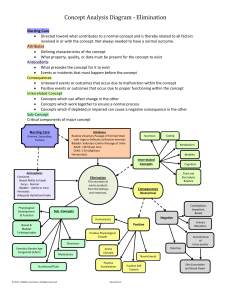
Chapter 47 study guide Functions of the following Mouth: The teeth masticate food, breaking it down to swal-low, and saliva is produced to dilute and soften the food for easier swallowing. Esophagus: The bolus of food travels down and is pushed along by peristalsis, which propels the food through the length of the GI tract. Stomach: The stomach stores swallowed food and liquid; mixing of food, liquid, and digestive juices and empties its contents into the small intestine; produces HCI, mucus, pepsin, and intrinsic factor, which is essential for the absorption of vitamin B12. Small intestine: Segmentation and peristaltic movement facilitate both digestion and absorption; chyme mixes with digestive juices. Lage intestine: The lower GI tract (colon) is divided into the cecum, colon, and rectum. It is the primary organ of elimina-tion. Anus: Contraction and relaxation of the internal and external sphincters, innervated by sympathetic and parasympathetic stimuli, aid in control of defecation. List the physiological factors essential to bowel function and defection a) b) c) d) Normal GI tract function Sensory awareness of rectal distention and rectal contents Voluntary sphincter control Adequate rectal capacity and compliance Identify the 12 factors that influence bowel elimination a. Age b. Diet - fiber provides bulk in fecal material; good sources include whole grains, fresh fruits, and vegetables. c. Fluid intake - recommended 2.7 L/day; fluid liquefies the intestinal contents, easing its passage through the colon; reduced fluid intake slows the passage of food through the intestine and results in hardening of stool contents. d. Physical activity - promote peristalsis, immobilization depresses it; weakened abdominal and pelvic floor muscles impair the ability to increase intraabdominal pressure and to control the external sphincter. e. Psychological factors - during emotional stress the digestive process is accelerated, and peristalsis is increased; stress is associated with ulcerative colitis, irritable bowel syndrome, certain gastric and duodenal ulcers, and Crohn disease. f. Personal habits - work habits and best time for elimination g. Position during defecation - squatting is the normal position h. Pain - hemorrhoids, rectal surgery, anal fissures I. Pregnancy - temporary obstruction created by fetus impairs passage of feces J. Surgery and anesthesia - action of the anesthetic slows or stops peristaltic waves: direct manipulation of the bowel temporarily stops peristalsis (paralytic ileus). k. Medications - slow peristalsis and contractions (constipation) 1. Diagnostic tests - increased gas or loose stool List the conditions that may result in painful defection a. Hemorrhoids b. Rectal surgery c. Rectal fistulas d. Abdominal surgery List the four factors that place a patient at risk for constipation a. Improper diet b. Reduced fluid intake c. Lack of exercise d. Certain medications List the signs of constipation a. Infrequent bowel movements <3 per week b. Hard, dry stools that are difficult to pass Define fecal impaction Fecal impaction occurs when a collection of hardened feces that a person cannot expel (as a result of unrelieved constipation) becomes wedged in the rectum. List signs and symptoms of fecal impaction a. Oozing of diarrhea b. Loss of appetite (anorexia) c. Nausea or vomiting d. Abdominal distention and cramping e. Rectal pain Define diarrhea Diarrhea is an increased number of stools and the passage of liquid, unformed feces associated with disorders affecting digestion, absorption, and secretion. Name the two complications associated with diarrhea a. Contamination and risk of skin ulceration b. Fluid and electrolyte or acid-base imbalances Explain clostridium difficile infection C. difficile is a causative agent of mild diarrhea to severe colitis acquired by the use of antibiotics, chemotherapy, invasive bowel procedures, or a health care worker's hands or direct contact with environmental surfaces. Explain the following Fecal incontinence: the inability to control passage of feces and gas from the anus caused by physical conditions that impair anal sphincter function or control. Flatulence: gas accumulation in the lumen of the intestine; stretches and distends (a common cause of abdominal fullness, pain, and cramping). Hemorrhoids are: dilated, engorged veins in the lining of the rectum; either internal or external Define the following diversions Stoma: an artificial opening in the abdominal wall Ileostomy: a surgical opening in the ileum Colostomy: a surgical opening in the colon List the 14 factors that affect elimination that need to be included in nursing history with pts with altered elimination status a. Determination of the usual elimination pattern b. Patient's description of usual stool characteristics c. Identification of routines followed to promote normal elimination d. Presence and status of bowel diversions e. Changes in appetite f. Diet history g. Description of daily fluid intake h. History of surgery or illness affecting the GI tract i. Medication history j. Emotional state k. History of exercise 1. History of pain or discomfort m. Social history n. Mobility and dexterity Summarize the following steps for assessing the abdomen Inspection: Inspect all four quadrants for contour, shape, sym-metry, and skin color. Note masses, peristaltic waves, scars, venous patterns, stomas, and lesions. Auscultation: assess bowel sounds in all four quadrants Palpation: palpate for masses or areas of tenderness Percussion: detect lesions, fluid, or gas Define fecal occult blood testing (FOBT) Fecal occult blood testing, measures microscopic amounts of blood in feces; useful as a screening tool for colon cancer List the common radiologic and diagnostic tests for pts with altered bowel elimination a. Endoscopy b. Anorectal manometry c. Plain film of abdomen/kidneys, ureter, and bladder (KUB) d. Barium enema e. Ultrasonography f. Computed tomography g. Colonic transit study h. Magnetic resonance imaging List the potential or actual nursing diagnoses for pts with altered bowel elimination a. Bowel Incontinence b. Constipation c. Risk for Constipation d. Diarrhea e. Lack of Knowledge of Dietary Regime List the overall outcomes appropriate for pts with elimination problems a. Patient establishes a regular defecation schedule. b. Patient is able to list proper fluid and food intake needed to achieve elimination. c. Patient implements a regular exercise program. d. Patient reports daily passage of soft, formed brown stool. e. Patient does not report any discomfort associated with defecation. List the factors to consider to promote normal bowel elimination a. Establishes a regular defecation schedule b. Lists proper fluid and food intake needed to soften stool and promote regular bowel elimination c. Implements a regular exercise program d. Reports daily passage of soft, formed brown stool e. Does not report straining or discomfort associated with defecation Identify the primary action for the following Cathartics and laxatives: Cathartics and laxatives (bulk forming, emollient or wetting, saline, stimulant, lubricant) have the short-term action of emptying the bowel. Antidiarrheals: opiate agents decrease intestinal muscle tone to slow passage of feces. Enemas: provide temporary relief of constipation, emptying the bowel before diagnostic tests, and bowel training. Types of enemas Cleansing enema: include tap water, normal saline, soapsuds solution, and low-volume hypertonic saline. Cleansing enemas promote the complete evacuation of feces from the colon. Tap water enema: hypotonic and exerts a lower osmotic pressure than fluid in interstitial spaces. Normal saline: safest enema solution; it exerts the same osmotic pressure as fluids in interstitial spaces surrounding the bowel. Hypertonic solution: exert osmotic pressure that pulls out of interstitial spaces; they are contraindicated in patients who are dehydrated and in young infants. Soapsuds: create the effect of interstitial irritation to stimulate peristalsis. Oil retention: lubricate the rectum and the colon and make the feces softer and easier to pass. Explain the purpose of a carminative enema provides relief from gaseous distention; it improves the ability to pass flatus. List the complications of excessive rectal manipulation a. Can cause irritation to the mucosa b. Can cause bleeding c. Can cause stimulation of the vagus nerve, which results in a reflex slowing of the heart rate List the purpose of nasogastric (NG) intubation a. Decompression - removal of secretions and gaseous substances from GI tract b. Enteral feeding - nutritional supplements for patients with impaired swallowing c. Compression - internal application of pressure by inflated balloon to prevent GI hemorrhage d. Lavage - irrigation of the stomach Explain how the nurse would provide comfort to a pt with a NG tube The nurse should assess the condition of the nares and mucosa for inflammation and excoriation, frequent changing of the tape and lubrication of the nares, and frequent mouth care. List the measures included for a successful bowel training program a. Assessing the normal elimination pattern and recording times when the patient is incontinent b. Incorporating principles of gerontologic nursing when providing bowel training programs for older adults c. Choosing a time in the patient's pattern to initiate defecation-control measures d. Offering a hot drink or fruit juice before the defecation time e. Assisting the patient to the toilet at the designated time f. Providing privacy g. Instructing the patient to lean forward at the hips when on the toilet, apply manual pressure with the hands over the abdomen, and bear down but not strain to stimulate colon emptying h. Unhurried environment and a nonjudgmental caregiver i. Maintaining normal exercise within the patient's physical ability Identify some positive outcomes for a pt with alterations in bowel elimination Patient is able to have regular, pain-free defecation of soft, formed stool.