Marital and Sexual History
advertisement

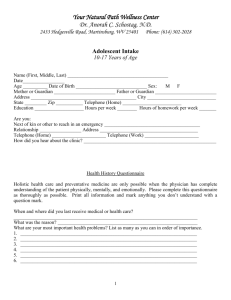
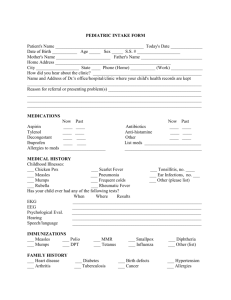
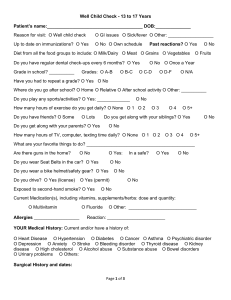
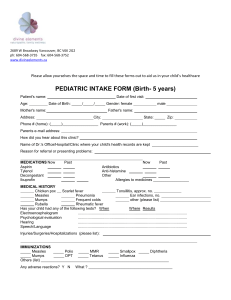
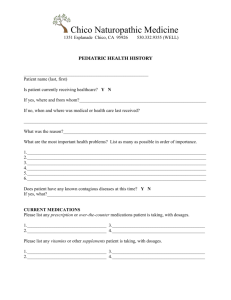
HEALTH HISTORY I. DATE AND TIME OF INTERVIEW II. SOURCE AND RELIABILITY III. GENERAL INFORMATION (Demographic Data) (Identification Data) A. B. C. D. E. F. G. H. I. J. K. L. IV. Name Address Telephone Age Marital Status Occupation Religion Ethnicity Billing Information Source of Referral Date of Last Exam Other: Can include current and/or previous involvement in health care system; i.e., attending physician, clinic/HMO involvement, Visiting Nurse, Home Care Agency, etc. CHIEF COMPLAINT (CC): Main reason for consulting health professional. State briefly in client’s own words (when possible). State onset and duration briefly. V. HISTORY OF PRESENT ILLNESS (HPI): (Narrative format) Needs to be well organized and sequentially developed. Clear, chronological account of problem for which client is seeking care. Should include: A. B. C. D. E. F. G. H. I. Time of onset of complaint (problem) Character of complaint (problem) Mode of onset Location Relationship to other symptoms Exacerbations and remissions Effect of past treatment Relevant diagnostic testing done Significant negatives Note: All principal symptoms should be described in terms of their 1) location, 2) quality, 3) quantity or severity, 4) timing (i.e., onset, duration, frequency), 5) setting, 6 factors that aggravate or relieve symptoms, and 7) associated manifestations. 1 V. PAST HISTORY A. GENERAL STATE OF HEALTH This is often cited briefly in the opening statement of the HPI B. CHILDHOOD ILLNESSES, IMMUNIZATIONS, COMMUNICABLE DISEASES List disease separately and chronological Cite age of occurrence (if known) Ask specifically rheumatic fever, serology for rubella, when last boosters were given, History of polio and any residual disability, exposure to communicable diseases, travel, etc. Note: Communicable disease and travel history are not usually addressed directly in this section which is often limited to Childhood illness and immunizations. With Current lifestyles their inclusion here may be warranted. C. MEDICAL ILLNESSES (HISTORY) List medical illnesses (cite specific detail if indicated) List previous (medical) hospitalizations chronologically (date, place, discharge diagnosis (es) when known, etc. D. SURGICAL HISTORY List chronologically (date, place, procedure done, etc. ) Give specific details of surgery and post-op period (if indicated) E. INJURIES (ACCIDENTS) (TRAUMA) List only those that are significant. Cite type of injury, date, treatment, residual effects, etc. F. PSYCHIATRIC ILLNESSES G. ALLERGIES List allergies to food, pollen, drugs, chemicals, biological. Describe how allergy is manifested (Reaction), treatment history, etc. 2 H. CURRENT MEDICATIONS AND DOSAGES Name, Dose, Route, Frequency List all prescribed and non-prescribed drugs I. DIET AND NURTRITION J. REST AND SLEEP PATTERN K. HABITS 1. 2. 3. 4. 5. Smoking (tobacco) Drinking (caffeine, ethanol, other) Use of drugs (prescribed, non-prescribed, drugs of abuse) Exercise Hobbies VII. FAMILY HISTORY (Genogram required) ** A. Age and health, or age and cause of death, of each immediate family member (ie, parents, siblings, spouse, children). Information re: grandparents and grandchildren also sometimes indicated. This information is to diagrammed B. Occurrence within the family of any of the following is cited. Relationship to the patient is signified. Hypertension, Stroke, Heart Disease, Diabetes, Kidney Disease, Cancer, Anemia, Bleeding Tendency, Tuberculosis, Arthritis, Peptic Ulcer, Hyperlipidemia, Headaches, Mental Illness, or symptoms like those of the patient. VII. PSYCHOSOCIAL HISTORY (PERSONAL AND SOCIAL HISTORY) Outline or narrative format A. Cultural and Social 1. Nationality 2. Religious affiliation and or preferential practices 3 3. Dominant language used. How well does the client understand and use the English language? 4. Cultural Values. Influence of culture on client’s view of family, male and female roles, childrearing practices, use of resources, health and illness behavior. 5. Socioeconomic background (influence of social and economic status on patterns of socialization, family structure, health beliefs, etc. 6. Relationships with significant others and family constellation 7. Membership in professional and social organizations What meaning do these groups have for the client? B. Marital and Sexual History Normal patterns of interaction; feelings toward sexuality; satisfaction with sexual relationships; patterns of closeness, warmth, and companionship with others; changes in sexual response since any change in life style; etc. C. Educational History D. Occupational History Occupation, pattern of employment, occupational hazards and exposure to Irritants, any work related disability, etc. E. Typical Day F. Developmental tasks of the individual (extent met) G. Client’s Perception and Satisfaction with his health status. H. Family’s perception of client’s health problems and its impact on the family I. Environmental factors J. Client’s Health Goals 4 IX. REVIEW OF SYSTEMS 1. GENERAL: weight change, weakness, fatigue, fever, chills, night sweats, sleeping Habits 2. INTEGUMENT (SKIN): rashes, sweating, dryness, color change in hair or nails, Itching, lumps, bleeding tendency/bruising 3. HEAD (CENTRAL NERVOUS SYSTEM): headache, head injury, syncope, seizures, vertigo, paralysis/paresis, tremor, ataxia, dysesthesias 4. EYES: acuity, glasses/contact lenses, prosthetics, last eye exam, pain, redness, excessive tearing, double visison, blurred vision, cataracts, glaucoma 5. EARS: pain, hearing loss, deafness, infection, discharge, tinnitus, ruptured Tympanic membrane 6. NOSE AND SINUSES: nasal stuffiness, frequent colds, sinus trouble, epistaxis olfactory changes, deviated septum, hay fever 7. MOUTH AND THROAT: condition of teeth and gums (caries, extractions, dentures, caps, bleeding gums, pyorrhea), difficulty chewing, date of last dental exam, sore tongue, taste changes, frequent sore throats, coarseness, difficulty swallowing (dysphagia) 8. NECK: lumps in neck, “swollen glands”, goiter (thyroid problem), pain in neck 9. BREASTS: skin changes, pain, nipple changes,lumps (masses),fibrocystic disease, breast cancer history, knowledge of self-exam 10. RESPIRATORY: cough, sputum (color and quantity), hemoptysis, wheezing, dyspnea, pain on respiration, frequent respiratory infections, asthma, bronchitis, emphysema, pneumonia, tuberculosis, exposure to tuberculosis, tuberculin test (date and result) 11. CARDIOVASCULAR: chest pain, typical angina pectoris, palpitations, exertional, dyspnea, orthopnea, paroxysmal nocturnal dyspnea, murmur, rheumatic fever, heart disease, past EKG or other heart tests 12. GASTROINTESTINAL: trouble swallowing (dysphagia), appetite, dietary habits, food intolerance, heartburn (indigestion), abdominal pain, nausea, 5 13. 14. 15. 16. vomiting, vomiting blood (hematemesis), excessive belching or flatus (passing gas), change in bowel habits, diarrhea, constipation, frequency of bowel movements, hemorrhoids, rectal bleeding, black tarry stools (melana), mucous in stool, hernia, liver or gallbladder disease (hepatitis, jaundice, stones), pancreatitis, use of laxatives or antacids URINARY: dysuria (painful urination), frequency, urgency, hesitancy, polyuria, incontinence, decreased urinary stream, nocturia, urinary infections, stones (calculi), prostate problems REPRODUCTIVE: Male: penile discharge or lesion, history of VD and its treatment, serology, hernias, testicular pain, swelling, or masses, infertility, impotence, libido, sexual problems Female: Gynecologic History: age of menarche________, LMP___/___/___, age of menopause ______, Abnormal masses, amount of bleeding (menstrual, intermenstrual, postcoital, postmenopausal), leukorrhea, pruritis, history of VD and its treatment, serology, libido, sexual difficulties, frequency of intercourse, Last PAP:___/__/__,results_____, Obstetric History: pregnancies________, abortions_______,(spontaneous and induced), full term deliveries_______, complications, contraceptive methods__________________ MUSCULOSKELETAL: joint pain, stiffness, swelling (edema), heat, redness (rubor), deformity, stiffness (limited motion/activity), myalgias (muscle pains or cramps), weakness, bone fracture, arthritis, gout, backache, sciatica ENDOCRINE: thyroid disease, goiter, hear or cold intolerance, change in voice, excessive sweating, diabetes, polyuria, polyphagia, polydipsia, (i.e.,excessive urination, hunger,thirst), gynecomastia, hirsutism 17. HEMATOLOGIC (HEMATOPOIETIC): anemia, abnormal bleeding (easy bruising or bleeding), swollen glands (adenopathy), past transfusion and possible reactions 18. PSYCHIATRIC (EMOTIONAL STATUS): nervousness, hyperventilation, tension, mood, depression, insomnia, nightmares, memory loss, phobias 6