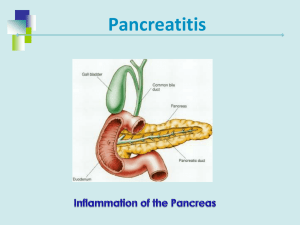
April 6, 2015 Unit Five – Nutrition Therapy for Hepatobiliary and Pancreatic Disorders Case 13 – Acute Pancreatitis 1. Describe the normal exocrine and endocrine functions of the pancreas. The pancreas is a large digestive gland located behind the stomach. The pancreas has two major functions – endocrine and exocrine functions. The pancreas is the only organ that has both exocrine and endocrine functions. The exocrine functions produce enzymes necessary for digestion while the endocrine functions produces hormones to regulate the use of body fuel, mainly glucose. 2. Determine the potential etiology of both acute and chronic pancreatitis. What information provided in the physical assessment supports the diagnosis of acute pancreatitis? Acute pancreatitis has some persisting symptoms. These symptoms include upper abdominal pain that normally worsens with ingestion of food. The mechanism that leads to pancreatic injury is not known, however there are common characteristics like the premature activation of trypsin within the pancreas, resulting in auto digestion of the pancreatic cells. The enzymes released by destroying by destroyed pancreatic cells eventually reach the bloodstream, which causes elevated serum amylase and lipase levels. A diagnosis of acute pancreatitis is based on clinical symptoms and abnormal serum amylase and lipase levels. Chronic pancreatitis is an irreversible inflammation, which leads to fibrosis with tissue calcification. Signs and symptoms are chronic abdominal pain and elevated pancreatic enzyme levels. The patient described having increasing abdominal pain, which is a typical symptom. He also complained of frequent nausea and which are both associated with acute pancreatitis as well. 3. What laboratory values or other tests support this diagnosis? List all abnormal values and explain the likely cause for each abnormal value. The patient has several lab values that support the diagnosis of acute pancreatitis. His LDH levels, AST levels, BUN levels, Serum cholesterol and triglyceride levels, CRP levels, and WBC count are all elevated. The most telling lab values are the extremely elevated Lipase and Amylase levels. The high levels of bilirubin are common among pancreatitis patients. These are what helped diagnose acute pancreatitis. The patient has several other abnormal laboratory values. His high serum osmolality, BUN, and creatinine all indicate that the patient is dehydrated. There is an elevated level of alkaline phosphatase could be due to inflammation in the liver. If there is inflammation, gallstones can form and then block bile ducts, this then causes bile to collect and back up. This backup causes damage to liver which in turn causes an increase in ALP levels. ALT is alanine aminotransferase. The ALT levels are a biological marker of gallstone pancreatitis. Creatine phosphokinase or CPK levels could be elevated because of the inflammation in the patient’s muscle. CPK is an enzyme found in muscles and CPK levels become elevated when there is any kind of muscle damage or inflammation. Segs % and Bands % are types of neutrophils. The neutrophils are elevated because they are a type of white blood cells and elevated white blood cell count is typical among acute pancreatitis patients. He also tested positive for Bilirubin and Urobilinogen, in his urine. These all indicate that there is a problem in the in the some type of biliary obstruction. Protein and Protein chk were both positive and this could be seen in the urine of some patients with pancreatitis. The presence of ketones is also a possible sign of pancreatic problems. 4. The physician lists an APACHE score in his note. What factors are used to determine this score? What does this mean? APACHE means Acute Physiology and Chronic Health Evaluation II and it is a classification system in which the severity of the disease is calculated. Values of 12 clinical measures are used from the first twenty-four hours after admission. The patient’s age, chronic health conditions and physiological variables are all taken into account when determining a score. The higher the APACHE score, the more severe the disease and also the higher the risk of death. The criteria used to get a score are: the age, Glasgow coma score, temperature, MAP, heart rate, respiratory rate, FiO2 levels, PaO2 levels, Arterial pH, Sodium levels, Potassium levels, Creatinine levels, whether or not the patient had acute renal failure, hematocrit levels, and WBC. The patients APACHE score was 4, this indicates that his severity of disease is low and also that his mortality rate is low. 5. What are the potential complications of acute pancreatitis? Potential complications of acute pancreatitis include shock, pulmonary failure, renal failure, gastrointestinal bleeding, and multiorgan system failure. 6. Historically, the patient with acute pancreatitis was made NPO. Why? This patient has an NG tube placed—why? Usually a patient with acute pancreatitis is made NPO because it is assuming that not having the patient consume foods by mouth would stimulate the pancreas and aggravate it causing even more inflammation of the pancreas. This patient has an NG tube placed because he needs nutrients to his body as soon as possible, but he also needs the food to be partially digested in order for his body to be able to break them down. He stated that he has eaten very little over the past three days because of pain, nausea, and vomiting, so it is important that he gets some nutrients into him through enteral feeding immediately. 7. The physician has written an order for a nutrition consult to start enteral feedings. Using the most current literature and ASPEN guidelines, explain the role of enteral feeding in acute pancreatitis. Do you agree with the initiation of enteral feeding? Why or why not? In past years, it was thought that pancreatic neglect was the best way to treat pancreatitis, but now new research has been done with shows that stimulating the gut with enteral nutrition is beneficial to the patient. Also, parenteral nutrition is used as a last resort for patients, if they can process food even a little bit then having them still use their digestive tract is important to keep it functioning. I agree with the initiation of enteral feeding in this patient, because it is important he get nutrients using his digestive tract. Enteral feeding would have the food already partially broken down so it would be easier for the stomach to break down, which would reduce the pain. Also, if the digestive tract is not used, then the patient could be at risk for the digestive tract to stop working. Also,recent studies have shown that enteral nutrition helps patients to recover faster over parenteral nutrition. 8. Does this patient’s case indicate the use of an immune-modulating formula? According to current evidence, enteral feeding is prefered over parenteral feeding. It is recommended that the tube feeding consists of supplements such as omega-3 fatty acids, and other necessary vitamins. Immunemodulating formula is not recommended because extra supplementation is not needed. The patient shows signs of elevated WBC, which indicates an immune response. This is probably due to the pancreatitis. Immune modulating formula formula is not needed. 9. What research supports the use of probiotics in acute pancreatitis? Is there any evidence supporting the use of supplemental glutamine? There is conflicting evidence when it comes to the use of probiotics and its effects in acute pancreatitis. Some studies have shown that there are positive effects of using probiotics, but more recent studies have found opposite results. There is evidence supporting the use of supplemental glutamine in acute pancreatitis patients. Studies show that glutamine supplementation reduced the mortality rate of patients. 10. Assess Mr. Mahon’s height and weight. Calculate his BMI and % usual body weight. BMI: BMI = ( Weight in Pounds / ( Height in inches x Height in inches ) ) x 703 (245 lbs / (71 in)^2) x 703 = 34 BMI Classified as obese UBW: 195 lbs %UBW = (100 x Actual Weight)/Usual body weight = (100 x 245 lbs)/195 lbs = 126% 11. Evaluate Mr. Mahon’s initial nursing assessment. What important factors noted in his nutrition assessment will affect your nutrition recommendations? His excessive intake of alcohol, constant vomiting and nausea, and a steady weight gain over the past 5 years would affect my nutrition recommendations to him. His excessive amounts of alcohol intake puts more strain on his pancreas because of the need to process the high amounts of alcohol, causing oxidative stress to the gland. He would need to cut down on the alcohol consumption or remove alcohol from his diet to allow his pancreas to recover. His constant nausea and vomiting would affect my nutrition recommendations because I would need to keep in mind that it is hard for him to eat and keep food down. Supplements of vitamins and minerals may need to be given to make sure he receives the appropriate amount of nutrients to keep him healthy and in safe ranges of nutrient intake. His constant weight gain over the past five years could make me recommend for him to decrease his his caloric intake once he is able to keep food down again. I believe his decrease in alcohol consumption would help with this issue, but counseling him on a general healthy diet could help him decrease his weight to a healthy BMI. 12. Determine Mr. Mahon’s energy and protein requirements. Explain the rational method you used to calculate these requirements. Energy Needs Harris-Benedict Equation Height: 5’11’’= 71 in = 180.34cm Weight: 245lb = 111.13kg Age: 29 Males: REE= 66.5 + 13.8 (weight in kg) + 5.0 (height in cm)- 6.8 (year old) 66.5 + (13.8 x 111.13kg) + (5 x 180.34) - (6.8 x 29) 66.5 + 1,533.6 + 901.7 - 197.2 = 2,305 kcal Light activity : 2,305 X 1.3 = 2,997 kcal per day - to maintain weight Protein Intake: High levels of distress from abdomen pain 2 g/kg = 2g x 111.13kg = 222 g of protein daily 13. Determine Mr. Mahon’s fluid requirements. Compare this with the information on the intake/output record. 30-40 cc/kg avg size adult and 18-54 yrs old 35cc = 35cc x 111.13kg = 3,890 cc or 3,890 ml The information on the intake/output record says he is intaking 4,500mL and he is output is 4,879mL per day. This information tells me that he needs more fluid than his recommended fluid requirements and more fluid than his nutrition chart suggests because he is losing more fluid than he is taking in. This could lead to dehydration and cause other health complications. 14. From the nutrition history, assess Mr. Mahon’s alcohol intake. What is his average caloric intake from alcohol each day using the information that he provided to you? His average caloric intake from alcohol would be about 1,100 kcals or more from consuming about 11 alcoholic servings daily and more on weekends. One serving of alcohol averages at about 100 kcals. He consumes 6 beers and 4.5 shots daily, and more than that on weekends. 15. List all medication that Mr. Mahon is receiving. Determine the action of each medication and identify any drug-nutrient interactions that you should monitor. Drug Mechanism of Action Drug-nutrient interactions Imipenen inhibits bacterial cell-wall synthesis; binds to penicillin-binding proteins Alcohol should not be consumed. Taking with meals or on an empty stomach may affect results - should be taken in between meals. Pepcid H-2 histamine blocker. Reduces the amount of acid in the stomach. Helps to heal and prevent stomach ulcers, and prevents symptoms like heartburn. H-2 blockers inhibit B12 absorption, and are associated with decreased iron absorption. Meperidine Analgesic; acts as an agonist at the µopioid receptor Alcohol should not be consumed or else dangerous side effects or death can occur. Ondansteron Antiemetic through inhibition of 5-HT3; selective serotonin 5- HT3 receptor antagonist. Low levels of potassium or magnesium in the blood may also increase your risk of QT prolongation (delayed repolarization of the heart). Milk of Magnesia Draws fluid from the body and retains fluid that’s in the lumen of the intestine, thus stimulating nerves within the colon wall, inducing peristalsis and resulting in successful release of colonic content Interferes with absorption of many nutrients, such as thiamine. Colace (docusate) Softens stool by allowing incorporation of water and fat, by the reduction of surface tension of the oil-water interface of the stool. Impacts magnesium levels and increases amount of potassium excreted in the stool. Ativan CNS depressant. Alcohol and other CNS depressants should not be consumed, as consumption could lead to fatal respiratory depression. 16. Identify the pertinent nutrition problems and the corresponding nutrition diagnoses. The patient has not been able to eat due to pain - inadequate oral/food intake The patient drinks 4-5 shots and 6 beers daily - excessive alcohol intake Patient is diagnosed with acute pancreatitis, which compromises the function of his pancreas - impaired nutrient utilization 17. Write you PES statement for each nutrition problem. Inadequate oral intake, RT patient feeling pain resulting in loss of appetite, AEB diagnosed acute pancreatitis secondary to N/V. Impaired nutrient utilization, RT compromised pancreatic function AEB excessive vomiting and diarrhea and significantly elevated liver enzymes Lipase (980 U/L) and amylase (543 U/L). Excessive alcohol intake, RT lack of nutrition education and/or unwillingness to stop drinking, AEB 24-hour recall (4-5 shots of bourbon/day and 6 beers/day). 21. If this patient’s acute pancreatitis resolves, what will be the recommendation for him regarding nutrition and his alcohol intake when he is discharged? Alcohol should be avoided, even well after he is recovered. Supplementation of thiamin and folate, as well as a general multivitamin would be wise due to take care of any deficiencies resulting from his alcoholism. Once a liquid or solid diet is reached, the diet should consist of high-protein, low-fat, easily digestible foods over 5-6 small meals. References Asrani, V, et al. "Glutamine supplementation in acute pancreatitis: a metaanalysis of randomized controlled trials." 6 August 2013. 7 April 2015 <Glutamine supplementation in acute pancreatitis: a meta-analysis of randomized controlled trials.>. Bobroff, Linda B., Ashley Lentz, and R. Elaine Turner. "FOOD/DRUG AND DRUG/NUTRIENT INTERACTIONS: What You Should Know About Your Medications." University of Florida, 1 May 2009. Web. 4 Apr. 2015. <http://edis.ifas.ufl.edu/pdffiles/He/HE77600.pdf>. LeWine, Howard. "What Does It Mean to Have a High CPK Reading?" Sharecare. Sharecare, Inc. Web. 1 Apr. 2015. <http://www.sharecare.com/health/lab-tests/what-have-high-cpk-reading>. Marlik, PE. "What is the best way to feed patients with pancreatitis?" April 2009. 7 April 2015 <http://www.ncbi.nlm.nih.gov/pubmed/19300086>. Matull, W. R., S. P. Pereira, and J. W. O'Donohue. "Biochemical Markers of Acute Pancreatitis." US National Library of Medicine National Institutes of Health. Apr. 2006. Web. 1 Apr. 2015. <http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1860356/>. McClave, Stephen A., Daren K Heyland and Paul Wischmeyer. "Conflicting Results with Use of Probiotics in Severe Acute Pancreatitis." 9 April 2015 <http://www.criticalcarenutrition.com/docs/Manuscript_Editorial_Probiotics_in _Pancreatitis.pdf>. Medscape Log In. (n.d.). Retrieved April 7, 2015, from <http://www.medscape.com/viewarticle/706319>. Nelms M, Sucher K, Lacey, K., Habash, D., Roth S. Nutrition Therapy and Pathophysiology. 2nd ed. Belmonte, CA: Thomson Brooks/Cole, 2010. Robin, Suzanne. "High Levels of Alkaline Phosphatase & Pancreatitis." LiveStrong.com. Demand Media, Inc., 24 Jan. 2014. Web. 1 Apr. 2015. <http://www.livestrong.com/article/412083-high-levels-of-alkalinephosphatase-pancreatitis/>. "Serum Osmolality." Web MD. Web MD. Web. 1 Apr. 2015. <http://www.webmd.com/a-to-z-guides/serum-osmolality?page=2>. "Term: Acute Physiology and Chronic Health Evaluation II (APACHE II)." University of Manitoba. University of Manitoba, 20 Apr. 2012. Web. 1 Apr. 2015. <http://mchp-appserv.cpe.umanitoba.ca/viewDefinition.php? definitionID=104274>. Tremblay, Sylvie. "What Are the Signs and Symptoms of Pancreatic Problems and High Sugar Levels?"LiveStrong.com. Demand Media, Inc., 18 June 2011. Web. 1 Apr. 2015.<http://www.livestrong.com/article/473433-what-are-thesigns-and-symptoms-of-pancreatic-problems-and-high-sugar-levels/>. "Urinalysis: Three Types of Examinations." Lab Test Online. American Association for Clinical Chemistry. Web. 1 Apr. 2015. <http://labtestsonline.org/understanding/analytes/urinalysis/uiexams/start/1/>. "Urine Protein Excretion in Acute Pancreatitis." Pubmed. US National Library of Medicine National Institute of Health, Jan. 1996. Web. 1 Apr. 2015. <http://www.ncbi.nlm.nih.gov/pubmed/2431086>. Windsor, John A. "Nutrition in Acute Pancreatitis: Moving Full Circle or Moving Forward?" 1 July 2014. 6 April 2015 <http://www.gastro.org/journalspublications/aga-perspectives/junejuly-2014/nutrition-in-acute-pancreatitismoving-full-circle-or-moving-forward>.