Reproductive (Men Only) - Meta
advertisement

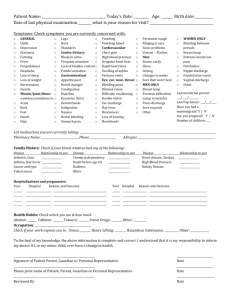
Patient Health Intake Form Note: This is a confidential record of your medical history and will be kept in this office. Information herein will not be released to any person unless you have authorized us to do so in writing. Please complete the questionnaire as thoroughly as possible. Thank you! PERSONAL INFORMATION (Name)Last, First, MI____________________________________________DOB_______ Age _____ Address: St.___________________________Apt#_____City _______________St. ____ Zip _______ Phone (day) _________________ (cell) _______________Occupation_________________________ Marital status _______________ SS#___________________________ Emergency Contact: _________________________________ Ph#_________________________ Primary Insurance Information (Please bring your ins. card with you) Insurance Company:_____________________________ Ins Co. PH # _________________________ Insured Name:____________________________ DOB___________ SS#_______________________ Employer:____________________________ PH:#___________________ Relationship to patient: ______________________ What are your major health concerns that have brought you to seek medical attention? ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ When did this begin? _______________________________________________________ ________________________________________________________________________ Has anything recently changed or become worse? ________________________________ ________________________________________________________________________ ________________________________________________________________________ Have you had a diagnosis? If so, what was it, how was it arrived at, and by whom? _____ ________________________________________________________________________ Are you currently receiving care from any other health professional? Name: ___________________________________________________________________ What condition(s)? _________________________________________________________ Are you currently taking any medications, prescription or otherwise? YES ____ NO _____ Please list them: ___________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ Do you have any infectious diseases that you know of? YES _____ NO _____ If yes, please list them: __________________________________________________________________________________________ ____________________________________________________________________________________ Are you pregnant? YES/NO If yes, how many months?____ What is your anticipated delivery date: ___________ 1 Do you have any known allergies or sensitivities? If so, please list them:____________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ Is there any reason why you could not take remedies made in alcohol? ________________________________________________________________________ Have you ever been hospitalized or had any surgeries? If so, please note date and reason: ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ FAMILY MEDICAL HISTORY Please complete this section only for family members with particular health issues. AGE (If deceased, age at death and cause) HEALTH PROBLEMS: Father: ___________________________________________________________________ Mother:___________________________________________________________________ Brothers/__________________________________________________________________ Sisters:____________________________________________________________________ Children:___________________________________________________________________ Other close blood relatives:_______________________________________________________________ PERSONAL HEALTH / HABITS Height ________ Current weight ________ Weight 1 year ago __________ Do you smoke? ________ How many years? ________ Amount daily ________ Do you drink alcohol? ________ What? ________ Frequency ________ Do you use recreational drugs? ________ What? ________ Frequency ________ Do you drink coffee? ________ How many oz? ________ Tea? ________ How much? ________ Do you exercise regularly? Yes_____ No _____ Frequency? __________________________ Type of exercise? _____________________ Duration? _______________________________ Occupational Concerns Stress Hazardous Substances Heavy Lifting Your Occupation _________________________________ Other HEALTH CONCERNS: Check off any experienced in the last year: SKIN & HAIR: Change in skin texture Hives Rashes Eczema Pimples Itching Hair Loss Change in Moles Scars Bruises Easily Poor healing sores 2 EYES, EARS, NOSE & THROAT Poor vision Cataracts Glaucoma Earaches/Discharge Blurred vision Poor hearing or Loss Ringing in the ears Sore throat Canker sores Cold sores Grinding teeth Nose bleeds Facial pain Clicking jaw Eye pain Sinus congestion Mucous in throat Swollen glands Ear infections Dizziness Frequent colds Spots in front of eyes Bleeding gums Crossed eyes Difficulty swallowing Double vision Hay fever Hoarseness Persistent cough Vision – flashes/Halos High Blood Pressure Low Blood Pressure Chest pain Irregular heart beat Fainting Palpitations Cold hands or feet Poor circulation Rapid heart beat Swelling of feet/ankles Varicose veins Other:___________________________ Cough Bronchitis Asthma Coughing blood Pneumonia Pain on breathing CARDIOVASCULAR RESPIRATORY Shortness of breathe without exertion Difficulty breathing when lying down Production of phlegm YES ____ NO ____ If yes, what color? _______________ Other: _____________________________________________________________ GASTROINTESTINAL Nausea Hemorrhoids Black stools Constipation Excessive hunger Indigestion Abdominal pain Difficulty swallowing Mucous in stools Blood in stools Vomiting Gas Poor appetite Bad breathe Bloating Heartburn Food allergies Diarrhea Rectal pain/bleeding Bowel changes Excessive thirst Stomach pain Vomiting blood Other: _______________________________ # of bowel movements daily ______________ Loose Normal Hard 3 URINARY Painful urination Frequent urination Blood in urine Urinary urgency Kidney stones Irregular flow Incontinence Inability to hold urine Decreased flow Frequent Infections Difficulty starting/stopping slow Other: _________________________________________________________ MUSCULOSKELETAL-Pain, Weakness or Numbness Neck Hand Shoulder/Arm Back Leg/Foot Reduced range of motion Other:_______________________________________________________ Do you see a chiropractor or massage therapist? Yes / No (Name) ______________________ For how long? _________________ REPRODUCTIVE (Women Only) Age at first menses: _______________ Date of Last Pap Smear__________________ Length of cycle: ___________________ Mammogram _________________ Duration of bleeding: _________________ Heavy bleeding Cramps Breast lumps Pain with intercourse Vaginal Discharge Clots Unusual bleeding Irregular cycles Color: Brown / Black / Bright Red Abnormal Pap Smear Extreme Menstrual Pain Hot Flashes Nipple Discharge Migraines (Yes / No) Duration/frequency: _______________________________________________ PMS? If yes, what symptoms and how long before cycle do they start?___________________________ ____________________________________________________________________________________ ____________________________________________________________________________________ # of pregnancies _______ # of births ____ # of miscarriages _______ Premature births ________ Type of birth control used: ______________________________________________________________ Any other gynecological problems? ______________________________________________________ Reproductive (Men Only) Breast Lump Penis discharge Lump in Testicles Erection difficulties Sore on penis Other: ____________________________ 4 NEUROPSYCHOLOGICAL Poor sleep Loss of balance Other: _________________________ Depression Poor memory Numbness Seizures Irritability Anxiety Headaches High stress levels Migraine Lack of coordination Difficulty concentrating “Spacey” / foggy feeling Hours of sleep per 24 hour day _____________________________ When?: AM PM Shift work GENERAL Fatigue Depression Headaches Fevers Sweats/ Night sweats Dizziness Loss of Sleep Excessive thirst Slow metabolism Fainting Chills Weight loss Sudden energy drops Forgetfulness Nervousness Weight gain Intolerance to heat/cold Other:___________________________ CONDITIONS Aids Cancer Heart Disease Multiple Sclerosis Alcoholism Cataracts Hepatitis Pacemaker Anemia/Bulimia Chemical Dependency Herpes Pneumonia Anorexia Diabetes High Cholesterol Prostate Problem Appendicitis Emphysema HIV Positive Psychiatric Care Arthritis Epilepsy Kidney Disease Rheumatic Fever Asthma Glaucoma Liver Disease Scarlet Fever Bleeding Disorders Goiter Migraine Headaches Stroke Breast Lump Gonorrhea Miscarriage Suicide Attempt Bronchitis Gout Mononucleosis Thyroid Problem Tonsillitis Chicken Pox Measles Mumps Tuberculosis Polio Typhoid Fever Ulcers Vaginal Infections Venereal Disease I certify that the above information is correct to the best of my knowledge. I will not hold my doctor or any members of his/her staff responsible for any errors or omissions that I may have made in completion of this form. Signature _______________________________________________ Date __________________________ Reviewed _______________________________________________ Date __________________________ 5 In addition to the above information, please include the following: - 3-5 day diet diary, including snacks and water intake - Supplements taken (both vitamins and herbal) Include name of supplement Manufacturer’s name How many mg/mcg/iu in each tablet/capsule Dosage: how many YOU take per day - Copies of any recent lab work (within one year) Notes:______________________________________________________________________________________ ____________________________________________________________________________________________ ____________________________________________________________________________________________ Payment Policy All copays are due and payable at each visit. There is an additional $5 charge if you forget your copay. There is a $25 NSF charge for any returned check. There is a $25 No Show charge for any missed appointment that was not cancelled prior to the appointment. There is also a $100 No Show charge for a missed appointment with a LifeStyle Educator. Please be considerate and call at least 24 hours in advance if you cannot make your appointment. If you are a private paying patient without insurance, all charges are due at the time of service. We do not send statements to private paying patients. Prescription Policy Please do not wait until your last pill to call for a refill. There is a 24 HOUR turn around time for the nurses to call the pharmacy. If you have not seen the Doctor in six months, the request for the prescription will be denied. Assignment of benefits are payable to Dr. Kenneth C. Browning. “I have read and understand the procedures and policies described above.” Signature: ____________________________________ Date: ___________________________ 6