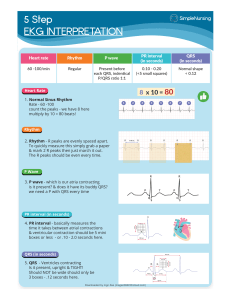
Chapter 1 - The Basics CARDIAC CYCLE ● DIASTOLE → ventricles relax & fill. ○ Rapid-Filling Phase: ventricles passively fill with blood from the atria. ○ Diastasis: blood flow from atria to ventricles slow as the pressures between the two equalize. ○ Atrial Kick: atria contracts to squeeze the remaining blood into the ventricle (accounts for 15% - 30% of ventricular filling). ● SYSTOLE → ventricles contract & expel. ○ Isovolumetric Contraction: ventricles contract BUT the valves are still closed, because the ventricular pressures are not high enough yet to overpower the pulmonary artery and the aorta. - Greatest consumption of myocardial oxygen. ○ Ventricular Ejection: ventricles build up enough pressure via contraction to overcome the pressure of the aorta and pulmonary arteries, thus opening the semilunar valves. ○ Protodiastole: pressure equalizes between the great vessels (aorta & pulmonary arteries) and the ventricles as the blood leaves, which results in slower flow into the vessels. ○ Isovolumetric Relaxation: pressure in the ventricles drop as the blood leaves and the muscle begins to relax, and due to the increased pressure in the vessels, the semilunar valves shut close. CORONARY CIRCULATION The myocardium receives blood flow only during diastole, because the coronary arteries are compressed when the heart contracts during systole. ● Deoxygenated blood returns to the right atrium via coronary sinus (a coronary vein). ● Left Main Coronary Artery (LCMA) → Left Anterior Descending (LAD) and Circumflex ○ LMCA (which includes the LAD + Circumflex) provides blood to the ANTERIOR and LATERAL walls of the LEFT VENTRICLE (this supplies about 60% of the myocardium). - Blockage in the LMCA can produce a massive MI, which is why it’s called the widow maker. ○ LAD = ANTERIOR Circumflex = LATERAL ● Right Coronary Artery (RCA) → provides blood to the RIGHT VENTRICLE and the INFERIOR part of the LEFT VENTRICLE. Posterior Descending Artery (PDA) ● In 70% of people, the PDA branches from the RCA. ○ These people are referred to as “right-dominant”. ○ The RCA is dominant in perfusing the POSTERIOR wall of the heart. ● In 30% of people, the PDA branches from the circumflex coronary artery. ○ These people are referred to as “left-dominant”. ○ The LMCA is dominant in perfusing the POSTERIOR wall of the heart. AUTONOMIC NERVOUS SYSTEM (Influencing the Heart) ● Sympathetic Nervous System → mediated by NOREPINEPHRINE (chemical released by the adrenal glands). ○ ⇧ HR & BP, ⇩ digestion, pupil dilation. ● Parasympathetic Nervous System → mediated by ACETYLCHOLINE (chemical released when the vagus nerve is stimulated). ○ Vagus nerve (CN X) travels from the brain to the heart, stomach, and other areas. - Stimulated by any action that CLOSES THE GLOTTIS (i.e. holding breath, straining for a BM). ○ ⇩ HR & BP, ⇧ digestion, pupil constriction. Chapter 2 - Electrophysiology Cardiac cells at rest are NEGATIVELY charged– there is more Na+ in the cell, and there is more K+ outside of the cell. ● When cardiac cells are stimulated*, Na+ goes into the cell and K+ leaks out, which causes an electrical discharge → this is called depolarization, and it results in an action potential. ○ The cardiac cells are now POSITIVELY charged. ● Na+ and K+ shift back to their original places using the sodium-potassium pump → this is called repolarization. ACTION POTENTIALS ● Phase 4 → cardiac cells are at rest, negatively charged at -90 mV (shown as a flat line). ● Phase 0 → cardiac cells are stimulated & depolarization occurs; the cells are now positively charged at 20 mV (shown as the QRS complex). ● Phase 1 & 2 (Early Repolarization) → Ca(2+) is released as a response to Phase 0, which results in VENTRICULAR CONTRACTION. ○ Shown as the ST segment → although there is no electrical activity, there is mechanical activity (i.e. the heart is contracting). ○ Phase 2 → Plateau Phase ● Phase 3 (Rapid Repolarization) → Na+ and K+ return back to their original places via sodium-potassium pump (shown as T wave). REFRACTORY PERIODS ● ABSOLUTE → cardiac cells CANNOT accept another impulse, because it’s dealing with the previous one (no matter how strong the impulse is). ○ Occurs from the start of the QRS complex to the start of the T wave. ● RELATIVE → a strong enough impulse can force the cardiac cells to receive it, however, the response will not be the same vigor as it was before. ● SUPERNORMAL → the cardiac cells accept impulses that are weaker than normal because the cells are in a “hyper” state, resulting in fast & dangerous rhythms. EKG WAVES & COMPLEXES ● P wave → ATRIAL DEPOLARIZATION ● Ta wave → ATRIAL REPOLARIZATION ○ Masked by the QRS wave! ● QRS complex → VENTRICULAR DEPOLARIZATION ● T wave → VENTRICULAR REPOLARIZATION ● U wave → LATE VENTRICULAR REPOLARIZATION (normally NOT seen). ● PR & ST segments → no electrical activity is present! ○ Atrial contraction occurs during the P wave and PR segment. ○ Ventricular contraction occurs during the QRS complex and the ST segment. ● The flat line after the T wave and before the next P wave is called the baseline or isoelectric line. BREAKING DOWN THE QRS COMPLEX Q wave → negative deflection that occurs before a positive deflection. ● There is only ONE Q wave, and it must be the first wave of the complex. R wave → any positive deflection. ● There CAN be MORE THAN ONE– a second R wave is named R prime (R’). S wave → negative deflection that is after the R wave. QS wave → negative deflection with no positive deflection. CARDIAC CONDUCTION SYSTEM SA node → interatrial tracts → atrium → internodal tracts → AV node → bundle of His → bundle branches → Purkinje fibers → ventricles 1. The SA node is one of the body’s pacemakers– this starts the impulse. ● Found in the upper right atrium, just below the SVC. 2. Impulse travels through the interatrial tracts (conductive tissues that bring the impulses to the atrial tissue)-- the atria will depolarize, which shows up as the P wave. 3. Impulse travels through the internodal tracts (bottom right side of the interatrial septum) and brings it to the AV node. ● The AV node holds onto the impulse and slightly delays it, so that the atrium has enough time to contract and push blood into the ventricles. 4. The impulse travels to the bundle of His (right underneath the AV node), to the left and right branches found in the interventricular septum. and to the Purkinje fibers. 5. The impulse arrives at the ventricles, causing it to depolarize (which shows up as the QRS complex). PACEMAKER CELLS & THEIR INHERENT RATES SA node → 60 to 100 BPM AV junction → 40 to 60 BPM ventricles → 20 to 40 BPM The fastest pacemaker at any given moment is the one in control. Each pacemaker can fire at faster rates IF there is OUTSIDE stimuli! escape → occurs when the predominant pacemaker slows dramatically/ fails, and the lower pacemaker has to take over (provides a new rhythm that is slower than the previous). ● Escape beats is any beat that comes after a pause that is longer than the normal, established heartbeat-to-heartbeat cycle (also known as the R-R cycle). ● Escape rhythm is a series of escape beats. usurpation/ irritability → when one of the lower pacemakers fires earlier and faster than the predominant pacemaker, which results in a new and faster rhythm. Any abnormalities in the conduction can result in an arrhythmia. EKG PAPER Each small box represents 1 mm in height and width. ● Dark lines are present every 5th small box. 5 BIG boxes = 1 SECOND ● 1 BIG box = 0.20 SEC ● 1 SMALL box = 0.04 SEC ● 300 BIG box = 1 MIN EKG paper can either be a 12-lead EKG or rhythm strip. ● 12-lead EKGs view the heart’s electrical activity from 12 different angles (leads). ● Rhythm strips view the heart’s electrical activity from 1 or 2 different angles (leads) for either 6 or 12 seconds. INTERVALS ● PR interval = 0.12 to 0.20 seconds ○ Time it takes for impulse to get from the atria to the ventricles. ○ Includes the P wave and the PR segment. - P wave < 0.10 seconds ● QRS interval = 0.06 to 0.10 seconds (< 0.12 seconds) ○ Time it takes to depolarize the ventricles. ○ Includes the QRS complex (from beginning to end). ● QT interval ≤ ½ the distance between successive QRS complexes (R-R interval) if heart rate is between 60 - 100 BPM. ○ Time it takes to depolarize and repolarize the ventricles. ○ Includes the QRS complex and the T wave. ○ HOW to know if QT is prolonged… - Draw a line midway between two QRS complexes. - NORMAL = T wave is before or at the midline. PROLONGED = T wave is after the midline. ○ QTc is the QT interval determined by the EKG machine that is ADJUSTED for the heart rate. Chapter 3 - Lead Morphology & Placement 12-LEAD EKG: LEAD TYPES IMPORTANT NOTE: The right leg electrode is called the “ground” or “earth” electrode– it reduces the risk of electrical shock to the patient & stabilizes the EKG. It does NOT make a lead!!! 1. BIPOLAR LEADS View the heart’s electrical activity between two limbs– one limb will be designated (+) and the other will be (-). The POSITIVE limbs will “see” the electrical activity traveling from the negative limb. ● Lead I forms from the RA electrode (-) and the LA electrode (+). ○ This creates a left → right view of the heart. ● Lead II forms from the RA electrode (-) to the LL electrode (+). ○ This creates a diagonal view of the heart, specifically bottom → upper right. ● Lead III forms from the LA electrode (-) to the LL electrode (+). ○ This creates a diagonal view of the heart, specifically bottom → upper left. Einthoven’s Law → Lead I + Lead III = Lead II - The height of the QRS in Lead II will be the same height as the QRS in Lead I and III combined! - PURPOSE: Determine if EKG is truly abnormal or placed in the wrong limb. 2. AUGMENTED LEADS aV stands for augmented voltage, and the letter after represents the location of the (+) limb. ● aVR forms from the midpoint of LA and LL (-) to the RA electrode (+). ● aVL forms from the midpoint of RA and LL (-) to the LA electrode (+). ● aVF forms from the midpoint of RA and LA (-) to the LL electrode (+). Both BIPOLAR and AUGMENTED leads are considered to be FRONTAL LEADS, which means they view the heart’s electrical activity from the FRONTAL PLANE → top to bottom, left to right. When combining all 6 BIPOLAR and AUGMENTED leads, it creates a hexaxial diagram. The frontal leads allow you to view the heart from 6 different views on the frontal plane! 3. PRECORDIAL LEADS Unipolar leads (each electrode is POSITIVE) located on the CHEST that view the heart in a HORIZONTAL plane. ● V1 is found at the 4th ICS at the right sternal border (RSB). ● V2 is found at the 4th ICS at the left sternal border (LSB). ● V3 is found between V2 and V4 at the 5th rib cage. ● V4 is found at the 5th ICS at the midclavicular line (MCL). ● V5 is found at the 5th ICS at the anterior axillary line (AAL) ● V6 is found at the 5th ICS at the midaxillary line (MAL). CONTINUOUS MONITORING Continuous EKG monitoring is attached to either a 3-lead or a 5-lead cable connected telemetry. ● The two MOST COMMONLY used leads for continuous monitoring include… ○ Lead II → most utilized, because it provides the best views for atrial activity (P waves) and ventricular activity (QRS complexes). ○ V1 (or MCL1) → assesses rhythms with wide QRS complexes, and helps pinpoint ventricular conduction abnormalities. ■ Found in V1 position– 4th ICS at the RSB. EKG TRUTHS ● Electrical impulses traveling TOWARDS a (+) electrode will have a POSITIVE (UPWARD) QRS complex. ● Electrical impulses traveling AWAY from a (+) electrode– in other words, towards a (-) electrode– will have a NEGATIVE (DOWNWARD) QRS complex. ● Electrical impulses traveling at a RIGHT ANGLE to a (+) electrode will have an ISOELECTRIC complex. ● If there is NO impulse detected, then there will just be a FLAT LINE. NORMAL EKG DEFLECTIONS Normal vector forces (i.e. current flow) of the heart flow from TOP → BOTTOM and RIGHT → LEFT. ● For the FRONT LEADS… ○ Leads I, II, III, aVL, and aVF should have POSITIVE deflections, because they FOLLOW the vector forces of the heart. ○ aVR should have a NEGATIVE deflection, because it GOES AGAINST the vector forces of the heart. ● For the PRECORDIAL LEADS… ○ V1 (or MCL on continuous monitoring) and V2 should be NEGATIVE. - V1 initially begins as a (+) because the current is going through the septum first (meaning the vector is going from L → R)– this is depicted at 1. - However, the current heads to the ventricles and stays there for the majority of the time (meaning the vector is now L → R)– this is depicted at 2. - The complex will mostly be NEGATIVE due to this pattern. There will be a small R wave (1), and a deep S wave (2). ○ V3 and V4 should be ISOELECTRIC. ○ V5 and V6 should be POSITIVE. - OVERALL EKG V6 works similarly to V1 BUT in the opposite way. Chapter 4 - Technical Aspects of EKGs VOCABULARY lead wires the small wires attached to the electrodes amplifier magnifies the signal received from the electrodes and lead wires digital converter converts signal from the electrodes and lead wires into a digital signal that can be recorded and printed chart speed CONTROL FEATURE on the EKG regulates the speed a which the paper records - Default speed is 25 mm/seconds, meaning there are 25 little blocks in one second. gain CONTROL FEATURE on the EKG regulates the height of the complexes - Default is 10 mm/mV → this means that 1 mV of electricity picked up will show up as 10 mm on the paper. - Increase gain if the rhythm is small and hard to read! frequency response CONTROL FEATURE on the EKG filters out unwanted interference & artifacts to create a smoother EKG macroschock ELECTRICAL SAFETY high-voltage shock (about 110 volts) that can cause severe injury - Normally caused by frayed/ broken wires and cords, electrical outlet damage, or other malfunctions. microshock ELECTRICAL SAFETY smaller shock that is normally produced by a device (i.e. pacemaker) - Leakage currents are often offset by the artifacts unwanted interference or jitter on the EKG TYPES of ARTIFACTS ● Somatic Tremors → jittery patterns caused by the patient’s tremors or shaking wires. ○ If patient’s tremors can’t be corrected (i.e. Parkinson’s patients), then make a few attempts and choose the best EKG that contains the cleanest QRS. ● Baseline Sway → baseline of the EKG moves up and down, which is normally caused by breathing pattern, lotion, or sweat. ● 60-Cycle Interference → thick-looking patterns, which is caused by electrical devices nearby (i.e. hospital machines, hand-held devices). ● Broken Recording → caused by frayed or fractured wires, or loose electrodes. HOW to TELL the DIFFERENCE BETWEEN REAL OR ARTIFACT? ● If the rhythm is DIFFERENT from the patient’s previous rhythm (artifact or real)– CHECK & ASSESS the patient! ● Observe rhythms in other leads– preferably V1 or MCL1, because it has less muscle artifacts. ● Check if the rhythm meets all of its normal criteria– if NOT, check another lead to be sure. ● Check the monitor wires and electrodes to see if they are loose/detached. ● Check the patient to see if they are having any muscle activity that could be affecting the EKG. ● Follow the QRS complexes. Chapter 5 - Calculating Heart Rate To calculate heart rate, you must calculate the ventricular rate → count the # of QRS complexes. If you want to determine the atrial rate → count the # of P waves. METHODS for CALCULATING HEART RATE ● 6-Second Strip Method ○ Tells the mean rate, or “ballpark heart rate”. ○ LEAST accurate method, and MUST be used in addition to the “memory” or “little block” method. ● Memory Method → count the # of BIG boxes between QRS complexes, & then go to that same number on the sequence below (that’s your heart rate). ○ FASTEST method, widely used in hospitals. ● Little Block Method ○ Used to calculate HEART RATE RANGES in irregular rhythms. - Find 2 consecutive QRS complexes that are FARTHEST apart & find the heart rate– this will be your slowest rate. - Find 2 consecutive QRS complexes that are CLOSEST apart & find the heart rate– this will be your fastest rate. REGULARITY TYPES To determine regularity of a rhythm, compare the # of little blocks within an R-R interval. ● REGULAR → ± 1-2 little boxes between R-R intervals. ○ To calculate heart rate– use the LITTLE BLOCK or the MEMORY method! ● REGULAR BUT INTERRUPTED → regular rhythm that contains either a “premature beat” or “pause”. ○ Every other R-R interval MUST be regular (± 1-2 little boxes)! ○ PREMATURE BEATS → to calculate heart rate, IGNORE the premature beat, & use the LITTLE BLOCK or MEMORY method! - Premature beats don’t impact the heart rate as much, since they are typically followed by a short pause to make up for the prematurity. ○ PAUSES → to calculate heart rate, use the 6-SECOND STRIP to find the mean rate, and then use either LITTLE BLOCK or MEMORY to calculate the lower & upper range of the heart rate. - Find 2 consecutive QRS complexes that are FARTHEST apart & find the heart rate– this will be your slowest rate. - Find 2 consecutive QRS complexes that are CLOSEST apart & find the heart rate– this will be your fastest rate. ● IRREGULAR → R-R intervals may vary throughout the strip; it’s unpredictable and all over the place. ○ To calculate heart rate– use the 6-SECOND STRIP to find the mean rate, and then use either LITTLE BLOCK or MEMORY to calculate the lower & upper range of the heart rate. - Find 2 consecutive QRS complexes that are FARTHEST apart & find the heart rate– this will be your slowest rate. - Find 2 consecutive QRS complexes that are CLOSEST apart & find the heart rate– this will be your fastest rate. Chapter 6 - How to Interpret a Rhythm Strip FIVES STEPS to EKG INTERPRETATION