Bowel elimination
advertisement

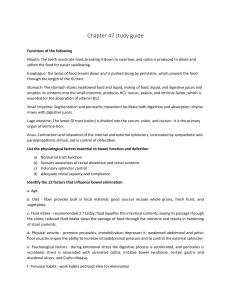
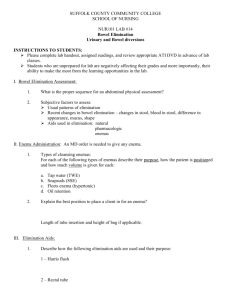
Chapter 45 Bowel Elimination The esophagus is a long muscular tube, which moves food from the mouth to the stomach. The abdomen contains all of the digestive organs. The stomach, situated at the top of the abdomen, normally holds just over 3 pints (about 1500 ml) of food from a single meal. Here the food is mixed with an acid that is produced to assist in digestion. In the stomach, acid and other digestive juices are added to the ingested food to facilitate breakdown of complex proteins, fats and carbohydrates into small, more absorbable units. A valve at the entrance to the stomach from the esophagus allows the food to enter while keeping the acid-laden food from "refluxing" back into the esophagus, causing damage and pain. The pylorus is a small round muscle located at the outlet of the stomach and the entrance to the duodenum (the first section of the small intestine). It closes the stomach outlet while food is being digested into a smaller, more easily absorbed form. When food is properly digested, the pylorus opens and allows the contents of the stomach into the duodenum. The small intestine is about 15 to 20 feet long (4.5 to 6 meters) and is where the majority of the absorption of the nutrients from food takes place. The small intestine is made up of three sections: the duodenum, the jejunum and the ileum. The duodenum is the first section of the small intestine and is where the food is mixed with bile produced by the liver and with other juices from the pancreas. This is where much of the iron and calcium is absorbed. The jejunum is the middle part of the small intestine extending from the duodenum to the ileum; it is responsible for digestion. The last segment of the intestine, the ileum, is where the absorption of fat-soluble vitamins A, D, E and K and other nutrients are absorbed. Another valve separates the small and large intestines to keep bacteria-laden colon contents from coming back into the small intestine. In the large intestines, excess fluids are absorbed and a firm stool is formed. The colon may absorb protein, when necessary. Structures of the Gastrointestinal Tract (alimentary canal) Related to Bowel Elimination – Small intestine – Ileocecal valve – Large bowel (colon) – Ileocecal sphincter – Anal sphincter Physiology of Bowel Elimination Continence – Consistency of the stool (fecal material) – Intestinal motility – Compliance and contractility of the rectum – Competence of the anal sphincters Intestinal Motility and Rectal Accommodation – Rectal filling – Rectal contractions – Rectal accommodation – Postponement of defecation – Constipation Anal Sphincter Mechanism – Internal and external sphincters – Striated muscle fibers – Sensory receptors Factors Affecting Elimination Age Diet Exercise Medications Alterations in Bowel Elimination Constipation Diarrhea Fecal Incontinence Bowel Retention Constipation is infrequent and difficult passage of hardened stool. – Dietary factors, dehydration – Inadequate dietary bulk – Diverticular disease – Neuropathic conditions – Functional limitations Bowel Retention Fecal Impaction – Bolus of hardened stool – Further slows colonic transit time and passage of further fecal contents Bowel Retention Perceived constipation is influenced by psychological and emotional stress. Alterations in Bowel Elimination Diarrhea is the passage of liquefied stool with increased frequency and consistency. Primary Causes of Diarrhea – Malabsorption syndromes – Inflammatory bowel disease – Short bowel syndrome – Side effects of drugs – Laxative or enema misuse Infectious diarrhea is caused by a pathogen. Bowel (fecal) Incontinence – Dysfunction of the anal sphincter – Disorders of the delivery of stool to the rectum – disorders of rectal storage – Anatomic defects Assessment Health History – Elimination habits – Type of incontinence – Complicating factors Assessment Physical Examination – Mental status – Mobility and dexterity – Inspection of perineum for skin integrity – Inspection of vaginal vault – Pelvic support – Perineal sensation – Perianal area, digital rectal exam Diagnostic and Laboratory Data – Stool culture – Defecography – Anorectal ultrasonography Nursing Diagnoses Constipation Perceived Constipation Diarrhea Bowel Incontinence Other Nursing Diagnoses Low Self-Esteem Deficient Knowledge Risk for Infection Risk for Impaired Skin Integrity Toileting Self-Care Deficit Outcome Identification and Planning Target outcomes center around restoring and maintaining regular elimination habits and preventing complications. Implementation Maintain Elimination Health – Fluid intake – Diet – Lifestyle and Prevention Lifestyle and Prevention – Alcohol and tobacco use – Stress management – Weight reduction – Elimination habits – Positioning Lifestyle and Prevention – Initiate pelvic muscle exercise regimen – Suggest environmental modifications – Initiate behavioral intentions – Monitor skin integrity Rectal pouch and rectal tube Initiate Diet and Fluid Therapy Administer Enemas – Cleanse the lower bowel – Assist in evacuation – Instill medication Initiate Rectal Stimulation instruction Various types of enema equipment and solutions equipment Monitor Elimination Diversions – Bowel Diversions Ileostomy Colostomy Ileoanal reservoir (usually done only for ulcerative colitis and familial Polyposis patients. A reservoir is made from the ileum (small bowel) and connected directly to the anus. The sphincter muscle is in place. A temporary Ileostomy is performed to allow the reservoir to heal. Later the Ileostomy is closed and feces exits normally through the anus. ) ileostomy Surgical Management – Implanted devices – Surgical reconstruction – Surgical closure of fistulae and ectopia – Endoscopy, other procedures to alleviate obstruction or dyssynergia Complementary Therapies – Holistic approach to effective elimination of waste products and toxins Diuretics Antimicrobials Antiseptics Stimulants and Cathartics Evaluation Client’s level of maintenance or restoration of elimination patterns and return to an appropriate level of independence Prevention of skin breakdown and infection Client understanding of procedures and self-care coloscopy