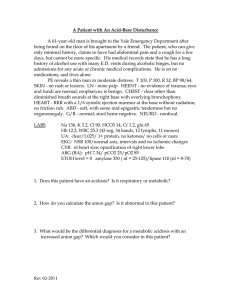
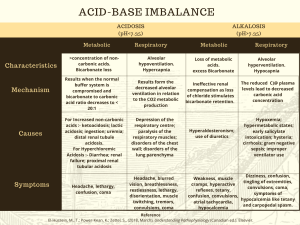
1 Module 1 Reply Hi Roxanne, Your post on Mr. B’s arterial blood gasses and potential causes was well written and easy to follow. Your detailing of why he may be experiencing these symptoms made it an easy post to track, and your recommendations are spot on. I also thought that Mr. B’s acidosis was metabolic and caused by lactic acid for some of the same reasons you detailed. Acting fast, as you point out, is critical, and I wish I would have mentioned how critical in my post. According to Redfors et al. (2021), the amount of cardiac damage that occurs after MI symptoms start is directly associated with the amount of time that passes before a patient receives a percutaneous coronary intervention (PCI) (p. 1). In Mr. B’s case, it’s not only the ischemia from the MI but also his acidosis that makes acting quickly imperative. As you mention, he does not appear to be compensating quickly enough (as evidenced by his PH level) through Kussmaul respirations and intervention will need to occur. According to Huether et al. (2020), more symptoms of metabolic acidosis will start to occur if compensation is inadequate, including anorexia, nausea, vomiting, diarrhea and death in prolonged severe cases (p. 556). While his metabolic acidosis is primarily caused by lactic acid build-up, research indicates that lactic acid is not the only factor in the imbalance. According to an older study by Makino et al. (2005), lactic acid is the primary culprit, and most patients with metabolic acidosis after an MI were also hyperkalemic, hypochloremic, and hyperphosphatemic (p. 1). References 2 Huether, S. E., McCance, K. L., & Brashers, V. L. (2020). Understanding pathophysiology (7th ed.). Elsevier. Makino, J., Uchino, S., Morimatsu, H., & Bellomo, R. (2005). Critical Care, 9(4), R357. https://doi.org/10.1186/cc3714 Redfors, B., Mohebi, R., Giustino, G., Chen, S., Selker, H. P., Thiele, H., Patel, M. R., Udelson, J. E., Ohman, E., Eitel, I., Granger, C. B., Maehara, A., Ali, Z. A., Ben-Yehuda, O., & Stone, G. W. (2021). Time delay, infarct size, and microvascular obstruction after primary percutaneous coronary intervention for st-segment–elevation myocardial infarction. Circulation: Cardiovascular Interventions, 14(2). https://doi.org/10.1161/circinterventions.120.009879