Burn Injuries: Classification, Stages, and Management
advertisement

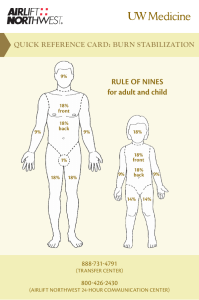
BURN INJURIES Burn is one of the common condition that is being brought in the hospital / E.R ● Cell destruction of the layers of the skin and the resultant depletion of fluid and electrolytes. - When patient have burns, they have problems in fluid and electrolytes Burn size 1. Small burns: body's response is localized to the injured area. - Burn on extremities 2. Large or extensive burns: a. consist of 25% or more of the total body surface area (TBSA) yung response is systemic b. body's response to injury is systemic c. affect all of the major systems of the body - Most of the major organs in the body will response especially to the response in inflammatory - Response of the major organ in the body - Whenever you have 25% TBA, brain will response → brain will secrete ADH (brain is trying to compensate by secreting ADH) → because technically, patient is depleting fluid (intravascular compartment walang laman / kulang kidney is compromised to receive oxygenated blood), the kidney will secrete renin angiotensin → will be converted to angiotensin 1 and later on will convert to angiotensin 2 into the lungs via ACE (which is powerful vasoconstrictor) - The heart will response → whenever to have decrease blood pressure → body will try to compensate by increasing cardiac rate → tachycardia will evident to patient with burn FACTORS THAT DETERMINE SERIOUSNESS OF BURN 1. Depth - lalim ng burn 2. Amount if surface area - if it is consist of 25% or more -it will become more serious 3. Involvement of critical area affectation of the face → affectation of the lungs (because upper airways is present in the face - nose and mouth) - Whenever you have scalding burn → nasinghot sobrang init na fumes → hindi lang burn sa mukha, burn also in passage airway - Affectation to face, bring patient to the nearest hospital for proper observation because inflammation will happen several hours after the burn injury 4. Patient's age - sobrang bata, the body will not be able to respond. - Sobrang tanda, meaning 60 years old pataas → considered as major type of burn (kahit less than 25% TBSA lang) 5. Patients general health - Whenever patient has comorbidities - Example:patient is suffering with MI, renal failure, diabetes - Patient with heart failure or renal failure → sobrang hirap, because we will do fluid challenge (the patient will do fluid challenge then later on will be subject to fluid dialysis? Quite hard to manage those patient) → usually patient die several hours after burn because very limited access in line with the management STAGES OF BURNS 1st stage ● Shock/fluid accumulation - During burn, there’s depletion in fluids together with electrolytes - ● ● ● ● ● ● ● Fluid is shifting from one compartment to another compartment → from intravascular compartment to intracellular compartment that’s why there’s inflammation 1st 48 hours IVC - ISC Generalized DHN Hypovolemia, hpn - Hypovolemia because the fluid technically was not in the intravascular compartment - Hypovolemia leading to hypotension → evaluate and analyze the laboratory examination of patient → might be appreciate increased in hematocrit Hemoconcentration, Increased hematocrit - Puro dugo - Mataas ang hematocrit because of lacking in fluid components into intravascular compartment oliguria → decreased perfusion, increase ADH, aldosterone - Oliguria because the kidney was being deperfuse, less perfusion in the kidney because of the systemic peripheral vascular resistance HyperK, hypoNa - Technically, walang blanket → yung tubig, tumatapon nang tumatapon → continuously with atmospheric air, nagde-deplete ang fluid because do not have skin → kaya kahit may aldosterone, di kaya protektahan si sodium - Shifting of fluids (IVC -ISC) → Sodium in intracellular compartment which is full of water because fluid shifting → sodium is ultradiuted in that area → nawawala ang power of tonicity (positive power) EXPECTED PHARMACOLOGICAL MANAGEMENT IN ADDRESSING THIS (HYPERKALEMIC EPISODE): ❖ Loop diuretics / furosemide will not give because patient is already has fluid loss ❖ Sodium Bicarbonate - pwede, most specially this patient is also suffering with ACIDOSIS → technically, lahat ng nabu-burn, more than 25% TBSA - they suffer Acidosis ❖ Calcium gluconate - pwede ❖ Insulin together w/ D5050 ALTERNATIVE TO FUROSEMIDE ● Metabolic acidosis → Hyperk, HypoNa, increased HCO3 excretion - Because skin is exposed 2nd Stage : diuretic / fluid remobilization phase ● After 48 hr ● ISC → IVC - Giving fluids → sodium chloride, NSS is the compatible fluid - Giving sodium bicarbonate through IV → tataas na ang solute particles which is present in intravascular compartment → maghahatak ng maghahatak ng fluid pabalik → yung gradient babalik - Dinagdagan yung salt in intravascular of the patient → technically ang gagawin ni salt na nandun sa ugat, lahat ng tubig na yun na nawala ay hahatakin nya ● Hypervolemia - Accurate I and O, physical examination, noting the lung sounds is very important ● HEMODILUTION, decrease Hct - Diluted ang dugo ng maraming fluid ● diuresis → decreased ADH/ aldosterone ● HypoK, HypoNa WHY STILL PATIENT IS HYPOK AND HYPONA? - Because potassium cannot go back inside, sodium is still there - Sodium is trapped → because there’s edema → systemic ang approach ng inflammation response - Inversely proportional also ● metabolic acidosis → hypoNa, decrease HC03 - Need to replace sodium bicarbonate It will only lead to 2nd stage of burn if we have good interventions - both medical, pharmacological and nursing interventions Cannot just maintain fluid outside extravascular compartment → patient might die because of hypotension, fluid accumulation in the lungs 3rd Stage: Recovery ● 5th day onwards ● HypoCa - Transulations - the blisters has water → to have protection in invasions of other organisms → pinapalabas si calcium → Loss of Ca in the exudate → utilized for wound healing ● (-) nitrogen balance - Because of too much consumption in CHON inside the body - Kulang ang CHON intake compare sa CHON catabolism - CHON is very important into building blocks → in the process of mitosis,magbuo yung tissue and cell para mag-generate ang skin → R/T stress response → increase CHON catabolism → CHON demands intake is less than DIET: - (X) high protein diet because patient whose suffering from burn, also suffering from acute renal injury - On the recovery phase → give high CHON diet because kidney is already okay → kidney was able to excrete out those metabolic products by protein - During the time that suffering from hypovolemia → also suffering from decrease blood supply in GIT → technically, suffering from paralytic ileus → konti ang bowel sounds → hypoactive bowel - Kulang ang dugo sa GIT / stomach → depleted ang production of HCL acid ● HypoK - Very careful in addressing potassium level of the patient Characteristics 1. Minor Burns A. Partial thickness burns are no greater than 15% of the BSA in the adult B. Full thickness burns are <2% of the TBSA in the adult C. Burn areas do not involve the eyes, ears, hands, face, feet, or perineum D. There are no electrical burns or inhalation injuries E. The client is an adult younger than 60 y.0. F. The client has no pre existing medical condition at the time of the burn injury G. No other injury occurred with the burn H. For children: 2nd degree burn less than 10% ➢ SUNBURN is the most common cause of minor burns ➢ 60 years old and above - eliminate for minor burns → tumataas ang category automatically kahit less than 15% ➢ Pag sobrang bata, same thing ➢ Pag meron injury , injury post burn (nakuryente, humampas, napaso, natumba, nagkaroon ng fracture another injury) → tumataas ang category. ➢ May comorbidities → even though it is less than 15% tataas din ang category 2. Moderate Burns a. Superficial Burns are 50% or more b. Partial thickness burns are deep and are 15% to 25% of the TBSA in the adult c. Full thickness burns are 2% to 10% of the TBSA in the adult d. Burn areas do not involve the eyes, ears, hands, face, feet, or perineum e. There are no electrical burns or inhalation injuries f. The client is an adult younger than 60 y.0. g. The client has no chronic cardiac, pulmonary, or endocrine disorder at the time of the burn injury h. No other complicated injury occurred with the burn i. For Children: 2nd degree burn of 10-20% ➢ Older → tataas ulit ang category ➢ May comorbidities → tataas ang category - c. d. e. f. g. h. i. j. Evaluate the affectation of vascularity - Pag pati ang ugat ay nasunog, there’s no oxygenated blood in the extremities → AMPUTATION - Pag may ugat na patuloy na nagcicirculate → save as much as possible - Check also the presence of pulsations → pag may maganda pang circulation → pwede pa makapagpatubo ng balat - Remove eschar tissues → if there’s eschar tissue, there’s no regeneration - Maintain body alignment para di dumikit ang mga balat (remove pressure areas) - Contractures should be addressed properly Burn areas involve the eyes, ears, hands, face, feet, or perineum The burn injury was an electrical or inhalation injury The client is older than 60 y.0. The client has a chronic cardiac, pulmonary, or metabolic disorder at the time of the burn injury Burns are accompanied by other injuries Any degree of Respiratory difficulty All burns complicated by fractures For Children: any 2nd or 3rd degree burn of the body ESTIMATING THE EXTENT OF INJURY 3. Major Burns a. Partial thickness burns are > 25% of the TBSA in the adult - There’s disruption of dermis and epidermis - May blister na kadalasan b. Full thickness burns are > 10% of the TBSA - 3rd degree burn - hanggang sa buto; nasunod ang fasts, adipose tissue - There’s eschar formations - - - - Lund and Browder Method ● Modifies percentages for body segments acc. to age ● Provides a more accurate estimate of the burn size ● Uses a diagram of the body divided into sections, with the representative % of the TBSA for ages throughout the lifespan ● Should be reevaluated after initial wound debridement - initially , need to rule out the patient → need to calculate the TBSA → reevaluate patient post operatively (post debridement) - Repeatedly debridement EXTENT / DEGREE First Degree Pt debridement on bedside or OR - depends on the situation of patient If lesser ang possibility of cardiogenic shock debridement on bedside Pag medyo matanda, need to anesthetize the patient bring patient on OR After debridement, evaluate patient using rule of nine Debridement initially pagdating ni patient sa hospital - most especially if the cause of burn is chemical - wash patients because of possibility of absorptions of chemical through the skin most especially in subcutaneous level ➢ Ang buttocks ay kasama na sa lower extremities na 18 ➢ Using of parkland formula for the fluid challenge ➢ BOARD EXAM: rule of nine (ang ginagamit both local and international) ASSESSMENT OF EXTENT: REPARATIVE PROCESS ➢ Pink to red: slight edema, which subsides quickly. - No blister (kadalasan) depends of the exposure ➢ Pain may last up to 48 hours. ➢ Relieved by cooling. ➢ Sunburn is a typical example. ➢ In about 5 days, epidermis peels, heals spontaneously. ➢ Itching and pink skin persist for about a week. ➢ No scarring. ➢ Heals spont. If it does not become infected within 10 days - 2 weeks. On this particular stage of burn, heal spontaneously without the aid of any medications Usually heals within 5 days Second degree Superficial: ➢ Pink or red; blisters form (vesicles); weeping, edematous, elastic. - There’s blister (Small) - Do not require hospitalization, otherwise, there’s big affectation in TBSA ➢ Superficial layers of skin are destroyed; wound moist and painful. Deep dermal: ➢ Mottled white and red: edematous reddened areas blanch on pressure. ➢ May be yellowish but soft and elastic - may or may not be sensitive to touch; sensitive to cold air. ➢ Hair does not pull out easily Usually, hindi nawawalan ng hair otherwise direct burn (Apoy ang nakaburn) Hair in the skin is still intact Tinutusok yung blister ng karayom and remove the fluid, yung balat hinahayaan lang as a natural covering Colloidal dressing expensive; 1 week healing phase On 2nd degree burn, we can see scar formation as compared into the first degree Takes several weeks to heal. Scarring may occur. Takes several weeks to heal. Scarring may occur. Toothpaste is only good upto 2nd degree although thi is not being practiced by so many medical professionals → Toothpaste has antibacterial property but there’s many component that can absorb by skin THIRD DEGREE ➢ Destruction of epithelial cells - epidermis and dermis destroyed - Up until in the muscle and bone ➢ Reddened areas do not blanch with pressure. ➢ Not painful; inelastic; coloration varies from waxy white to brown;leathery devitalized tissue is called eschar. ➢ Destruction of epithelium, fat, muscles, and bone. AGE AND GENERAL HEALTH 1. Mortality rates are higher for children <4 y.o, particularly those < 1 y.o., and for clients over the age of 60 years. 2. Debilitating disorders, such as cardiac, respiratory, endocrine, and renal d/o negatively influence the client's response to injury and treatment. 3. Mortality rate is higher when the client has a preexisting disorder at the time of the burn injury TYPES OF BURNS A. Thermal Burns: caused by exposure to flames hot liquids, steam or hot objects B. Chemical Burns: a. Caused by the tissue contact with strong alkali ., or organic compounds ➢ Eschar must be removed, Granulation tissue forms to the nearest epithelium from wound margins or support graft. - Eschar is being removed by operations ➢ For areas larger than 3-5 cm, grafting is required. ➢ Expect scarring and loss of skin function. ➢ Area requires debridement, formation of granulation tissue, and grafting. - weak acid (vinegar) pangwash para macounter b. Systemic toxicity from cutaneous absorption can occur C. Electrical Burns: a. Caused by heat generated by electrical energy as it passes through the body b. Results in internal tissue damage c. Cutaneous burns cause muscle and soft tissue damage that may be extensive, particularly in high voltage electrical injuries d. Alternating current is more dangerous than direct current because it is associated with CP arrest, ventricular fibrillation, tetanic muscle contractions, - and long bone or vertebral fractures Paa ng mga nakuryente → parang popcorn - nagpuputok putok kasi kailangan ng kuryente na lumabas sa katawan D. Radiation Burns: caused by exposure to UV light, X-rays, or radioactive source INHALATION INJURIES A. SMOKE INHALATION INJURY ➢ Results from inhalation of superheated air,steam, toxic fumes , or smoke Assessment: ■ facial burns ■ swelling of oro / nasopharynx - Patient who is suffering from oronasopharynx - Adventitious sounds is present; Musical breath sounds (wheezing) and stridor ■ stridor, wheezing and dyspnea - Wheezing and stridor will lead to dyspnea ■ sooty sputum and cough ■ agitation and anxiety ■ erythema ■ singed nasal hair - Evaluate using penlight → check the nose if there’s singed nasal hair ■ flaring nostrils ■ hoarse voice ■ tachycardia Wala na buhok sa ilong ang patient, pulang pula ang oropharynx pero humihinga ng maayos → doctor will intubate patient → because inflammation will occur → do it habang kontrolado pa → when there’s endotracheal tube at namaga, may airway na, di na mag-worry na magkaroon ng airway obstruction B. Carbon Monoxide Poisoning - - - CO is colorless, odorless and tasteless gas that has an affinity for Hgb 200 times greater than that of oxygen O2 molecules are displaced and carbon monoxide reversibly binds to Hgb to form carboxyhemoglobin can lead to coma and death C. Smoke poisoning (lahat ng nagkaroon ng smoke poisoning ay nagkakaroon ng ARDS) ● Caused by inhalation of by-products of combustion ● A localized inflammatory reaction occurs, causing a decrease in bronchial ciliary action and a decrease in surfactant Assessment: ○ mucosal edema in the airways ○ wheezing on auscultation ○ after several hours, sloughing of the tracheobronchial epithelium may occur, and hemorrhagic bronchitis may develop ○ ARDS can result know the size of intubation set or ask doctor D. Direct Thermal Heat Injury ● Can occur to the lower airways by the inhalation of steam or explosive gases or the aspiration of scalding liquids ● Can occur to the upper airways, w/c appear erythematous and edematous, with mucosal blisters and ulcerations ● Mucosal edema can lead to upper airway obstruction, esp, during the 24 to 48 hours PATHOPHYSIOLOGY OF BURNS Increased vascular permeability → magle-leak ng fluid from IVC to ISC → edema → deplete ang volume Increase hematocrit because patient have hemoconcentration → increase and viscosity → hindi makaka-receive ng oxygenated blood ang kidney → kidney will release renin angiotensinogen → converted into angiotensin 2 (one of the most powerful vasoconstrictor into body) → will lead to peripheral resistance → decreased cardiac output → binibilisan ng puso tumibok → tachycardia HEMODYNAMIC / SYSTEMIC CHANGES A. Initially hyponatremia and hyperkalemia occur. Followed by hypokalemia as fluid shifts occur and K+ is not replaced. B. The hematocrit level increases as a result of plasma loss; this initial increase falls to below normal at the 3id to 4th day postburn as a result of the BC damage and loss at the time of injury. C. Initially, the body shunts blood from the kidneys, causing oliguria; then the body begins to reabsorb fluid, and diuresis of the excess fluid occurs over the next days to weeks. D. Blood flow to the GIT is diminished, leading to intestinal ileus (paralytic ileus) and GI dysfunction. E. Immune system function is depressed, resulting in immunosuppression and thus increasing the risk of infection and sepsis. — susceptible to infections (MAINTAIN STRICT ASEPTIC TECHNIQUE) - Stress → body try to compensate → adrenal gland will release cortisol → too much cortisol in circulation → decrease in immune response → immunocompromised → risk to infections F. Pulmonary hypertension can develop, resulting in a decrease in the arterial 02 tension and a decrease in lung compliance. - Di makacirculate ng maayos ang dugo that’s why tumataas ang pressure in the lungs → pulmonary hypertension G. Evaporative fluid losses through the burn wound are greater than normal, the losses continue until complete wound closure occurs - Mas marami ang nawawalang fluid as compared sa nagtatae - Yung tatlong araw nagsusuka at tae, if may 3rd degree burn - kayang ideplete ang fluid just 3 hours H. If the intravascular space is not replenished with IV fluids, hypovolemIa - Shock secondary to hypovolemic - Fluid replacement FIRST AID STOP THE BURNING PROCESS!!! 1. Immerse affected part in cold water 2. Advise Client to roll on the ground it clothing is in flame 3. Throw a blanket over the blanket to smother the flame MANAGEMENT OF THE BURN INJURY Phases of Management of the Burn Injury Emergent phase ● begins at the time of injury and ends with the restoration of capillary permeability, usually at 48-72 hours after the injury ● the 1° goal is to prevent hypovolemic shock and preserve vital organ functioning ● includes prehospital care and emergency room care ● Establish open airway; administer 02 Resuscitative phase ● begins w/ the initiation of fluids and ends when capillary integrity returns to near normal levels and the large fluid shifts have decreased ● the amount of fluid administered is based on the client's weight (kg) and extent of injury ● most fluid replacement formulas are calculated from the time of injury and not from the time of arrival at the hospital ● the goal is to prevent shock by maintaining adequate circulating blood volume and maintaining vital organ perfusion Acute phase ● begins when the client is hemodynamically stable, capillary permeability is restored, and diuresis has begun ● usually begins 48 - 72 hours after the time of injury ● emphasis during this phase is placed on restorative therapy, and the phase continues until wound closure is achieved ● the focus is on infection control, wound care, wound closure, nutritional support, pain management, and physical therapy - Maintain good body alignment after the event of burn - Need the aid of the physical therapy to be sure that there will be contratures Rehabilitative phase ● final phase of burn care ● overlaps the acute care phase and goes well beyond hospitalization ● goals of this phase are designed so that the client can gain independence and achieve maximal function ● Goal: bring back to normal status FLUID RESUSCITATION Indications: ● Adults with burns involving more than 15% - 20% TBSA (need fluid challenge) ● Children with burns involving more than 10-15% TBSA ● Patients with electrical injury, the elderly, or those with cardiac or pulmonary disease and compromised response to burn injury What if a patient with renal failure has 10% TBSA, are we going to do a fluid challenge? - Fluid challenge is difficult to patient’s who are having renal failure, CHF, but in the event that we can’t see evidence that the patient needs fluid, we do not give fluid. Meaning, patient is hemodynamically stable How to know that the patient is hemodynamically stable,what assessment parameters? - Urine output of 30cc/hour → good hydration status - Patient good VS, GOOD MAINTATION (awake, conscious and coherent with orientation to place,time and person) ● Successful fluid resuscitation is evidenced by: ➢ Stable vital signs ➢ Palpable peripheral pulse ➢ Adequate urine output ➢ Clear sensorium - awake, conscious and coherent with orientation to place,time and person ● Urinary output is the most common and most sensitive assessment parameter for cardiac output and tissue perfusion - Urinary output is the most sensitive parameter to know good hydration of the patient - Example: urine output of 30-50 cc/hour - More than 50 cc - terminate fluid challenge - Example: 7,000 ml in the first 8 hours → 7,000 divided into 2 or if the patient is still hydrated, bring back patient to a normal IV fluid ● Generally, a crystalloid (Ringer's lactate) solution is used initially. ● Colloid is used during the 2nd day (5% albumin, plasmate or hetastarch) ● The amount of fluid administered depends on how much intravenous fluid per hour is required to maintain a urinary output of 30 - 50 ml/hr Brooke and Parkland (Baxter) Fluid Resuscitation Formulas for 1st 24 hours after a burn injury FORMULA SOLUTION INDICATION RATE BROOKE 2ml x kg x %BSA + 2000ml/ 24hr (maintenance) ¾ crystalloid, ¼ colloid D5W maintenance ½ in the first 8 hours ½ in the next 16 hours PARKLAND(BAXTER) 4ml x kg x %BSA for Crystalloid only(lactated ½ in the first 8 hours ringer’s) - for the 1st 24 hours ½ in the next 16 hours 24 hour period On the 2nd 24 hours - colloid ❖ Do fluid resuscitation on the time of injury not the time of when the patient go inside the hospital ❖ If a patient goes to hospital after 4 hours, wala na yung 4 hours. 4 hours nalang i-infuse instead of 8 hours PARKLAND FORMULA (included in exam-bring calcu) Example: Patient's weight: 70 kg; % TBSA burn: 80% 1st 24 hours: FORMULA: 4 ml x weight in kg x % TBSA 4ml x 70kg x 80% TBSA = 22,400ml of lactated Ringer's 1st 8 hours = 11.200 ml (divided into 8 hours) or 1.400 ml/hour 2nd 16 hours = 11.200 ml (divided into 16 hours) or 700 ml/hour 2nd 24 hours: FORMULA: 0.5ml colloid x weight in kg × TBSA + 2000ml D5W run concurrently over the 24 hour period 0.5ml x 70kg × 80% = 2800 ml colloid (divided into 24 hours) + 2000 ml D5W (divided into 24 hours) = 117 ml colloid/hour + 84 ml D5W/hour = 201 ml/hr PAIN MANAGEMENT ● Administer morphine sulfate or meperidine (Demerol), as prescribed, by the IV route ● Avoid IM or SC routes because absorption through the soft tissue is unreliable when hypovolemia and large fluid shifts are occurring ● Avoid administering medication by the oral route, because of the possibility of Gl dysfunction - Diminished blood supply in GIT → decreased absorption of medications ● Medicate the client prior to painful procedures ● Use of bed cradle to relieve pressure from topsheet ● Avoid exposure to draft > exposed nerve endings are sensitive NUTRITION ● Essential to promote wound healing and prevent infection ● Maintain nothing by mouth (NPO) status until the bowel sounds are heard; then advance to clear liquids as prescribed - avoid oral fluids 1st 48H (Paralytic ileus, water intoxication) ● Nutrition may be provided via enteral tube feeding, peripheral parenteral nutrition, or total parenteral nutrition ● Provide a diet high in protein, carbohydrates, fats and vitamins ABC - Vit. A › maintains skin and mucous membrane integrity - Provide high protein diet if patient do not suffer from acute renal failure - If suffering from ARF, know the stages and when to give protein (on recovery phase) Preventing infection ● Asepsis - Aseptic technique of all procedure and management ● Reverse/ Protective Isolation ● Tetanus Toxoid, ATS, TIG - Use of vaccines - TT → active, because we give live attenuated vaccines. (do not use alcohol) - Antigenic material - ACTIVE - Equine - came from ANIMAL SERUM → do skin testing - SKIN TESTING: intradermal; 0.9 of sterile water extract first to prevent contamination then 0.1 of medication - Do not write anything on the skin of the patient - they may have an allergy to inks. Instead of putting circle on the bleb, write time and date on micropore then place near the bleb - ATS and TIG → passive because it is antibodies ● Steile NSS to irrigate area ● Antibiotics ESCHAROTOMY - (bedside) to remove pressure on the skin ● A lengthwise incision is made through the burn eschar to relieve ● constriction and pressure and to improve circulation ● Performed for circulatory compromise resulting from circumferential burns ● After escharotomy, assess pulses, color, movement, and sensation ● of affected extremity and control any bleeding with pressure ● Pack incision gently with fine mesh gauze for 24 hours after escharotomy, as prescribed ● Apply topical antimicrobial agents as prescribed FASCIOTOMY - (Operating Room - general anesthesia) lies beneath subcutaneous → before reach the muscle / on the muscle ● • An incision is made, extending through the SQ tissue and fascia ● Performed if adequate tissue perfusion does not return after an escharotomy ● Performed in OR under GA, after procedure assess same as above WOUND CARE 1. The cleansing, debridement and dressing of the burn wounds 2. Hydrotherapy - Usually soak the patient in the water, not the water use in bathing (faucet) → usually NSS A. Wounds are cleansed by immersion, showering or spraying B. Occurs for 30 minutes or less, to prevent increased sodium loss through the burn wound, heat loss, pain and stress C. Client should be premedicated prior to the procedure D. Not used for hemodynamically unstable or those with new skin grafts 3. Debridement A. Removal of eschar to prevent bacterial proliferation under the eschar and to promote wound healing B. May be mechanical, enzymatic or surgical C. Deep partial- or full-thickness burns: Wound is cleansed and debrided and topical antimicrobial agents are applied once or twice daily OPEN DEBRIDEMENT - mechanical, someone will manipulate CLOSE DEBRIDEMENT - use of dressing Open Method Versus Close Method of Wound Care METHOD ADVANTAGES DISADVANTAGES OPEN ● Antimicrobial cream applied, and wound is left open to the air without a dressing ● Antimicrobial cream is applied every 12 hours ● Visualization of the wound ● Easier mobility and joint ROM ● Simplicity in wound care ● Increase chance of hypothermia from exposure CLOSE ● Gauze dressing are carefully wrapped from the distal to the proximal area of the extremity to ensure circulation is not compromised ● No 2 burn surfaces should be allowed to touch; can promote webbing of digits, contractures and poor cosmetic outcome ● Dressing are changed every 8 - 12 hours ● Decreases evaporative fluid and heat loss ● Aids in debridement ● Mobility limitations ● Prevents effective ROM exercises ● Wound assessment is limited