▪ Electrophoresis (M-protein spikes) ▪ CBC, Electrolytes (BMP) ▪ Bone marrow biopsy ▪ Ben jones proteins (tumor markers) ▪ Bone imaging Management: Supportive care, chemotherapy, bone marrow transplant C R C – Calcium Elevated calcium d/t lytic bone lesions caused by rapid growth of cancer cell Classic S/S: Bone pain to lower back (most common symptom) R – Renal Monoclonal antibodies called M-protein overwhelms the kidneys leading to kidney failure. Regular kidney function is checked to determine disease progression A A – Anemia Crowding of the cancer cells affects hematopoietic stem cells in the bone marrow. This also leads to low levels of WBCs and platelets. Risk for infection and bleeding B B – Back pain A common symptom related to hypercalcemia and pathological bone fractures. Spine and ribs are usually affected 322 NCLEX-RN study guide 100 m Cell cycle: G1 checkpoint Checks for: ▪ Cell size ▪ Nutrients ▪ DNA damage ▪ Growth factors G2 checkpoint Checks for: ▪ DNA damage ▪ DNA replication and completeness Remember: As cells move through the cell cycle, do they breeze through from one phase to the next? If they're cancer cells, the answer might be yes. Normal cells, however, move through the cell cycle in a regulated way. This regulation makes sure that cells don't divide under unfavorable conditions (for instance, when their DNA is damaged, or when there isn't room for more cells in a tissue or organ). 323 NCLEX-RN study guide 100 m Chromosomes, Genes, DNA: Remember: Cells are made up of trillions of cells. Cells contains nucleus where identical pairs chromosomes are located. One chromosome from each of its pair is inherited from each parent. Segments from each chromosomes are called genes. Lastly, genes are made up of DNA where the genetic make-up (information) is transcribed intricately through group of proteins overtime in an organized process. Any disturbance to this process is an abnormality. However, the human body has its own mechanism to autocorrect whatever is detected abnormal. This happens before it regularly undergoes cell division, carrying DNA information from one to the other. Chromosome: Humans has 23 pairs, designated 1 to 22 in order of decreasing size and X and Y (23rd) for the female and male sex chromosomes respectively. 324 NCLEX-RN study guide 100 m 325 DNA damage vs Mutation: Replication is the process of producing two identical replicas of DNA from one original DNA molecule. This process is the basis for biological inheritance. A DNA damage during replication can be repaired as it undergoes a process of correction overtime. In contrast, DNA mutation cannot be corrected and remains present in the new DNA strand because it is simply not recognizable. Then every time that strand of DNA is replicated the error will be carried to next cycle. Implication: Mutation or damage supports the idea of inheritance from one generation to another. Ironically, cancer occurs at anyone and at anytime in an unpredictable manner. How does cancer develop? It simply remains unclear. However there are available theories that supports the concept. Proto-oncogenes vs Oncogene (Tumor) suppressor theory: Proto-oncogene ▪ A dominant gene ▪ Promotes mutation ▪ More active and mutation becomes permanent once activated Oncogene suppressor ▪ A recessive gene ▪ Induces apoptosis (programmed cell death for damaged/non useful cells. ▪ Protects the stability of genetic make-up NCLEX-RN study guide 100 m Inheritance: Dominant vs recessive, Autosomal vs X-linked (Sex-linked) Dominant It only needs to inherit one copy of the gene for the trait to be expressed. For instance, if one parent has a dominant gene of a green eyes, there is 50 % chances that the child will have green eyes. Recessive Needs to inherit two copies of the gene from each parents for the trait to be expressed. Both parents must have recessive genes of green eyes for their child to have it at a 25% chance (both parents are carrier) X-linked (sex linked) The inheritance of a trait is determined by a gene located on one of the sex chromosomes (23rd Ch) Autosomal The inheritance of a trait is determined by a gene located on 1-22 chromosomes. X-linked Dominant Every affected person has at least one parent with a trait. A male with trait passes it on all his daughters. A female , may pass to both sons and daughters. e.g. Alport syndrome X-linked recessive Affected fathers do not pass to sons. Males manifest the disease than females. Females are carrier (passed from mother to son) e.g. Hemophilias, color blindness Autosomal dominant Affected fathers or mothers passes on the disease to both sons and daughters e.g. Marfan’s syndrome, polycystic kidney disease Autosomal recessive Males and females can be equally affected. Parents are asymptomatic carriers. e.g. Sickle cell disease, cystic fibrosis 326 NCLEX-RN study guide 100 m Benign tumors vs malignant tumors Benign ▪ Slow growing ▪ Capsulated ▪ Non invasive ▪ Do not metastasize ▪ Well differentiated ▪ Suffix “oma” e.g. Fibroma Malignant ▪ Fast growing ▪ Non-capsulated ▪ Invasive and infiltrating ▪ Metastasize ▪ Poorly differentiated ▪ Suffix “carcinoma or sarcoma” 327 NCLEX-RN study guide 100 m Common cancers: Early and late signs/symptoms Cancer Early S/S Late S/S Brain Headache Loss of consciousness Esophageal/ tracheal Hoarseness Dysphagia Stomach Indigestion/dyspepsia Chronic indigestion Lung Nagging cough Hemoptysis Dimpling “Peau d’orange” (breast skin is similar to orange peel) Asterixis (flapping tremors) Breast Lump Liver RUQ pain Colon LLQ pain Bloody stool Bladder Dysuria Hematuria Cervical/Uterine/ Ovarian Dysplasia from pap smear Foul smelling vaginal bleeding Testicular Dragging pain Spongy testes Skin Non healing sore Ulceration Bone Bone pain d/t easy fracture Deformity Bone marrow Exhaustion Pancytopenia 328 NCLEX-RN study guide 100 m Screening tests: CDC recommendation Cancer Screening tests (early detection) Breast Breast self-examination: Monthly starting age 20 YO Best time: End of the menstrual cycle (variable: few days after). This is the time when hormonal changes have the least influence on breast tissue, and the breasts are the least tender. Postmenopausal women/Irregular menses: Choose a day of the month (usually single digits to easily remember) and consistently perform breast self-exam on that same day every month. Mammogram: Annually starting age ≥ 40 YO Every 2 years (age ≥ 50-70 YO) Cervical Colorectal/colon Lung Pap Smear: Every 3 years age 21-65 YO >65 with previous positive (+) results/history of cervical cancer: Also needs testing >65 YO with negative (-) results: No need for testing Colonoscopy: Every 10 years age 50-75 YO, may also have sigmoidoscopy as an alternative (fairly quick and safe). Done every 5 years. If high risk may do fecal occult blood (FOB) done annually. Chest X-ray: Every year for chronic smokers Chronic smokers: 30 pack years or 1 pack/day and 15 pack years or 2 packs/day >80 YO or quit smoking for 15 years: no need testing Remember: Other screening test such as prostate examinations and testicular test examinations are not included according to CDC because of low probability and specificity issues. However, this test are still done to high risk individuals 329 NCLEX-RN study guide 100 m Treatment: Chemotherapy and radiation Chemotherapy Non Cell specific Cell specific Vina alkaloids ▪ Vincristine ▪ Vinblastine Antimetabolites ▪ 5 Fluorouracil (5FU) ▪ Methotrexate Adverse: Bone marrow suppression DOC to increase: WBC: Neupogen (Filgrastim) RBC: Epoetin (Epogen) PLT: Neumega (Oprelvekin) Infection risk : Neutropenic precaution Absolute neutrophil (ANC) Normal: 3,500 – 7000/mm3 Severe risk: <500/mm3 Moderate risk: 500-1000/mm3 Mild risk: 1000-1500/mm3 Insignificant: >1500/mm3 Acute tumor lysis syndrome (TLS): A potential complication of chemotherapy d/t rapid release of intracellular components such as potassium, phosphorus and nucleic acids into the bloodstream. This will cause hyperkalemia, hyperuricemia hyperphosphatemia. Released phosphorus binds calcium, producing calcium phosphate mixture but lowering serum calcium levels (hypocalcemia). Both calcium phosphate and uric acid are deposited into the kidneys, causing renal failure. Antibiotic antitumor ▪ Adriamycin ▪ Bleomycin Alkylating agents Hormones ▪ Tamoxifen ▪Cyclophosphamide “Those not mentioned” e.g. Cisplatin Adverse for antibiotic anti tumor: Pulmonary fibrosis Adverse for Hormones: “ACHES” A – Abdominal pain (bowel ischemia) C – Chest pain (PE or AMI) H – Headache (CVA) E – Eye problem (retinal ischemia) S – Severe leg pain (DVT) Remember: Hormones (estrogen, progesterone) generally affects cardiovascular system. Adverse for alkylating agents: Hemorrhagic cystitis 330 NCLEX-RN study guide 100 m Radiation External (Teletherapy) Internal (Brachytherapy) Sealed (regional) e.g. Cobalt Intracavitary radiation D D – Distance ▪ Maintain at least 6 feet from the radiation source ▪ Assign the client to a private room with a private bath ▪ Keep the door closed ▪ Ensure that caution signages are affixed to the door ▪ Instruct the client to remain on bedrest to prevent dislodgement of the implant Unsealed (systemic) ▪ Radioactive isotopes (IV) ▪ Radioactive iodine (PO) T S T – Time S – Shielding ▪ Limit staff time spent in the room to 30 minutes per shift. ▪ Cluster nursing care to minimize exposure ▪ Rotate staffing ▪ All staff must wear a dosimeter film badge when assigned ▪ No pregnant or under age 18 may be in the room ▪ All staff providing nursing care that requires physical contact must wear a lead apron. 331 100 m NCLEX-RN study guide Question: The nurse is providing medication instructions to a client with breast cancer who is receiving cisplatin. The nurse should tell the client to take which action? 1.Take the medication with food 2. Increase fluid intake to 2000 to 3000 mL daily 3. Decrease sodium intake while taking the medication 4. Increase potassium intake while taking the medication Answer: 2 Rationale: Hemorrhagic cystitis is an adverse effect that can occur with the use of cisplatin. The client needs to be instructed to drink copious amounts of fluid during the administration of this medication. Clients also should monitor urine output for hematuria. Remember that those that are not mentioned from the common examples above are classified as alkylating agents. 332 NCLEX-RN study guide 100 m 17 Immunology/Infectious disease Remember: acronym “Be DR. HIP” Age 2 and 4 months: Dr. HIP (DTaP, RV, Hib, IPV, PCV) Age 6 months: Be Dr. HIP (Hep B, DTaP, RV, Hib, IPV, PCV) 333 100 m NCLEX-RN study guide Active/Live vaccines: ▪ Varicella Zoster (VZV) ▪ Measles-mumps-rubella (MMR) ▪ Influenza nasal spray (out in the market 2017) Remember: Live vaccines ▪ Live vaccines cannot be given to immunocompromised and pregnant clients. ▪ The only vaccines given SQ Routes of administration: Oral: OPV, RV (Rota) IM: DTaP, Hep B, IPV, HiB, PCV, Hep A SQ: MMR, VZV (active vaccines) Contraindications: Encephalopathy: DTaP Antibiotic allergy “mycins”: IPV, MMR, VZV Gelatin allergy: MMR, VZV Egg, protein allergy: MMR, VZV Baker’s yeast: Hep B Common misperceptions: ▪ Penicillin allergy ▪ Mild illness (with or without an elevated temperature) ▪ Mild site reactions (e.g. swelling, erythema, soreness) ▪ Recent infection exposure ▪ Current course of antibiotics Key points: ▪ IPV - a new form of polio vaccine because OPV (Oral) had caused incidences of vaccine-associated paralytic poliomyelitis (VAPP). ▪ RV – not given with immunodeficiency or intussusception ▪ Newborns at risk for HIV infection need to receive all recommended immunizations at the regular schedule; live vaccines are not administered until HIV status is determined ▪ Infants with (+) Hep B mothers should receive Hep B vaccine and hepatitis B immunoglobulin (HBIG) within 12 hours of birth. Key points: ▪ Hep B Vaccines – can be given to MS, GBS, autoimmune, autoimmune diseases, and pregnant women except allergy to baker’s yeast. ▪ Cervical Cancer: Cervarix, Gardasil - 3 IM Injections (6 months period) before becoming sexually active ▪ In HIV (CD4 <200, <15%): Varicella, MMR cannot be given ▪ MMR & Varicella if not administered on the same day, must be separated by 28 days ▪ Hep B Vaccines should not be given if infant weighs <2000gms. ▪ Tdap (Tetanus toxoid, diphtheria and pertussis) is a booster vaccines for DTaP given at age 11 YO ▪ Hib vaccine is for H. influenza Type B bacteria to prevent bacterial croup in children (epiglottitis). Flu vaccine (flu shots) is for seasonal flu (NovemberMarch) caused by influenza virus (type A and B, given annually starting age 6 months and above including elderlies. Routinely recommended during pregnancy: ▪ Flu (influenza) shot during flu season. Avoid influenza nasal spray (active) ▪ Tdap - given between 27 and 36 weeks AOG. 334 100 m NCLEX-RN study guide Common disorders: Systemic Lupus Erythematosus (SLE) SLE: An autoimmune disorder in which the body's immune system produces autoantibodies that attack the body's tissues and cells. It is characterized by alternating periods of exacerbation (flare) and remission (latent). The skin is one of the target organs commonly affected by the disease. The characteristic cutaneous manifestation of SLE (> 50%) is a flat or raised red rash that forms a butterfly shape across the bridge of the nose and cheeks “butterfly rash”. It is often related to sunlight exposure (ultraviolet light) and is more pronounced during a disease flare. Mechanism: Genetic susceptibility plays the role in the development of the disease. If susceptible skin is exposed to sun (environment), apoptosis develops (programmed cell death) and releases chemicals as antigens. This leads to production of autoimmune cells (antibodies) that attack own tissues (autoimmune) Lab tests: Most specific: ▪ Anti-double stranded DNA (dsDNA) ▪ Anti-smith DNA Anti-nuclear antibodies (ANA) Anti-phospholipid Diagnostic criteria: SOAP DISH MD Any combination of 4 or more of 11 criteria, well-documented at any time during a patient's history. Treatment: ▪ Limit stress to prevent flare-ups ▪ Disease modifying drugs (immune suppressants: steroids) Remember: Disease modifying drugs are generally given to autoimmune diseases such as arthritis, SLE, Multiple sclerosis etc. The goal of treatment is prolong remission thereby limiting exacerbations. Autoimmune diseases are chronic diseases that are not curable. Malar rash: a rash shaped like a butterfly that is usually found of the bridge of the nose and the cheeks “butterfly rash” Discoid rash: a raised rash usually found on the head, arms, chest, or back. 335 NCLEX-RN study guide 100 m Common disorder: HIV-AIDS Remember: CD4 cell or T-helper cells orchestrates immune response. Acquired immunodeficiency syndrome (AIDS): A chronic, potentially life-threatening condition caused by the human immunodeficiency virus (HIV). By damaging your immune system (CD4), HIV interferes with your body's ability to fight the organisms that cause disease. Transmission: ▪ Sexual intercourse ▪ Contaminated blood transfusions ▪ Contaminated IV drug paraphernalia ▪ During pregnancy or delivery or through breast-feeding. Remember: Infected mothers may or may not pass the virus on to their babies. HIV-positive mothers who get treatment for the infection during pregnancy can significantly lower the risk to their babies. Phases of HIV-AIDS: 1. Primary infection (Acute HIV): flu-like illness within a month or two after the virus enters the body. 2. Clinical latent infection (Chronic HIV): Persistent swelling of lymph nodes occurs during this stage. Otherwise, there are no specific signs and symptoms. Generally lasts around 10 years if not receiving antiretrovirals. 3. Symptomatic HIV infection: Develops chronic signs and symptoms of infections 4. Progression to AIDS: Immune system has been severely damaged. More likely develop s opportunistic infections and cancers. >5 YO-adults: CD4 cells <200/mm3 1-5YO: CD4 cells <500/mm3 <1YO: CD4 cells <750/mm3 Normal CD4: 500-1500/mm3) Diagnosis: CDC recommendation 1. P24 antigen test (2-3 weeks result): Antigen test contrary to the conventional ELISA (antibody test) which takes longer (3 months). Longer results means higher chances of transmission if the patient is (+) 2. If P24 is (+) do Differential assay (+): Either HIV 1 or HIV 2 Western blot: Confirm HIV1 or HIV2 3. If Diff. assay is (-) do Nucleic acid test (NAT) (+): HIV 1 (-): No HIV and P24 is false positive For pregnant: ▪ Test is done for high risk mothers during first and last trimester ▪ Pregnant with (+) HIV can take retroviral to limit transmission to babies For newborns with (+) HIV mothers: ▪ First 48 hours: PCR test (antigen test) ▪ 1-2 months: NAT (96% specificity) ▪ 3-6 month: ELISA (antibody test) Infections common to HIV/AIDS: ▪ Tuberculosis (most common) ▪ Cytomegalovirus ▪ Candidiasis ▪ Cryptococcal meningitis ▪ Toxoplasmosis ▪ Cryptosporidiosis ▪ Kaposi's sarcoma ▪ Lymphoma 336 NCLEX-RN study guide 100 m Question: An HIV-positive patient who has been started on HAART is seen in the clinic for follow-up. Which test will be most helpful in determining the response to therapy? 1. CD4 level 2. Complete blood count 3. Total lymphocyte percent 4. Viral load Answer: 4 Rationale: Viral load testing measures the amount of HIV genetic material in the blood, so a decrease in viral load indicates that the highly active antiretroviral therapy (HAART) is effective. HAART: Acts by inhibiting the enzymes responsible for viral replication Nucleoside/nucleotide reverse-transcriptase inhibitors (NRTI): zidovudine, abacavir, lamivudine, emtricitabine, tenofovir Non-nucleoside reverse-transcriptase inhibitors (NNRTI): nevirapine, efavirenz, etravirine and rilpivirine Integrase inhibitors: elvitegravir, dolutegravir Protease inhibitors: lopinavir, indinavir, nelfinavir, amprenavir, ritonavir The CD4 level, total lymphocytes, and complete blood count will also be used to assess the impact of HIV on immune function but will not directly measure the effectiveness of antiretroviral therapy 337 NCLEX-RN study guide 100 m Common disorders: Tuberculosis Induration (After 48-72 hours) Population with positive results (Tuberculin testing) ≥ 5 mm Immunocompromised (HIV, Autoimmune diseases) Post organ transplant ≥ 10 mm Health care workers, homeless, drug users, endemic countries, <4 YO ≥ 15 mm Unknown risk Remember: Latent TB (asymptomatic TB) does not need to have airborne isolation. Active TB with symptoms are highly contagious and needs to be isolated accordingly. 338 100 m NCLEX-RN study guide Rifampicin Red orange secretions, hepatotoxic Isoniazid (+ VitB6) Peripheral Neuritis, hepatotoxic Pyrazinamide Increase Uric acid, hepatotoxic Ethambutol Optic neuritis Streptomycin Ototoxic, neurotoxic, nephrotoxic Remember: Isoniazid or Rifampin may be taken alone to prevent a latent TB infection from turning into active 339 NCLEX-RN study guide 100 m Common Infections: Diarrheal infection Giardiasis (Parasite) Salmonellosis (bacteria) Shigellosis/Dysentery (bacteria) Classic sign “Greasy Stool” “Blood in the stool” “Blood in the stool” DOC Metronidazole Penicillin, Quinolones Penicillin, Quinolones Macrolides Preventive standard vaccines: Rotateq, Rotarix Rotavirus “Stomach Flu” High fever, black tarry with pus in the stool Norovirus/Norwalk Virus “Winter vomiting disease” Low grade fever, Vomiting Supportive treatment Fluids - Priority Sexually transmitted Classic sign DOC Herpes Simplex (Virus) Painful Genital Vesicles (Lifelong Infection) Genital Warts (Virus) Syphilis/Chancre (Bacteria) Chancroid (Bacteria) Gonorrhea (Bacteria) Flesh colored, swollen Cauliflower Painful/itchy Painless Sore (Genital, Rectum, Mouth) Painful Sore From asymptomatic to symptomatic genital pus, painful sex, rectal, throat, eyes, joints inflammation Complication: Infertility Epididymitis (male) Pelvic inflammatory disease (female) Acyclovir (Zovirax) Vaccines (IM): Gardasil, Cervarix Penicillin, Doxycycline, Azithromycin Azithromycin Ceftriaxone Azithromycin Doxycycline 340 NCLEX-RN study guide 100 m Chlamydiasis/ “Tracho” (Bacteria) Same with gonorrhea Azithromycin Doxycycline Moniliasis/Candidiasis (Fungal) Cheese-like discharge odor free Cotrimoxazole – Topical Miconazole – Topical Itraconazole – Systemic Fluconazole - Systemic Trichomoniasis/”Trich” (Parasite) Foul smelling frothy discharge with Itchiness Metronidazole Animal associated Animal source Classic sign Histoplasmosis (Fungal) Birds, bats Flu like symptoms, extreme tiredness Rabies (Virus) Racoon, dog, rat bites Hypersalivation, photophobia, hydrophobia Toxoplasmosis (Protozoal) Cat litter Flu like symptoms, lymphadenopathy Viral encephalitis (West Nile virus) Mosquito bites Bulging fontanels in infants Lyme disease “Borreliosis” (Bacteria) Deer ticks Bull’s eye rash Infections prevented by standard vaccines Classic signs Standard vaccines Hepatitis B (Virus) Fatigue, low grade fever, jaundice, RUQ pain Hep B vaccine (HBV) Diphtheria (Bacteria) Tetanus (Bacteria) Skin: gray thick ulcers Respiratory: gray thick secretions surrounding throat, epiglottitis Severe muscle spasms: Opisthotonos: arching of neck and spine Trismus: lock jaw Risus sardonicus: 'sarcastic' grimace, drawing eyebrows DTaP, TDaP DTaP, TDaP 341 NCLEX-RN study guide 100 m Pertussis (Bacteria) “whooping cough” or violent cough Rota virus High fever, black tarry with pus in the stool Rota vaccine (RV) Hemophilus Influenzae Type B (HiB: bacteria) Epiglottitis: 4 Ds dysphonia (muffled voice), dysphagia (difficulty swallowing), drooling, and distressed respiration. HiB vaccine Poliomyelitis (Virus) Infantile paralysis Inactivated polio vaccine (IPV) Pneumococcal pneumonia (Bacteria) Purulent rusty sputum Pneumococcal conjugate vaccine (PCV) Measles (Rubeola virus) White Koplik’s spots: clustered, white lesions on the buccal mucosa Measle, Mumps, Rubella vaccine (MMR) Mumps (Virus) Painful swelling of parotid glands in the neck Measle, Mumps, Rubella vaccine (MMR) German measles (Rubella virus) Chicken pox (Varicella virus) Hepatitis A Seasonal Flu (influenza A, B viruses) Red Forcheimer spots: small, red spots (petechiae) on the soft palate Itchy skin rash with red blisters Remember: Most contagious 1-2 days before the rash appears until all blisters are dried & crusted. DTaP, TDaP Measle, Mumps, Rubella vaccine (MMR) Varicella zoster virus vaccine (VZV) Fatigue, low grade fever, jaundice, RUQ pain Hep A vaccine (HBV) Fever, malaise, chills Flu vaccine (flu shots) Trivalent: ▪ H1N1(swine flu): Type A ▪ H3N2: Type A ▪ Type B Quadrivalent: covers 2 type A and 2 type A influenza 342 NCLEX-RN study guide 100 m Common Antibiotic resistant infections Associated with Manifestation DOC Clostridium difficile Fluoroquinolones, Cephalosporins, Carbapenems, Clindamycin Severe diarrhea Vancomycin Metronidazole Vancomycin-resistant Enterococcus (VRE) Vancomycin Severe diarrhea Linezolid Penicillin, Cephalosporins Skin and respiratory infections, bacteremia Vancomycin Linezolid Methicillin-resistant Staphylococcus aureus (MRSA) Other infections Classic sign DOC Pediculosis (Parasite) Occipital itchiness Permethrin cream 10% Scabies (Parasite) Burrowing tract Permethrin cream 10% Infectious Mononucleosis “Kissing’s disease” (Epstein Virus) Lymphadenopathy, splenomegaly NSAIDs, Steroids Legionnaire’s Disease (Bacteria) Pneumonia symptoms (severe form) with high fever and relative bradycardia, dry cough Fluoroquinolones, Azithromycin, Doxycycline 5th Disease (Parvovirus B19) “Slapped cheek” red rashes Supportive treatment with NSAIDs Question: A parent brings her 4-month-old infant to a well-baby clinic for immunizations. The child is up to date with the immunization schedule. The nurse should prepare to administer which immunizations to this infant? 1. Varicella, hepatitis B vaccine (Hep B) 2. Diphtheria, tetanus, acellular pertussis (DTaP); measles, mumps, rubella (MMR); inactivated poliovirus vaccine(IPV) 3. MMR, Hemophilus influenzae type b (Hib), DTaP 4. DTaP, Hib, IPV, pneumococcal vaccine (PCV), rotavirus (RV) Answer: 4 Rationale: (Refer to standard vaccine schedule). Active vaccines [Varicella Zoster (VZV), Measles-mumps-rubella (MMR) ] are given at 12 months due to low immune system at younger age. 343 NCLEX-RN study guide 100 m 18 Maternal & child Antepartum: Signs of pregnancy Presumptive signs “subjective” (as verbalized by client) Breast tenderness Urine frequency Nausea/vomiting Fatigue Amenorrhea Quickening (fetal movement) Probable signs “objective” (as assessed by nurse) (+) HCG (+)Pregnancy test (PT) Hegar’s sign: softening uterus Chadwick’s sign: Bluish discoloration of vagina Goodell’s sign: softening of cervix Braxton Hicks: false contractions Ballottement: fetal bouncing after pushing uterus Fetal outline: Leopold’s maneuver Positive signs “confirmatory” (+) Fetal heart tone (FHT) 4-8 weeks: vaginal USD 12 weeks: doppler USD 16 weeks: Stethoscope Remember: Presumptive signs are verbalized by clients to which they “feel they are pregnant. Probable signs are assessed by nurse, however there is no fetal heart rate. Fetal heart rate is a confirmatory sign. In addition, probable signs are “signs with medical names implicated”. Normal values: Amniotic fluid: 500—1000 ml > 1500 ml: Polyhydramnios < 500 ml: Oligohydramnios 344 NCLEX-RN study guide 100 m Additional calorie intake: Pregnancy: 300 kcal/day Lactating: 500 kcal/day Weight gain: First trimester: 1 lb/month 2nd Trimester: 1 lb/week 3rd Trimester: 1 lb/week Protein Intake: 65 g/dl (Pre-pregnant) 45 – 50 g/dl (Female) 65 – 70 g/dl (Male) RSA: right sacrum anterior ROP: right occiput posterior ROA: right occiput anterior LSA: left sacrum anterior LOP: left occiput posterior LOA: left occiput anterior Remember: Folic acid intake on planning to get pregnant Must consume 400-800 mcg of folic acid daily. Inadequate maternal intake of folic acid during the critical first 8 weeks after conception (often before a woman knows she is pregnant) increases the risk of fetal neural tube defects (NTDs), which inhibit proper development of the brain and spinal cord. Common NTDs are spina bifida and anencephaly (lack of cerebral hemispheres and overlying skull). 345 NCLEX-RN study guide 100 m Approximate fundal height Gestational age Fundal height 12 weeks Symphysis pubis 20 weeks Umbilicus 36 weeks Xiphoid process 37-40 weeks Regression of fundal height between 36-32 cm Postpartum: ≤ 24 hours Umbilicus Antepartum: Expected day of confinement (EDC) EDC Get first day of a woman's LMP (M/D/Y) - 3 (M) +7 (D) + 1 (Y) e.g. LMP 09 – 7 – 19 09 7 19 - 3 +7 + 1 = 06 14 20 (June 14, 2020) 346 NCLEX-RN study guide 100 m Antepartum: Aortocaval syndrome (supine hypotensive syndrome) Remember: Best position during pregnancy is LATERAL POSITION Supine hypotensive syndrome occurs when the weight of the abdominal contents compresses the vena cava causing decreased venous return to the heart. This results in low cardiac output (maternal hypotension) and reflex tachycardia as a compensatory mechanism. This leads to dizziness, pallor, and cold and clammy skin, similar to symptoms oh hypovolemic shock. The client should be immediately repositioned laterally (right or left side) until the symptoms subside. Utilizing a wedge pillow prevents this condition. Antepartum: Biophysical profile testing Biophysical profile: A combination of USD and nonstress test done during 26-28 weeks gestation. A score of 8 requires further evaluation such as contraction stress test/stress test 32 weeks near delivery. Indication: High risk pregnancy ▪ Multiple pregnancy ▪ Hypertension, DM, CV diseases ▪ Previous pregnancy complication ▪ RH incompatibility ▪ Obesity ▪ Pregnancy ≥ 35 YO Criteria: Highest score 10 points 1. Fetal heart rate 20 mins: ≥ 2 Acceleration (2 points) 40 mins: No acceleration (0 points) 2. Fetal breathing 30 secs: (+) rhythm (2 points) (-) rhythm (0 points) 3. Fetal body movement 30 mins: ≥ 3 movements (2 points) No movements (0 points) 4. Fetal leg movement (+) extension from flexed position (2 points) No extension (0 points) 5. Amniotic fluid (+) pocket of fluid (2 points) (-) pocket of fluid (0 points) 347 NCLEX-RN study guide 100 m Non stress test vs Stress test/Contraction stress test (CST) Non stress test Remember that in NST, you are looking for acceleration (fetal heart activity). ▪ Done 26-28 weeks (biophysical profile) ▪ A positive result (+) is normal ▪ A negative (-) result is abnormal ST/CST Remember that in ST/CST, you are looking for deceleration “late deceleration” This time, the mother is given oxytocin to see how the fetus’ heart responds to stress when uterus contracts ▪ Done 32 weeks near delivery ▪ A positive result (+) is abnormal ▪ A negative (-) result is normal Both are prenatal test for high risk pregnancies by monitoring fetal heart activity and fetal well-being in general. Fetal Heart Monitoring: VEAL CHOP Variable deceleration Early deceleration Acceleration Late deceleration Cord compression Head compression Okay! Poor placental perfusion Variable Deceleration Cord compression Variable deceleration means, at any time during uterine contraction by mother the fetus decelerates (fetal heart rate decreases/downward deflection) due to cord compression. Top rhythm represents the fetal activity while bottom is maternal contraction 348 100 m NCLEX-RN study guide Early Deceleration Head compression Early deceleration: At each uterine contraction by mother, the fetus decelerates (fetal heart rate decreases/downward deflection) due to head compression. This reflects a “mirror image” on the monitor. Acceleration OK-normal/reassuring Acceleration: Fetal heart activity showing upward deflection specially during maternal contraction. This activity is reassuring and indicates fetal well-being anticipating a stressful event during labor and delivery. 349 NCLEX-RN study guide 100 m Late Deceleration Poor placental perfusion Late deceleration: Fetal heart activity showing wherein fetus decelerates (fetal heart rate decreases/downward deflection) after each uterine contractions. This indicates that fetus responds poorly to stressful events. This can be caused by poor placental perfusion. Common conditions: Hyperemesis gravidarum, ectopic pregnancy Hyperemesis gravidarum Overview A disorder that causes severe nausea and vomiting that leads to fluid and electrolyte imbalances, nutritional deficiencies, ketonuria, and weight loss up to 5 kg body weight. Usually occurs at 8-12 weeks AOG. Etiology Genetics, hormonal response to human chorionic gonadotropin (HCG), Estrogen decreases intestinal motility and gastric emptying leading to nausea/vomiting Ectopic pregnancy Occurs when a fertilized egg implants and begins to grow outside the uterine cavity, most often in the fallopian tubes. A growing fetus causes rupture to fallopian and is a life threatening to the mother. ▪ Age 35 – 40 YO ▪ Pelvic inflammatory disease (PID) ▪ Smoking ▪ Previous ectopic pregnancy 350 NCLEX-RN study guide 100 m Classic S/S ▪ Dehydration (dry mucous membranes, poor skin turgor, decreased urine output, tachycardia, and low blood pressure ▪ Headache ▪ Hallucination ▪ Weight loss ▪ Ketonuria (breaking down fats d/t starvation state) ▪ Electrolyte imbalance (hypokalemia) ▪ Metabolic alkalosis Complications ▪ Low birth weight ▪ Kidney failure Diagnostics ▪ Electrolyte levels ▪ HCG ▪ Hemoglobin/hematocrit Treatment ▪ Sudden-onset abdominal pain Referred: Shoulder pain d/t irritation of the diaphragm from intraabdominal bleeding. ▪ Cullen’s sign (periumbilical bruising) ▪ Hypovolemic shock: Hypotension, Tachycardia, Tachypnea Hypovolemic shock DOC: Ondansetron (antiemetic) Rehydration Diet: Small frequent feeding, High protein, low odor food ▪ Pregnancy test (+) HCG ▪ Physical exam ▪ CBC, BUN, Creatinine DOC: Methotrexate (anticancer) – to stop proliferation of cells preventing rupture Treat shock: Fluid management Surgery (if ruptured) Types of abortion: Type according to degree of severity Threatened Reversible Inevitable Possible or inevitable loss Missed Fetal loss and retained for a period of time Incomplete Partially retained products Complete All products of pregnancy removed 351 NCLEX-RN study guide 100 m Type according to cause of abortion Spontaneous Recurrent Non-induced or natural passage of products of conception before 20 weeks AOG. A form of infertility characterized by 3 consecutive spontaneous abortions Induced Use of medicine to end an undesired pregnancy. Criminal termination of pregnancy illegally, usually undertaken when legal induced abortion is unavailable Common conditions: Pregnancy induced hypertension (PIH) Pregnancy induced hypertension (PIH): Is a condition characterized by high blood pressure during pregnancy beyond 20th week AOG. Gestational Hypertension can lead to a serious condition called Preeclampsia (Triad: HTN, Proteinuria that leads to edema and weight gain). If left untreated it will lead to organ damage and eclampsia (Triad + Seizure). Remember: The term eclampsia means “shining forth” which implicates a common aura for patients with occurring seizure. 2oth week AOG Preexisting HTN PIH Remember: Hypertension prior to 20th week gestation is a preexisting HTN not related to pregnancy. Pregnancy induced hypertension (PIH) is beyond 20th week. 352 100 m NCLEX-RN study guide Mechanism: The exact cause of PIH-Preeclampsia-Eclampsia mechanism is unknown. However, certain facts are developed to support its pathophysiology. Genetically, the abnormal development of placenta causing fibrosis to spiral arteries which supplies nutrients and O2 to uterus and placenta contributes to the disease process. This leads to inadequate blood supply leading to release of placental factors that causes systemic damage to endothelium as it travels to maternal circulation. Remember, once the body tissues are deprived of O2, it tends to create dysregulation by releasing certain chemicals. In placenta, these placental factors promote harmful effects not only within tissues but systemically. Clinical presentation: Preeclampsia TRIAD HTN (>140/90 mmhg): d/t vasoconstriction by placental factors and retained fluids by inadequately perfused kidneys. Proteinuria: d/t damage glomerulus in kidneys. Edema: d/t loss of protein from proteinuria Organ damage: Eclampsia Seizure: d/t decrease blood supply to brain characterized by headache and visual disturbances as an “aura” prior to seizure. Pulmonary edema: d/t low protein (albumin) HELLP syndrome: Liver malfunction characterized by epigastric pain or RUQ pain (cardinal sign), N/V, and eventually hematomas and bleeding 353 NCLEX-RN study guide 100 m HELLP syndrome: A potentially life-threatening disorder that is usually associated with preeclampsia. HELLP syndrome is a disorder of the liver and blood that can be fatal if left untreated. The symptoms of HELLP syndrome are wide-ranging and vague, and can often be difficult to initially diagnose. The name HELLP syndrome has three major abnormalities seen on the initial lab analysis. These include: Hemolysis, elevated liver enzymes and low platelet count Treatment: ▪ Delivery of fetus (depends on the severity and AOG) ▪ Seizure management DOC: Magnesium sulfate ▪ BP management DOC: Hydralazine, Labetalol Diagnosis: ▪ Physical examination ▪ Blood tests: CBC, Liver profile, BUN, creatinine ▪ Urinalysis: Urine protein ▪ CXR: pulmonary edema ▪ Biophysical profile ▪ Fetal USD Common conditions: Abruptio placenta vs Placenta previa Overview Abruptio placenta Placenta previa Premature and abrupt separation (full or partial) of the placenta from the uterine wall resulting in hemorrhage. Its main mechanism is the degeneration of the arteries supplying the placenta leading to rupture and separation. Primarily, the word “previa” means first. In this condition you see the placenta first lying on the cervical os. The implantation is normally on the upper part of uterus d/t high vascularization. However, d/t previous trauma to uterus, the placenta is not able implant on 354 NCLEX-RN study guide 100 m a normal location. Types: Complete: fully covering the cervical os Partial: Partially covers the cervical os Marginal: 2 cm near the cervical os Etiology Classic S/S HTN Chronic smoking Trauma Drug abuse (Methamphetamines, cocaine) d/t significant vasoconstriction ▪ Multiparity ▪ Age >35 YO ▪ ▪ ▪ ▪ ▪ ▪ Painful rigid abdomen: d/t uterine spasms ▪ Usually concealed bleeding ▪ Hypovolemia (hypotension, tachycardia, tachypnea) ▪ Painless soft boggy abdomen: because the bleeding is not concealed which does not cause contractions and spasm ▪ Bleeding: d/t cervical thinning (effacement) in preparation for delivery ▪ Hypovolemia (hypotension, tachycardia, tachypnea) ▪ ▪ ▪ ▪ Maternal: ▪ Hypovolemic shock d/t bleeding ▪ Acute kidney injury (d/t hypovolemia) Complications ▪ DIC Fetal: ▪ Intra uterine hypoxia (late decelerations) ▪ Premature birth Diagnostics ▪ USD ▪ Blood stained amniotic fluid Previous CS Abortion Smoking Multiparity Age >35 YO Maternal: ▪ Hypovolemic shock d/t bleeding Fetal: ▪ Intra uterine hypoxia (late decelerations) ▪ Premature birth ▪ Prenatal USD 355 NCLEX-RN study guide 100 m Treatment ▪ IV fluids to support fluid volume ▪ Blood products (prevent DIC) ▪ Emergency CS (if severe) ▪ Major bleeding: Blood products IV fluids ▪ Corticosteroids: enhance lung maturity ▪ Emergency CS (if severe) Remember: No internal examination (IE) indicated Placenta previa Marginal/low lying placenta previa Partial placenta previa Complete placenta previa Abruptio placenta 356 NCLEX-RN study guide 100 m Labor and delivery: Stages of Labor 1. Cervical Dilatation (Dilatation – Duration – Interval) Latent: 0 - 3 cm; 20 - 40 secs; 5 - 10 mins Active: 4 - 7 cm; 40 - 60 secs; 3 - 5 mins Transitional: 8 -10 cm; 60 - 90 secs; 1-3 mins Number of hours: Primipara: 10 - 14 hours Multipara: 6 – 8 hours Remember: No opioids 1-4 hours prior to giving birth Do not administer opioids 1-4 hours prior to giving birth to avoid neonatal abstinence syndrome (NAS). Initially, it causes CNS depression that may lead to respiratory distress similar to opioid intoxication if left untreated. NAS follows after the opioid effects has already subsided causing withdrawal effects to NB such as agitation, increases reflexes and seizure. In addition, do not encourage mother to bear down not until fully dilated at 10 cm to avoid laceration. Providing emotional support is the priority concern when fully dilated as it is the most emotionally challenging phase of labor. 2. Expulsion of baby Hallmark: Crowning RBOW: Primipara: 10 cm Multipara: 7 - 8 cm Acronym: “Every darn fool in Egypt eats raw eggs” 357 100 m NCLEX-RN study guide 3. Placental Separation Signs: Calkin’s sign (Globular shape of abdomen) Sudden gush of blood Lengthening of cord 358 NCLEX-RN study guide 100 m Schultz Mechanism – shiny inverted umbrella (fetal side) Duncan Mechanism – Raw red umbrella (maternal side) 4. Immediate post-partum (1 – 4 hours) Lochia – Psychological Task Rubra: 1-3 days - Taking In - physiologic need Serosa: 4-10 days Taking Hold – accepting status Alba: 11-20 days Letting Go - adapted to roles Remember: Post-partum blues vs. post-partum depression Post-partum blues normally resolves within this period of psychological tasks. If the mother does not overcome this needs and exceeds beyond, it can lead to depression and psychosis. High risk mothers include history of depression, abuse, smoking or alcohol use, anxiety, poor marital relationship. Newborn safety is a priority because mothers may not adapt to roles. It can also lead to possible suicide and homicide. Labor and delivery: Umbilical cord prolapse Knee chest position uses gravity to shift fetus out of the pelvis. Patient’s thighs must be at the right angles and chest flat on bed A gloved hand in the vagina pushes the fetus upward and off the cord The patient’s hips are elevated with 2 pillows; this is often combined with the Trendelenburg (head down) position. Umbilical cord prolapse: Occurs when the umbilical cord slips under the presenting part of fetus. This causes cord compression and eventually fetal hypoxia. The prolapsed cord may be palpated during a vaginal examination or visualized protruding from the vagina. Emergency CS may be required if it causes severe fetal hypoxia. 359 NCLEX-RN study guide 100 m Question: A nurse is evaluating the external fetal monitoring strip of a laboring primigravida at 36 weeks gestation. Which nursing interventions should the nurse implement? (Select all that apply) 1. Administer supplemental oxygen by mask 2. Increase the intravenous (IV) fluid rate 3. Prepare the client for an amnioinfusion 4. Reposition the client to the supine position 5. Stop the client's oxytocin infusion Answer: 1, 2, 5 Rationale: Late decelerations are caused by uteroplacental insufficiency. The client should be given O2 via facemask, repositioned to the right or left side, stop ongoing oxytocin if administered, and provide NS bolus. The nurse will need to prepare for delivery if the deceleration persists. Amnioinfusion is a transvaginal infusion of fluid for oligohydramnios. Maternal hypotension: Acronym: STOP Stop infusion of Pitocin. Turn the client on her left side. Administer Oxygen. If hypovolemia is present, Push IV fluids 360 NCLEX-RN study guide 100 m Post-partum: Hemorrhage Contraction of uterine muscles. Compression of vessels prevents bleeding Uterine atony: Lack of uterine contraction Post-partum hemorrhage (PPH): Defined as the significant blood loss of more than 500 ml (vaginal delivery or 1,000 ml (CS delivery) within the first 24 hours following childbirth. Causes include 4 Ts (Tone, trauma, tissue and thrombin). In addition saturating a peri pad in 1-2 hours could indicate hemorrhage. This can be assessed by a boggy fundus. The nurse should also assess the client's vital signs for signs of shock. Tone: Uterine atony Causes: ▪ Repeated distention (multipara, multifetal) ▪ Muscle fatigue from delivery ▪ Distended bladder ▪ Anesthesia Treatment: ▪ Fundal massage to promote contraction ▪ Promote urination ▪ Catheterization Tissue: Retained placental fragments Causes: ▪ Placenta accrete (deep attachment of placenta to uterus). This also promotes uterine atony Treatment: ▪ Removal of retained fragments Trauma: Damage to genital structures (vagina, perineum, uterus, cervix) Causes: ▪ Incision from delivery ▪ NB coming from vaginal canal ▪ Medical instrument (forceps, vacuum) Treatment: ▪ Repair of trauma site Thrombin: Abnormal clotting condition Causes: ▪ DIC caused by abruptio placenta ▪ Preexisting coagulation disorders (thrombocytopenia) Treatment: ▪ Treat the specific underlying cause 361 NCLEX-RN study guide 100 m Post-partum: Breastfeeding ▪ ▪ ▪ ▪ Good latch Baby’s mouth is widely open, like a yawn Tongue is over his lower gum Lips are curled out like a fish Chin firmly touches breast ▪ ▪ ▪ ▪ Poor latch Baby’s mouth is barely open Tongue behind the lower gum Lips are curled in Chin barely touches breast Remember: Proper breastfeeding technique promotes adequate intake and emotional bonding. Normally NB will feed at least 8-12 times a day. at approximately 15-20 minutes each breast. Remember that at approximately every 2 hours they require attention (feeding and diaper change). This is also an important indication of the infant’s hydration status considering intake and output. Breastfeeding principles: ▪ The client should hold the infant "tummy to tummy," with the mouth positioned in front of the nipple. The head should be facing forward keeping the body in alignment. ▪ The infant needs to grasp both the nipple and part of the areola to ensure proper latching otherwise it will cause pain. ▪ Insert a finger to break the suction prior to moving the infant away after feeding or in cases on incorrect latching. This prevents trauma to nipples that may cause mastitis. 362 NCLEX-RN study guide 100 m Newborn: APGAR score APGAR score: Assessed during first (1st) and fifth (5th) minutes of life. Score of 7-10 is normal and reassuring, 4-6 is guarded and needs further monitoring (repeated every 5 mins until the 20th minute of life), 0-3 is critically low and may need resuscitation. Newborn: Reflexes Reflexes Rooting Sucking Palmar grasp Description When stroked baby will turn his or her head and open his or her mouth & follow When the roof of the baby's mouth is touched, the baby will start to suck Stroking the palm of a baby's hand causes the baby to close his or her fingers in a grasp Disappears 3-4 months 10-12 months 3-4 moths Plantar grasp Similar to the palmar reflex in that stroking or pressing on the ball of the foot causes the foot and toes to flex, or curl, so as to grasp whatever caused the stimulus. 8-10 months Tonic neck When a baby's head is turned to one side, the arm on that side stretches out and the opposite arm bends up at the elbow. This is often called the fencing position 4-6 months 363 NCLEX-RN study guide 100 m Moro (Startle) Babinski Stepping The baby throws back his or her head, extends out his or her arms and legs, cries when startled Occurs after the sole of the foot has been firmly stroked. The big toe then moves upward or toward the top surface of the foot. The other toes fan out. Also called the walking or dance reflex because a baby appears to take steps or dance when held upright with his or her feet touching a solid surface 3 months 2 years 2 months Newborn: Sudden infant death syndrome (SIDS) Risk factors ▪ ▪ ▪ ▪ ▪ ▪ ▪ Prone or side lying while sleeping Exposure to tobacco Infant sleeping with adults Low birth weight (prematurity) Overheating during sleep Soft mattresses Loose linens, beddings bumper pads to cribs Prevention ▪ ▪ ▪ ▪ ▪ ▪ ▪ Supine position Breastfeeding Up to date vaccinations Pacifier use during sleep (focuses infants attention to sucking) Sleep sack Firm mattress No loose items or toys Sudden infant death syndrome (SIDS): Unexplained death, usually during sleep, of a seemingly healthy baby less than a year old. Although the cause is unknown, it appears that SIDS might be associated with defects in the portion of an infant's brain that controls breathing and arousal from sleep. 364 NCLEX-RN study guide 100 m Newborn: Jaundice (physiologic vs. pathologic) Physiologic Pathologic Not present until 72 hours after birth Present in the first 24 hours of life Bilirubin rises <5 mg/dl/day Bilirubin rises >5mg/dl/hour Bilirubin peaks at <14-15 mg/dl Bilirubin peaks up to >15 mg/dl Direct bilirubin <10% of total Direct bilirubin >10% of total Resolves by 1 week (term infants) Resolves by 2 weeks (preterm infants) Persists beyond 1 week (term infants) Persists beyond 2 weeks (preterm infants) Cause: normal heme breakdown Cause: Various conditions (e.g. Erythroblastosis fetalis or Hemolytic disease of the NB) Bilirubin levels: Remember that high levels of bilirubin can cause brain damage (kernicterus) Normal: < 1.5 mg/dl, Jaundice: ≥ 5 mg/dl, Hyperbilirubinemia: ≥ 30 mg/dl Phototherapy: Phototherapy: Is the use of intense fluorescent lights to reduce serum bilirubin levels in the NB. Adverse effects from treatment, such as eye damage, dehydration, or sensory deprivation, can occur Nursing care: ▪ Monitor skin temperature closely ▪ Reposition the newborn every 2 hours. ▪ Cover the newborn’s eyes with eye shields or patch ▪ Increase fluids to compensate for water loss ▪ The fluorescent light turned off every 4 to 8 hours and is monitored for bronze baby syndrome, a grayish brown discoloration of the skin. 365 NCLEX-RN study guide 100 m Newborn: Erythroblastosis fetalis (Hemolytic disease of the NB) 1 2 3 4 5 1. RH (+) father and RH (-) mother yields an RH (+) baby. An RH is an antigen in the surface of the RBC 2. RH antigen is acquired by fetus from the father (RH+). At this time, there is no antigen-antibody reaction from the mother and fetus because there is non-mixing of blood between mother and fetus by way of placental barrier. 3. After birth, fetal erythrocytes with RH antigen (RH+) leaks into maternal blood due to breakage of the chorion (placental barrier). 4. The maternal B-cells develop antibodies against RH antigen and potentially react to future pregnancies. 5. During subsequent pregnancy with acquired RH antigen (RH+) from the father, the maternal antibodies that are developed by the mother attack the RH antigen (RH+) of the fetus causing antigen-antibody reaction. This leads to hemolytic reaction. 366 NCLEX-RN study guide 100 m S/S: Hemolytic anemia: The 4Fs Fatigue Forgetfulness Fainting Fast heartbeat (tachycardia) Jaundice Kernicterus: neurotoxicity Prevention: Rhogam Given 26-28 weeks during pregnancy or within 24-72 hours after delivery if determined that the baby is RH (+). Rhogam is an antibody given before the mother is able to produce its own by simply halting the B-cells “signaling not to produce anymore”. This antibodies does not cause immune response. Coombs test: Test for antibodies Direct: Test that directly detects antibodies in the surface of RBC. It can diagnose HDN. If positive it means that these antibodies may cause Ag-Ab reaction (hemolysis) Indirect: Detects antibodies from the serum (plasma). Used to determine if there are chances of developing Ag-Ab reaction. It is an important tool in diagnosing hemolytic diseases (e.g. HDN) or in general, a possible BT reactions of any conditions. Placental barrier: The placenta is composed of several layers of cells acting as a barrier for the diffusion of substances between the maternal and fetal circulatory systems. However, the placental barrier between mother and fetus is the “leakiest” barrier and is a very poor block to chemicals. Remember: TORCH Infectious agents that may cross placental barrier during first trimester leading to congenital abnormalities T: Toxoplasmosis, O: Others (syphilis, varicella-zoster, parvovirus B19) R: Rubella (German measles) C: Cytomegalovirus H: Herpes simplex 367 NCLEX-RN study guide 100 m Blood compatibilities: ABO and RH ABO blood system: Is used to symbolize the presence of one, both, or neither of the A and B antigens on the surface of RBCs. The body also tends to produce antibodies against a certain antigen considered as foreign that may cause reaction. For instance, type A (with antigen A) has developed antibodies against type B that whenever transfused a foreign blood type B, it will cause Ag-Ab reaction resulting into hemolysis. On the other hand, a type AB blood can receive either A, B, O (no antigen) because it does not have neither antibodies against A or B. Remember: Do not interchange RH from ABO system. RH blood system is normally described with a positive or negative suffix after the ABO type. For instance, if you have a blood type A(+) it means you have both antigens A and RH (aka antigen D) in the surface of RBCs. A(-) has antigen A but with no RH antigens on its surface. RH (+) blood does not develop antibodies against RH (+) itself, RH (-) does. If RH (-) is exposed to RH (+) blood, the antibodies cause immune reaction. 368 100 m NCLEX-RN study guide Remember: ABO and RH combined AB (+): Universal recipient since type AB does not contain antibodies against A or B and RH (+) also does not have antibodies against any antigen. O (-): Universal donor since the recipient blood with RH (+) does not contain antibodies and RH (-) recipients only contains antibodies against RH (+). Type O blood from a donor does not have A or B antigen, it means there is nothing for a recipient with a type A, B blood to react with. Type AB does not have antibodies. 369 NCLEX-RN study guide 100 m Growth & development 19 Theories: Psychosexual development (Freud) Stage Age Sexual focus Key task Fixation Oral Birth-1 YO Mouth Weaning Anal 2-3 YO Anus Toilet training Obsession on cleanliness, sexual anxiety Identifying gender role Genitals models (masturbation) Oedipus: boys Electra: girls Difficulty in intimate relationship, inadequacy, inferiority Obsessive eating, smoking, drinking (alcoholism Phallic 4-5 YO Latency 6-12 YO None Social interaction Genital Puberty & later Genitals (sexual intimacy) Intimate relationship/ Productivity No fixation Return to previous fixation (low sexual interest or if no previous fixation, may have sexual motivation Cognitive development (Piaget) Stage Age Sensorimotor Birth – 2 YO Pre-operational “mental operations” 2-7 YO Concrete operational 7-11 YO Important features ▪ Object permanence: Differentiates self from objects e.g. “If you remove the toy or object, they will think that it does not exist anymore” ▪ Egocentric: self centered ▪ Understands symbols ▪ Classifies objects by it single feature: groups all together red blocks regardless of shape ▪ Conservation: e.g. the same amount of fluid is what it is even if you transfer it to a different containers. ▪ Classifies objects according to several features 370 NCLEX-RN study guide 100 m 12 and up Formal operation ▪ Abstract: believes that there is always a consequence of actions ▪ Moral reasoning: believes in what is right and what is wrong Moral development (Kohlberg) Level and age Stage Preconventional (Pre-moral) Up to age 9 YO Conventional (Most adolescents and adults) What determines right and wrong? “Obey or punished” Defined by what they get punished for. If you get told off for stealing then that is wrong “Individuals have different viewpoints” Determined by what we are rewarded or by doing what others want Good boy, good girl Being good is what pleases others. Right and wrong is determined by the majority Law and order Being good is doing your duty to society. Showing respect to society Social contract Determined by personal values: “Rules in society is not absolute, people have rights” Universal ethical principle In accordance with deeply held moral principles: “human rights is more important than the law even if you are persecuted” (e.g. Martin Luther King, Nelson Mandela principles) Post conventional (0-15 % of over 20 YO) Psychosocial/Personality development (Erikson) Age Infancy (0-1 YO) Toddlerhood (1-3 YO) Preschool (4-6 YO) Significant Virtues Crisis Hope Trust vs mistrust Mother Can I trust the world? Feeding, abandonment Will Autonomy vs shame and doubt Parents Is it OK to be me? Toilet training, clothing their own selves Purpose Initiative vs guilt Family Is it OK for me to move? Exploring tools, making arts relationship Question Crucial events 371 NCLEX-RN study guide 100 m Can I make it in the world of people and things? School activities, sports Who am I? Who I can be? Social relationships Compe tence Industry vs inferiority Neighbors, school teachers Adolescence (12-19 YO) Fidelity Identity vs role confusion Peers, role models Early adulthood (20-35 YO) Love Intimacy vs isolation Friends and partners Can I love? Romantic relationships Adulthood (35-65 YO) Care Generativity vs stagnation Household, workmates Can I make my life count? Work, parenthood Wisdom Ego integrity vs despair Mankind, my kind Is it OK to have been me? Reflection on life School age (6-12 YO) Late adulthood (65 and up) Developmental milestones: Infants - toddlers Age (Months) 1 2-3 Gross motor Attempts to hold head up when prone Gains head control when held 4-5 ▪ Rolls from frontback then back-front ▪ Sits with support 6-9 ▪ Sits without help ▪ Begins to crawl ▪ May pull to stand 10-12 ▪ May walk with help or independent steps ▪ Crawls up stairs Language Social/cognitiv e Maintains fisted hand Cries when upset Gazes at parents when they speak Holds rattle when placed in hand Makes cooing sounds Smiles in response to talking and smiling ▪ Begins to laugh ▪ Makes some consonant sounds Calms by parent’s voice Fine motor ▪ Holds object with palmar grasp ▪ Puts things in mouth ▪ Moves objects between hands ▪ Uses crude pincer grasp (using pads of index finger) ▪ Uses 2 finger pincer grasp ▪ Hits 2 object together ▪ Babbles and imitates sounds ▪ May say “Mama” ▪ Says 3-5 words ▪ Non-verbal gesture like waving goodbye ▪ Recognizes familiar faces ▪ May have stranger anxiety ▪ May have stranger anxiety ▪ Searches for hidden objects 372 NCLEX-RN study guide 100 m 18 ▪ Walks up/down stairs with help independently ▪ Throws ball overhand ▪ Jumps in place ▪ Builds 3-4 blocks tower ▪ Turns 2-3 book pages ▪ Scribbles ▪ Uses cup and spoon ▪ Says 10+ words ▪ Identifies common objects ▪ Has temper tantrums ▪ Understands ownership “mine” ▪ Imitates others 2 YO ▪ Walks up/down stairs alone, 1 step at a time ▪ Runs without falling ▪ Kicks ball ▪ Builds 6-7 block tower ▪ Turns 1 book page ▪ Draws a line ▪ 300+ words ▪ 2-3 word phrases ▪ States own name ▪ Begins parallel play ▪ Begins to gain independence from parents 3 YO ▪ Walks up stairs with alternating feet ▪ Pedals a tricycle ▪ Jumps forward ▪ Draws a circle ▪ Feeds self without help ▪ Grips a crayon with fingers instead of fist ▪ 3-4 sentences ▪ Ask “why” questions ▪ States own age ▪ Begins group play ▪ Toilet trained except wiping Others: Readiness in toilet training: ▪ Ambulates to and sit on the toilet ▪ Remain dry for several hours or through a nap ▪ Pull clothes up and down ▪ Understand a two-step command ▪ Express the need to use the toilet (urge to defecate or urinate) ▪ Imitate the toilet habits of adults or older siblings ▪ Express an interest in toilet training Remember: There is no magic age for toilet training. Developmental milestones rather than the child's age signal a child's readiness for toilet training 373 NCLEX-RN study guide 100 m Age Birth to 2 YO 3-5 YO 6-9 YO 10-12 YO Adolescent Belief on death ▪ Does not understand death ▪ Sensitive to loss and separation ▪ Death is reversible ▪ Thoughts may include magical thinking and fantasy ▪ Concrete finality of death ▪ Difficult in perceiving their own death ▪ May be preoccupied with the medical or physical aspects of dying ▪ Understands that death affects everyone ▪ Thinks about how death may affect them personally ▪ View death on an adult level and understands that their own death is inevitable but is a difficult concept to perceive ▪ Incorporates spiritual and religious aspects of death Separation anxiety: Also known as anaclitic depression, affects children age 6-30 months and peaks at 10-18 months. May last until 3 years. Stages: Protest – Characterized by refusing from others so the parent returns by crying Despair – Withdraw, quiet, displays younger behavior Detachment – Suddenly appears friendly and builds relationships Nursing care: ▪ Encouraging the parents to leave favorite toys, books, and pictures from home ▪ Establishing a daily schedule that is similar to the child's home routine ▪ Maintaining a close, calming presence when the child is visibly upset ▪ Facilitating phone or video calls when parents are available ▪ Providing opportunities for the child to play and participate in activities 374 100 m NCLEX-RN study guide Question: The parents of a hospitalized 3-month-old have to leave the infant while they work. One parent fears that the baby will cry as soon as they walk out. The nurse teaches both parents about separation anxiety. Which statement by the parent indicates that the teaching has been effective? 1. "At this age, my baby will not cry because we are leaving." 2. "I know my baby will feel abandoned when we leave." 3. "My baby is too young to sense my anxiety about leaving." 4. "My baby understands that we will return later in the day." Answer: 1 Rationale: A 3-month-old can be soothed by any comforting voice and does not develop separation anxiety at this time. This behavior starts around age 6 months, peaks at age 10-18 months, and can last even until age 3 years. It produces more stress than any other factor for children in this age group. However, this reaction is normal and resolves as the child approaches age 3 years. 375 NCLEX-RN study guide 100 m 20 Therapeutic communication: Behavioral 376 100 m Non therapeutic communication: NCLEX-RN study guide 377 100 m Defense mechanism: NCLEX-RN study guide 378 NCLEX-RN study guide 100 m Eating disorders: Bulimia nervosa vs Anorexia nervosa Anorexia nervosa vs Purging without eating Overview Purging after binge eating Weight loss of up to < 75% ideal body weight since patient is not eating General Appearance Normal appearance, may or may not have weight loss since patient still eats. Yes May or may not use Induced vomiting (purging) Laxative use (Abuse to drugs) Bulimia nervosa Yes Yes Low Potassium Low Low Blood sugar Low Suppression as characterized by consciously forgetting to eat because they think they are fat Defense mechanism Compulsiveness characterized by repetitive and excessive induced vomiting Tricyclic antidepressants Imipramine (Tofranil) DOC Tricyclic antidepressants Imipramine (Tofranil) Nursing ▪ Setting limits ▪ Staying after meals to ensure intake ▪ Be alert of hidden or discarded food wrappers (common sign) ▪ Assess for dehydration and electrolyte imbalance ▪ Daily weights ▪ Allowing them to keep food diary to understand disorder. However, close supervision is indicated ▪ Setting limits ▪ Staying after meals to ensure intake ▪ Assess for dehydration and electrolyte imbalance ▪ Daily weights ▪ Allowing them to keep food diary to understand disorder. However, close supervision is indicated Remember: Common etiologies associated with eating disorders are associated with factors such as: Individual (self-imposed), familial (perfectionist parents), social (peer pressure). Eating disorders are potentially life threatening due to fluid and electrolyte imbalances implicated. 379 NCLEX-RN study guide 100 m Cognitive disorder: Alzheimer’s disease Alzheimer's disease Accounts for 50% to 70% of cases of dementia (broad definition of brain disease that causes a long term or chronic cognitive malfunctioning). It is one of the most common causes of injuries resulting from fall among elderlies in the US, both in and out patient population. Alzheimer’s implies SAFETY precautions as a priority at any time. Remember: Pick’s disease is a form of dementia with similar symptoms of Alzheimer’s disease which is most specific to frontotemporal degeneration of the brain. Defining characteristic of the disease is build-up of tau proteins in neurons, accumulating into silverstained aggregations known as "Pick bodies" which can only be done on autopsy. Acronym: 3 As Aphasia: Language deficit either expressive, receptive or both Agnosia: Unable to recognize things Anomia: (A form of aphasia) unable to recall the names of everyday objects Safety: “Sundowning” Also known as sundown syndrome, is a phenomenon associated with increased confusion and restlessness in patients with Alzheimer's disease, usually before the day ends. Acronym: ATE Aricept (Donepezil) Tacrine (Cognex) Exelon (Rivastigmine) 380 NCLEX-RN study guide 100 m Schizophrenia spectrum disorder: Schizophrenia spectrum disorder: Psychotic disorders Includes a range of linked conditions of schizophrenia. Symptoms fall into two broad categories: positive and negative symptoms. Positive symptoms are current manifestation and are not present before diagnosis and are all present to each disorders under this spectrum. Negative symptoms are normal characteristics of an individual before the diagnosis which are not currently seen and may or may not be present to each disorders. Disorder Characteristics Signs & symptoms Brief psychotic Symptoms last for 30 days (+) symptoms (-) symptoms Schizophreniform Symptoms last 30 days – 6 months (+) symptoms Schizophrenic Persistent symptoms more than 6 moths (+) symptoms (-) symptoms Schizoaffective Exhibiting symptoms of both schizophrenia and a mood disorder (bipolar, depression) (+) symptoms (-) symptoms Delusional Previously called paranoid disorder. Exhibits delusion as a major manifestation (+) symptoms (delusional) Substance abuse psychosis Psychotic disorder with substance abuse etiology (+) symptoms With or without (-) symptoms Schizotypal Always fantasizing and socializes in a strange way “awkward”. If without (+) symptoms, can be a cluster A personality disorder (+) symptoms 381 NCLEX-RN study guide 100 m Positive (+) symptoms ▪ Anxiety/Akathisia/Agitation ▪ Hallucination (perception of something not present) ▪ Delusion (false conviction to something that is not real) Remember: Positive symptoms are treated with typical anti-psychotics with suffix “AZINE”, “DOL” except Loxapine and Molindone. Example: Haloperidol, Chlorpromazine Remember: Both negative and positive symptoms are treated with atypical anti-psychotics with suffix “PINE”, “ONE”, “ZOLE” Example: Olanzapine, Quetiapine, Clozapine, Ziprasidone, Risperidone, Aripiprazole Remember: Psychotropic medications are major tranquilizer except for antianxiety (minor). This medications can cause major CV effects (hypotension). Remember: 2-3 Rule 2-3 minutes antianxiety medications takes effect 2-3 days anti-Parkinson medications takes effect 2-3 weeks anti-depressant medications takes effect Side effects: ▪ Drowsiness, Dizziness, ▪ Tremors, Restlessness ▪ Tachycardia ▪ Blurred vision ▪ Constipation ▪ Dry mouth ▪ Skin rash ▪ Photosensitivity ▪ Muscle spasms Negative (-) symptoms Acronym: 6 As (except anxiety, akathisia, agitation) ▪ Anhedonia: Loss of pleasure ▪ Avolition: Loss of motivation ▪ Ambivalence: indecisiveness ▪ Alogia: Loss of logic ▪ Anergia: Loss of energy ▪ Apathy/Affect disturbance: Loss of feelings Psychotropic medications are given with food or after meals except for antianxiety (pre-meals) Adverse effects: ▪ Agranulocytosis: sore throat and fever ▪ Malignant hyperthermia: Fever and rigidity ▪ Neuroleptic malignant syndrome (NMS): Fever, rigidity, etc. (all s/s) Tardive dyskinesia (dystonia) Minor: Puffing of cheeks, Lip smacking, tongue protrusion Major: Oculogyric crisis (rolling of eyes), Torticollis (stiffed neck), Opisthotonus (arching of back) Hepatotoxicity, Orthostatic hypotension, Pseudo parkinsonism 382 NCLEX-RN study guide 100 m Common disorders related to psychopharmacology: Malignant hyperthermia Neuroleptic malignant syndrome (NMS) Serotonin syndrome Causative drug Succinylcholine, Antipsychotics Antipsychotics, Withdrawal from anti-Parkinson’s Serotonergic agents (overdose or combination) Onset of symptoms Minutes to hours Days to weeks Hours Mental status Agitation Stupor Agitated Muscle symptoms Rigidity Rigidity Rigidity with tremors Vitals Severe hyperthermia, Tachycardia, Hypertension, Tachypnea Hyperthermia, Tachycardia, Hypertension, Tachypnea Hyperthermia, Tachycardia, Hypertension, Tachypnea Dantrolene Bromocriptine, Dantrolene Chlorpromazine, Benzodiazepines (e.g. Diazepam) DOC Remember: There must be a minimum of 14 days (2 weeks) between the administration of anti-depressants (e.g. MAOIs and SSRIs) to avoid serotonin syndrome;, these medications cannot be administered concurrently. Serotonin syndrome: A life-threatening condition, develops when drugs affecting the body's serotonin levels are administered in combination or in overdose. This include anti-depressants such as selective serotonin reuptake inhibitor (SSRI), serotonin norepinephrine reuptake inhibitor (SNRI), monoamine oxidase inhibitor (MAOI), tricyclic antidepressants (TCAs), tramadol, dextromethorphan, St. John's wort, ondansetron. metoclopramide, 383 NCLEX-RN study guide 100 m Mood disorders: Depression and Bipolar disorders Depression (Unipolar depression) Major depressive disorder: Characterized by: Meets 5 criteria Last ≥ 2 weeks Persistent depressive disorder/Dysthymia (PDD) Characterized by: Meets 3 criteria Last ≥ 2 years Depression criteria: SIGECAPS S: Sleep problems (Insomnia or hypersomnia) I: Interest lost (anhedonia) G: Guilt (worthlessness, hopelessness) E: Energy deficit C: Concentration deficit A: Appetite (increased or decreased) P: Psychomotor retardation or agitation S: Suicidality Bipolar Disorder Bipolar I: Bipolar II Characterized by: ▪ Mania episode ▪ Positive (+) symptoms of psychosis ▪ Psychotherapy, cognitive therapy, and medications ▪ Treated with electroconvulsive therapy Characterized by: ▪ Hypomania episode ▪ No positive (+) symptoms of psychosis ▪ Psychotherapy, cognitive therapy, and medications ▪ No electroconvulsive therapy needed 384 NCLEX-RN study guide 100 m Antidepressants: 1 Selective serotonin reuptake inhibitor (SSRI) Increase the serotonin level in the brain by preventing it's reuptake by the presynaptic neurons. It simply means it will remain available to bind to postsynaptic neurons and exert its mood enhancing effects. Low serotonin levels are a cause of depression. Remember: Reuptake is the reabsorption of a neurotransmitter by transporter located along the plasma membrane of an axon terminal after it has performed its function of transmitting a neural impulse. Reuptake is necessary because it allows for the recycling of neurotransmitters and regulates the level of neurotransmitter. Any abnormal amounts of neurotransmitter may affect neuronal function easily. 385 NCLEX-RN study guide 100 m Remember: Excitatory neurotransmitters (SEND-G) FSF Fluoxetine (Prozac) Sertraline (Zoloft) Fluvoxamine (Luvox) ▪ ▪ ▪ ▪ ▪ Nursing: SSRI S: Sexual dysfunction S: Sleep disturbance (Insomnia) R: Restlessness I: Increase weight Serotonin Epinephrine Norepinephrine Dopamine Glutamate (most abundant) Decrease levels in excitatory NT may cause the opposite (depression) than may be caused by acetylcholine as an inhibitory NT. 2 Serotonin and norepinephrine reuptake inhibitor (SNRI) Inhibits the reuptake of serotonin and norepinephrine in the presynaptic neurons. 3 Venlafaxine (Effexor) Nursing: SNRI S: Sexual dysfunction N: Nausea/vomiting R: Reduced weight I: Insomnia IAC “ine’s, il’s” Tricyclic antidepressants (TCA) Inhibits both reuptake of serotonin and norepinephrine as well as inhibiting production of acetylcholine (anticholinergic effects) Imipramine (Tofranil) Amitriptyline (Elavil) Clomipramine (Anafranil) Nursing: TCA T: Tension/tention (hypotension, urinary retention) C: Cardiovascular effects (e.g. palpitations, hypotension, arrhythmias) A: Arrhythmias 386 NCLEX-RN study guide 100 m 4 5 Multimodal/Atypical antidepressants Frequently used in patients with major depression who have inadequate responses or intolerable side effects during first-line treatment with SSRIs or other antidepressants. In general, they increase excitatory NT same with the other class. Monoamine oxidase inhibitors (MAOI) Inhibits monoamine oxidase an enzyme which is responsible in breaking down amines (dopamine, serotonin, epinephrine). By inhibiting these enzymes, it tends to increase levels of tyramine, a precursor of the amines. Last line of medication due to tyramine Cardiovascular effects such as hypertensive crisis. Remember that this NT chemicals are excitatory. Bupropion (Wellbutrin) Trazodone (Oleptro) Vortioxetine (Brintelix) Remember: These medications are most commonly indicated in the US these days. Trazodone is tetracyclic antidepressant with similar effects such as TCA. Crushing, cutting and chewing these medications are contraindicated because its mostly prepared as extended release (XR) to minimize side effects PAMANA (Parnate) Tranylcypromine (Marplan) Isocarboxacid (Nardil) Phenelzine Nursing: Avoid tyramine rich food Avoid: ABC ▪ Aged cheese, avocado ▪ Bananas, beers (alcoholic beverages) ▪ Cold cuts, cured meats Remember: Selegiline is a MAOI that has less chances of causing hypertensive crisis due to its route of administration given as a patch. Remember: Fresh cheese is OK When I was in AMERICA, I visited my aunt RICOTTA, she is a FARMER. I usually stay in a COTTAGE and eat my favorite CREAM cheese. Fresh cheeses: American Ricotta Farmer’s Cottage Cream 387 NCLEX-RN study guide 100 m Lithium: Lithium is a mood stabilizer most often used to treat bipolar disorders. It is usually given with antipsychotics for the first 2 weeks to treat symptoms of mania because it will take 2 weeks to achieve its effects. Lithium has a narrow therapeutic index or a “thin line” between therapeutic effects and toxicity. Lithium toxicity is triggered by dehydration, impaired kidney function (in the elderly), diet low in sodium, and drugdrug interactions (e.g. NSAIDs and diuretics). Acute manifestations: NAVDA (GI symptoms) N: Nausea A: Abdominal pain V: Vomiting D: Diarrhea A: Anorexia Prevention: ▪ Extra sodium intake to avoid depletion: Hyponatremia, dehydration triggers toxicity ▪ Increase fluid intake (2-3 L/day) ▪ Regular blood works for lithium levels and kidney function Chronic manifestations: Neurologic symptoms Neuromuscular excitability (tremors, agitation, restlessness, confusion) followed by coma if not treated promptly. Dialysis is a treatment of choice. Lithium level: 0.5—1.5 mEq/L (Acute/Adult) 0.6—1.2 mEq/L (Maintenance) 0.4—1.0 mEq/L (>65 YO) 6 to 8 mEq/L: needs dialysis Electroconvulsive therapy: Electroconvulsive therapy: ECT is an effective treatment for severe form major depression with psychotic symptoms (bipolar I). Can be used also in clients who do not respond to medications or patient with severe symptoms awaiting for the effects of medications (2 weeks). The usual course is 1-1 ½ months (2-3 sessions per week) Remember: Confusion and memory loss are common effects due to anesthesia and muscle relaxants administered concurrently during brief convulsions. 388 NCLEX-RN study guide 100 m Anxiety disorders: Are group of disorders characterized by significant feelings of anxiety and fear. Anxiety is a worry about future events, and fear is a reaction to current events. The implication is that, it may cause variety of physiological symptoms such as tachycardia, palpitations, arrhythmias, etc. Safety is a priority because potentially it can lead to panic attack and may cause potential death. Generalized anxiety disorder is a common disorder that may last more than 6 months and is characterized by excessive, exaggerated anxiety and worry about everyday life events with no obvious reasons. Below are the specific disorders of anxiety that severely affects individuals’ various aspects of life. Disorders Overview “Irrational fear or aversion to something” which is persistent and excessive. Example: 1. Agoraphobia - Fears and avoid places or situations that might cause panic and make you feel trapped or helpless. The fear they experience is out of proportion to any actual danger. Need to get accompanied by a relative or friend when facing situations is common. Phobia Common situations: In a crowd, Traveling in a public transport, in a bridge or in a tunnel or enclosed spaces such as malls, halls, theaters, open spaces such parking. 2. Social anxiety disorder - Fear of “scrutiny” or embarrassment in a public in a performance such public speaking. 3. Specific phobias – Claustrophobia (specific to confined spaces, not necessarily in public), Aerophobia (Airplane), Acrophobia (heights) Post-traumatic stress disorder (PTSD) “Reaction to a traumatic or disastrous event that is lifethreatening to oneself or others” Characteristics: ▪ Flashbacks/nightmares ▪ Reminder avoidance (e.g. avoids watching news related to traumatic event experienced) ▪ Increased anxiety and arousal 389 NCLEX-RN study guide 100 m “Pattern of unreasonable thoughts and fears (obsessions) that lead to do repetitive behaviors (compulsions)” Obsessive compulsive (OCD) Characteristics: OCD is distinguished from OC personality disorders (OCPD) as the former suffers from depression. They are fully aware that their obsession/compulsion is undesirable for others, in which they could not control leading to depression. In OCPD, they are not aware of their behavior. For them, it’s just but part of daily routine. This insight leads to a better outcome (no depression) comparing to OCD. “Unintentional, extreme focus on physical symptoms such as pain or fatigue that causes major emotional distress and anxiety as well as problems in functioning” Somatic symptom disorder Factitious (Munchausen) disorder Hypochondriasis - exaggerated symptoms of serious illness Body dysmorphic - perceived defects or flaws in your appearance “feeling ugly” Pain disorder – exaggerated symptom of pain Conversion disorder – (aka functional neurological symptom d/o) converting to neurologic symptom such as seizure, loss of consciousness, blindness, deafness with no medical basis. “Intentional, habitual lying or faking disease in order to play the patient role, not necessarily to achieve a personal gain” Munchausen by proxy syndrome – a more harmful type in which the person involves other person (mostly their children) to make it appear that their ill. They intentionally injure the child. This syndrome is a form of child abuse. “Intentional, habitual lying or faking disease in order to necessarily achieve a personal gain” Malingering Primary gain – patient wants attention to increase his/her self-esteem (internal motivators)as a gain by faking. Secondary gain – patient wants a sick leave even not sick, to gain money from converted leaves (external motivators) Tertiary gain – Uses someone’s illness (third person) to achieve a personal gain 390 NCLEX-RN study guide 100 m Personality disorders: Are a group of mental illnesses involving long-term patterns of thoughts and behaviors that are unhealthy and inflexible. The behaviors cause serious problems with relationships and work. They are categorized into 3 clusters: Cluster A: “Odd or weird personalities”, associated with schizophrenia Cluster B: “Wild, overly dramatic personalities”, associated with mood disorders and substance abuse Cluster C: “Easily worried and anxious personalities”, associated with anxiety disorders Cluster A Paranoid Schizoid Schizotypal Cluster B Overview “Accusatory and underdeveloped trust” Characteristics: ▪ Eager observant ▪ Mistrust ▪ Pervasive suspicion ▪ Hypersensitive “Social withdrawal, aloof” Characteristics: ▪ Does not socialize and distant from people ▪ Does not find socialization enjoyable ▪ Solitary in activity “Always fantasizing and awkward” Characteristics: ▪ Socializes but in an awkward or strange way ▪ Classified within schizotypal spectrum if with positive (+) symptoms of schizophrenia Overview “No rules, disregards others rights” Antisocial Characteristics: ▪ Womanizer/Unfaithful ▪ Lack of empathy and guilt ▪ Highly aggressive and irritable ▪ Impulsive ▪ Consistently irresponsible ▪ Blaming others ▪ History of conduct disorder from childhood 391 NCLEX-RN study guide 100 m “Split personalities” Borderline Characteristics: ▪ Risk takers, suicidal ▪ Dissociates from one personality to another (from joyful to anger/rage) “mood swings” ▪ Impulsive ▪ Also manifest antisocial behavior but they are not persistent in disregarding rules “Self centered” Narcissistic Characteristics: ▪ Sense of self-importance and entitlement ▪ Excessive admiration to self ▪ Arrogant ▪ Lack of empathy and guilt ▪ Taking advantage of people around them “Overly acting (OA)” Histrionic Cluster C Characteristics: ▪ Excessive attention seeking ▪ Seductive behavior “Flirt” ▪ Dramatic ▪ Rapid shifts of emotion (more to drama) ▪ Seeks approval from others Overview “Clingy” Dependent Characteristics: ▪ Excessive reliant from other people ▪ Inability to make his/her own decisions ▪ Fear of abandonment or being alone ▪ Helpless when relationship ends ▪ Afraid of confrontation ▪ Low self confidence ▪ Advice seekers “Coward” Avoidant Characteristics: ▪ Avoids social interaction ▪ Inferiority behavior ▪ Afraid of criticism from others ▪ Low self confidence 392 NCLEX-RN study guide 100 m Obsessive compulsive personality (OCPD) “OC” Characteristics: ▪ Dislikes unpredictable events or situations ▪ “Time is gold” character but inflexible to circumstances ▪ Excessive concern to orderliness, cleanliness, attention to details ▪ Imposes own standards, reluctant in delegating task ▪ Rigid and determined ▪ Hoarder ▪ Aware and happy with their behavior otherwise may lead into depression (OCD) Autism spectrum disorders (ASD) vs Attention deficit hyperactivity disorder (ADHD): ASD A group of disorders generally characterized by 1. antisocial behavior and 2. repetitive movements or fixation to a certain actions such as spinning, hand shaking, rocking. ASD Management No medication is needed unless with severe form(CDD) to treat symptoms. Behavioral and enrichment of skills education are also indicated ADHD Is one of the most common neurobehavioral disorders of childhood. It is usually first diagnosed in childhood and often lasts into adulthood. Generally characterized by 1. Hyperactivity, 2. impulsiveness and 3. inattentiveness ADHD management DOC: Methylphenidate (Ritalin). Mechanism of action is to balance dopamine Nursing: ▪ Given in the morning to prevent insomnia or 4-6 hours prior to sleeping hours ▪ Monitor BP and HR since it increases dopamine ▪ Given after meal because it cause decrease appetite 393 NCLEX-RN study guide 100 m ASD Overview Classic autism Characteristics: Antisocial and fixation ▪ Speech delay (classic sign) ▪ Low IQ autism ▪ Common in < 3 YO Asperger’s disorder Characteristics: Antisocial and fixation ▪ Mild autism ▪ Normal or high intelligence ▪ “High-functioning autism” Pervasive developmental disorder nonotherwise specified (PDD-NOS) Characteristics: Antisocial and fixation ▪ Does not meet other criteria of autism ▪ Mild autism/atypical autism Childhood disintegrative disorder (CDD)/ Heller’s syndrome Characteristics: Antisocial and fixation ▪ Severe form of autism ▪ Deterioration in skills which were attained previously ▪ Late onset developmental delays ▪ Loss of bladder and bowel control ▪ May have seizures Substance abuse: depressants and stimulants Depressant “downers” Chemicals or drugs that slows down the central nervous system (CNS) function such as bradycardia, hypotension, hypoventilation, drowsiness. Commonly abused are alcohol and narcotic or opioid medications. Stimulants “uppers” Chemicals or drugs that speeds up the central nervous system (CNS) function such as tachycardia, hypertension, hyperventilation, confusion, agitation. Commonly abused are amphetamines, marijuana, cocaine, ecstasy. 394 NCLEX-RN study guide 100 m Withdrawal Intoxication Describes as ingestion of large quantity of a substance either a stimulant or a depressant achieving it toxic effects. Group of symptoms that occur upon the abrupt discontinuation or decrease in intake of abused chemical in which a person develops dependence. Remember that these chemicals are addictive, if stopped abruptly, the body springs off (rebound effect) and produces opposite effect of the substance. Commonly abused substance: Stimulants and depressants STIMULANTS Intoxication classic sign Withdrawal classic sign Chronic use Cocaine Epistaxis Mental depression Nasal septum deviation Amphetamines Halitosis Mental depression Cachexia (muscle wasting), Psychosis Marijuana Blood shot eyes “no withdrawal” Memory loss, Psychosis DEPRESSANTS Intoxication classic sign Withdrawal classic sign Chronic use Alcohol Hypoventilation, CNS depression Delirium tremens “DTs” Wernicke’sKorsakoff syndrome Codeine Muscle incoordination Headache, Insomnia, sweating Impotence Morphine Extreme drowsiness Piloerection “goosebumps” Personality changes Heroin Pinpoint pupils Rhinorrhea Personality changes 395 NCLEX-RN study guide 100 m General symptoms of INTOXICATION from depressants Remember: CNS depressant means respiratory compromise as a priority. Other effects are cardiovascular and autonomic. ▪ Hypoventilation resulting to respiratory acidosis and respiratory depression ▪ Bradypnea ▪ Bradycardia ▪ Decrease level of consciousness ▪ Miosis (pupil constriction) ▪ Constipation ▪ Nausea/vomiting ▪ Urinary incontinence ▪ Pruritus DOC (antidote): Naloxone General symptoms of WITHDRAWAL from depressants Remember: Withdrawal symptoms are the rebound effects of this substances. The body tends to “crave” for its addictive effects by increasing the amounts of excitatory NT. Dehydration and seizure are the priority. Early S/S: ▪ Hyperventilation resulting to respiratory alkalosis ▪ Tachypnea, Tachycardia ▪ Anxiety, agitation, tremors ▪ Diaphoresis ▪ Mydriasis (pupil dilation) Late S/S: ▪ Diarrhea ▪ Severe nausea/vomiting ▪ Piloerection (goosebumps) ▪ Rigidity ▪ Seizure ▪ Hallucination DOC (antidote): Methadone Remember: Methadone is also an opioid medication. However, due to its long half-life up to 60 hours, the drug can still remain in the body in large amounts enough to sustain the “craving” and limit symptoms. Remember: Intoxication from stimulant substances cause the same manifestations from withdrawal to depressants, vice versa. This is caused by the rebound effects. Neurotransmitters from the brain are sensitive to this substances. 396 NCLEX-RN study guide 100 m Alcohol use disorder: Lethal alcohol levels: 400 mg/dL (> or =0.4%) Antabuse vs Librium Remember: Disulfiram (Antabuse) is for alcohol intoxication to keep patient sober from alcohol. Antabuse is an antidote that blocks the enzyme necessary in alcohol metabolism and produces an UNPLEASANT effects to patients making the body get rid of it. This leads into gradual non-craving from alcohol. On the other hand, Chlordiazepoxide (Librium), a CNS depressant is given to limit symptoms of withdrawal such as agitation, anxiety, restlessness, tremors etc. Acronym: A L cohol Antabuse – Intoxication Librium – Withdrawal Nursing care: Disulfiram (Antabuse) ▪ Patient should be alcohol free for at least 12 hours before giving the medication ▪ Avoid “MOFAVS” M: Mouthwash O: OTC medications F: Fermented wines A: Aftershave V: Vinegar S: Skin products Delirium tremens: Rapid onset of confusion and other symptoms related to withdrawal from alcohol substance. Safety is the priority for this patient (risk for injury). Wernicke’s – Korsakoff syndrome: is a type of brain disorder caused by a lack of Vit B1(thiamine)and Vit B3 (niacin) most commonly caused by chronic alcoholism. The syndrome is actually two separate conditions that can occur at the same time characterized by gradual memory loss (amnesia) specifically confabulation, a form of memory loss wherein a patient fills in false stories during a talkative conversation 397 100 m NCLEX-RN study guide Question: The home health aide reports to the nurse care manager that the client has been trying to give away possessions. When the nurse asks the client about this behavior, the client says, "With my spouse dead, there's no reason for me to go on." What is the best priority response by the nurse? 1. "Do you have any friends in the building?" 2. "Have you had any thoughts of hurting yourself?" 3. "Tell me more about how you're feeling." 4. "You're not thinking of killing yourself, are you?" Answer: 2 Rationale: A suicide risk assessment is the priority nursing action for a client who expresses thoughts about "not wanting to go on" or "wishing for death" or engages in potential suicidal indicators such as giving away possessions. Asking the client directly about thoughts of hurting or killing oneself is a therapeutic approach necessary to assess risk of immediate suicide. Option 4 is a misleading statement and provokes suicide thought. Other options (1 and 3) are correct but are not priority. 398 NCLEX-RN study guide 100 m 21 Miscellaneous Normal Values: Vital Signs: Heart rate: 80-100 bpm Respiratory rate: 12-16 rpm Blood pressure: 110-120/60-70 mmHg Temperature: 37 °C (98.6 °F) T (°C) = (T (°F) - 32) × 5/9 T (°F) = T (°C) × 9/5 + 32 Basic Conversions 1 teaspoon (t) = 5 ml 1 tablespoon (T) = 3 t = 15 ml 1 gram (g) = 1,000 mg 1 mg = 1000 mcg 1 kilogram (kg) = 2.2 lbs. 1 grain (gr) = 65 mg 1 lb. = 16 oz 1 oz = 30 ml 1 cup = 240 ml 1 cup = 8 oz 1 quart = 2 pints 1 pint = 2 cups 1 meter = 3.28 feet Hematologic • RBCs: WBCs: Platelets: 4.5 - 5.0 million/liter 5,000 - 10,000 /µL 200,000 - 400,000/µL Rapid Response Team (RRT): consists of a group of health care providers who bring critical care expertise to the bedside of clients demonstrating early signs of deterioration. It differs from the "Code" team that is called when a client stops breathing or goes into cardiac arrest. Criteria in activating RRT: 1. Nurse is worried 2. An acute change in any of the following: ▪ Heart rate: <40 or >130/min Systolic BP: <90 mm Hg ▪ RR: <8 or >28/min ▪ O2 Sat: <90 despite O2 ▪ Urine output: <50 mL/4 hr. ▪ Decrease LOC Safety Alert: Critical results Are tests and diagnostic procedures that fall significantly outside the normal range and may indicate a life threatening situation. The objective is to provide the responsible licensed caregiver these results within an established time frame so that the patient can be promptly treated. 399 NCLEX-RN study guide 100 m Hemoglobin (Hgb): 12 - 16 gm (f) 14 - 18 gm (m) Hematocrit (Hct): 37 - 47 (f) 40 - 54 (m) Acronym: Never Let Monkeys Eat Bananas (WBC percentage amount) Neutrophils: Never 54 - 62% Lymphocytes: Let 25 - 32% Monocytes: Monkeys 3 - 7% Eosinophils: Eat 1 - 3% Basophils: Bananas <0.75% Comprehensive Metabolic Panel (CMP) Sodium: Potassium: Serum Glucose: Calcium: BUN: Creatinine : Chloride: CO2: Total Protein: Albumin: Bilirubin: Alkaline Phosphatase (ALP): Aspartate aminotransferase (AST): Alanine aminotransferase (ALT): 135 -145 mEq/L 3.5 - 5.5 mEq/L 70-110 mg/dl 9 -10.5 mEq/L 10 – 20 mg/dl 0.5 – 1.5 mg/dl 90 - 110 mEq/L 35 – 45 mmHg 6 – 8 g/dl 3.5 – 5 g/dl <1.5 mg/dL 44 to 147 U/L 10 - 50 IU/L 5 - 35 IU/L Remember: CMP Is a frequently ordered panel of 14 tests that gives a healthcare provider important information about the current status of a person's metabolism, including the health of the kidneys and liver, electrolyte and acid/base balance as well as levels of blood glucose and blood proteins. 400 NCLEX-RN study guide 100 m Others: Magnesium: Phosphorus: Ammonia: LDH: Total Cholesterol: Triglyceride: HDL (Good Cholesterol): LDL (Bad Cholesterol): HBA1C: 1.7 - 2.2 mEq/L Tumor lysis syndrome (TLS): 3 - 4.5 mEq/L A potential complication of 15 - 110 ug/dl chemotherapy is acute TLS, a rapid release of 100 - 190 U/L intracellular components <200 mg/dL into the bloodstream. TLS <150 mg/dL include rising blood uric >45 mg/dl (m) acid, potassium, and phosphate levels, with >50 mg/dl (f) decreasing calcium levels. 60 - 80 mg/dl With diabetes: < 7% Good control > 9% Poor Control > 12% Very Poor Control With no diabetes: 4 - 5.6% normal level 5.7 - 6.4% high chance of diabetes ≥6.5% Diabetes 1.010 - 1.030 3.5 - 7.5 mg/dL Urine Specific Gravity: Uric Acid: Heart failure: B-Type Natriuretic Peptide (BNP): <125 pg/mL (0 - 74 YO) <450 pg/mL (75 - 99 YO) • • Brain (or b-type) natriuretic peptide (BNP): Secreted in response to ventricular stretch and wall tension when cardiac filling pressures are elevated. The BNP level is used to differentiate dyspnea of heart failure from dyspnea of noncardiac etiology. Remember: Refeeding syndrome A serious complication of nutritional replenishment. It is marked by declines in serum phosphorus, potassium, and/or magnesium (mnemonic PPM). Most common to homeless and anorexia when abruptly giving food after periods of starvation. Electrolytes should be monitored frequently. 401 NCLEX-RN study guide 100 m Acute Coronary Syndrome (ACS): In order rising: Myoglobin: 0 - 85 ng/ml Troponin: < 0.6 ng/ml (most specific and most sensitive) CPK: 12 - 70 U/ML (m), 10 - 55 U/ml (f) AST: 10 - 50 IU/L LDH: 100 - 190 U/L Anticoagulant Therapy: Heparin – Antidote: Protamine sulfate aPTT: 30 - 40 sec (more sensitive) (1.5 - 2X is therapeutic) Risk for Bleeding: > 80 secs PTT: 25 - 35 sec (less sensitive) (1.5 - 2X is therapeutic) Risk for Bleeding: > 70 secs Warfarin (Coumadin) - Antidote: Vitamin K PT: 10 - 12 sec (1.5 - 2X is therapeutic) Risk for Bleeding: > 24 secs INR: 0.9 - 1.18 (up to 3X is therapeutic) Risk for Bleeding: > 3.5 secs Drug Therapeutic Levels: Carbamazepine (Tegretol): Phenobarbital : Digoxin (Lanoxin): Theophylline (Aminophylline): Phenytoin (Dilantin): 4 - 10 mcg/ml 15 - 0 mcg/mL 0.8 - 2.0 ng/ml 10 - 20 mcg/dL 10 - 20 mcg/dL 402 NCLEX-RN study guide 100 m Valproic Acid (Depakene): 50—100 mcg/ml Lithium: 0.5 - 1.5 mEq/L (Acute/Adult) Remember: 0.6 - 1.2 mEq/L (Maintenance) Toxic levels mean 0.4 - 1.0 mEq/L (>65 YO) compromised KIDNEY function. Always check for 6 - 8 mEq/L (Severe toxicity) renal panel. (BUN, Vancomycin: creatinine) 20 - 40 mcg/ml (peak) 5 - 15 mcg/ml (trough) Remember: Vancomycin Peak (effectivity): Blood Magnesium Sulfate: draws 15 - 30 mins after the 4 - 8 mg/dl (therapeutic level) dose 8 - 10 Absence of reflexes Trough (toxicity): Blood 10 - 12 Respiratory depression draws 15 – 30 mins before the next dose > 15 Coma/death Poisoning: Lead: 5 U - Safe Level 10 U - Toxic Level 70 U - Medical Emergency Lead poisoning in children: Can lead to many severe complications of the kidneys & neurological system (e.g. developmental delays, cognitive impairment, seizures). A common source of exposure is lead-based paints found in houses built before 1978, when such paint was banned. Blood lead level (BLL) screenings are recommended at ages 1 and 2, and up to age 6 if not previously tested. Carbon Monoxide: 10 to 20% (Headache) > 20 % (Generalized weakness) > 30% (Chest Pain) > 40% (Seizure, unconsciousness) > 60% (Coma - Death) Remember: The priority action is to administer 100% oxygen using a nonrebreather mask to treat hypoxia and help eliminate CO. 403 NCLEX-RN study guide 100 m Aspirin: 50 - 100 mg /ml Remember: Aspirin should not be given to those under the age of 16 years, unless specifically indicated in Kawasaki disease or in the prevention of blood clot formation. Severe liver damage is closely associated with acetaminophen & aspirin overdose or Reye syndrome. Pressures (mmHg): ICP: 0 - 10 mmHg IOP: 12 - 15 mmHg Airway Suction Pressure: 100 - 120 mmHg (adults) 80 - 100 mmHg (children) 60 - 80 mmHg (infants) ET/Tracheostomy cuff pressure: 15 mm Hg (20 cm H2O) Chest tube negative pressure: 20 cm H2O Hemodynamics Remember: Permissive hypertension is allowed within the first 24-48 hours of an acute ischemic stroke provided that the BP is <220/120 mm Hg. This practice allows adequate cerebral perfusion to keep the stroke from extending. Mean arterial pressure (MAP) formula: = 2 (DBP) + SBP 3 Pulse Pressure formula: = SBP - DBP MAP: 70-105 mm Hg Pulse Pressure: 40 mm Hg Central Venous Pressure (CVP)/Right Atrial Pressure (RAP): 2 - 8 mmHg Right Ventricular Pressure (RVP): 15 - 25 mmHg (systolic) 0 - 8 mmHg (diastolic) Pulmonary Artery Pressure (PAP): 20 - 30 mmHg Pulmonary Capillary Wedge Pressure (PCWP): 8 - 13 mmHg 404 100 m NCLEX-RN study guide Positioning: Above Knee Amputation: Elevate for first 24 hours on pillow, position on prone daily to prevent Hip Flexion Contractures Air/Pulmonary embolism: Turn to left side and lower HOB to promote resistance, preventing emboli going towards pulmonary artery Asthma: Orthopneic position, patient sitting up and bent forward with arms supported on a table or chair . Promotes O2 and lung expansion Autonomic Dysreflexia: Sitting position (elevate HOB) first before any other implementation. Promotes comfort, breathing Below Knee Amputation: Foot of bed elevated for first 24 hours, position prone daily to prevent hip flexion contractures Bronchiolitis: Tripod position to promote drainage of secretion, improves lung expansion Buck’s Traction: Elevate foot of bed for counter-traction Cardiac Catheterization: Seep site extended. Preventing impede circulation Cast: Elevate extremity to prevent edema Cerebral Aneurysm: High Fowler’s to prevent rupture Cleft-lip: Position on back or in infant seat to prevent trauma to the suture line. While feeding, hold in upright position to prevent aspiration Cleft-palate: Prone to promote drainage of secretion Cleft Lip and Palate: Supine or side to prevent rubbing Detached retina: Area of detachment should be in the dependent position to promote reattachment of retina Dumping Syndrome: Eat in reclining position, lie down after meals for 20-30 minutes to slow down food movement Enema Administration: left-side lying (Sim’s position) with knees flexed to rest rectum Epistaxis: Lean forward to prevent aspiration Flail Chest: Affected side to facilitate expansion of unaffected lung 405 100 m NCLEX-RN study guide Fracture of the neck of femur: Internal rotation of the leg with extension of the knee to promote alignment Head Injury: HOB 30° to prevent Increased ICP Hemorrhoidectomy: Assist to lateral position to promote comfort Hemorrhagic Stroke: HOB elevated 30 degrees to reduce ICP and facilitate venous drainage. Hiatal Hernia: Upright position to prevent reflux Increased ICP: High Fowler’s to facilitate venous drainage. Internal radiation implant: Complete bed rest while implant is in place to prevent dislodgement Intestinal Tubes: Right side lying to facilitate passage into duodenum Laminectomy: Back as straight as possible; log roll to move and sand bag on sides to promote alignment Liver Biopsy: Right side lying with pillow, or small towel under puncture site for at least 3 hours to prevent bleeding Lobectomy: Semi fowlers to promote breathing Mastectomy: Elevate affected side with pillow to prevent lymphedema Myelogram: (Water-based dye) semi Fowler’s for at least 8 hours to promote drainage (Oil-based dye) flat on bed for at least 6-8 hours to prevent leakage of CSF, (Air dye)Trendelenburg to suspend air promoting drainage to venous circulation Nasogastric Tubes: Elevate HOB 30°, Maintain elevation for continuous feeding or 1hour after intermittent feedings, prevents aspiration Paracentesis: Flat on bed or sitting, promotes comfort, lung expansion Peritoneal Dialysis: When outflow is inadequate turn patient side to side before checking for tube kinks to mobilize fluids Post abdominal aneurysm surgery: Fowler’s position to improve circulation Post Bronchoscopy: Flat on bed with head hyperextended to promote patent airway 406 100 m NCLEX-RN study guide Post cataract surgery: Sleep on unaffected side with a night shield for 1-4 weeks to prevent increase IOP Post infratentorial surgery (incision at nape of neck): Flat and lateral on either side to prevent trauma to incision site, to promote patent airway and drainage of secretions Post Lumbar puncture: Flat for 2-3 hours to prevent headache and leaking of CSF. Post myringotomy: On the side of affected ear post-surgery to allow drainage of secretion Post Supratentorial surgery (incision behind hairline): Elevate HOB 3045 degrees, neutral position, to promote patent airway and drainage of secretions Post Total Hip Replacement: Don’t sleep on operated side, don’t flex hip more than 45-60 degrees, don’t elevate HOB more than 45 degrees. Maintain hip abduction by separating thighs with pillows to prevent displacement. Postural Drainage: Lung segment to be drained should be in the uppermost position to allow gravity Prolapsed cord: Knee-chest position or Trendelenburg to prevent compression Pyloric stenosis: Right side lying after meals to facilitate entry of stomach contents into intestines Rectal Exam: Knee-chest position, Sim’s, or dorsal recumbent to promote access to rectum Seizure: Side lying to promote airway, facilitate drainage of secretions Shock: Bed rest with extremities elevated 20°, knees straight, head slightly elevated (modified Trendelenburg) to promote venous return Spina Bifida: Infant on prone to prevent sac rupture Spinal Cord Injury: Immobilize on spine board, with head in neutral position. Immobilize head with padded C-collar, maintain traction and alignment of head manually. Log roll client, don’t allow to twist or bend 407 100 m NCLEX-RN study guide Thoracentesis: Sitting on the side of the bed and leaning over the table (during procedure) to promote lung expansion; affected side up (after procedure) to promote re-expansion of the affected side and prevent leaking. If leaking, position on the affected Thyroidectomy: Semi fowlers, avoid hyperflexion & hyperextension of neck to prevent tension of suture Tonsillectomy: Side lying or prone to promote drainage Total Parenteral Nutrition (TPN): Trendelenburg during insertion to prevent air embolism Tracheoesophageal fistula (TEF): Supine with HOB elevated 30° to minimize reflux, prevent aspiration Tube feeding for patients with decreased LOC: Right side to promote emptying of the stomach with HOB elevated to prevent aspiration A must have bedside equipment: Amputation – Tourniquet Autonomic Dysreflexia – Urinary Catheter Chest Tube Drainage – Extra sterile bottle with sterile H20, clamp/forceps, Vaselinized gauze Cholinergic crisis – Tracheostomy/ET tube Hydrocephalus – Tape measure Laryngotracheobronchitis – Tracheostomy Myasthenic Crisis – Tracheostomy/ET tube Parkinson’s Disease – Suction equipment Radium Implant – Lead container, long handled forceps Seizure– Suction equipment Spinal Cord Injury – Tracheostomy Tamponade tube (Sengstaken–Blakemore)– Scissors Thyroidectomy – Tracheostomy Tonsillectomy – Flashlight 408 100 m NCLEX-RN study guide Tracheostomized Patient – Obturator, hemostat (Dilator), one size smaller tracheostomy tube, Ambubag Wired Jaw – Suction equipment, Wire cutter Diets: Acute Glomerulonephritis: Low Na, low protein Addison’s disease: High Na, low potassium ADHD: High-calorie, finger foods Bedsore: High Protein, High Vitamin C Bipolar Disorder: Finger foods Burns: High protein, high caloric, high Vitamin C Cancer: High-calorie, high-protein. Celiac Disease: Gluten-free diet (no BRW: barley, rye, and wheat) selected oats only Cholecystitis: High protein, High carbohydrate, Low fat Chronic Renal Disease: Low protein, low sodium and potassium , Low phosphate, fluid-restricted Cirrhosis (stable): Normal protein Cirrhosis with hepatic insufficiency: Low protein, Low Sodium Constipation: High-fiber, increased fluids COPD: Soft, high-calorie, low-carbohydrate, high-fat, small frequent feedings Crohn’s disease: High protein, high carbohydrate, low fat Cushing’s disease: High potassium, Low Na Cystic Fibrosis: High fluids & Na, High Calorie Cystitis (Stones): Acid ash for alkaline stones (Uric, Cystine), Alkaline ash for acid stones (Calcium, Struvite), Increase OFI Diarrhea: Liquid, low-fiber, regular, fluid & electrolyte replacement Diabetes Mellitus: Balanced Diverticulitis: Low residue Diverticulosis: High Residue 409 100 m NCLEX-RN study guide Dumping Syndrome: High fat, high protein, drink 30 - 60 minutes before or after meals (no fluids with meals) Gallbladder diseases: Low fat, low calorie, regular Gastritis: Low-fiber, bland diet Gouty Arthritis: Low purine Hepatitis: Regular, high-calorie, high-protein Hirschsprung’s: High Calorie, high protein, low residue Hyperlipidemias: Fat-controlled, Low calorie Hyperparathyroidism: Low calcium Hypertension, CHF, CAD: Low sodium, low-calorie, fat - controlled Hyperthyroidism: High calorie, high protein Hypoparathyroidism: High Calcium, low phosphate Hypothyroidism: Low calorie, low fat Kawasaki disease: Clear liquid Meniere’s disease: Low sodium Nephrotic Syndrome: Low sodium & potassium, high calorie & protein Osteoporosis: High calcium, high vitamin D Pancreatitis: Low-fat, regular, small frequent feedings; tube feeding or TPN Peptic ulcer: Bland, high carbohydrate, low protein Phenylketonuria: Low phenylalanine Pregnancy Induced Hypertension (PIH): High protein Pernicious Anemia: High Vitamin B12 (Cobalamin) Renal Failure (Acute): High protein, high-calorie, fluid-controlled, sodium and potassium controlled Renal Failure (Chronic): Low sodium, potassium, low protein Sickle Cell Anemia: Increase fluids Stroke (CVA): Mechanical soft, regular, or tube- feeding Tonsillitis: Clear Liquid 410 100 m NCLEX-RN study guide Classic signs: Acute coronary syndrome – Levine’s sign (clenched fist held over the chest to describe ischemic chest pain) Infective endocarditis – Janeway lesion, splinter hemorrhages, Osler’s node, Roth spots Cardiac tamponade – Beck’s triad: Narrowed pulse pressure (hypotension), muffled/distant heart sound, distended neck veins Rheumatic heart disease – JONES criteria: Joint problem, O (looks like a heart) carditis, nodules (subcutaneous), erythema marginatum, Sydenham’s chorea. CAFE PAL criteria: CRP increased, arthralgia, fever, elevated ESR, prolonged PR interval, anamnesis (history) of rheumatism, leukocytosis Kawasaki Disease – CRASH and Burn (fever): Conjunctivitis, rash, adenopathy (cervical), strawberry tongue, hands (palmar erythema, swelling), fever Patent ductus arteriosus – Machinery like murmur Tricuspid atresia – Holosystolic murmur CHF in children – Brow or scalp sweating Abdominal aortic aneurysm – Pulsatile lump with abdominal pain (enlarging aneurysm) Aortic dissection - Moving, "ripping" back pain Deep vein thrombosis (DVT) – Virchow’s triad (venous stasis, vein trauma/endothelial injury, hypercoagulability) Peripheral arterial disease (PAD) – Intermittent claudication Asthma - High-pitched, sibilant wheezing on expiration Emphysema – Barrel chest, pursed lip breathing (pink puffers) Bronchitis (Chronic) – Obese and cyanotic (blue bloaters) Cystic fibrosis – Layered sputum, steatorrhea, salty skin, meconium ileus on birth Obstructive sleep apnea (OSA) - Loud snoring, witnessed apnea episodes, morning headaches Acute Respiratory Distress Syndrome (ARDS) aka non cardiogenic pulmonary edema – Refractory hypoxemia Superior vena cava syndrome (SVC) – Facial edema Epiglottitis - 4 Ds: dysphonia (muffled voice), dysphagia, drooling, and distressed respiration 411 100 m NCLEX-RN study guide Trigeminal neuralgia - Severe, intense, burning, or electric shock-like pain Bell’s palsy – Facial drooping Traumatic brain injury (TBI) - “Lucid interval”, followed by a quick decline in mental function Basilar skull fracture - Otorrhea, racoon’s eye, post-auricular ecchymosis (battle’s sign) Increase intracranial pressure (IICP) – Late sign: Cushing’s triad: Irregular respiration, bradycardia , widened pulse pressure (systolic HTN) Myasthenia gravis - Ptosis/diplopia, Bulbar signs (difficulty speaking or swallowing) Multiple sclerosis - Lhermitte’s sign, Charcot’s Triad: Intentional tremors, Nystagmus, Scanning speech (staccato speech) Guillain-Barre Syndrome (GBS) – Ascending paralysis Meningitis - Brudzinski Sign, Kernig Sign Alport syndrome - Hematuria (Tea colored), proteinuria, hypoalbuminemia Nephrotic syndrome – Proteinuria, hypoalbuminemia, hyperlipidemia, low anti-thrombin Nephritic syndrome - Hematuria (Tea colored), proteinuria, hypoalbuminemia Kidney stones - Flank pain (mid-lower back), renal colic (constant sharp pain) Syndrome of inappropriate ADH (SIADH) - Dilutional hyponatremia (water intoxication) Diabetes insipidus - Polyuria (2-3L/H), polydipsia Cushing’s - Truncal obesity, buffalo hump, moon shaped face hypernatremia, hypokalemia, hypocalcemia, hirsutism, acne, gynecomastia (males) Addison’s disease (primary adrenal insufficiency) - Bronze skin (hyperpigmentation), hyponatremia, hyperkalemia, hypercalcemia Diabetes mellitus (DM) – Polyphagia, polyuria, polydipsia, glucosuria Gastric ulcer – Pain while eating (relieved by vomiting), weight loss Duodenal ulcer – Pain if not eating (relieved by food), weight gain Crohn's disease (Regional enteritis) – Crampy RLQ abdominal pain, diarrhea (3-4 /day) 412 100 m NCLEX-RN study guide Ulcerative colitis – Crampy LLQ pain abdominal pain, diarrhea (More severe and painful: 10 or more x /day) Diverticulitis (inflamed diverticula) - Painless rectal bleeding, hematochezia, LLQ abdominal pain Acute pancreatitis - Epigastric pain radiating to back, Grey turner’s sign, Cullen’s sign Acute cholecystitis - Mid epigastric to RUQ radiating to scapula and shoulders, Murphy’s sign Appendicitis - RLQ (Mc Burney’s point) abdominal pain, Psoas Sign, Obturator Sign, Rouvsing sign, Blumberg Sign Pyloric stenosis - Projectile vomiting, non-bilious vomitus, olive shaped mass Intussusception - RLQ pain (intermittent cramping), currant jelly stool, sausage shaped mass Hirschsprung’s disease - LLQ pain, meconium ileus, ribbon like stool Rheumatoid arthritis – Joint pain, Boutonnière deformity, Swan-Neck deformity Osteoarthritis - Joint pain, Bouchard’s deformity, Heberden’s deformity Gouty arthritis – Joint pain, podagra, tophi (uric deposits) Developmental dysplasia of the hip (DDH) - Extra gluteal or inguinal folds/asymmetrical folds, Galeazzi sign, Barlow Sign, Ortolani sign Fat embolism – Petechial rash on the neck, chest, and axilla (defining characteristic from PE) Acute compartment syndrome - The 6 Ps: Pain, Pressure, Paresthesia, Pallor, Pulselessness, Paralysis Carpal tunnel syndrome – Tingling pain on Phalen’s maneuver, Tinel’s maneuver, Durkan’s test Age related Macular degeneration (AMD) - Los of central vision Retinal detachment – Painless, floaters, curtain sensation, flashes of light Chronic open angle glaucoma (COAG) - Loss of peripheral vision (tunnel vision) Acute close angle glaucoma (ACAG) - Eye pain, headache, nausea, blurred vision, eye redness, halos, tunnel vision Meniere’s disease (Endolymphatic hydrops) – Triad: Vertigo, tinnitus, sensorineural hearing loss 413 100 m NCLEX-RN study guide Anemia - 4Fs: Fatigue, Forgetfulness, Fainting, Fast heartbeat (tachycardia) Hodgkin’s lymphoma - (+) Reed Sternberg cells on biopsy, lymphadenopathy usually in neck and chest Non-Hodgkin’s lymphoma - (-) Reed Sternberg cells on biopsy, lymphadenopathy affects upper and lower extremities Multiple myeloma – CRAB: Calcium (hypercalcemia), Renal, Anemia, Bone pain (spine and ribs) Systemic Lupus Erythematosus (SLE) – SOAP BRAIN MD: Serositis, oral ulcers, arthritis, photosensitivity, blood disorders, renal involvement, ANA (+), immunologic, neurologic, malar rash (butterfly rash), discoid rash Pregnancy induced hypertension (PIH) - Triad: HTN, proteinuria, edema Abruptio placenta - Painful rigid abdomen, concealed bleeding Placenta previa - Painless soft boggy abdomen, bleeding Alzheimer's disease - 3 As: Aphasia, Agnosia, Anomia, “Sundowning” Drug causing urine discoloration: Amitriptyline – Blue or blue green Daunorubicin or Doxorubicin - Red/Pink Ferrous / iron dextran - Dark / Brown Heparin - Orange/yellow, Red/Pink Ibuprofen - Red/Pink Levodopa - Dark / Brown Methyldopa - Dark / Brown, Red/Pink Metronidazole - Dark / Brown, Yellow-brown Nitrates - Dark / Brown Nitrofurantoin - Dark / Brown, Yellow-brown Phenazopyridine - Orange/yellow Phenothiazines - Red/Pink Phenytoin - Red/Pink Rifampin - Orange/yellow, Red/Pink Salicylates - Red/Pink Sulfasalazine - Orange/yellow Sulfonamides - Dark / Brown, Yellow-brown 414 NCLEX-RN study guide 100 m Triamterene - Blue or blue green Warfarin - Orange/yellow Herbal remedies: Remember: Avoid the G’s (ginseng, ginger, gingko, garlic) when on anticoagulants. Do not combine with drugs with the same effects Di Huang – Diabetes Mellitus Ma Huang – Weight Loss Echinacea – Immune booster Black Cohosh – Flushing in menopause Blue Cohosh – Uterine tonic Saw Palmetto – BPH Arnica – Post operative bruising Ginger – Anti emetic, anti-inflammatory – Bleeding risk Ginkgo Biloba – Memory enhancement – Bleeding risk Ginseng – Improve mental performance – Bleeding risk Garlic – HPN, cholesterol – Bleeding risk St. John’s wort – Depression, Insomnia Kava – Anxiety, Insomnia Valerian - Insomnia Licorice – Bronchitis, anti-ulcer Ephedra – Colds & flu, weight loss, improve athletic performance Sample calculations: A HCP prescriptions reads phenytoin 0.2 g orally twice daily. The medication label states that each capsule is 100 mg. The RN prepares how many capsule(s) to administer 1 dose? Fill in the blank. Answer: ______ capsules Formula: Ordered dose x quantity Stock on hand = 0.2 g x 1000 mg (1000 mg in 1 g) x 1 capsule 100 mg = 2 capsules 415 NCLEX-RN study guide 100 m A HCP prescription reads potassium chloride 30 mEq to be added to 1000 ml NS and to be administered over 10 hour period. The label on the medication bottle reads 40 mEq/20 ml. the RN prepares how many ml of potassium chloride to administer the correct dose of medication? Fill in the blank. Answer: ______ ml Formula: Ordered dose x quantity Stock on hand = 30 mEq x 20 ml 40 mEq = 15 ml A HCP prescribes 1 unit PRBC to infuse over 4 hours. The unit of blood contains 250 ml. The drop factor is 10 drops/1 ml. The RN prepares to set the flow rate at how many drops per minute? Fill in the blank. Record your answer in the nearest whole number. Answer: ______ drops/min Formula: Volume (ml) x drop factor (drops/ml) Duration x 60 mins/hr. 250 (ml) x 10 drop factor (drops/ml) 4 hours x 60 mins/hr. = 2500 240 = 10.42 drops/min = 10 drops/min (nearest whole number) 416 NCLEX-RN study guide 100 m Give Nitroprusside 5 mcg/kg/min via continuous infusion for a patient weighing 205 lbs. Nitroprusside is available in a solution of 200 mg in 250 ml D5W. What rate on the infusion pump will deliver the correct dose? Record answer using 1 decimal place. Answer: ______ ml/hour Formula: Ordered dose (mcg/kg/min) x Weight (kg) x 60 min/hr x quantity (ml) Stock on hand in mcg (1000 mcg=1mg) Convert lbs. to kg = 202 lbs. / 2.2 = 93.18 kg = 5 mcg/kg/min x 93.18 kg x 60 min/hr x 250 ml 200,000 mcg (200 mg x 1000) = 34. 9 ml/hour A health care provider prescribes regular insulin, 8 units/hour by continuous intravenous (IV) infusion. The pharmacy prepares the medication and then delivers an IV bag labeled 100 units of regular insulin in 100 mL normal saline (NS). An infusion pump must be used to administer the medication. The nurse sets the infusion pump at how many milliliters per hour to deliver 8 units/hour? Fill in the blank. Answer: ______ ml/hr Formula: Ordered dose (units/hr) x quantity (ml) Stock on hand = 8 units/hr x 100 ml 100 units = 8 ml/hour 417 NCLEX-RN study guide 100 m You have an order to administer heparin sodium IV 1000 units per hour. It is supplied by tour pharmacy as 25,000 units in 250 ml of D5W. How many ml per hour will you set on the infusion pump? Record your answer in the nearest whole number. Answer: ______ ml/hr Formula: Ordered dose x quantity (ml) Stock on hand = 1,000 units x 250 ml 25,000 units = 10 ml/hour Your patient has an order of heparin SC 2500 units BID. You have on hand heparin 5000 units/ml/. How many ml will you administer? Record your answer using 1 decimal place. Answer: ______ ml Formula: Ordered dose x quantity (ml) Stock on hand = 2,500 units x 1 ml 5,000 units = 0.5 ml HCP orders 10 mcg/kg/min of Dopamine infusion. The patient weighs 170 lbs. Dopamine is supplied as 500 mg/500 ml. How many ml/hr will you administer? Record your answer using 1 decimal place. Answer: ________ ml/hr 418 NCLEX-RN study guide 100 m Formula: Ordered dose (mcg/kg/min) x Weight (kg) x 60 min/hr x quantity (ml) Stock on hand in mcg (1000 mcg=1mg) Convert lbs. to kg = 170 lbs. / 2.2 = 77.27 kg = 10 mcg/kg/min x 77.27 kg x 60 min/hr x 250 ml 500,000 mcg (500 mg x 1000) = 46.362 ml/hour = 46.4 ml/hour (1 decimal place) You have an order to run epinephrine at 10 mcg/min. You have a solution of 3 mg in 250 ml fluid. What rate you will set for your IV pump? Record your answer using 1 decimal place. Answer: _______ ml/hr Formula: Ordered dose (mcg/min) x 60 min/hr x quantity (ml) Stock on hand in mcg (1000 mcg=1mg) = 10 mcg/min x 60 min/hr x 250 ml 3,000 mcg (3 mg x 1000) = 0.5 ml/hour 419 NCLEX-RN study guide 100 m 6 The Day On the day of exam make sure you avoid the things that you think might affect your performance. You have spent a lot of hours and sacrifices to achieve your goals, only to be beaten by things you can easily avoid. For instance, anxiety might be a reason to lose what you have mastered. A day before the exam you must have turned your worry into confidence. Following are the habits on your way to success. 1. Get plenty of sleep not only a night before the exam but starting from the days ahead before the exam. Hydrate adequately. 2. Avoid distractions the day before exam. You may have some relaxation activities. 3. Don’t isolate yourself, get out of your room and have some light exercise 4. Don’t cram, but you need to calibrate your level of confidence, too much is dangerous. 5. Plan to dress comfortably 6. Plan to arrive at least 30 minutes early in your testing center. If the Test Center is in a busy district, you may come visit days ahead of the exam. 7. Take along with you a high-energy snack, a chocolate bar for instance. 8. Try not to focus on the length of your exam. Your goal is passing at 75 items but it might be a little longer. That is where your good sleep a night before will take its job. 9. Plan something fun to do after the exam. You’ll need at least a reward after a series of hard work on studying. 10. Above all, don’t forget to put your faith into action. Pray hard, claim your success and give back the glory. 420 NCLEX-RN study guide 100 m 7 Destination RN Absolutely it is OK to be anxious at this moment of waiting for the result. This might be the longest 48 hours of your life waiting for the quick results. If you are to inflict more anxiety to yourself then wait for 6 weeks for NCSBN to release your result. Then came the SUCCESS. Passing NCLEX® is not easy, it is a culmination of hardwork and a result of free will to welcome a future made by the Almighty. Get going, get it and be a NURSE. Created by: Jay Padong, RN, USRN Powered By: IPASS International Nursing Exams Processing 421