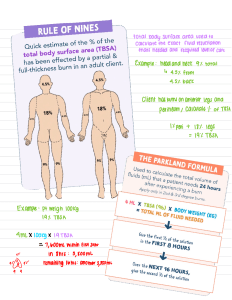
(a lot of the information in the textbook was the same as patho info – hence why these notes are short – I had the patho exam first which basically meant I didn’t need to study this section much since it was still fresh in my head). Med Surg - Nursing Management: Burns (pp. 530-553) - Alkali burns more difficult to manage than acidic since alkalis adhere to tissue better. Three types of smoke/inhalation injuries: 1. Carbon monoxide poisoning – CO displaces O2 on hemoglobin and causes asphyxia – skin colour is “cherry red” in appearance. 2. Inhalation injury above the glottis (i.e. upper airway) – redness, blistering, edema which could lead to mechanical obstruction. Singed nasal hair, hoarseness, painful swallowing, carbonaceous sputum. 3. Inhalation injury below the glottis (i.e. lower airway injury) – usually chemically produced. - - The severity of electrical injuries difficult to determine since most of the damage is below the skin (iceberg effect). Consider transfer of patient to a major burn center if: >20% TBSA partial/full thickness at any age; >10% TBSA partial/full thickness for ages <10 and >50; >5% full thickness burns at any age, burns to face/hands/feet/joints/perineum, electrical burns, chemical burns, inhalation injury, burns with comorbidity, burns with patients with special healthcare needs. Between 10-20% TBSA in adults only minor burn center needed. Also consider if pt has other comorbidities even if minor burn (e.g. diabetes, pregnancy) cause then need major burn center. Prehospital Care - First, remove the patient from the burn source (e.g. fire, electricity, chemical, etc.) If burn injury small (<10%) then cover burn when clean, cool, tap water-dampened towel to minimize the depth of the injury. If burn injury large (>10%) or if pt unresponsive, CAB. If patient responsive, ABC. To prevent hypothermia, don’t put large burns in cool water for more than 10 mins and don’t ever use cold water (we don’t want heat loss). Emergent Phase (Resuscitative) - - The period of time required to resolve the immediate, life-threatening problems resulting from the burn injury – lasts up to 72 hours. Primary concerns are hypovolemic shock and edema. Phase ends when fluid mobilization and diuresis begin. Sludging is when blood is viscous after the burn injury because of the loss of fluid. The combination of decreased blood volume and increased viscosity produces increased peripheral resistance. Intubation is required for all patients with major urns to face and neck. - - Priorities in order: Airway Fluid Therapy Wound care IV antibiotics not routinely used because there is little to no blood supply to the eschar wound so AB won’t even reach there – topical is used instead. Unless sepsis or pneumonia then we use IV AB. Burn patients also at risk of venous thromboembolism so give heparin (or if contraindicated, then use compression stockings). Acute Phase - - Begins with mobilization of extracellular fluid and subsequent diuresis. This phase concludes when the burned area is completely covered by skin grafts or when the wounds are healed (so this phase takes weeks/months). To prevent Curling’s Ulcer (GI ulcers), begin feeding as soon as possible. Give meds that reduce stomach acid as prophylaxis. Nursing management: wound care, excision and grafting, pain management, PT/OT, nutrition, psychosocial care. Feeding: high protein, high carb diet. Rehabilitation Phase - Begins when wound has healed and the patient is able to resume a level of self-care activity. Goals: (a) To assist the patient in resuming a functional role in society and (b) Rehabilitation after functional and cosmetic reconstructive surgery. Pressure can be placed on scar tissue to help flatten it. Most common complications in this phase: o Contractures – An abnormal, usually permanent condition of a joint, characterized by flexion and fixation) – develops as a result of shortening of scar tissue in the flexor tissues of a joint – tends to happen because burn patients are in pain so they like to stay in one flexed position for comfort – to minimize: proper positioning, splinting, exercise. o Hypertrophic scarring SIRS Systemic inflammatory response syndrome (SIRS) is a systemic inflammatory response to a variety of insults, including infection, ischemia, infarction, and injury. Characterized by at least two of the following: fever, edema, hypotension, tachycardia, impaired oxygenation, and elevated WBC. SIRS can be triggered by many mechanisms. Examples: abscess formation, endotoxin release, global perfusion deficits, ischemic or necrotic tissue, mechanical tissue trauma, microbial invasion, regional perfusion deficits. Must determine if there is an infection involved to prevent it from developing into sepsis. To differentiate b/w SIRS and sepsis, serum procalcitonin is a useful biomarker. Interventions: supportive measures such as mechanical ventilation, aggressive fluid resuscitation, nutritional support, cardiac pharmacology, broad-spectrum antibiotics. SIRS can progress to MODS (def’n: failure of two or more organ systems). Goals of care for MODS: (a) prevention and treatment of infection, (b) maintenance of tissue oxygenation, (c) nutritional and metabolic support, (d) appropriate support of individual failing organs.