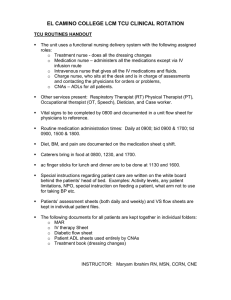
lOMoARcPSD|14963689 CASE Study MH clinical paperwork assignemnt Psychiatric & Mental Health Nu (Horry-Georgetown Technical College) StuDocu is not sponsored or endorsed by any college or university Downloaded by Dana Marie (danamk5611@gmail.com) lOMoARcPSD|14963689 Mental Health Case Study Inpatient Care Facility-Adult Unit As you read through the case study, please answer the questions in bold print. Respond to the questions thoroughly. After completing the packet, please upload it to the designated Dropbox along with other documents as directed. Your clinical group is assigned to visit a mental health inpatient care facility for the first clinical. You are required to wear navy or black slacks, a white top, and non-skid shoes along with your lab jacket instead of the usual uniform worn during the medical-surgical clinical. Review your student handbook. What other elements of professional image required by the nursing program? I am a firm believer that professional image can increase your patient's trust in your abilities. We should wear neat clean clothes without holes, not showing cleavage (for women), for men not showing body hair (with exception of trimmed beard), avoid tight pants and inappropriate logos, carry yourself in a respectful manner, and wear name tags above the waist. Review current ergonomic safety standards used in psychiatric/mental health care settings before going to the facility. List three standards. To avoid muscle and ligaments strains and tears utilize cart to assist with transport, Hold items being carried close to the body, bend at knees when lifting a heavy box. Your group arrives at the hospital and are greeted by the instructor. Downloaded by Dana Marie (danamk5611@gmail.com) lOMoARcPSD|14963689 At the front desk there is a receptionist who welcomes you and gives you a description of their role. Janet answers all incoming calls to the hospital. When a person calls asking for help, she transfers them to a designated nurse or counselor. She gets many calls from individuals asking if an individual is a patient at the hospital. In this situation, she lets them know that patients are given a number for family members to use when calling the hospital. If the caller does not have this information, the receptionist has no way of confirming or denying the person is a patient in the facility. Janet assists family members who drop off things for patient, who come for family meetings, and who are picking up clients who have been discharged. When someone brings items for a client, she uses a metal detector to check for weapons and calls a staff member to retrieve the items for further assessment before giving them to the client. Before individuals can go beyond the waiting room, they must leave keys, bags/purses, cell phone in their car or at the front desk. Janet explains that the same policy goes for student nurses. In addition to these duties, the receptionist announces all of the agency codes over the call system (For example: code red, code blue, code 1, code 10). Review the orientation handbook under Exhibit A. What does a code 1 mean when is announced at this psychiatric facility? When a patient is acting out of control a code 1 is called. It is an emergency What does a code 10 mean? Code 10 means elopement. How would a student respond when these codes are called? Clear the area to open passage of staff, remove equipment, carts and items that could be dangerous or hazardous Before going back into the hospital, you are asked to leave all keys, cell phones, potentially lethal items, such as paper clips and spiral ring note pads in your instructor’s bag. You may have a pen and paper but should not allow a client to use your pen. These are items clients can use to injure themselves or others. Downloaded by Dana Marie (danamk5611@gmail.com) lOMoARcPSD|14963689 What are 3 other common items clients could use to commit self-harm? Car/house keys, metal paper clips, metal spiral ring from books, Sharp pencils and pens. Your instructor takes you to the admission area where clients are brought in by law enforcement and medical transport. Nurses and therapists are assigned to interview clients before taking them to the unit they will be admitted to (Adult, Geriatric, Adolescent, Chemical Dependence, etc.). How should the interview room be set up? What type of furniture should be use? (Use your textbook to assist with this activity.) Open room so the patient doesn’t feel trapped or claustrophobic, HCP staff during interview has a clear way between patient and door in case the situation gets dangerous, the furniture has no attachments that can come off and be used as weapons and is spill-proof in case any foreign substances spill on it. No chords, covered outlets and etc. You are taken to the Adult Unit today. Through a locked door in the nursing unit, there is a board with all the patients’ names listed. (See on next page.) Why is the board with this information kept in a locked room with patient records? Patient privacy, following HIPPA guidelines and additional unit guidelines to protect the patient’s information. What will you do to keep clients’ information confidential while at the facility and after you leave? Anything with the patient’s information on it needs to be shredded before leaving the facilities and nothing is to be discussed with another person in regard to any patients. Keep electronic devices locked (phones, tablets, computers, cameras) when entering the facility Room#/Bed 10 0A James Bennett Date of Admissio n 1/27 Doctor Diagnosis Precautio ns Other diagnoses Miscellaneo us Jefferso n Depressio n SH, SI HTN, Diabetes FS ac and HS 1500 ADA diet, low carb snacks Downloaded by Dana Marie (danamk5611@gmail.com) lOMoARcPSD|14963689 10 0B 10 1A 10 1B Walter Jeffries LOS Allison Gorer 1/25 Wetbac k Psychosis ETOH E, Agg Asthma VS q4 hrs x 24 hrs 1/22 Flowers PTSD HI, Agg HTN, hypercholesterolem ia Low Na, Cardiac Diet Jennifer Sweene y Dennis Griffin 1/25 Jefferso n Anxiety F 10 1/25 Wetbac Depressio SH, SI HIV RD consult 2 k n A 10 Frances 1/25 Jamison Bipolar II SI 2 B Ray Your nursing instructor reviews the board with you. She let you know that you should be aware of the three clients who are aggressive, Ms. Ray, Ms. Gorer, and Mr. Jeffries. The first two clients have a staff member assigned to them at all times (one-to-one status), but Mr. Jeffries is free to move around the unit as he pleases after completing detoxification from alcohol. Mr. Jeffries’ nurse tells you that the client has been participating in group sessions more often. He has not exhibited aggressive behavior in the last 48 hours. Medication Administration Record Dr. Ervin Hill Medication Administration Metformin 1000 mg One tablet PO BID Olanzapine 10 mg One tablet PO BID Losartan 25 mg One tablet PO QD Multi-vitamin One tablet PO every morning Phenytoin 100mg One extended-release capsule PO every day PRN Magnesium hydroxide (400mg/5mL) 30 mL PO at HS PRN for constipation Acetaminophen 500 mg (250 mg tabs) Two tablets PO Q4 hrs. 0900 2100 0900 2100 Assessments Required Walter Jeffries Room 100B DOB 5/4/1962 NKDA Other 0900 0900 0900 Monitor blood levels weekly. 2100 Date Time Init. Assessment Assessment Downloaded by Dana Marie (danamk5611@gmail.com) lOMoARcPSD|14963689 PRN for pain or fever Diazepam 1-2 mg PO Q8 hours PRN for agitation Date Time Init. Assessment You follow the nurse as she administers medications to her clients. She pulls only one patient’s medications at a time. Why is this best practice? To avoid giving the wrong medications, making sure it’s for the right patient, at the correct time and correct dose. Medication errors are a common mistake so enforcing these rules are a must for medication safety. What could happen if you pull more than one client’s medications at once before administering them to them? This could hurt he patient and cause major health concerns opening the door for legal actions against the HCP. A mix up of medications could be fatal. Mr. Jeffries. See her MAR above. The patent refuses his morning dose of Metformin. Should the nurse inform Mr. Jeffries that he will be put in seclusion immediately if he does not take this medication? Why or why not? No. The patient has the right to refuse medication. Nurse should ask why the refusal then document. What would you do if you were the nurse? I would ask the patient the reason for refusal, explain why the medication is recommended and try again at a later time. Which drugs would you pull for the patient? (Make a drug card for each drug you will administer) I would pull Metformin, Olanzapine, Losartan, Multi-vitamin, and Phenytoin. PRN drugs would be based on needs either from my judgment as a nurse or if the patient asks for it. What diagnostic test would you want to review before giving Mr. Jeffries his Phenytoin? Why? Does the patient have liver issues? Check AST, ALT, liver enzymes. Check blood levels to make sure phenytoin is within the therapeutic range. 10.0-20.0 mcg/mL Concerns should be shared with the HCP. Are there any foods or drinks the client should be taught to limit or avoid while taking these drugs? If so, give a description of what you would teach. Advise patient to avoid alcohol. Warn patient not to stop drug abruptly. Stress importance of good oral hygiene and regular dental exams. Female patients teach about preventing pregnancy as drug may be harmful to fetus Wear sunscreen Avoid salt substitutes Downloaded by Dana Marie (danamk5611@gmail.com) lOMoARcPSD|14963689 Vitamin D and calcium supplements may be needed If the psychiatrist orders the Olanzapine to be administered intramuscularly, what site would you use for solutions of 3 mL or more? (Review your IM administration sites for the recommend volume to inject.) Gluteal injection (IM) to avoid erratically absorption of medication and possibly fatal SE. As you know, patient identifiers are vitally important in preventing medication errors. Name and date of birth along with a picture of the psychiatric client are used to verify a client in facilities with or without a scanning system. What questions would the nurse need to ask when verifying this information? 2 verifiers (first, last name and dob of the patient) checking a matching wristband or badge identifier The instructor shows your group a patient room. (Freemont Hospital, San Francisco,CA) . (Norvoplastic.com) besafeprod.com Downloaded by Dana Marie (danamk5611@gmail.com) lOMoARcPSD|14963689 You notice the beds and other furnishings have bolts attaching them to the floor, and call light cords are less than 6 inches long. Trash cans have paper liners instead of plastic ones. Door-knobs inside each patient room and restroom are cone-shaped. Cubbies or shelves are available for clients to keep their clothes. No belts or shoestrings are allowed. Any valuables and clothing with strings should be sent home with family or are locked away. The facility provides all personal care items. Each unit has a washer and dryer for clients to launder their clothes (laundry supplies provided). Restroom doors are slanted. Mirrors consist of plexiglass, and all pipes are covered. The showerhead is short, and the tissue paper holder is just an opening in the wall. Shower curtains are attached by Velcro and pull away when weight is applied. Also, the water level in the toilet bowl is low, and the tank's lid is sealed. A motion sensor activates water to flow in the sink instead of knobs. When looking at the inpatient environment (beds, doorknobs, etc.), how can these quality improvement measures impact the safety of clients? Alarm above the door prevents the patient from hanging, sounding when the patient attempts to hang or tie something to it. Showerhead is short and close to the wall to prevent the patient hanging self, antiligature doorknobs, safety handles are filled in, curtains are Velcro and detach with over 40lbs of weight, outlets are filled in and etc. The facility cannot accommodate clients who require airborne and droplet precautions but can implement contact precautions if needed. You are the nurse for a client who needs to be placed on contact precautions. What would be required? How would you plan to care for the patient in this environment? Hand hygiene is the main focus for prevention of spread for staff and patients, don’t share the patient’s personal items and equipment, and they can’t leave the facility. Clients need to be 3-6 feet apart. Make sure wounds are clean, dry, intact, or covered when the patient is out of room. MRSA, VRE should be isolated in private room. Standard precautions are always in place for staff. At 1000, group sessions begin a large room at the end of the hall. The room has 30 heavy upholstered single chairs lined in rows around the room. A staff member starts the Goals Meeting by welcoming everyone and asks everyone to take turns sharing information from their goals sheet. Everyone who is willing shares in the Goals Group this morning. The clients will have a one- and- a -half hour break to make outside calls. Each patient has 5 minutes to call family members. Clients may be called in to speak with their therapists during the morning also. How would a goals group be beneficial a client with mental illness when they are discharged from the facility? Downloaded by Dana Marie (danamk5611@gmail.com) lOMoARcPSD|14963689 Patients find relatability in group sessions which gives them a sense of belonging. Reducing social isolation and sharing common experiences that they will work on pursuing once discharged from the facility. Nurse Session. The nursing students have been asked to teach patients about “__________________.” Record a 10 -minute session of yourself sharing the information your group compiled on the topic in an audio or audio-visual format. Upload your case study with answers to the designated clinical Dropbox. Place your recorded teaching media to the designate Discussion Board for group members to access. Review two classmates’ recordings and give them feedback on their work using 60 or more words. Make mention of how safety, patient-centered care, CDM, and professional behavior was reinforced by this clinical assignment in the discussion. Downloaded by Dana Marie (danamk5611@gmail.com)