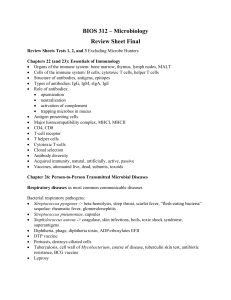
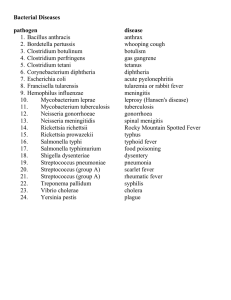
MDN 2341: Medical Microbiology and Immunology Dr. Kherie Rowe MDN 2341 : Medical Microbiology and Immunology * 1 Bacteriology Upper Respiratory Tract Infections (URTIs) Learning objectives • Identify the most common bacteria that cause infections in the upper respiratory tract • Compare the major characteristics of specific bacterial diseases of the upper respiratory tract • Identify the means of diagnosis and culture of the bacteria that could cause upper respiratory tract infections. • Describe the possible means of treatment of prevention of infection. Upper respiratory tract infections (URTIs) • Streptococcus pyogenes (strep throat) • Corynebacterium diphtheria • Haemophilus influenzae • Streptococcus pneumoniae • Bordetella pertussis PHARYNGITIS Streptococcal pharyngitis (Strep throat) • High fever – >100.4 0F ( 38oC) • Intense pharyngeal pain (sore throat) • Erythema (associated with pharyngeal inflammation) • Swollen tonsils with exudate (pus) • Petechiae (pin-point red patches) on the soft or hard palate • Cervical lymphadenopathy (swollen submandibular lymph nodes) • Swollen uvula Streptococcal pharyngitis (strep throat) The mucosal membranes are damaged by the release of a variety of exoenzymes and exotoxins by this extracellular pathogen. Many strains of S. pyogenes can degrade connective tissues by using hyaluronidase, collagenase and streptokinase. Streptokinase activates plasmin, which leads to degradation of fibrin and, in turn, dissolution of blood clots, which assists in the spread of the pathogen. Released toxins include streptolysins that can destroy red and white blood cells. Streptococcus pyogenes Pathogenesis Streptococcus pyogenes GAS: Group A streptococcus 5-15% of individuals harbor S. pyogenes within the respiratory tract Pathogenesis (inflammation and cell destruction) in pharyngitis is mediated by the release of several exoenzymes and exotoxins: Hyularonidase Collagenase Streptokinase Streptolysin DNAse Protein Activity Interest Hyaluronic acid capsule Antiphagocytic Same as human hyaluronic acid in basement membrane; antibody cross-reactivity M protein Fimbral protein binds fibronectin, blocks complement C3b (inhibiting opsonization and lysis) Cross reactive epitope with cardiac myosin F protein Adhesin Binds fibronectin, associated with M protein. Hyaluronidase Degrades hyaluronic acid Invasion Streptokinase Dissolves fibrin clots “Clot buster” drug Pyrogenic exotoxins (Erythrogenic toxins) Spe A SpeB Cysteine protease SpeC Scarlet fever, TSST of GAS, necrotizing fasciitis Superantigens erythematous skin reactions, pyrogenicity, specific and nonspecific T-cell mitogenicity, immunosuppression Streptolysin O Oxygen labile hemolysin Hemolysis Streptolysin S Oxygen stable hemolysin Responsible for beta hemolysis. Transmission • Can be spread through direct contact or via aerosol droplet spread (coughing and sneezing) • Children (5-15 years old) are usually at higher risk for contracting strep throat. – Overcrowded conditions are a predisposing factor – Prevalent during winter and spring Clinical presentation Differential diagnosis Lab diagnosis and identification • Rapid enzyme immunoassay for Group A antigen (false negatives occur frequently ~30%) • Specimens: throat swab or pus. – Culture (growth on sheep blood agar) – Microscopy Gram positive cocci in chains Beta-hemolysis on SBA Bacitracin sensitive Catalase negative Lab diagnosis and identification Lab diagnosis and identification Treatment and prevention • • • Antibiotic resistance is limited. Beta-lactams continue to be effective: – Oral amoxicillin (children) – Intramuscular penicillin G For those with penicillin allergies: – Cephalosporin – Macrolides (Erythromycin) Scarlet Fever • Caused by strains of streptococci which carry a lysogenic bacteriophage that codes for pyrogenic toxins which are also erythrogenic. • 1 or 2 days after pharyngitis, streptococci release toxins that trigger fever and a rash that starts on the chest and spreads across the body. Sandpaper-like rash Strawberry tongue Complications • Non-suppurative sequelae – May occur 1-4 weeks following inadequate treatment of GAS infection of the respiratory tract and skin. – This period of latency suggests a hypersensitivity response (TYPE II and III) to streptococcal products – Glomerulonephritis may follow throat or skin infections, whilst rheumatic fever follows only throat infections. Rheumatic fever • Rheumatic fever can result from infection by any of the serotypes of S. pyogenes. • Onset of the condition usually occurs 14 weeks (20 days) after pharyngitis caused by GAS. • It may result in damage to the heart valves and muscle. • Characterized by fever, polyarthritis, carditis, erythema marginatum, Sydenham chorea. • Common in children between 5-15. Rare in children under 3 and adults. • Type II hypersensitivity Rheumatic Fever • Major and minor criteria diagnosis for rheumatic fever • Rising antistreptolysin O (ASO) titer • Management: – Aspirin – Corticosteroids – Positive throat culture: antibiotics • Jones criteria Rheumatic Fever Glomerulonephritis • Develops 3 weeks after infection with Streptococci (types 2, 4, 12 or 49)mostly associated with skin infections. • Children are more likely to develop this complication • Characterized by fever, edema, elevated BUN, hematuria (smoky urine), high blood pressure, low serum complement levels. Blood casts in the urine. • Condition is due to Ag-Ab complex deposition on the glomerular basement membrane. (Type III hypersensitivity) Glomerulonephritis • Anti-DNase B titer OTITIS MEDIA OTITIS MEDIA • Otitis media is an inflammatory condition that affects the middle ear. • Acute otitis media is an infection with rapid onset that usually presents with ear pain (otalgia). • In young children, this may result in the pulling of the ear, increased crying and poor sleep. • Fever, anorexia, vomiting and lethargy may also present. Red, bulging tympanic membrane OTITIS MEDIA • Most common causes of bacterial infection are Haemophilus influenzae (non-typeable strains) and Streptococcus pneumoniae. • Infection is primarily seen in children between 6 months to 12 years of age. • More than 90% of H. influenza strains are non-typeable. Streptococcus pneumoniae • • • • • Encapsulated Non-pyogenic (non-pus forming bacterial infections) Alpha-hemolytic Normal inhabitant of the upper respiratory tract Carrier rate is 20-40% Streptococcus pneumoniae • • • • • • • • • • • • Gram positive Catalase negative Lancet shaped diplococci Facultative anaerobe Non-motile Do not display M protein Capsulated in animal tissues Ferment glucose to lactic acid Bile soluble Optochin sensitive Quellung test positive Capnophilic (grows best in 5% carbon dioxide) Risk factors for infection • • • • • • • • • • Reduced disease resistance Viral respiratory infections Excessive smoking Alcoholism Malnutrition COPD (chronic obstructive pulmonary disease) Complement deficiencies (C3b) Splenectomy Sickle cell anemia Leading cause of bacterial disease in children and the elderly Pathogenesis • • • • Does not produce toxins Pathogenicity is related to the presence of the capsule Enables tissue invasion and evasion of the immune response Other important virulence factors include: – IgA protease – Teichoic acid – Pneumolysin O: released with bacterial death, damages respiratory epithelium.. Pathogenesis Lab diagnosis and identification • Specimens: throat swab or pus: – Culture (growth on sheep blood agar) – Microscopy • Quellung reaction • Latex agglutination • Colonies are bile soluble Gram positive diplococci Alpha-hemolysis on SBA Optochin sensitive Catalase negative Lab diagnosis and identification • Quellung reaction – Swelling of the capsule on exposure to serum containing anticapsule antibodies.(Serotyping) • Latex particle agglutination – Antibody is adhered to latex particles and then used to detect antigen. Prevention • The mortality rate is high in the elderly and infants. • Elderly, immumocompromised and asplenic individuals can be immunized with polyvalent (23) polysaccharide vaccine. (PPV) • It is safe, effective and provides at least 5 years protection. • In infants younger than 5 years, a polyvalent (13) polysaccharide vaccine conjugated to a carrier protein (diphtheria toxoid). (PCV) Haemophilus influenzae • Gram-negative coccobacillus (pleomorphic rod) • Facultative anaerobe • Most strains are opportunistic pathogens – they usually live in their host without causing disease, but cause problems only when other factors (such as a viral infection, reduced immune function or chronically inflamed tissues, e.g. from allergies) create an opportunity. – Transmission is via respiratory droplets; shared toys Haemophilus influenzae • Bacterial culture is achieved on chocolate blood agar with hemin (factor X) and NAD (factor V). • Incubation is best at 37°C in a CO2 enriched environment. • Catalase positive • Oxidase positive • Quellung reaction Quellung reaction Pathogenesis • Haemophilus can be either encapsulated or unencapsulated. • The polysaccharide capsule is the most important determinant of virulence. • There are six capsular serotypes (a-f). Most infections are caused by strains belonging to capsular serotype b. • Unencapsulated strains are part of the normal flora of the URT and cause local mucosal infections but not invasive infections. – Sinusitis, otitis media or bronchitis • IgA protease is also produced. Lab diagnosis and identification • Culture on chocolate agar with factors X and V. • Culture with Staphylococcus aureus on blood agar with X factor (produces satellite colonies) • Latex particle agglutination for capsular antigen detection. • PCR Treatment • Antibiotic sensitivity tests must be done on organisms isolated from serious infections. • Most are susceptible to penicillins (high-dose amoxicillin) • In penicillin-allergic patients, erythromycin or one of its derivatives (azithromycin) can be used. • Vancomycin is the drug of choice for penicillin resistant species. Prevention • Vaccine (protein conjugate) against Haemophilus influenzae type b (Hib). • Antibodies produced against serotype b promote opsonization, complement fixation and phagocytosis and killing. • Vaccination against type b H. influenza is recommended by 2 months old. • Type b is also associated with disseminated disease, pneumonia, epiglottitis and meningitis. Question 1. Microscopic examination of a sputum sample from a 34-yearold male with fever and cough reveals Gram positive lanctshaped cocci in pairs. The bacteria are likely to be : A. B. C. D. E. Catalase positive Optochin resistant Bile soluble Capable of complete hemolysis Bacitracin sensitive Gram positive Lancet shaped diplococci is suggestive of S. pneumoniae. All streptococci are catalase negative. S. pneumoniae is optochin sensitive, exhibits alpha hemolysis and is bacitracin resistant. Hence the answer is: C. DIPHTHERIA Diphtheria Regional lymph nodes are inflamed, sore throat and dysphagia (difficulty swallowing) Pseudomebrane Pseudomembrane is composed of dead cells, fibrin and bacterial pigment. Profuse bleeding occurs if the pseudomembrane is dislodged. Extension of the pseudomembrane into the trachea can cause obstruction. Diphtheria • In severe cases, the exotoxin may diffuse into the neck tissue. • This produces severe edema (bull neck). • Enlarged cervical lymph nodes ( cervical lymphadenopathy) Corynebacterium diphtheriae • Aerobic, Gram-positive bacillus • Irregularly shaped rod (club-shaped) – arranged in V or L shapes • • • • • Non-motile Non-spore forming Non-capsulate Causative agent of diphtheria Grows on Löffler’s medium Corynebacterium diphtheriae • Pre-school age children are at highest risk of contacting the bacterium • Prevalent in autumn and winter months • Humans are the chief reservoirs (throat, nasopharynx) • Transmission is via secretions from an infected person (aerosol droplets) or by direct contact. • May enter by the respiratory tract or by the conjunctiva or an open wound. Risk Factors • Low VACCINE coverage among infants and children • Lack of mass immunization programs amongst children and adults at high risk • Poor nutrition • Community outbreaks • Crowded or unsanitary living conditions Clinical manifestations • Incubation period : 2-5 days • Prodrome: fever (39°C), malaise, anorexia (loss of appetite), sore throat, headache. • Child appears very ill and toxic • Complications: – Airway obstruction – Delirium – Circulatory collapse (myocarditis) Pathogenesis • Upon entry, the bacilli multiply in the throat and secrete a powerful EXOTOXIN. • This exotoxin production stimulates both local and systemic inflammation. • Local: – Causes necrosis of epithelial cells and liberates serous and fibrinous material which forms a grayish-white PSEUDOMEMBRANE. – The membrane bleeds on being dislodged. – Surounding tissues are inflamed and edematous Pathogenesis • Toxin production only occurs when the bacterium is infected with bacteriophage carrying the tox gene (toxigenic strains). • It is an ADP- ribosyltransferase that inhibits host protein synthesis. • Inactivates EF-2 by ADP ribosylation • Diphtheria toxin is an A-B toxin. – Portion A mediates the enzymatic activity that prevents protein synthesis – Portion B binds to the cell receptor and mediates translocation of Portion A into the cytosol. Other examples of lysogenic infection Pathogenesis Pathogenesis Pathogenesis • Systemic: – Exotoxin can affect the heart, kidneys and CNS. – Heart: Conduction disturbance (myocardial fibers are degenerated and the heart is dilated) – Kidneys: Renal tubular necrosis – CNS: Polyneuritis Diagnosis and identification • Albert’s staining [specific to volutin (metachromic) granules found in Corynebacterium diphtheriae] • Club shaped rods present • Non-motile • Non-encapsulated • Tellurite (Loeffler’s medium) agar (gray-to-black colonies) • Elek test (toxigenic strains) Diagnosis and identification Elek test • The test colony, along with a positive and negative control are streaked onto the Elek agar plate. • Filter paper strip with the antitoxin is placed on an agar plate. • As the antitoxin diffuses away from the strip, precipitin lines form at the zone of equivalence (Ag-Ab precipitation). • ELISA test is now more commonly used. Treatment • Neutralization of free circulating toxin by the administration of antitoxin. • Administration of antibiotics to eradicate bacteria (erythromycin) • Supportive and symptomatic therapy • Management of complications. Treatment • Antitoxin administration – Pharyngeal or laryngeal diphtheria of 48 hours duration (20, 00040,000 units) – Nasopharyngeal lesions: (40,000-60,000 units) – Extensive disease of 3 or more days with swelling of the neck (80,000-120,000 units) – Antitoxin may be repeated if the clinical improvement is slow Treatment • Antibiotic administration – Procaine penicillin (3-6 lac units IM at 12 hour intervals)-endocarditis – Oral penicillin (Penicillin G) 125-250mg four times a day – Erythromycin (25-30 mg/kg/day) for 14 days • Three negative cultures at 24 hour intervals should be obtained before the patient is declared cured. Complications Prevention • Vaccination: immunization with diphtheria toxoid combined with tetanus and pertussis toxoid (DTaP) should be given to all children at 2, 3 and 4 months of age. • Booster doses are given between the ages of 3 and 5. • Further booster is given before leaving school and is considered protected for a further 10 years.