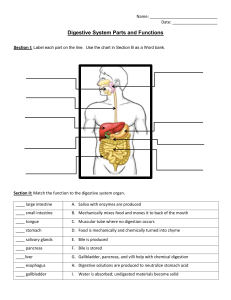
DISEASES OF THE GALLBLADDER ANATOMY Anatomy – Gallbladder ❖ The gallbladder is a pear-shaped sac, about 7-10 cm long. ❖ The average capacity of the gallbladder is 30-50 mL. ➢ When obstructed, the gallbladder can distend markedly and contain up to 300 mL. ❖ The gallbladder is located in a fossa on the inferior surface of the liver. ➢ A line from this fossa to the inferior vena cava divides the liver into right and left liver lobes (Cantlie line). ❖ The gallbladder is divided into four anatomic areas: ➢ Fundus, ➢ Corpus (body), ➢ Infundibulum, ➢ Neck. ❖ The fundus is the rounded, blind end that normally extends 1-2 cm beyond the liver's margin. ➢ It contains most of the smooth muscles of the organ. ❖ The body extends from the fundus and tapers into the neck, a funnel-shaped area that connects with the cystic duct. ➢ It is the main storage area and contains most of the elastic tissue. ❖ The neck usually follows a gentle curve, the convexity of which may be enlarged to form the infundibulum or Hartmann's pouch. ❖ The neck lies in the deepest part of the gallbladder fossa and extends into the free portion of the hepatoduodenal ligament. ❖ The same peritoneal lining that covers the liver covers the fundus and the inferior surface of the gallbladder. ❖ The gallbladder is lined by a single, highly folded, tall columnar epithelium that contains cholesterol and fat globules. ❖ The epithelial lining of the gallbladder is supported by a lamina propria. ❖ The muscle layer has circular longitudinal and oblique fibers, but without well-developed layers. ❖ The perimuscular subserosa contains connective tissue, nerves, vessels, lymphatics, and adipocytes. ❖ The subserosa is covered by the serosa except where the gallbladder is embedded in the liver. ❖ The gallbladder differs histologically from the rest of the GI tract in that it lacks a muscularis mucosa and submucosa. ❖ The cystic artery that supplies the gallbladder is usually a branch of the right hepatic artery (>90%). ➢ The course of the cystic artery may vary, but it nearly always is found within the hepatocystic triangle, the area bound by the cystic duct, common hepatic duct, and the liver margin (triangle of Calot). ➢ When the cystic artery reaches the neck of the gallbladder, it divides into anterior and posterior divisions. ❖ Venous return is carried either through small veins that enter directly into the liver or, rarely, to a large cystic vein that carries blood back to the portal vein. ❖ Gallbladder lymphatics drain into nodes at the neck of the gallbladder. ➢ Frequently, a visible lymph node overlies the insertion of the cystic artery into the gallbladder wall (Mascagni’s lymph node). ❖ The nerves of the gallbladder arise from the vagus and from sympathetic branches that pass through the celiac plexus. ❖ Anatomy – Bile Ducts ❖ The extrahepatic bile ducts consist of; ➢ Right and left hepatic ducts, ➢ Common hepatic duct, ➢ Cystic duct, ➢ Common bile duct (choledochus). ❖ The common bile duct (choledochus) enters the second portion of the duodenum through a muscular structure, the sphincter of Oddi. ❖ The left hepatic duct is longer than the right hepatic duct and has a greater tendency for dilatation as a consequence of distal obstruction. ❖ The two ducts join to form a common hepatic duct, close to their emergence from the liver. ➢ The common hepatic duct is 1-4 cm in length and has a diameter of approximately 4 mm. ➢ It lies in front of the portal vein and to the right of the hepatic artery. Anatomy – Bile Ducts ❖ The common hepatic duct is joined at an acute angle by the cystic duct to form the common bile duct. ❖ The length of the cystic duct is quite variable. ➢ It may be short or absent and have a high union with the hepatic duct, or long and run parallel, behind, or spiral to the main hepatic duct before joining it, sometimes as far as at the duodenum. ➢ Variations of the cystic duct and its point of union with the common hepatic duct are surgically important. ❖ The segment of the cystic duct adjacent to the gallbladder neck bears a variable number of mucosal folds called the spiral valves of Heister. ➢ They do not have any valvular function but may make cannulation of the cystic duct difficult. ❖ Variations of the cystic duct anatomy. 1. Low junction between the cystic duct and common hepatic duct. 2. Cystic duct adherent to the common hepatic duct. 3. High junction between the cystic and the common hepatic duct. 4. Cystic duct drains into right hepatic duct. 5. Long cystic duct that joins common hepatic duct behind the duodenum. 6. Absence of cystic duct. 7. Cystic duct crosses posterior to common hepatic duct and joins it anteriorly. 8. Cystic duct courses anterior to common hepatic duct and joins it posteriorly. ❖ The union of the common bile duct and the main pancreatic duct follows one of three configurations; ➢ 70% � The ducts unite outside the duodenal wall and traverse the duodenal wall as a single duct. ➢ 20% � The ducts join within the duodenal wall and have a short or no common duct, but open through the same opening into the duodenum. ➢ 10% � The ducts exit via separate openings into the duodenum. ❖ The sphincter of Oddi, a thick coat of circular smooth muscle, surrounds the common bile duct at the ampulla of Vater. ➢ It controls the flow of bile, and in some cases pancreatic juice, into the duodenum. ❖ The arterial supply to the bile ducts is derived from the gastroduodenal artery and the right hepatic artery, with major trunks running along the medial and lateral walls of the common duct (sometimes referred to as 3 o'clock and 9 o'clock). ■ These arteries anastomose freely within the duct walls. The density of nerve fibers and ganglia increase near the sphincter of Oddi, but the nerve supply to the duct and the sphincter of Oddi is the same as for the gallbladder. common bile Anatomy – Anomalies ❖ The gallbladder may have abnormal positions; be intrahepatic, be rudimentary, have anomalous forms, or be duplicated. ❖ Isolated congenital absence of the gallbladder is very rare, with a reported incidence of 0.03%. ➢ Before the diagnosis is made, the presence of an intrahepatic bladder or anomalous position must be ruled out. ❖ Duplication of the gallbladder with two separate cavities and two separate cystic ducts has an incidence of 1:4000. ❖ A left-sided gallbladder with a cystic duct emptying into the left hepatic duct or the common bile duct and a retrodisplacement of the gallbladder are both extremely rare. ❖ A partial or totally intrahepatic gallbladder is associated with an increased incidence of cholelithiasis. ❖ Small ducts (of Luschka) may drain directly from the liver into the body of the gallbladder. ➢ If present, but not recognized at the time of a cholecystectomy, a bile leak with the accumulation of bile (biloma) may occur in the abdomen. ❖ An accessory right hepatic duct occurs in about 5% of cases. ❖ Anomalies of the hepatic artery and the cystic artery are quite common (50%). ❖ In about 5% of cases, there are two right hepatic arteries, one from the common hepatic artery and the other from the superior mesenteric artery. ❖ In about 20% of patients, the right hepatic artery comes off the superior mesenteric artery. ❖ The right hepatic artery may course anterior to the common duct. ❖ The right hepatic artery may be vulnerable during surgical procedures, in particular when it runs parallel to the cystic duct or in the mesentery of the gallbladder. ❖ The cystic artery arises from the right hepatic artery in about 90% of cases. ➢ The cystic artey may arise from the left hepatic, common hepatic, gastroduodenal, or superior mesenteric arteries (10%). PHYSIOLOGY Bile Formation and Composition ❖ The liver produces bile continuously and excretes it into the bile canaliculi. ❖ Bile production within the liver of a normal adult consuming an average diet: 500-1000 mL / day ❖ The secretion of bile is responsive to neurogenic, humoral, and chemical stimuli. ❖ Vagal stimulation increases secretion of bile. ❖ Splanchnic nerve stimulation results in decreased bile flow. ❖ Hydrochloric acid, partly digested proteins, and fatty acids in the duodenum stimulate the release of secretin from the duodenum that, in turn, increases bile production and bile flow. ❖ Bile flows from the liver through the hepatic ducts, into the common hepatic duct, through the common bile duct, and finally into the duodenum. ❖ With an intact sphincter of Oddi, bile flow is directed into the gallbladder. ❖ Bile is mainly composed of; ➢ Water, ➢ Electrolytes, ➢ Bile salts, ➢ Proteins, ➢ Lipids, ➢ Bile pigments. ❖ Sodium, potassium, calcium, and chlorine have the same concentration in bile as in plasma or extracellular fluid. ❖ The pH of hepatic bile is usually neutral or slightly alkaline. ➢ This pH varies with diet; an increase in protein shifts the bile to a more acidic pH. ❖ Primary bile salts ➢ Cholate ➢ Chenodeoxycholate ❖ Secondary bile salts ➢ Deoxycholate ➢ Lithocholate ➢ Cholesterol and phospholipids synthesized in the liver are the principal lipids found in bile. ➢ The synthesis of phospholipids and cholesterol by the liver is, in part, regulated by bile acids. ➢ The color of the bile is due to the presence of the pigment bilirubin diglucuronide, which is the metabolic product from the breakdown of hemoglobin, and is present in bile in concentrations 100 times greater than in plasma. ➢ Once in the intestine, bacteria convert it into urobilinogen, a small fraction of which is absorbed and secreted into the bile. Sphincter of Oddi ❖ The sphincter of Oddi; ➢ Regulates flow of bile (and pancreatic juice) into the duodenum, ➢ Prevents the regurgitation of duodenal contents into the biliary tree, ➢ Diverts bile into the gallbladder. ➢ It is a complex structure that is functionally independent from the duodenal musculature and creates a high-pressure zone between the bile duct and the duodenum. ➢ The sphincter of Oddi is about 4-6 mm in length. ➢ The sphincter of Oddi has a basal resting pressure of about 13 mmHg above the duodenal pressure. ➢ Relaxation occurs with a rise in CCK, leading to reduced basal pressure, allowing increased flow of bile into the duodenum. The effect of cholecystokinin on the gallbladder and the sphincter of Oddi. ❖ A. During fasting, with the sphincter of Oddi contracted and the gallbladder filling. ❖ B. In response to a meal, the sphincter of Oddi relaxed and the gallbladder emptying. DIAGNOSTIC STUDIES Blood Tests ❖ When patients with suspected diseases of the gallbladder or the extrahepatic biliary tree are evaluated, a complete blood count and liver function tests are routinely requested. ❖ An elevated white blood cell (WBC) count may indicate or raise suspicion of cholecystitis. ❖ If an elevated WBC count is associated with an elevation of bilirubin, alkaline phosphatase, and aminotransferase, cholangitis should be suspected. ❖ Cholestasis, an obstruction to bile flow, is characterized by an elevation of bilirubin (i.e., the conjugated form), and a rise in alkaline phosphatase. ➢ Serum aminotransferases may be normal or mildly elevated. ❖ In patients with biliary colic or chronic cholecystitis, blood tests will typically be normal. Ultrasonography ❖ An ultrasound is the initial investigation of any patient suspected of disease of the biliary tree. ➢ Noninvasive, ➢ Painless, ➢ Does not submit the patient to radiation, ➢ Can be performed on critically ill patients. ❖ It is dependent upon the skills and the experience of the operator. ❖ Adjacent organs can frequently be examined at the same time. ❖ Conditions that may be difficult to examine satisfactorily with an ultrasound: ➢ Obese patients, ➢ Patients with ascites, ➢ Patients with distended bowel. ❖ Ultrasound will show stones in the gallbladder with sensitivity and specificity of >90%. ❖ Stones are acoustically dense and reflect the ultrasound waves back to the ultrasonic transducer. ❖ they also produce an acoustic shadow. ❖ Stones move with changes in position. ❖ Polyps may be calcified and reflect shadows, but do not move with change in posture. ❖ Some stones form a layer in the gallbladder; others a sediment or sludge. ❖ A thickened gallbladder wall and local tenderness indicate cholecystitis. ❖ The patient has acute cholecystitis if a layer of edema is seen within the wall of the gallbladder or between the gallbladder and the liver in association with localized tenderness. ❖ When a stone obstructs the neck of the gallbladder, the gallbladder may become very large, but thin walled. ❖ A contracted, thick-walled gallbladder is indicative of chronic cholecystitis. An ultrasonography of the gallbladder. Arrows indicate the acoustic shadows from stones in the gallbladder. ❖ The extrahepatic bile ducts are also well visualized by ultrasound, except for the retroduodenal portion. ❖ Dilation of the ducts in a patient with jaundice establishes an extrahepatic obstruction as a cause for the jaundice. ❖ Frequently, the site and, sometimes, the cause of obstruction can be determined by ultrasound. ❖ Small stones in the common bile duct frequently get lodged at the distal end of it, behind the duodenum, and are, therefore, difficult to detect. ❖ A dilated common bile duct on ultrasound, small stones in the gallbladder, and the clinical presentation allow one to assume that a stone or stones are causing the obstruction. ❖ Periampullary tumors can be difficult to diagnose on ultrasound, but beyond the retroduodenal portion, the level of obstruction and the cause may be visualized quite well. ❖ Ultrasound can be helpful in evaluating tumor invasion and flow in the portal vein, an important guideline for resectability of periampullary and pancreatic head tumors. Oral Cholecystography ❖ Once considered the diagnostic procedure of choice for gallstones, oral cholecystography has largely been replaced by ultrasonography. ❖ It involves oral administration of a radiopaque compound that is absorbed, excreted by the liver, and passed into the gallbladder. ❖ Stones are noted on a film as filling defects in a visualized, opacified gallbladder. ❖ Oral cholecystography is of no value in patients with; ➢ intestinal malabsorption, ➢ vomiting, ➢ obstructive jaundice, ➢ hepatic failure. Computed Tomography ❖ Abdominal CT scans are inferior to ultrasonography in diagnosing gallstones. ❖ The major application of CT scans is to define the course and status of the extrahepatic biliary tree and adjacent structures. ❖ It is the test of choice in evaluating the patient with suspected malignancy of the; ➢ gallbladder, ➢ the extrahepatic biliary system, ➢ nearby organs, in particular, the head of the pancreas. ❖ Use of CT scan is an integral part of the differential diagnosis of obstructive jaundice. ❖ Spiral CT scanning provides additional staging information, including vascular involvement in patients with periampullary tumors. Percutaneous Transhepatic Cholangiography ❖ Intrahepatic bile ducts are accessed percutaneously with a small needle under fluoroscopic guidance. ❖ Once the position in a bile duct has been confirmed, a guidewire is passed and, subsequently, a catheter is passed over the wire. ❖ Through the catheter, a cholangiogram can be performed and therapeutic interventions done, such as biliary drain insertions and stent placements. ❖ Percutaneous transhepatic cholangiography (PTC) has little role in the management of patients with uncomplicated gallstone disease. ❖ PTC is particularly useful in patients with bile duct strictures and tumors, as it defines the anatomy of the biliary tree proximal to the affected segment. ❖ As with any invasive procedure, there are potential risks of PTC; ➢ Bleeding, ➢ Cholangitis, ➢ Bile leak, ➢ Other catheter-related problems. Magnetic Resonance Imaging (MRI) ❖ Available since the mid-1990s, MRI provides anatomic details of the liver, gallbladder, and pancreas similar to those obtained from CT. ❖ Many MRI techniques (i.e., heavily T2-weighted sequences, pulse sequences with or without contrast materials) can generate high resolution anatomic images of the biliary tree and the pancreatic duct. ❖ Choledocholithiasis � Sensitivity: 95% / Specificity: 89% ❖ MRI with magnetic resonance cholangiopancreatography (MRCP) offers a single noninvasive test for the diagnosis of biliary tract and pancreatic disease. Magnetic This view extrahepatic bile pancreatic duct (arrowheads). resonance shows cholangiopancreatography the ducts course (arrow) of and the the ERCP(Endoscopic Retrograde Cholangiopancreatography) ❖ Using a side-viewing endoscope, the common bile duct can be cannulated and a cholangiogram performed using fluoroscopy. ❖ The procedure requires IV sedation for the patient. ❖ The advantages of ERCP include direct visualization of the ampullary region and direct access to the distal common bile duct, with the possibility of therapeutic intervention. ❖ The test is rarely needed for uncomplicated gallstone disease. ❖ For stones in the common bile duct, in particular, when associated with obstructive jaundice, cholangitis, or gallstone pancreatitis, ERCP is the diagnostic and often therapeutic procedure of choice. ❖ Once the endoscopic cholangiogram has shown ductal stones, sphincterotomy and stone extraction can be performed, and the common bile duct cleared of stones. ❖ In the hands of experts, the success rate of common bile duct cannulation and cholangiography is >90%. ❖ Complications of diagnostic ERCP include pancreatitis and cholangitis, and occur in up to 5% of patients. ERCP A. A schematic picture showing the side-viewing endoscope in the duodenum and a catheter in the common bile duct. B. An endoscopic cholangiography showing stones in the common bile duct. Endoscopic Ultrasound ❖ An endoscopic ultrasound requires a special endoscope with an ultrasound transducer at its tip. ❖ The results are operator dependent, but offer noninvasive imaging of the bile ducts and adjacent structures. ❖ It is of particular value in the evaluation of tumors and their resectability. ❖ The ultrasound endoscope has a biopsy channel, allowing needle biopsies of a tumor under ultrasonic guidance. ❖ Endoscopic ultrasound also has been used to identify bile duct stones, and although it is less sensitive than ERCP, the technique is less invasive. GALLSTONE DISEASE Prevalence and Incidence ❖ ❖ ❖ ❖ ❖ ❖ Gallstone disease is one of the most common problems affecting the digestive tract. Autopsy reports � prevalence of gallstones: 11-36% The prevalence of gallstones is related to many factors, including age, gender, and ethnic background. Women are 3 times more likely to develop gallstones than men First-degree relatives of patients with gallstones have a 2 fold greater prevalence. Certain conditions predispose to the development of gallstones; ➢ Obesity, ➢ Pregnancy, ➢ Dietary factors, ➢ Crohn's disease, ➢ Terminal ileal resection, ➢ Gastric surgery, ➢ Hereditary spherocytosis, ➢ Sickle cell disease, ➢ Thalassemia. Natural History ❖ Most patients will remain asymptomatic from their gallstones throughout life. ❖ For unknown reasons, some patients progress to a symptomatic stage, with biliary colic caused by a stone obstructing the cystic duct. ❖ Symptomatic gallstone disease may progress to complications related to the gallstones; ➢ Acute cholecystitis, ➢ Choledocholithiasis (with or without cholangitis), ➢ Gallstone pancreatitis, ➢ Cholecystocholedochal fistula, ➢ Cholecystoduodenal or cholecystoenteric fistula leading to gallstone ileus, ➢ Gallbladder carcinoma. ❖ Rarely, complication of gallstones is the presenting picture. ❖ Because few patients develop complications without previous biliary symptoms, prophylactic cholecystectomy in asymptomatic persons with gallstones is rarely indicated. ❖ A prophylactic cholecystectomy may be advisable; ➢ For elderly patients with diabetes, ➢ For individuals who will be isolated from medical care for extended periods of time, ➢ In populations with increased risk of gallbladder cancer. ❖ Absolute indication for cholecystectomy: ➢ Porcelain gallbladder ■ A rare premalignant condition in which the wall of the gallbladder becomes calcified. Gallstone Formation ❖ Gallstones form as a result of solids settling out of solution. ➢ The major organic solutes in bile are bilirubin, bile salts, phospholipids, and cholesterol. ❖ Gallstones are classified by their cholesterol content as; ➢ Cholesterol stones ➢ Pigment stones ■ Black pigment stones ■ Brown pigment stones ❖ In Western countries; ➢ 80% of gallstones are cholesterol stones, ➢ 15-20% are black pigment stones, ➢ Brown pigment stones account for only a small percentage. ❖ Both types of pigment stones are more common in Asia. Cholesterol stones ❖ Pure cholesterol stones are uncommon and account for <10% of all stones. ➢ They usually occur as single large stones with smooth surfaces. ❖ Most other cholesterol stones contain variable amounts of bile pigments and calcium, but are always >70% cholesterol by weight. ➢ These stones are usually multiple, of variable size, and may be hard and faceted or irregular, mulberryshaped, and soft. ❖ Colors range from whitish yellow and green to black. ❖ Most cholesterol stones are radiolucent. ❖ <10% cholesterol stones are radiopaque. Pigment stones ❖ Pigment stones contain <20% cholesterol and are dark because of the presence of calcium bilirubinate. Black pigment stones ❖ Black pigment stones are usually small, brittle, black, and sometimes spiculated. ❖ They are formed by supersaturation of calcium bilirubinate, carbonate, and phosphate, most often secondary to; ➢ hemolytic disorders such as; ■ hereditary spherocytosis, ■ sickle cell disease, ➢ cirrhosis. ❖ Like cholesterol stones, they almost always form in the gallbladder.. Brown pigment stones ❖ Brown stones are usually <1 cm in diameter, brownish-yellow, soft, and often mushy. ❖ They may form either in the gallbladder or in the bile ducts, usually secondary to bacterial infection caused by bile stasis. ❖ Precipitated calcium bilirubinate and bacterial cell bodies compose the major part of the stone. ❖ Bacteria such as Escherichia coli secrete β-glucuronidase that enzymatically splits up bilirubin glucuronide to produce the insoluble unconjugated bilirubin. ❖ It precipitates with calcium, and along with dead bacterial cell bodies, forms soft brown stones in the biliary tree. ❖ Brown stones are typically found in the biliary tree of Asian populations and are associated with stasis secondary to parasite infection. SYMPTOMATIC GALLSTONES CHRONIC (Biliary colic) CHOLECYSTITITS ❖ About 2/3 of patients with gallstone disease present with chronic cholecystitis characterized by recurrent attacks of pain, often inaccurately labeled biliary colic. ❖ The pain develops when a stone obstructs the cystic duct, resulting in a progressive increase of tension in the gallbladder wall. ❖ The pathologic changes, which often do not correlate well with symptoms, vary between; ➢ An apparently normal gallbladder with minor chronic inflammation in the mucosa, ➢ A shrunken, nonfunctioning gallbladder with gross transmural fibrosis and adhesions to nearby structures. Chronic Cholecystitis Clinical Presentation ❖ The chief symptom associated with symptomatic gallstones is pain. ❖ The pain is constant and increases in severity over the first half hour or so and typically lasts 1-5 hours. ❖ It is located in the epigastrium or right upper quadrant and frequently radiates to the right upper back or between the scapulae. ❖ The pain is severe and comes on suddenly, typically during the night or after a fatty meal. ❖ It often is associated with nausea and sometimes vomiting. ❖ The pain is episodic. ➢ The patient suffers discrete attacks of pain, between which they feel well. ❖ Physical examination may reveal mild right upper quadrant tenderness during an episode of pain. ➢ If the patient is pain free, the physical examination is usually unremarkable. ❖ Laboratory values, such as WBC count and liver function tests, are usually normal in patients with uncomplicated gallstones. ❖ In patients with atypical presentation, other conditions with upper abdominal pain should be sought out, even in the presence of gallstones. These include; ➢ Peptic ulcer disease, ➢ Gastroesophageal reflux disease, ➢ Abdominal wall hernias, ➢ Irritable bowel disease, ➢ Diverticular disease, ➢ Liver diseases, ➢ Renal calculi, ➢ Pleuritic pain, ➢ Myocardial pain. ❖ Many patients with other conditions have gallstones… ❖ When the pain lasts >24 hours � an impacted stone in the cystic duct or acute cholecystitis should be suspected. ❖ An impacted stone without cholecystitis will result in what is called hydrops of the gallbladder. ❖ The bile gets absorbed, but the gallbladder epithelium continues to secrete mucus, and the gallbladder becomes distended with mucinous material. ❖ The gallbladder may be palpable but usually is not tender. ❖ Hydrops of the gallbladder may result in edema of the gallbladder wall, inflammation, infection, and perforation. ❖ Although hydrops may persist with few consequences, early cholecystectomy is generally indicated to avoid complications. diagnosis ❖ The diagnosis of symptomatic gallstones or chronic calculous cholecystitis depends on the presence of typical symptoms and the demonstration of stones on diagnostic imaging. ❖ An abdominal ultrasound is the standard diagnostic test for gallstones. ❖ Gallstones are occasionally identified on abdominal radiographs or CT scans. ➢ In these cases, if the patient has typical symptoms, an ultrasound of the gallbladder and the biliary tree should be added before surgical intervention. ❖ Stones diagnosed incidentally in patients without symptoms should be left in place. ❖ Occasionally, patients with typical attacks of biliary pain have no evidence of stones on ultrasonography. ➢ Sometimes only sludge in the gallbladder is demonstrated on ultrasonography. ➢ If the patient has recurrent attacks of typical biliary pain and sludge is detected on >2 occasions, cholecystectomy is warranted. management ❖ Patients with symptomatic gallstones should be advised to have elective laparoscopic cholecystectomy. ➢ While waiting for surgery, or if surgery has to be postponed, the patient should be advised to avoid dietary fats and large meals. ❖ Diabetic patients with symptomatic gallstones should have a cholecystectomy promptly, as they are more prone to develop acute cholecystitis that is often severe. ❖ Pregnant women with symptomatic gallstones who cannot be managed expectantly with diet modifications can safely undergo laparoscopic cholecystectomy during the second trimester. ❖ Laparoscopic cholecystectomy is safe and effective in children as well as in the elderly. ❖ Cholecystectomy, open or laparoscopic, for patients with symptomatic gallstones offers excellent long-term results. Acute cholecystitis pathogenesis Acute cholecystitis is secondary to gallstones in 90-95% of cases. ❖ Acute acalculous cholecystitis is a condition that typically occurs in patients with other acute systemic diseases. ❖ In <1% of acute cholecystitis, the cause is a tumor obstructing the cystic duct. ❖ Obstruction of the cystic duct by a gallstone is the initiating event that leads to; ➢ gallbladder distention, ➢ inflammation, ➢ edema of the gallbladder wall. ❖ Secondary bacterial contamination is documented in 15-30% of patients undergoing cholecystectomy for acute uncomplicated cholecystitis. ❖ In acute cholecystitis; ➢ The gallbladder wall becomes grossly thickened and reddish with subserosal hemorrhages, ➢ Pericholecystic fluid often is present, ➢ The mucosa may show hyperemia and patchy necrosis. ❖ In severe cases, the inflammatory process progresses and leads to ischemia and necrosis of the gallbladder wall (5-10%). ❖ Acute gangrenous cholecystitis: When the gallbladder remains obstructed and secondary bacterial infection supervenes an abscess or empyema forms within the gallbladder. ➢ Rarely, perforation of ischemic areas occurs. ■ The perforation is usually contained in the subhepatic space by the omentum and adjacent organs. ■ Free perforation � peritonitis, ■ Intrahepatic perforation � intrahepatic abscesses, ■ Perforation into adjacent organs (duodenum or colon) � cholecystoenteric fistula ❖ Emphysematous gallbladder: When gas-forming organisms are part of the secondary bacterial infection, gas may be seen in the gallbladder lumen and in the wall of the gallbladder on abdominal radiographs and CT scans. clinical manifestations ❖ About 80% of patients with acute cholecystitis give a history compatible with chronic cholecystitis. ❖ Acute cholecystitis begins as an attack of biliary colic; ➢ In contrast to biliary colic, the pain does not subside; it is unremitting and may persist for several days. ➢ The pain is typically in the right upper quadrant or epigastrium, and may radiate to the right upper part of the back or the interscapular area. ➢ It is usually more severe than the pain associated with uncomplicated biliary colic. ❖ The patient is often febrile, complains of anorexia, nausea, and vomiting, and is unwilling to move, as the inflammatory process affects the parietal peritoneum. ❖ On physical examination, focal tenderness and guarding are usually present in the right upper quadrant. ➢ A mass, the gallbladder and adherent omentum, is occasionally palpable; however, guarding may prevent this. ➢ A Murphy's sign, an inspiratory arrest with deep palpation in the right subcostal area, is characteristic of acute cholecystitis. ❖ A mild to moderate leukocytosis (WBC: 12,000-15,000/mm3) is usually present. ➢ However, some patients may have a normal WBC. ❖ A high WBC (>20,000/mm3) is suggestive of a complicated form of cholecystitis such as; ➢ Gangrenous cholecystitis, ➢ Perforation, ➢ Associated cholangitis. ❖ Serum liver chemistries are usually normal, but a mild elevation of certain parameters may be present; ➢ Serum bilirubin (T. Bil. < 4 mg/mL), ➢ Alkaline phosphatase (ALP), ➢ Transaminases (AST, ALT), ➢ Amylase (Amy). ❖ Severe jaundice is suggestive of; ➢ Common bile duct stones, ➢ Obstruction of the bile ducts by severe pericholecystic inflammation secondary to impaction of a stone in the infundibulum of the gallbladder that mechanically obstructs the bile duct (Mirizzi's syndrome). ❖ In elderly patients and in those with diabetes mellitus, acute cholecystitis may have a subtle presentation resulting in a delay in diagnosis. ❖ The differential diagnosis for acute cholecystitis includes; ➢ A peptic ulcer with or without perforation, ➢ Pancreatitis, ➢ Appendicitis, ➢ Hepatitis, ➢ Perihepatitis (Fitz-Hugh–Curtis syndrome), ➢ Myocardial ischemia, ➢ Pneumonia, ➢ Pleuritis, ➢ Herpes zoster involving the intercostal nerve. ❖ Ultrasonography is the most useful radiologic test for diagnosing acute cholecystitis. ➢ It has a sensitivity and specificity of 95% for showing; ■ The presence or absence of stones, ■ Thickening of the gallbladder wall ■ Pericholecystic fluid. ➢ Focal tenderness over the gallbladder when compressed by the sonographic probe (sonographic Murphy's sign) also is suggestive of acute cholecystitis. ❖ CT scan is frequently performed on patients with acute abdominal pain. ➢ It demonstrates thickening of the gallbladder wall, pericholecystic fluid, and the presence of gallstones as well as air in the gallbladder wall, but is less sensitive than ultrasonography. Treatment ❖ Patients who present with acute cholecystitis will need; ➢ IV fluids, ➢ Antibiotics, ➢ Analgesia. ❖ The antibiotics should cover gram-negative aerobes as well as anaerobes. ➢ Third-generation cephalosporin with good anaerobic coverage ➢ Second generation cephalosporin combined with metronidazole ➢ Aminoglycoside with metronidazole (for patients with allergies to cephalosporins) ❖ Although the inflammation in acute cholecystitis may be sterile in some patients, more than 50% will have positive cultures from the gallbladder bile. ❖ It is difficult to know who is secondarily infected; therefore, antibiotics have become a part of the management in most medical centers. ❖ Cholecystectomy is the definitive treatment for acute cholecystitis. ❖ In the past, the timing of cholecystectomy has been a matter of debate. ❖ Early cholecystectomy performed within 2-3 days of the illness ➢ is preferred over ❖ interval or delayed cholecystectomy that is performed 6-10 weeks after ❖ initial medical treatment and recovery. ❖ Several studies have shown that unless the patient is unfit for surgery, early cholecystectomy should be recommended, as it offers the patient; ➢ A definitive solution in one hospital admission, ➢ Quicker recovery times, ➢ Earlier return to work. ❖ Laparoscopic cholecystectomy is the procedure of choice for acute cholecystitis. ❖ The conversion rate to an open cholecystectomy is higher (10-15%) in the setting of acute cholecystitis than with chronic cholecystitis. ❖ The procedure is harder and takes longer than in the elective setting. ❖ However, when compared to the delayed operation, early operation carries a similar complication rate. ❖ When patients present late, after 3-4 days of illness, or if they are unfit for surgery, they can be treated with antibiotics with laparoscopic cholecystectomy scheduled for approximately two months later. ❖ Approximately 20% of patients will fail to respond to initial medical therapy and require an intervention. ❖ Laparoscopic cholecystectomy could be attempted, but the conversion rate is high and some prefer to go directly for an open cholecystectomy. ❖ For those unfit for surgery, a percutaneous cholecystostomy or an open cholecystostomy under local analgesia can be performed. ❖ Failure to improve after cholecystostomy usually is due to gangrene of the gallbladder or perforation. ➢ For these patients, surgery is unavoidable. ❖ For those who respond after cholecystostomy, the tube can be removed once cholangiography through it shows a patent ductus cysticus. ❖ Laparoscopic cholecystectomy may then be scheduled in the near future. ❖ For the rare patients who can't tolerate surgery, the stones can be extracted via the cholecystostomy tube before its removal. Acalculous Cholecystitis ❖ Acute inflammation of the gallbladder can occur without gallstones. ❖ Acalculous cholecystitis typically develops in; ➢ Critically ill patients in the intensive care unit, ➢ Patients on parenteral nutrition with extensive burns, ➢ Sepsis, ➢ Major operations, ➢ Multiple trauma, ➢ Prolonged illness with multiple organ system failure. ❖ The cause is unknown, but gallbladder distention with bile stasis and ischemia has been implicated as causative factors. ❖ Pathologic examination of the gallbladder wall reveals; ➢ Edema of the serosa and muscular layers, ➢ Patchy thrombosis of arterioles and venules. ❖ The symptoms and signs depend on the condition of the patient, but in the alert patient, they are similar to acute calculous cholecystitis; ➢ Right upper quadrant pain and tenderness, ➢ Fever, ➢ Leukocytosis. ❖ In the sedated or unconscious patient, the clinical features are often masked, but indications for further investigation include; ➢ Fever, ➢ Elevated WBC count, ➢ Elevation of alkaline phosphatase and bilirubin. ❖ Ultrasonography is usually the diagnostic test of choice, as it can be done bedside in the intensive care unit. It can demonstrate; ➢ Distended gallbladder with thickened wall, ➢ Biliary sludge, ➢ Pericholecystic fluid, ➢ Presence or absence of abscess formation. ❖ Abdominal CT scan can aid in the diagnosis of acalculous cholecystitis and additionally allows imaging of the abdominal cavity and chest to rule out other sources of infection. ❖ Acalculous cholecystitis requires urgent intervention. ❖ Percutaneous ultrasound- or CT-guided cholecystostomy is the treatment of choice for these patients, as they are usually unfit for surgery. ❖ If the diagnosis is uncertain, percutaneous cholecystostomy is both diagnostic and therapeutic. ❖ About 90% of patients will improve with the percutaneous cholecystostomy. ❖ However, if they do not improve, other steps, such as open cholecystostomy or cholecystectomy, may be required. ❖ If needed, cholecystectomy is performed after the patient has recovered from the underlying disease. INTERVENTIONS FOR GALLSTONE DISEASE ❖ Percutaneous cholecystostomy. A pigtail catheter has been placed through the abdominal wall, the right lobe of the liver, and into the gallbladder. ❖ Laparoscopic Cholecystectomy ● A. The trocar placement. ● B. The fundus has been grasped and retracted cephalad to expose the proximal gallbladder and the hepatoduodenal ligament. Another grasper retracts the gallbladder infundibulum posterolaterally to better expose the triangle of Calot (hepatocystic triangle bound by the common hepatic duct, cystic duct, and the liver margin). ❖ Laparoscopic Cholecystectomy E. The cystic duct has been divided, and the cystic artery is being divided. F. An intraoperative picture showing a grasper pulling the infundibulum of the gallbladder laterally, exposing the triangle of Calot that has been dissected. The cystic artery can be seen crossing the dissected area upward and to the left. ❖ Intraoperative cholangiogram showing common A small amount of contrast has passed into the duodenum. ❖ Choledochal Exploration Extraction of the stone with a wire basket. ❖ An endoscopic A. The sphincterotome B. Completed C. Endoscopic completed TUMORS Carcinoma of the Gallbladder bile duct in picture stone (arrow). sphincterotomy. place. sphincterotomy. of sphincterotomy. ❖ Cancer of the gallbladder is a rare malignancy that occurs predominantly in the elderly. ❖ It is an aggressive tumor, with poor prognosis except when incidentally diagnosed at an early stage after cholecystectomy for cholelithiasis. ❖ The overall reported 5-year survival rate is about 5%. Carcinoma of the Gallbladder Incidence ❖ ❖ ❖ ❖ ❖ ❖ Gallbladder cancer is the 5th most common GI malignancy. It accounts for only 2-4% of all malignant GI tumors. Female / male: 2-3 / 1 The peak incidence is in the 7th decade of life. Its occurrence in random autopsy series is about 0.4%. Approximately 1% of patients undergoing cholecystectomy for gallstone disease are found incidentally to have gallbladder cancer. Carcinoma of the Gallbladder Etiology ❖ Cholelithiasis is the most important risk factor for gallbladder carcinoma. ➢ Up to 95% of patients with carcinoma of the gallbladder have gallstones. ■ However, the 20-year risk of developing cancer for patients with gallstones is <0.5% for the overall population and 1.5% for high-risk groups. ➢ The pathogenesis has not been defined but is probably related to chronic inflammation. ➢ Larger stones (>3 cm) are associated with a 10-fold increased risk of cancer. ➢ The risk of developing cancer of the gallbladder is higher in patients with symptomatic than asymptomatic gallstones. ❖ Polypoid lesions of the gallbladder are associated with increased risk of cancer, particularly in polyps >10 mm. ❖ The calcified "porcelain" gallbladder is associated with >20% incidence of gallbladder carcinoma. ❖ Patients with choledochal cysts have an increased risk of developing cancer anywhere in the biliary tree, but the incidence is highest in the gallbladder. ❖ Sclerosing cholangitis, anomalous pancreaticobiliary duct junction, and exposure to carcinogens (azotoluene, nitrosamines) also are associated with cancer of the gallbladder Carcinoma of the Gallbladder Pathology ❖ Gallbladder tumors; ➢ Adenoca (80-90%) ■ Papillary (<10%), ■ Nodular, ■ Tubular. ➢ Squamous cell ca, ➢ Adenosquamous ca, ➢ Oat cell ca, ➢ Anaplastic ca (rare). ❖ The papillary type is associated with an overall better outcome. ➢ They are most commonly diagnosed while localized to the gallbladder. ❖ Cancer of the gallbladder spreads through; ➢ The lymphatics, ➢ Venous drainage, ➢ Direct invasion into the liver parenchyma. Carcinoma of the Gallbladder Daignosis ❖ Signs and symptoms of carcinoma of the gallbladder are generally indistinguishable from those associated with cholecystitis and cholelithiasis; ➢ Abdominal discomfort, ➢ Right upper quadrant pain, ➢ Nausea & vomiting. ❖ Jaundice, weight loss, anorexia, ascites, and abdominal mass are less common presenting symptoms. ❖ >50% of gallbladder cancers are not diagnosed before surgery. ❖ Common misdiagnoses include chronic cholecystitis, acute cholecystitis, choledocholithiasis, hydrops of the gallbladder, and pancreatic cancer. ❖ Laboratory findings are not diagnostic. ➢ If abnormal, are most often consistent with biliary obstruction. ❖ Ultrasonography (US) often reveals a thickened, irregular gallbladder wall or a mass replacing the gallbladder. ➢ US may visualize tumor invasion of the liver, lymphadenopathy, and a dilated biliary tree. ➢ The sensitivity of ultrasonography in detecting gallbladder cancer ranges from 70 to 100%. ❖ A CT scan is an important tool for staging and may identify a gallbladder mass or local invasion into adjacent organs. ➢ In addition, a spiral CT scan can demonstrate vascular invasion, ➢ However, CT scan is a poor method for identifying nodal spread. ❖ In jaundiced patients, a percutaneous transhepatic / endoscopic cholangiogram may be helpful to delineate the extent of biliary tree involvement, and typically shows a long stricture of the common bile duct. ❖ With newer MRI techniques, MRCP has evolved into a single noninvasive imaging method that allows complete assessment of biliary, vascular, nodal, hepatic, and adjacent organ involvement. ❖ If diagnostic studies suggest that the tumor is unresectable, a CT scan or ultrasound-guided biopsy of the tumor can be obtained to provide a pathologic diagnosis. Carcinoma of the Gallbladder Treatment ❖ Surgery remains the only curative option for gallbladder cancer. ❖ However, palliative procedures for patients with unresectable cancer and jaundice or duodenal obstruction remain the most frequently performed surgery for gallbladder cancers. ➢ Patients with obstructive jaundice can frequently be managed with either endoscopic or percutaneously placed biliary stents. ❖ There are no proven effective options for adjuvant radiation or chemotherapy for patients with gallbladder cancer. ❖ The pathologic stage of gallbladder cancer determines the operative treatment for patients with localized gallbladder cancer. ❖ Patients without evidence of distant metastasis warrant exploration for tissue diagnosis, pathologic staging, and possible curative resection. ❖ Tumors limited to the muscular layer of the gallbladder (T1 tumors) are usually identified incidentally, after cholecystectomy for gallstone disease. And it is nearly 100% overall 5-survival rate . ❖ When the tumor invades the perimuscular connective tissue without extension beyond the serosa or into the liver (T2 tumors), an extended cholecystectomy should be performed. ➢ That includes resection of liver segments IVB and V, and lymphadenectomy of the cystic duct, and pericholedochal, portal, right celiac, and posterior pancreatoduodenal lymph nodes. ➢ Regional lymphadenectomy is an important part of surgery for T2 cancers because 1/2 of patients with T2 tumors are found to have nodal disease on pathologic examination. ❖ For tumors that grow beyond the serosa or invade the liver or other organs (T3 and T4 tumors), there is a high likelihood of intraperitoneal and distant spread. ➢ If no peritoneal or nodal involvement is found, complete tumor excision with an extended right hepatectomy (segments IV, V, VI, VII, and VIII) must be performed for adequate tumor clearance. ➢ An aggressive approach in patients who will tolerate surgery has resulted in an increased survival for T3 and T4 lesions. Carcinoma of the Gallbladder Prognosis ❖ ❖ ❖ ❖ Most patients with gallbladder cancer have unresectable disease at the time of diagnosis. The 5-year survival rate of all patients with gallbladder cancer is <5%. Median survival: 6 months. Patients with T1 disease treated with cholecystectomy have an excellent prognosis. ➢ 5-year survival rate: 85-100%. ❖ The 5-year survival rates for T2 lesions treated with; ➢ Extended cholecystectomy and lymphadenectomy � > 70 % ➢ Simple cholecystectomy � 25-40% ❖ Patients with advanced but resectable gallbladder cancer; ➢ 5-year survival rate: 20-50%. ❖ Patients with distant metastasis at the time of presentation; ➢ Median survival: 1-3 months. Thank you…