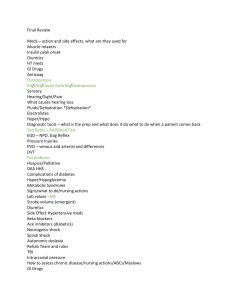
Diuretic Drugs: Pharmacology & Nursing Process
advertisement

Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 28: Diuretic Drugs Key Points Anatomy, Physiology, and Pathophysiology Overview Diuretics are drugs that accelerate the rate of urine formation via a variety of mechanisms, resulting in the removal of sodium and water from the body. The five main types of diuretics are carbonic anhydrase inhibitors, loop diuretics, osmotic diuretics, potassium-sparing diuretics, and thiazide and thiazide-like diuretics. The loop, potassium-sparing, and thiazide diuretics are the most commonly used. Remember that the loop diuretics are more potent than the thiazides, combination diuretics, and potassium-sparing diuretics. The Seventh Joint National Committee on the Detection, Evaluation, and Treatment of Hypertension reaffirmed the role of diuretics, especially the thiazides, as first-line drugs in the treatment of hypertension. All diuretics work primarily in the kidney. The kidney filters out toxic waste products from the blood while simultaneously conserving essential substances. This delicate balance between elimination of toxins and retention of essential chemicals is maintained by the nephron. The nephron is the main structural unit of the kidney, and each kidney contains approximately 1 million nephrons. The initial filtering of the blood takes place in the glomerulus, a cluster of capillaries surrounded by the glomerular capsule. The rate at which this filtering occurs is referred to as the glomerular filtration rate and it is used as a gauge of how well the kidneys are functioning as filters. It is important to have a thorough knowledge of renal anatomy and physiology and how it relates to the action of the various diuretics; for example, if a loop diuretic is given, its site of action is the loop of Henle and it causes the excretion of sodium, potassium, and chloride into the urine. Pharmacology Overview The various diuretics are classified according to their sites of action within the nephron, their chemical structure, and their diuretic potency. The most potent diuretics are the loop diuretics, followed by mannitol, metolazone (a thiazide-like diuretic), the thiazides, and the potassium-sparing diuretics. The potency of these diuretics is a function of where they work in the nephron to inhibit sodium and water resorption. The more sodium and water they inhibit from resorption, the greater the amount of diuresis and therefore the greater the potency. Carbonic Anhydrase Inhibitors Copyright © 2020 Elsevier Inc. All Rights Reserved. Key Points 28-2 Carbonic anhydrase inhibitors (CAIs) are chemical derivatives of sulfonamide antibiotics. They inhibit the activity of the enzyme carbonic anhydrase, which is found in the kidneys, eyes, and other parts of the body. The carbonic anhydrase system in the kidney is located just distal to the glomerulus in the proximal tubules, where roughly two thirds of all sodium and water is resorbed into the blood. For sodium and water to be resorbed back into the blood, hydrogen must be exchanged for it. The CAIs reduce the formation of hydrogen (H+) and bicarbonate (HCO3–) ions from carbon dioxide and water through the noncompetitive, reversible inhibition of carbonic anhydrase activity, resulting in a reduction in the availability of the ions, mainly hydrogen. An undesirable effect of CAIs is elevation of the blood glucose level and glycosuria in diabetic patients. This may be due in part to CAI-enhanced potassium loss through the urine. Therapeutic use of CAIs is in treatment of glaucoma, edema, and high-altitude sickness. Undesirable effects are metabolic abnormalities such as acidosis and hypokalemia, as well as drowsiness, anorexia, paresthesias, hematuria, urticaria, photosensitivity, and melena. Because CAIs can cause hypokalemia, an increase in digoxin toxicity may occur when they are combined with digoxin. Use with corticosteroids may also cause hypokalemia. Loop Diuretics Loop diuretics (bumetanide, ethacrynic acid, furosemide, and torsemide) are very potent diuretics. Loop diuretics have renal, cardiovascular, and metabolic effects. These drugs act primarily along the thick ascending limb of the loop of Henle, blocking chloride and, secondarily, sodium resorption. They are also thought to activate renal prostaglandins, which results in dilatation of the blood vessels of the kidneys, the lungs, and the rest of the body. Loop diuretics are used for edema associated with heart failure and hepatic or renal disease, hypertension, and to increase the renal excretion of calcium in patients with hypercalcemia. They may also be indicated for heart failure resulting from diastolic dysfunction. Loop diuretics produce a potent diuresis and subsequent loss of fluid. The resulting decreased fluid volume leads to a decreased return of blood to the heart, or decreased filling pressures resulting in reduced blood pressure, pulmonary vascular resistance, systemic vascular resistance, central venous pressure, and left ventricular end-diastolic pressure. Loop diuretics are particularly useful when rapid diuresis is needed because of their rapid onset of action. The diuretic effect lasts at least 2 hours. Loop diuretics have a distinct advantage over thiazide diuretics in that their diuretic action continues even when creatinine clearance decreases below 25 mL/min. The major adverse effect of loop diuretics is electrolyte disturbances. Prolonged administration of high dosages can also result in hearing loss stemming from ototoxicity. Copyright © 2020 Elsevier Inc. All Rights Reserved. Key Points 28-3 Hypokalemia is of serious clinical importance. To prevent hypokalemia, patients often receive potassium supplements along with furosemide. Electrolyte loss and dehydration, which can result in circulatory failure, are the main toxic effects of loop diuretics that require attention. Treatment involves electrolyte and fluid replacement. Furosemide can produce erythema multiforme, exfoliative dermatitis, photosensitivity, and in rare cases, aplastic anemia. Furosemide has a black box warning regarding fluid and electrolyte loss. Torsemide may rarely cause blood disorders, including thrombocytopenia, agranulocytosis, leukopenia, neutropenia, and Stevens-Johnson syndrome. Loop diuretics exhibit both neurotoxic and nephrotoxic properties, and they produce additive effects when given in combination with drugs that have similar toxicities. Loop diuretics also affect certain laboratory results, increasing serum levels of uric acid, glucose, alanine aminotransferase, and aspartate aminotransferase. Osmotic Diuretics The osmotic diuretics include mannitol, urea, organic acids, and glucose. Mannitol is the most commonly used of these drugs. Mannitol works along the entire nephron, but primarily in the proximal tubule and descending limb of the loop of Henle. Because it is not absorbed, it increases osmotic pressure in the glomerular filtrate, which in turn pulls fluid into the renal tubules from the surrounding tissues. This process also inhibits the tubular resorption of water and solutes, which produces a rapid diuresis. Mannitol may induce vasodilation and in doing so increases both glomerular filtration and renal plasma flow, making it an excellent drug for preventing kidney damage during acute renal failure. It is commonly used in the treatment of patients in the early, oliguric phase of acute renal failure. Mannitol is also often used to reduce intracranial pressure and cerebral edema resulting from head trauma. In addition, mannitol treatment may be tried when elevated intraocular pressure is unresponsive to other drug therapies. Significant undesirable effects of mannitol include convulsions, thrombophlebitis, and pulmonary congestion. Other less significant effects are headaches, chest pains, tachycardia, blurred vision, chills, and fever. Potassium-Sparing Diuretics The currently available potassium-sparing diuretics are amiloride, spironolactone, and triamterene. These diuretics are also referred to as aldosterone-inhibiting diuretics because they block the aldosterone receptors. Spironolactone is a competitive antagonist of aldosterone, and for this reason it causes sodium and water to be excreted while potassium is retained. It is the most commonly used of the three drugs. Potassium-sparing diuretics work in the collecting ducts and distal convoluted tubules, where they interfere with sodium-potassium exchange. Spironolactone competitively binds to aldosterone receptors and therefore blocks the resorption of sodium and water that is induced by aldosterone secretion. Copyright © 2020 Elsevier Inc. All Rights Reserved. Key Points 28-4 The potassium-sparing diuretics are relatively weak compared with the thiazide and loop diuretics. When diuresis is needed, they are generally used as adjuncts to thiazide treatment. This combination is beneficial in two respects. First, the drugs have synergistic diuretic effects; second, the two drugs counteract the adverse metabolic effects of one another. The thiazide diuretics cause potassium, magnesium, and chloride to be lost in the urine, and the potassium-sparing diuretics counteract this by elevating the potassium and chloride levels. Spironolactone and triamterene are used to treat hyperaldosteronism and hypertension and to reverse the potassium loss caused by the potassium-wasting (e.g., loop, thiazide) diuretics. Permanent ventricular myocardial wall damage, known as remodeling, may follow myocardial infarction. Various clinical trials have demonstrated a cardioprotective benefit of spironolactone in preventing this remodeling process due to aldosterone-inhibiting activity. Spironolactone can cause gynecomastia, amenorrhea, irregular menses, and postmenopausal bleeding. Triamterene may reduce folic acid levels and cause the formation of kidney stones and urinary casts. It may also precipitate megaloblastic anemia. Hyperkalemia may occur when potassium-sparing diuretics are used in combination with each other and/or with other potassium-sparing drugs such as angiotensin-converting enzyme (ACE) inhibitors. Thiazide Diuretics Thiazide diuretics are benzothiadiazines, chemical derivatives of sulfonamide antibiotics. The thiazide diuretics include chlorothiazide and hydrochlorothiazide. Hydrochlorothiazide is the most commonly prescribed and the least expensive of the thiazide diuretics. The thiazide-like diuretics are very similar to the thiazides and include chlorthalidone, indapamide, and metolazone. The primary site of action of thiazides and thiazide-like diuretics is the distal convoluted tubule, where they inhibit the resorption of sodium, potassium, and chloride, resulting in osmotic water loss. As renal function decreases, the efficacy of thiazides diminishes because delivery of the drug to the site of activity is impaired. The thiazide and thiazide-like diuretics are used in the treatment of edema of various origins, idiopathic hypercalciuria, and diabetes insipidus, in addition to hypertension. They are also used as adjunct drugs in the management of heart failure and hepatic cirrhosis. Major adverse effects of the thiazide and thiazide-like diuretics relate to electrolyte and metabolic disturbances—mainly reduced potassium levels and elevated levels of calcium, lipids, glucose, and uric acid. Other effects, such as gastrointestinal disturbances, skin rashes, photosensitivity, thrombocytopenia, pancreatitis, and cholecystitis, are less common. Dizziness and vertigo are common adverse effects of metolazone therapy and are attributed to sudden shifts in the plasma volume brought about by the drug. Headache, impotence, and decreased libido are other important adverse effects of these drugs. Copyright © 2020 Elsevier Inc. All Rights Reserved. Key Points 28-5 Nursing Process Perform a physical assessment and document all findings, with emphasis on the body systems affected by the disease process or indication for the diuretic and by potential drug-related adverse effects. Baseline assessment needs to include auscultation of breath sounds and heart sounds, determining neurologic status and checking skin turgor (for edema or dehydration), moisture levels of mucus membranes, and capillary refill. Assess and document the patient’s baseline fluid volume status and postural blood pressures before and during drug therapy because of diuretic-induced fluid volume loss. Methods for monitoring excess and deficit fluid volume states include assessment of skin and mucous membranes, blood pressure, pulse rate, intake and output, and daily weights. With diuretics, always be concerned about the more vulnerable patient populations, such as the older adult patient, those with chronic illnesses, and patients with altered renal or liver function. Carbonic anhydrase inhibitors require close assessment of sodium and potassium levels. These drugs are not to be used in patients with a history of renal or liver dysfunction. There is increased risk for digoxin toxicity with diuretics that result in loss of potassium. Loop diuretics are more potent than thiazide diuretics, combination products, and potassium-sparing diuretics, so these drugs may pose more problems for the elderly or those with severe electrolyte loss and liver failure. Use caution in administering loop diuretics with other medications that are neurotoxic or ototoxic. With potassium-sparing diuretics, hyperkalemia may be an adverse effect; therefore, assess the patient’s serum levels of potassium. Potassium supplements, ACE inhibitors, and severe renal failure are contraindications. Emphasize the importance of taking diuretics at the same time every day. These drugs are generally ordered to be taken in the morning to help prevent nocturia, which may result in lack of sleep. Measure and record blood pressure, pulse rate, intake and output, and daily weights during diuretic therapy. Monitor for the presence of dizziness, fainting, lightheadedness on standing or changing positions, weakness, fatigue, tremor, muscle cramping, changes in mental status, or cold clammy skin. Diuretic therapy may also precipitate cardiac irregularities or palpitations; therefore, continue to monitor heart rate and rhythm. Fluid loss from the action of the diuretic may lead to the adverse effect of constipation so that preventative measures are required, such as increased intake of fluids and fiber (unless contraindicated) and/or the use of natural bulk-forming products. The therapeutic effects of diuretics include the resolution of or reduction in edema, fluid volume overload, heart failure, or hypertension, or a return to normal intraocular pressures. Monitor the patient for the occurrence of adverse reactions to the diuretics, such as hypotension, electrolyte imbalances, metabolic acidosis, drowsiness (with CAIs), hypokalemia, tachycardia, and hyperkalemia (potassium-sparing diuretics). Copyright © 2020 Elsevier Inc. All Rights Reserved.