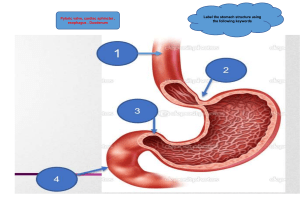
● ● ● ● ● ● ● ● ● Week 7 - Infection READ: Giddens○ CH 23–inflammation ○ CH 24–infection ■ Attributes – characteristics ● Pathogen ○ Mode of transmission ○ Immune response ○ Passageway ○ Susceptible host ■ Immune system READ: Lewis: pages 211-216, 897-909, 968-979 READ: ATI Chapters 49 & 55 REVIEW: Giddens Concept Infection 2020 pptx.pptx REVIEW: Lewis PUD Chapter_41-1-1.pptx REVIEW:Chapter_043_3 Hepatitis-1.pptx REVIEW: Health Promotion of Pre-Schooler Chapter_013.pptx REVIEW:Preschooler+to+School-ager_voice.pptx REVIEW:S390 Growth & Development 4-12 years.pptx; McKinney Chapter_008 HP schoolage 4 ed(1).ppt Apply the concepts of inflammation and infection to the manifestations, management, and expected outcomes of treatment for exemplars such as hepatitis and PUD across the lifespan. 01. Analyze the relationship of inflammation and infection in individuals with hepatitis and PUD. 02. Integrate guideline-based care and education to formulate a plan of care for a patient with hepatitis and PUD. 03. Prioritize clinical interventions, and manage individuals experiencing inflammation and infection. 04. Incorporate measures w/outcomes that reduce complications from the chronic nature of these diseases across the lifespan. 05. Evaluate how hepatitis and PUD affect the cost and quality of healthcare and influence the outcomes, standard/s of care and clinical practice. 06. Critique plans of care created above while justifying relationship between increased levels of prevention, improved healthcare outcomes, and reduced health care cost for individuals with hepatitis and PUD. Risk factors for PUD Why patients come in Bloating Pain after eating Dull annoying pain Urea breath testing Synthesizing prothrombin–prolonged PT/INRs in hepatitis/cirrhotic patients Common labs elevated–ammonia levels Can’t convert ammonia to urea to be excreted so it sits in bodies Similar to hepatitis–most definitave thing to do is liver biopsy Medications are difficult for this pt population Lactulose to excrete ammonia Infection Lewis (p. 211-216) ❖ ❖ ❖ ❖ ❖ ❖ Infection- occurs when a pathogen invades the body, multiplies, and produces disease, usually causing harm to the host. ➢ The signs and symptoms of infection are a result of specific pathogen activity, which triggers inflammation and other immune responses ■ Categorized as: ■ localized- limited to a small area ■ disseminated- spread to areas of the body beyond the initial site of infection ■ systemic- infections have spread extensively throughout the body, often via blood; affect the body as a whole ● signs/symptoms: fever, leukocytosis, malaise, fatigue, increase in plasma proteins pathogen- a microorganism that causes disease ➢ bacteria- one-celled organisms that are common throughout nature ■ “normal flora”--> live harmoniously in or on the human body without causing disease under normal circumstances; Normal flora protect the human body by preventing the overgrowth of other microorganisms ■ How “bad” bacteria cause disease: ● entering the body and growing inside human cells (e.g., TB) ● secreting toxins that damage cells (e.g., Staphylococcus aureus) ■ classification: shape ● cocci-round ● bacilli-rod-shaped ● vibrio-curved rods ● spirochetes-spiral shaped ➢ Viruses- non-cellular structure organisms that contain simple infectious particles consisting of a small amount of genetic material (either ribonucleic acid [RNA] or deoxyribonucleic acid [DNA]) and a protein envelope ■ reproduce only after releasing their genetic material into the cell of another living organism ➢ Fungi- organisms similar to plants but lack chlorophyll ■ Mycosis- any disease caused by a fungus ● Tinea pedis (athlete’s foot) and tinea corporis (ringworm) are common ■ infections are usually localized; can become disseminated in an immunocompromised person ➢ Protozoa- single-cell, animal-like microorganisms that normally live in soil and bodies of water; cause infection when introduced into the human body ➢ Prions- infectious particles that have abnormally shaped proteins that typically affect the nervous system ■ can cause a group of illnesses called transmissible spongiform encephalopathies (TSEs) ● i.e Creutzfeldt-Jakob disease and bovine spongiform encephalopathy in cattle ■ not all prions cause disease Emerging infection- infectious disease that has recently increased in incidence or that threatens to increase in the immediate future. ➢ can originate from unknown sources or from contact with animals, changes in known diseases, or biologic warfare ➢ i.e ebola virus can come from animal sources but can emerge when a previously treatable organism developed resistance to antibiotics Reemerging Infections- infective agents reemerge under right conditions Antimicrobial-Resistant Organisms ➢ Resistance: occurs when pathogenic organisms change in ways that decrease the ability of a drug (or a family of drugs) to treat disease ➢ emerging strains of of antibiotic-resistant organism ■ Methicillin-resistant S. aureus (MRSA) ■ vancomycin-resistant enterococci (VRE) ● more virulent than MRSA and can survive on environmental surfaces for weeks ■ vancomycin-resistant S. aureus (VRSA) ■ carbapenem-resistant Enterobacteriaceae (CRE) ■ penicillin-resistant Streptococcus pneumoniae HCP contribution to drug-resistant organisms: ➢ giving antibiotics for viral infections succumbing to patient pressure to prescribe unnecessary antibiotic therapy using inadequate drug regimens to treat infections using broad-spectrum or combination agents for infections that should be treated with first-line medications. Patient contribution to resistance: ➢ skipping doses ➢ not taking antibiotics for the full duration of prescribed therapy ➢ saving unused antibiotics “in case I need them later.” ■ limited resources and access to medications make it hard for some patients to get adequate treatment for infections. Health care-associated infections (HAIs)- infections that are acquired because of exposure to microorganisms in a health care setting ➢ usually manifest 48 hours of stay in the hospitals ■ most common: e.coli, staph. aureus, enterococci ➢ nearly 1 in every 25 hospitalized patients has at least 1 HAI ➢ Around one-third of HAIs are preventable ■ Prevention: handwashing before/after procedures, PPE, decontamination of equipment after use, ➢ Sources: ■ Endogenous- microorganisms originate from patients themselves ■ Exogenous- health care environment and personnel ■ Iatrogenic- direct result of diagnostic or therapeutic procedure ➢ CAUTI (catheter associated urinary tract infection): increased risk with increased days the catheter stays in place ➢ ➢ ➢ ❖ ❖ ➢ ❖ ❖ CLABSI (central line bloodstream infection)- increased risk with increased days the catheter is in place Gerontologic Considerations: infections in older adults ➢ the rate of HAIs is 2 to 3 times higher for older adults compared to younger patients ➢ common infections in older adults: pneumonia, UTIs, skin infections, TB ■ Atypical manifestations- cognitive/behavioral changes before the emergence of fever, pain, or changes in laboratory values Infection Precautions ➢ standard precautions- designed to reduce the risk for transmission of microorganisms in hospitals and is applied to ALL patients regardless of diagnosis/presumed infection status ■ applies to blood, all body fluids, secretions, and excretions, non-intact skin, and mucous membranes ➢ transmission-based precautions- used for patients known to be or suspected of being infected with highly transmissible epidemiologically important pathogens that require additional precautions to interrupt transmission and prevent infection (used in addition of standard precautions) ■ ■ ■ airborne- organism can cause infection over long distances when suspended in the air (e.g., TB, rubeola) droplet- minimize contact with pathogens that spread through the air at close contact and that affect the respiratory system or mucous membranes (e.g., influenza, pertussis). contact- minimize the spread of pathogens that are acquired from direct or indirect contact, especially multidrug-resistant organisms (e.g., MRSA, VRE, CRE). GI Disorders Lewis: 897-909 Esophageal Disorders ❖ Gastroesophageal reflux disease (GERD)→ chronic symptom of mucosal damage caused by reflux of stomach acid into the lower esophagus ■ Is a syndrome not a disease ➢ Etiology and Pathophysiology: no single cause; reflux of acidic gastric contents into the esophagus overwhelms the esophageal defenses ■ Esophagitis- esophageal irritation caused by gastric HCL acid and pepsin secretions in refluxate ■ Intestinal proteolytic enzymes (trypsin) and bile, further irritate the esophageal mucosa ■ The degree of inflammation depends on the amount and composition of the gastric reflux and on the esophagus’s mucosal defense mechanisms. ● Primary factor: incompetent Lower Esophageal Sphincter (LES) ◆ Normally acts as an antireflux barrier ◆ Incompetence lets gastric contents move from the stomach to the esophagus when the patient is supine or has an increase in intraabdominal pressure ● Decreased LES pressure can be due to certain foods and drugs ◆ Foods: Alcohol, Chocolate (theobromine), Fatty foods, Peppermint, spearmint, Tea, coffee (caffeine) ◆ Drugs: Anticholinergics. β-Adrenergic blockers, Calcium channel blockers, Diazepam (Valium), Morphine sulfate, Nitrates, Progesterone, Theophylline, Nicotine ● Obesity: intraabdominal pressure is increased ● Hiatal hernia ➢ Clinical Manifestations: Persistent mild symptoms (more than twice a week) or moderate to severe symptoms once a week is considered GERD. ■ Heartburn (pyrosis)- burning, tight sensation felt intermittently beneath the lower sternum and spreading upward to the throat or jaw. ● Most common symptom ● HCP should evaluate heartburn that occurs more than twice a week, is severe, is associated with dysphagia, or occurs at night and wakes a person from sleep ■ GERD-related chest pain can mimic angina- burning; squeezing; or radiating to the back, neck, jaw, or arms ● More common in older adults with GERD ● Relieved with antacids ■ Dyspepsia- pain or discomfort centered in the upper abdomen (mainly in or around the midline as opposed to the right or left hypochondrium). ■ Regurgitation- hot, bitter, or sour liquid coming into the throat or mouth. ■ Respiratory symptoms- wheezing, coughing, and dyspnea ■ Otolaryngologic symptoms- hoarseness, sore throat, a globus sensation (sense of a lump in the throat), hypersalivation, and choking. ➢ Complications: ■ Esophagitis (inflammation of the esophagus) and w/wo esophageal ulcerations; may lead to scar tissue formation, stricture, and dysphagia. ■ Barrett’s esophagus (BE)- (esophageal metaplasia) the flat epithelial cells in the distal esophagus change into columnar epithelial cells ● a precancerous lesion that increases the patient’s risk for esophageal cancer ● About 5% to 20% of people with chronic GERD have BE; those with BE undergo surveillance endoscopy or radiofrequency ablation as recommended. ■ ■ ❖ Respiratory complications- cough, bronchospasm, laryngospasm, cricopharyngeal spasm Asthma, chronic bronchitis, and pneumonia may develop from aspiration into the respiratory system ■ Dental erosion ➢ Diagnostic Studies- done when usual therapy is ineffective or when complications are suspected; determine the cause of GERD ■ Endoscopy- useful in assessing the LES competence & the degree of inflammation (if present), potential scarring, and strictures. ■ Biopsy and cytologic specimens- distinguish stomach or esophageal cancer from BE; the degree of dysplasia (low grade versus high grade) is determined. ■ Manometric studies- measure pressure in the esophagus and LES and esophageal motility function. ■ Ambulatory esophageal pH monitoring- for those with refractory symptoms and no evidence of mucosal inflammation. ■ Radionuclide tests- detect gastric content reflux & rate of esophageal clearance. Nursing and Interprofessional Management: GERD ➢ Lifestyle Modifications ■ Elevate head of bed on 4- to 6-in blocks (30 degrees) ■ Should not be supine 2-3 hours after a meal ■ Stop smoking ➢ Drug Therapy: focuses on decreasing the volume and acidity of reflux, improving LES function, increasing esophageal clearance, and protecting the esophageal mucosa ■ Patients who are symptomatic with GERD but do not have esophagitis (nonerosive GERD) achieve symptom relief with PPIs and H2 receptor blockers. ● PPIs are more effective in healing esophagitis than H2 receptor blockers ◆ also decrease the incidence of esophageal strictures, a complication of chronic GERD ◆ Therapy should start with once-daily dosing, taken before the first meal of the day ◆ Long-term use of PPIs may be associated with decreased bone density, kidney disease, vitamin B12 and magnesium deficiency, and increased risk for dementia ◆ may increase the risk for C. difficile infection in hospitalized patients ● H2 receptor blockers reduce symptoms and promote esophageal healing in 50% of patients; onset of action–1hr ◆ Amotidine, ranitidine, and cimetidine can be given orally or IV ◆ Nizatidine is only available orally ● Antacids produce quick, short-lived relief of heartburn. ◆ Last only 20-30 minutes, or 3-4hrs after meals ◆ most effective taken 1 to 3 hours after meals and at bedtime. ◆ not effective in relieving symptoms or healing lesions in patients w/frequent symptoms or esophagitis ◆ enhance the effects of some drugs, like benzodiazepines and pseudoephedrine ◆ decrease the absorption rates of other drugs, such as thyroid hormones, phenytoin, and tetracycline ● Prokinetics increase LES pressure and improve gastric emptying; improvement in regurgitation & vomiting ◆ use is limited only to those with known delayed gastric emptying due to significant side effects ➢ Nutritional Therapy ■ Avoid foods that decrease LES pressure: chocolate, peppermint, fatty foods, coffee, and tea ■ Reduce/avoid acidic pH: tomato-based products, orange juice, cola, red wine ■ Avoid late evening meals, nighttime snacking, and milk, especially at bedtime ■ Small, frequent meals and drinking fluids between meals help prevent overdistention of the stomach ■ Increased saliva production: gum, oral lozenges for mild symptoms ➢ Surgical Therapy: goal of surgical therapy is to reduce reflux by enhancing the integrity of the LES ■ The fundus of the stomach is wrapped around the lower part of the esophagus to reinforce and repair the defective barrier ● Nissen and Toupet fundoplications are common laparoscopic antireflux surgeries. A small number of patients have complications, including gastric or esophageal injury, splenic injury, pneumothorax, perforation, bleeding, infection, and pneumonia. ◆ In the first month after surgery, the patient may report mild dysphagia caused by edema, but it should resolve ◆ reflux symptoms should decrease but recurrence is possible ■ LINX Reflux Management System- option for patients who have symptoms despite maximum medical management ● a ring of small, flexible magnets enclosed in titanium beads and connected by titanium wires ● Implanted laparoscopically into the LES to strengthen it ● Under resting (nonswallowing) conditions, the magnetic attraction between the beads helps keep a weak LES closed to prevent reflux. ● When the person swallows, the force of pressure associated with the movement of fluids or foods overwhelms the magnetic forces and the fluid or food passes to the stomach ● Adverse events: difficulty swallowing, nausea, and pain when swallowing food ● Cannot have an MRI ➢ Endoscopic Therapy: endoscopic mucosal resection (EMR) & radiofrequency ablation ■ The heat energy delivered through radiofrequencies creates lesions and potentially thicken LES ■ EMR can be used as a diagnostic test to obtain biopsy samples Hiatal Hernia→ herniation of part of the stomach into the esophagus through an opening, or hiatus, in the diaphragm ➢ 2 types ◆ ❖ ➢ ■ ➢ ➢ ➢ ➢ (A) Sliding: The junction of the stomach and esophagus is above the diaphragm, and a part of the stomach slides through the hiatal opening in the diaphragm ● Most common and occurs when the patient is supine ● The hernia usually goes back into the abdominal cavity when the patient is standing upright ■ (B) Paraesophageal or rolling- The fundus and greater curvature of the stomach roll up through the diaphragm, forming a pocket alongside the esophagus; The esophagogastric junction stays in the normal position. ● Acute paraesophageal hernia is a medical emergency. Etiology and Pathophysiology ■ Structural changes (weakening of the muscles in the diaphragm around the esophagogastric opening) occur with aging ■ Factors that increase intraabdominal pressure: obesity, pregnancy, ascites, tumors, intense physical exertion, and heavy lifting on a continual basis Clinical Manifestations: Some are asymptomatic; present manifestations are similar to GERD Complications: GERD, esophagitis, hemorrhage from erosion, stenosis (narrowing of the esophagus), ulcerations of the herniated part of the stomach, strangulation of the hernia, and regurgitation with tracheal aspiration. Diagnostic Studies: ■ ■ ❖ ❖ ❖ esophagram (barium swallow)- may show the protrusion of gastric mucosa through the esophageal hiatus. Endoscopic visualization of the lower esophagus- gives information on the degree of mucosal inflammation or other abnormalities Nursing and Interprofessional Management: Hiatal Hernia ➢ Similar to GERD; Teach the patient to reduce intraabdominal pressure by eliminating constricting garments and avoiding lifting and straining ➢ Surgical approaches: goals are to reduce the hernia, provide an acceptable LES pressure, and prevent movement of the gastroesophageal junction ■ Can include reduction of the herniated stomach into the abdomen ■ herniotomy (excision of the hernia sac) ■ herniorrhaphy (closure of the hiatal defect) ■ Fundoplication & gastropexy (attachment of the stomach below the diaphragm; prevent reherniation) ■ often done laparoscopically by either Nissen or Toupet techniques ➢ Gerontologic Considerations: GERD and Hiatal Hernia ■ The incidence of hiatal hernia and GERD increases with age. ■ Hiatal hernia is associated with weakening of the diaphragm, obesity, kyphosis, or other factors (wearing girdles) that increase intraabdominal pressure. ■ Older patients may take drugs known to decrease LES pressure ■ nonsteroidal antiinflammatory drugs (NSAIDs) and potassium, can irritate the esophageal mucosa, causing medication-induced esophagitis. ■ The first sign may be a serious problem, such as esophageal bleeding from esophagitis or respiratory complications (e.g., aspiration pneumonia) due to aspiration of gastric contents. ■ An older patient with heart & lung problems may not be a good candidate for surgical intervention. Esophageal Cancer→ not common; most are adenocarcinomas; others-squamous cell tumors ■ Adenocarcinomas arise from the glands lining the esophagus and resemble cancers of the stomach and small intestine ■ The incidence is higher in men than in women ➢ Etiology and Pathophysiology ■ Cause is unknown ● Key risk factors include BE, smoking, excess alcohol use, and obesity ● Those with injury to the esophageal mucosa (occupational exposure to asbestos & cement dust) are at greater risk. ● Achalasia- delayed emptying of the lower esophagus;associated w/ squamous cell cancer. ■ Most esophageal tumors occur in the middle and lower portions of the esophagus & appear as an ulceration lesion ● May penetrate the muscular layer and extend outside the wall of the esophagus ➢ Clinical Manifestations & Complications ■ Tumor is advanced by the time symptoms occur ■ Progressive dysphagia- substernal feeling that food is not passing; initially occurs only with meat, then with soft foods, and eventually liquids; most common symptom ■ Pain- develops late; occurs in the substernal, epigastric, or back areas and usually increases with swallowing; may radiate to the neck, jaw, ears, and shoulders ■ When esophageal stenosis (narrowing) is severe, regurgitation of blood-flecked esophageal contents is common ■ Hemorrhage- occurs if the cancer erodes through the esophagus and into the aorta ■ Esophageal perforation with fistula formation into the lung or trachea sometimes develops ■ The tumor may enlarge enough to cause esophageal obstruction (later stages) ➢ Diagnostic Studies ; ■ Endoscopic biopsy- required to diagnose esophageal cancer. ■ Endoscopic ultrasonography (EUS)- important in staging esophageal cancer. ■ Esophagram (barium swallow)- may show narrowing of the esophagus at the tumor site Interprofessional Management: Esophageal Cancer→ depends on the tumor’s location and whether invasion or metastasis is present ➢ best results occur with a multimodal approach, including surgery, endoscopic ablation, chemotherapy, and radiation therapy ➢ Palliative therapy- restoring swallowing function & maintaining nutrition & hydration. Surgical Therapy ■ (1) removal of part or all of the esophagus (esophagectomy) with use of a Dacron graft to replace the resected part ■ (2) resection of a portion of the esophagus and anastomosis of the remaining portion to the stomach (esophagogastrostomy) ■ (3) resection of a portion of the esophagus and anastomosis of a segment of colon to the remaining portion (esophagoenterostomy) ■ Minimally invasive esophagectomy ➢ Endoscopic Therapy: includes photodynamic therapy, EMR, and radiofrequency ablation ■ photodynamic therapy- patient receives an IV injection of porfimer sodium (Photofrin), a photosensitizer; directs light towards the cancerous area using a fiber passed through an endoscope ● Patients must avoid direct sunlight for up to 6 weeks after the procedure. ■ EMR- option for small, early stage cancer; involves the removal of cancer tissue using an endoscope. ■ Radiofrequency ablation uses electric currents to kill cancer cells by heating them. ■ Dilation, stent placement, or both can relieve obstruction ➢ Radiation Therapy ➢ Chemotherapy ➢ Targeted Therapy ➢ Nutritional Therapy- A jejunostomy, gastrostomy, or esophagostomy feeding tube may be placed to feed the patient depending on the type of surgery Nursing Management: Esophageal Cancer ➢ Nursing Assessment ■ Ask about a history of GERD, hiatal hernia, achalasia, BE, and tobacco and alcohol use. ■ Assess the patient for progressive dysphagia and odynophagia (burning, squeezing pain while swallowing). ■ Ask about the type of substances (meats, soft foods, liquids) that cause dysphagia. ■ Assess the patient for pain (substernal, epigastric, or back areas), choking, heartburn, hoarseness, cough, anorexia, weight loss, and regurgitation. ➢ Planning–Overall Goals: (1) have relief of symptoms, including pain and dysphagia; (2) achieve optimal nutritional intake; and (3) have a quality of life appropriate to stage of disease &prognosis ➢ Nursing Implementation ■ Health Promotion: reduce GERD risk factors, Encourage patients to seek medical attention for any esophageal problems, especially dysphagia ■ Acute Care ● Preoperative Care ◆ Provide emotional and physical support, provide information, clarify test results, and maintain a positive attitude with respect to the patient’s immediate recovery and long-term survival. ◆ A high-calorie, high-protein diet is recommended; liquid diet; IV fluid replacement or parenteral nutrition are options ◆ Teach the patient and caregiver how to keep an intake and output record and assess for signs of fluid and electrolyte imbalance. ◆ Some treatment protocols include preoperative radiation and chemotherapy. ◆ Meticulous oral care; Milk of Magnesia with mineral oil helps remove crust formation. ◆ Teaching should include information about chest tubes (with a planned open thoracic approach), IV lines, NG tubes, pain management, gastrostomy or jejunostomy feeding, turning, coughing, and deep breathing ● Postoperative Care ◆ patient usually receives care in the ICU for 1 to 2 days ◆ The patient usually has an NG tube in place for 5 to 7 days. ➢ The drainage may be bloody for 8 to 12 hours. ➢ The drainage gradually changes to greenish yellow. ➢ Assessing the drainage, maintaining the tube, and providing oral and nasal care are key nursing responsibilities. ◆ Have the patient turn, cough and deep breathe, and use an incentive spirometer every 2 hours. ➢ ❖ Position the patient in a semi-Fowler’s or Fowler’s position to prevent reflux and aspiration of gastric secretions. ➢ Evaluation: Expected outcomes–Maintain a patent airway, Have relief of pain, Be able to swallow comfortably and consume adequate nutritional intake, Have a quality of life appropriate to stage of disease and prognosis Eosinophilic Esophagitis (EOE)→ characterized by swelling of the esophagus from an infiltration of eosinophils ➢ People with EoE often have a personal or family history of other allergic diseases ➢ Common food triggers: milk, egg, wheat, rye, beef ➢ Environmental allergens: pollens, molds, cat, dog, and dust mite allergens ➢ Symptoms: heartburn, difficulty swallowing, food impaction in the esophagus, nausea, vomiting, and weight loss ➢ Diagnosis: biopsy findings eosinophils infiltrating esophageal tissue obtained from endoscopy. ➢ Treatment: avoid allergens, corticosteroids, PPIs Esophageal Diverticula→ saclike outpouchings of 1 or more layers of the esophagus. ➢ Occur in 3 main areas: ■ (1) above the upper esophageal sphincter (Zenker’s diverticulum) ● most common location; common in people over 60yrs ■ (2) near the esophageal midpoint (traction diverticulum) ■ (3) above the LES (epiphrenic diverticulum) ➢ Food becomes trapped in outpouches; sour food, foul odor ➢ Symptoms: dysphagia, regurgitation, chronic cough, aspiration, and weight loss ➢ Complications: malnutrition, aspiration, and perforation ➢ Management: apply pressure to neck to empty food pocketing, blend food, Endoscopic stapling diverticulotomy or diverticulostomy Esophageal Strictures→ narrowing of esophagus caused by chronic GERD or ingestion of strong acids or alkalis, external beam radiation, and surgical anastomosis, scar formation (trauma) ➢ Can cause dysphagia, regurgitation, weight loss ➢ can be dilated using mechanical bougies (dilating instruments) or balloons with or without endoscopy, or with fluoroscopy ➢ Surgical excision with anastomosis is sometimes needed. ➢ The patient may have a temporary or permanent gastrostomy. Achalasia→ rare, chronic disorder peristalsis of the lower two thirds (smooth muscle) of the esophagus is absent with no exact cause known ➢ The pressure in the LES increases along with incomplete relaxation ➢ Esophageal obstruction at or near the diaphragm occurs. ➢ Food and fluid accumulate in the lower esophagus ➢ The result is dilation of the esophagus above the tapered affected segment of the lower esophagus ➢ Symptoms: dysphagia, globus sensation and/or substernal chest pain (similar to angina pain) during or right after a meal, nighttime regurgitation, halitosis, inability to eructate (belch) ➢ Diagnosis: esophagram (barium swallow), manometric evaluation (high-resolution manometry), and/or endoscopic evaluation. ➢ Treatment: symptom management; relieve dysphagia and regurgitation, improve esophageal emptying by disrupting the LES, and prevent the development of megaesophagus (enlargement of the lower esophagus) ■ Endoscopic pneumatic dilation: dilating the LES muscle using balloons of progressively larger diameter (3.0, 3.5, and 4.0 cm) ■ Heller myotomy: HCP cuts through the muscles of the LES, allowing food to pass ■ injection of botulinum toxin endoscopically into the LES gives short-term relief of symptoms and improves esophageal emptying ■ Nitrates (e.g., isosorbide dinitrate) and calcium channel blockers (e.g., nifedipine [Procardia]) relax the LES and may improve dysphagia Esophageal Varices→ dilated, tortuous veins occurring in the lower part of the esophagus because of portal hypertension ➢ Common complication of liver cirrhosis ◆ ❖ ❖ ❖ ❖ ❖ Drug Therapy: GERD & Peptic Ulcer Disease (PUD) Drug Proton Pump Inhibitors (PPIs): dexlansoprazole (Dexilant), esomeprazole (Nexium), lansoprazole (Prevacid), Omeprazole (Prilosec), omeprazole & sodium bicarbonate (Zegerid),pantoprazole (Protonix), rabeprazole (Aciphex) Histamine (H2) Receptor Blockers: Cimetidine, famotidine (Pepcid), nizatidine (Axid), ranitidine (Zantac) Mechanism of action Headache, abdominal pain, nausea, diarrhea, vomiting, flatulence -Block the action of histamine on the H2 receptors to ↓ HCl acid secretion, -↓ Conversion of pepsinogen to pepsin, -↓ Irritation of the esophageal and gastric mucosa Headache, abdominal pain, constipation, diarrhea -Neutralize HCl acid, -Taken 1–3 hr after meals and at Single Substance aluminum hydroxide (Amphojel), bedtime calcium carbonate (Tums), sodium bicarbonate (Alka-Seltzer), sodium citrate (Bicitra), Aluminum and Magnesium; Gelusil, Maalox, Mylanta aluminum/ magnesium, trisilicate (Gaviscon) Antacids, Acid Neutralizers: Cholinergic: bethanechol (Urecholine) Cytoprotective: sucralfate (Carafate) Prokinetic: metoclopramide (Reglan) Prostaglandin (Synthetic): misoprostol (Cytotec) Side effects -↓ HCl acid secretion by inhibiting the proton pump (H+-K+-ATPase) responsible for the secretion of H+, -↓ Irritation of the esophageal & gastric mucosa - Aluminum hydroxide: Constipation, phosphorus depletion w/chronic use, -Calcium carbonate: Constipation/diarrhea, hypercalcemia, milk-alkali syndrome, renal calculi, -Magnesium preparations: Diarrhea, hypermagnesemia -Sodium preparations: Milk-alkali syndrome if used w/large amounts of calcium. ↑ Lower esophageal sphincter pressure, improve esophageal emptying, increase gastric emptying Lightheadedness, syncope, flushing, diarrhea, stomach cramps, dizziness Act to form a protective layer and serve as a barrier against acid, bile salts, and enzymes in the stomach Constipation Block effect of dopamine, ↑ Gastric motility and emptying, Reduce reflux CNS side effects ranging from anxiety to hallucinations; Extrapyramidal side effects (tremor and dyskinesias similar to Parkinson’s disease) -Protect lining of stomach -Cytoprotective: Increase production of gastric mucus and mucosal secretion of bicarbonate -Antisecretory: ↓ HCl acid secretion Abdominal pain, diarrhea, GI bleeding, uterine rupture if pregnant Disorders of the Stomach and Upper Small Intestine ❖ Peptic Ulcer Disease→ condition characterized by erosion of the GI mucosa from the digestive action of HCl acid and pepsin ➢ Any part of the GI tract that is in contact w/gastric secretions is susceptible to ulcer development: esophagus, stomach, duodenum, and margin of a gastrojejunal anastomosis after surgical procedures ➢ Types: classified as acute or chronic, depending on the degree & duration of mucosal involvement, and gastric or duodenal, according to the location ■ acute ulcer- associated with superficial erosion and minimal inflammation ● Short duration ● resolves quickly when the cause is identified and removed ■ chronic ulcer- is one of long duration, eroding through the muscular wall with the formation of fibrous tissue ● More common ➢ Etiology and Pathophysiology: develop only in an acid enviro. ■ Helicobacter Pylori: 80% of gastric & 90% of duodenal ulcers ● Infection likely occurs during childhood with transmission from family members to the child, possibly through a fecal-oral or oral-oral route ● rate is highest in black and Hispanic people ● those infected with CagA-positive strains are more likely to have PUD ● Bacteria make urease→ metabolizes urea-producing ammonium chloride ● Urease activates immune response w/antibody production & cytokine release ◆ Leads to increased gastric secretion and tissue damage ■ Medication-Induced Injury: NSAIDs inhibit prostaglandin synthesis, increase gastric acid secretion, and reduce the integrity of the mucosal barrier ➢ ➢ ● Patients taking corticosteroids or anticoagulants w/ NSAIDs have a higher risk ● Corticosteroids affect mucosal cell renewal and decrease its protective effects ■ Lifestyle Factors ● High alcohol intake is associated w/ acute mucosal lesions. ● Alcohol & smoking stimulate acid secretion. Coffee (caffeinated and decaffeinated) is a strong stimulant of gastric acid secretion. ● Smoking and psychologic distress, including stress and depression, can delay the healing of ulcers once they have developed ■ Gastric Ulcers: occur in any part of the stomach (most often in antrum) ● more prevalent in women and those over 50 years of age ● are more likely than duodenal ulcers to cause an obstruction. ● H. pylori, NSAIDs, and bile reflux are the main risk factors. ■ Duodenal Ulcers: account for about 80% of all peptic ulcers; incidence is especially high between 35 and 45 years of age; often associated with a high HCl acid secretion ● High risk: (COPD), cirrhosis, pancreatitis, hyperparathyroidism, chronic kidney disease, and Zollinger-Ellison syndrome (ZES- severe peptic ulceration and HCl acid hypersecretion) ● tend to occur continuously for a few weeks or months and then disappear for a time, only to recur some months later ■ Stress-Related Mucosal Disease (SRMD): mucosal damage in the GI tract ranging from small single lesions to multiple gastric ulcers and major bleeding ● often occurs in critically ill patients who have had severe burns, trauma, or major surgery ● Patients with coagulopathy, liver disease, or organ failure and those receiving renal replacement therapy are at highest risk for SRMD Clinical Manifestations ■ Gastric ulcers- discomfort is generally high in the epigastrium and occurs about 1 to 2 hours after meals ● described as “burning” or “gaseous.” ● food worsens pain (ulcer eroded through gastric mucosa) ■ duodenal ulcers- symptoms occur when gastric acid comes in contact with the ulcers ● Food buffers acid; symptoms occur generally 2 to 5 hours after a meal ● pain is described as “burning” or “cramplike.” (midepigastric region beneath the xiphoid process; back pain) ■ bloating, nausea, vomiting, and early feelings of fullness ■ Silent peptic ulcers are more likely to occur in older adults & those taking NSAIDs Diagnostic Studies ■ Endoscopy: most accurate procedure to determine the presence and location of an ulcer ● direct viewing of the gastric and duodenal mucosa; assess degree of ulcer healing after treatment ● During endoscopy, tissue specimens are taken to determine if H. pylori is present and rule out stomach cancer. ■ H. pylori infection tests ● “gold standard”- biopsy of the antral mucosa with testing for urease (rapid urease testing)--Urea is a by-product of the metabolism of H. pylori bacteria ● Noninvasive- serology, stool, and breath testing ◆ urea breath and stool antigen tests can identify active infection ◆ Antibody tests for H. pylori can remain positive for years ■ barium contrast study- diagnose gastric outlet obstruction or for ulcer detection in those who cannot undergo endoscopy ■ Laboratory tests: CBC, liver enzyme studies, serum amylase, and stool examination ● A CBC may show anemia from ulcer bleeding. ● ➢ Liver enzyme studies help detect any liver problems (cirrhosis) that may complicate ulcer treatment. ● Stools are tested for blood. ● A serum amylase evaluates pancreatic function if we suspect posterior duodenal ulcer penetration of the pancreas. Interprofessional Management: PUD ■ Conservative Care ■ Drug Therapy: focuses on reducing gastric acid secretion and, if needed, eliminating H. pylori infection ● Strict adherence to the prescribed drug regimen is important–ulcers often recur ● ➢ Antibiotic therapy: prescribed concurrently w/a PPI for 14 days for H.pylori ◆ If the patient has a penicillin allergy, metronidazole is used instead of amoxicillin in the triple-drug regimen. ◆ Bismuth can be given alone or as part of a combination capsule (Pylera) containing bismuth, tetracycline, and metronidazole ● Proton Pump Inhibitors: more effective than H2 receptor blockers in reducing gastric acid secretion and promoting ulcer healing ● Cytoprotective Drug Therapy: Sucralfate is used for short-term ulcer treatment ◆ provides mucosal protection for esophagus, stomach, & duodenum. ◆ Does not have acid-neutralizing capabilities ◆ give it at least 60 minutes before or after an antacid ◆ binds with cimetidine, digoxin, warfarin, phenytoin, and tetracycline, reducing their bioavailability ● H2 receptor blockers and antacids may be used as adjunct therapy to promote ulcer healing; (antacids) increase gastric pH by neutralizing HCl acid, reduce acid content of chyme reaching duodenum ● Misoprostol: synthetic prostaglandin analog prescribed to prevent gastric ulcers caused by NSAIDs and LDA; protective and some antisecretory effects on gastric mucosa ● Tricyclic antidepressants (imipramine, doxepin): anticholinergic properties ● Anticholinergic drugs: several side effects–dry mouth, warm skin, flushing, thirst, tachycardia, dilated pupils, blurred vision, & urine retention ■ Nutritional Therapy: eat and drink foods and fluids that do not cause any distressing symptoms (pepper, carbonated beverages, broth (meat extract), and hot, spicy foods; caffeine-containing beverages, alcohol ■ Surgical Therapy- done on patients with complications that are unresponsive to medical management or concerns about stomach cancer Complications ■ Hemorrhage: most common complication of PUD. Duodenal ulcers cause more upper GI bleeding episodes than gastric ulcers ■ Perforation: most lethal complication of PUD; the ulcer penetrates the serosal surface with spillage of either gastric or duodenal contents into the peritoneal cavity ● Manifestations: sudden and onset ◆ initial phase (0 to 2 hours after perforation)→ patient has sudden, severe upper abdominal pain that quickly spreads throughout the abdomen and radiates to the back and shoulders ➢ Food or antacids do not relieve the pain. The abdomen appears rigid and boardlike as the abdominal muscles try to protect from further injury. ➢ The patient’s respirations become shallow and rapid. ➢ The heart rate is elevated, and the pulse is weak. ➢ Bowel sounds are usually absent. ➢ Nausea and vomiting may occur. ◆ bacterial peritonitis may occur within 6 to 12 hours ● Management: The immediate focus of managing a patient with a perforation is to stop the spillage of gastric or duodenal contents into the peritoneal cavity and restore blood volume ◆ NG tube- continuous aspiration and gastric decompression ◆ Circulating blood volume is replaced with lactated Ringer’s & albumin solutions; substitute for the fluids lost from the vascular and interstitial space as peritonitis develops ◆ Blood replacement in the form of packed RBCs may be needed. ◆ A central venous pressure line and an indwelling urinary catheter may be inserted and monitored hourly. ◆ Broad-spectrum antibiotic therapy is started immediately to treat bacterial peritonitis ■ Gastric Outlet Obstruction: result of edema, inflammation, pylorospasm, or fibrous scar tissue formation ● Manifestations: ◆ patient reports discomfort or pain that is worse toward the end of the day as the stomach fills and dilates. ◆ Belching or self-induced vomiting may provide some relief. ◆ Vomiting is common and often projectile; may contain food particles that were ingested hours or days before. ◆ Constipation occurs because of dehydration and decreased diet intake from anorexia. ◆ Over time dilation of the stomach and visible swelling in the upper abdomen may occur. ● Management: decompress the stomach, correct any existing fluid and electrolyte imbalances, and improve the patient’s general state of health Nursing Management: Peptic Ulcer Disease ➢ Nursing Assessment ; ■ Subjective Data ● PMH: Chronic kidney disease, pancreatic disease, COPD, serious illness or trauma, hyperparathyroidism, cirrhosis of the liver, ZES ● Medications: Aspirin, corticosteroids, NSAIDs ● Surgery or other treatments: Complicated or prolonged surgery ■ Functional Health Patterns ● Health perception–health management: Chronic alcohol use, smoking, caffeine use. Family history of PUD ● Nutritional-metabolic: Weight loss, anorexia, nausea and vomiting, hematemesis, dyspepsia, heartburn, belching ● Elimination: Black, tarry stools ● Cognitive-perceptual: (1) Duodenal ulcers: Burning, midepigastric/back pain 2–5 hr after meals and relieved by food; nighttime pain common (2) Gastric ulcers: High epigastric pain 1–2 hr after meals. Food may precipitate or worsen pain. ● Coping–stress tolerance: Acute or chronic stress ■ Objective Data ● General: Anxiety, irritability ● Gastrointestinal: Epigastric tenderness ● Possible Diagnostic Findings: Anemia. Guaiac-positive stools. Positive blood, urine, breath, or stool tests for H. pylori. Abnormal upper GI endoscopic and barium studies ➢ Planning: Overall goals for a patient with PUD ■ (1) adhere to the prescribed therapeutic regimen ■ (2) see a reduction in or absence of discomfort ■ (3) have no signs of GI complications ■ (4) have complete healing of the peptic ulcer ■ (5) make appropriate lifestyle changes to prevent recurrence ➢ ➢ ➢ ➢ Nursing Implementation ■ Health Promotion ● Early detection and effective treatment for ulcers ● Take ulcerogenic drugs (NSAIDs, LDA) with food ● Report symptoms related to gastric irritation, including epigastric pain, to HCP ■ Acute Care ● Hemorrhage ◆ Changes in vital signs and an increase in the amount and redness of aspirate often signal massive upper GI bleeding. ◆ With bleeding, the patient’s pain often decreases because the blood helps neutralize the acidic gastric contents. ◆ It is important to maintain the patency of the NG tube so that blood clots do not obstruct the tube ● Perforation ◆ Take vital signs promptly and record them every 15 to 30 minutes. ◆ Temporarily stop all oral or NG drugs and feedings. ● Gastric Outlet Obstruction ◆ Regularly irrigate the NG tube with a normal saline solution per agency policy to assist proper functioning ◆ To check for ongoing obstruction, clamp the NG tube intermittently and measure the gastric residual volume ■ Ambulatory Care: Patient teaching ● Avoiding foods that cause epigastric distress, such as acidic foods. ● Avoid cigarettes. Smoking promotes ulcer development and delays ulcer healing. ● Reduce or eliminate alcohol use. ● Avoid OTC drugs unless approved by the HCP. Many preparations contain ingredients, such as aspirin, that should not be taken unless approved by the HCP. Check with the HCP about the use of NSAIDs. ● Do not interchange brands of PPIs, antacids, or H2 receptor blockers that you can buy OTC without checking with the HCP. This can lead to harmful side effects. ● Take all medications as prescribed. This includes both antisecretory and antibiotic drugs. Not taking medications as prescribed can cause a relapse. ● It is important to report any of the following: Increased nausea or vomiting, Increased epigastric pain, Bloody emesis or tarry stools ● Stress can be related to signs and symptoms of PUD. Learn and use stress management strategies ● Share concerns about lifestyle changes and living with a chronic illness. ● PUD is a chronic, recurring disorder. Teach patients with chronic PUD about potential complications, and what to do until they see the HCP. Emphasize the need for long-term follow-up care. Evaluation: Expected outcomes ■ Have pain controlled without the use of analgesics ■ States an understanding of the treatment plan ■ Commit to self-care and management of the disease ■ Have no complications (hemorrhage, perforation) Gerontologic Considerations: Peptic Ulcer Disease ■ The morbidity and mortality rates associated with PUD in older adults are higher than for younger adults because of concurrent health problems and a decreased ability to withstand hypovolemia ■ Monitor older adults who use NSAIDs for osteoarthritis for PUD. ■ In older patients, pain may not be the first symptom associated with an ulcer. ■ For some patients the first sign is frank gastric bleeding or a decrease in hematocrit. Disorders of The Liver Lewis 968-979 ❖ Hepatitis→ inflammation of the liver. Incubation Period/ Mode of Transmission. Sources of Infection Infectivity Hepatitis A Virus (HAV) Incubation: 15–50 days (average 28) • Fecal- oral (primarily fecal contamination and oral ingestion) •Contaminated food, milk, water, shellfish •Crowded conditions (day care, nursing home) •Persons w/subclinical infections, infected food handlers, sexual contact, IV drug users • Poor personal hygiene •Poor sanitation • Most infectious during 2 wk before onset of symptoms • Infectious until 1–2 wk after the start of symptoms Hepatitis B Virus (HBV) Incubation: 115–180 days (average 56–96) • Percutaneous (parenteral) or mucosal exposure to blood or blood products • Sexual contact • Perinatal transmission • Contaminated needles, syringes, and blood products • •Before and after symptoms appear •Infectious HBV-infected mother (perinatal transmission) • Sexual activity for months • Carriers continue to be infectious with infected partners. Asymptomatic carriers • Tattoos or for life body piercing with contaminated needles Hepatitis C Virus (HCV) Incubation: 14–180 days (average 56) • Percutaneous (parenteral) or mucosal exposure to blood or blood products • High- risk sexual contact •Perinatal contact • Blood and blood products • Needles and syringes • Sexual activity with infected partners, low risk • 1–2 wk before symptoms appear •Continues during clinical course •75%–85% go on to develop chronic hepatitis C and remain infectious • Same as HBV • Can cause infection only when HBV is present • Blood infectious at all stages of HDV infection Hepatitis D Virus (HDV) Incubation: 2-26 wk •HBV must precede HDV •Chron. carriers of HBV always at risk Hepatitis E Virus (HEV) Incubation: 15-64 days (avg 26-42 days) •Fecal-oral route •Outbreaks assoc. w/contaminated water supply Hepatitis A Virus Hepatitis B Virus Hepatitis C Virus Hepatitis D Virus Hepatitis E Virus Pathophysiology ■ Liver ■ Systemic Effects ➢ Clinical Manifestations and Complications ■ Acute Hepatitis ● Acute Liver Failure ■ Chronic Hepatitis ➢ Diagnostic Studies ➢ Interprofessional Care ➢ Drug Therapy ■ Acute Hepatitis ■ Chronic Hepatitis B ● Nucleoside and nucleotide analogs ● Interferon ■ Chronic Hepatitis C ➢ Nutritional Therapy ➢ Nursing Management: Viral Hepatitis ■ Nursing Assessment ■ Nursing Diagnoses ■ Planning ■ Nursing Implementation ● Health Promotion ◆ Hepatitis A ◆ Hepatitis B ◆ Hepatitis C ● Acute Care ● Ambulatory Care ■ Evaluation Drug- and Chemical-Induced Liver Diseases Autoimmune, Genetic, and Metabolic Liver Diseases ➢ Autoimmune Hepatitis ➢ ➢ ➢ ➢ ➢ ➢ ❖ ❖ •Contaminated water, poor sanitation •Found in Asia, Africa, & •Not known •May be similar to HAV Mexico •Not common in US but increasing in some areas ➢ ➢ ➢ ➢ ➢ Wilson’s Disease Hemochromatosis Primary Biliary Cholangitis Primary Sclerosing Cholangitis Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis