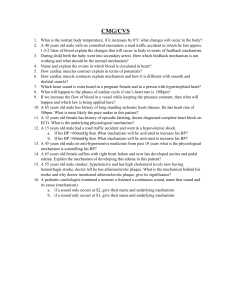
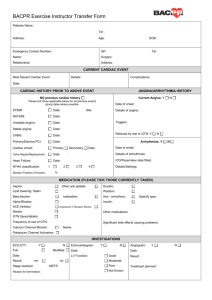
lOMoAR cPSD| 10103054 Exam 4 Review • Symptoms of and treatment for varicose veins • • Symptoms: heavy, achy feeling or pain after prolonged sitting or standing, which is relieved by walking or limb elevation. Some may feel pressure or an itchy, burning, tingling throbbing, or cramp-like leg sensation. Treatment: Sclerotherapy Drug is Venoactive drug. Transcutaneous therapy and high intensity pulsedlight therapy. • Risks: Age (people older than 65), HTN and CAD are primary risk factors; Others are Diabetes, Metabolic Syndrome, Advanced Age, Tobacco Use, Vascular Disease, Congenital Abnormalities (septal defects), infiltrative cardiomyopathies, infections, inflammatory processes, persistent dysrhythmias and toxins (ETOH). Risk factors: (Modifiable) HTN, CAD, diabetes, metabolic syndrome, tobacco use, and vascular disease; obesity and high serum cholesterol; (Non-modifiable) advanced age, ethnicity, family history/genetics Sclerotherapy procedure Complications/organ damage from HF • IV injection of a liquid or foam (any kind of liquid) sclerosing substance that chemically ablates or destroys the treated veins. • Self care for venous insuffiency • Self care includes frequently elevating legs above the level of the heart to reduce edema; Begin a daily walking program; avoid trauma to the limbs; provide proper foot and leg care to avoid further trauma; eat a proper diet of adequate high protein (meat, beans, cheese, tofu), vit A (green leafy veggies), vit C (citrus fruits, tomatoes, cantaloupe), and zinc (meat, seafood); maintain normal glucose levels; daily moisturizing is important to reduce itching and skin cracking; proper wound care Risk factors for HF Pleural Effusion (fluid between 2 layers that cover the lung and line the chest wall); Dysrhythmias and dyssynchronous contractions (Atrial and ventricular dysrhythmias), hepatomegaly, cardiorenal syndrome, and anemia. Risk factors for endocarditis • IV drug abuse, infection, valve replacement, oral surgery (3-6 months), surgery, and IV line placement; INVASIVE CATHETERS Symptoms of mitral valve regurgitation • • Acute: generally, poorly tolerated. New systolic murmur with pulmonary edema. Cardiogenic shock develops rapidly. Chronic: weakness, fatigue, EXERTIONAL DYSPNEA, lOMoAR cPSD| 10103054 palpitations, S3 gallop, holosystolic murmur Nursing care for post-TEE • Patient may not eat or drink until gag reflex returns; monitor patient until sedation resolves; sore throat is temporary; a designated driver is needed if test is done in the outpatient department. SE of ace inhibitors, calcium channel blockers, diuretics, beta blockers, nitrates • • • • • Ace: dry cough, HYPERKALEMIA, fatigue, dizziness, HA, loss of taste CCB: fatigue, HA, nausea, rash, dizziness, flushing, and peripheral edema. Diuretics: HYPOKALEMIA, HYPONATREMIA, HA, dizziness, thirst, increased blood sugar, muscle cramps BB: fatigue, dizziness, bradycardia, hypotension, wheezing from bronchospasm, weight gain, depression, and sexual dysfunction Nitrates: HA (most common), dizziness, weakness, ORTHO HYPO Nursing interventions for pulmonary edema • • • • Ongoing monitoring of VS, O2 sat, weight, mentation, ECGs and indications of fluid overload and decrease organ perfusion Assess vital every 4 hours High-fowler’s position Non-invasive positive pressure ventilation (non-rebreather but if worse, BiPAP) • Record I/O and daily weights; assess for edema, ascites, JVD, S3/S4 heart sounds, crackles, hypoxia, worsening renal function Hemodynamic monitoring (intraarterial BP, PAWP,CO) • Cardioversion (A-Fib) • GOTTA HELP THEM BREATH!! Pre-op care cardiac catheter. • • • • • • Assess allergies; contract dye Perform baseline assessment including VS, pulse ox, heart and breath sounds, neurovascular assessment of extremities (skin temp, skin color, sensation) Withhold food/fluids for 6-12 hrs before Assess baseline labs values (cardiac biomarkers, creatinine) Explain use of local anesthesia at insertion site, placement of catheter, flushed feeling when dye is injected, and possible fluttering sensation of heart as catheter is passed Give sedation and other drugs, as ordered Post-op cardiac catheter • • Perform assessment and compare to baseline; VS; pulse ox, and heart/breath sounds. Note hypotension or hypertension and signs of pulmonary emboli (respiratory difficulty). Assess neurovascular status including peripheral pulses, color, and sensation of extremity per agency protocol. lOMoAR cPSD| 10103054 • • • • • • • Place compression device over arterial site to achieve hemostasis, if indicated Observe insertion site for hematoma and bleeding every 15 min for 1 hr and then per agency protocol. Monitor ECG for dysrhythmias or other changes (ST segment elevation) Monitor pt for chest pain and other sources of pain or discomfort Maintain bedrest as ordered for femoral access Maintain IV and/or oral fluid intake and monitor urine output Teach pt and caregiver about discharge care, including s/s to report to HCP (site complications, return of chest pain), and any activity restrictions arterial spasm at the arm or anastomosis site Care of patients with infective endocarditis • • • • Care of patient during and after MI • REMEMBER THE RISK FOR HF; ALSO AFTER O2, EKG • Care AND DIAGNOSTICS of patient with HF • COMPLICATIONS OF HF: HYPOTENSION, LOW URINARY OUTPUT Arm precautions post CABG • Care: monitor sensory and motor function of the hand; patient with radial artery harvest should take a calcium channel blocker and/or a long-acting nitrate for around 3 months to reduce the incidence or • • Avoid people with infections, especially upper respiratory tract infections, and to report cold, flu, and cough symptoms; avoid excessive fatigue, plan rest periods use good oral hygiene and schedule regular dental visits Treat with antibiotics every 4-6 wks After initial treatment at home,; make sure patient has adequate nursing care for IV antibiotics Monitor body temp; elevated temp may mean that antibiotic is ineffective, and patient may be at risk for stroke, pulmonary edema, and HF; tell patients to recognize s/s of these complications (change in LOC, dyspnea, chest pain, unexplained weight gain) Get physical and emotional rest but patient may also wear SCD to perform ROM exercises, deep breathing and coughing every 2 hours; Teach how to reduce risk for infection; explain importance of follow-up COMPLICATIONS: PERICARIAL EFFUSION (BUILD UP OF FLUID IN THE PERICARDIUM) AND CARDIAC TAMPONADE (DEVELOPS AS PERICARDIAL EFFUSION VOLUME INCREASES AND COMPRESSES THE HEART) Hypokalemia’s effect on cardiac rhythm lOMoAR cPSD| 10103054 • Effect: impaired repolarization, resulting in a flattened T wave, depressed ST segment, and the presence of a U wave; P waves peak and QRS complex is prolonged; there is an increased incidence of heart block and potentially lethal ventricular dysrhythmias. • Findings: right ventricular heaves, increased HR, murmurs, JVD, lower extremity edema, weight gain, ascites, anasarca, hepatomegaly Normal sinus rhythm characteristics • P WAVE BEFORE EVERY QRS Patient teaching for permanent pacemaker Cardiac tamponade assessment findings • Findings: Chest pain, confused, anxious, restless, decreased CO, muffled heart sounds, narrowed pulse pressure, tachypnea, and tachycardia, JVD Indications AND TEACHING for SL nitroglycerin • • • • Indications: pt can take it once every 5 min if still feeling chest pain and/or symptoms of angina Pt may experience HA, dizziness, and flushing but this is normal Advise pt to also get up slowly but ortho hypo will also occur Report any pain such as increasing frequency, nighttime angina, or angina at rest DASH diet • • Dietary Approaches to Stop Hypertension; teaches you that you should eat fruits, veggies, fat-free or low-fat milk and milk products, whole grains, fish, poultry, beans, seeds, and nuts. Lowers BP and reduces low-density lipo-protein LDL cholesterol. Assessment findings in right HF Digoxin toxicity signs and symptoms • • • • • Lack of appetite, N/V/D HA, confusion, anxiety, or delusions Restlessness, weakness, or depression Changes in vision such as blurred vision or seeing ‘halos around bright objects’ Fast, slow, or irregular HR or palpitations CV findings in the elderly • • • • • Decreased cardiac reserve, HF, S4 may be present Difficulty in isolating apical pulse Decreased response to exercise and stress; slowed recovery from activity Decreased amplitude of QRS complex and slight lengthening of PR, QRS, and QT intervals; Irregular cardiac rhythms; decreased maximal HR; decreased HR variability Systolic murmur (aortic or mitral) possible w/o a sign of CVD AAA repair complications lOMoAR cPSD| 10103054 • • Endoleak (most common; seepage of blood back into the old aneurysm); Aneurysm growth above or below the graft; aneurysm rupture; aortic dissection; bleeding; renal artery occlusion caused by stent migration, graft thrombosis, incisional site hematoma, and incisional infection Potentially lethal complication in an emergency repair of a ruptured AAA is the development of a intraabdominal hypertension (IAH) with associated abdominal compartment syndrome • Stress test patient prep and teaching • Care of patient with AAA (Symptoms of rupture; care to avoid rupture) • Labs for MI • • Labs: cardiac troponin I or T Creatinine, Urea, Electrolytes, ABGs, Lipids, Full Blood Count (H&H, WBC, RBC, platelets), CKMB, Myoglobin Cardioversion precautions • • • Precautions: make sure an airway is maintained If patient is with supraventricular tachy or VT with pulse and becomes hemodynamically unstable, synchronized cardioversion should be done ASAP Start initial energy at 50 to 100 joules (biphasic defib) and 100 joules (monophasic defib) and increase if needed If patient becomes pulseless or goes into VF, switch off and perform defib. Prep BEFORE: tell patients to wear comfortable clothes and shoes that can be worn for running or walking; tell patient to report any symptoms; Beta-blockers may be held 24 hours before the test because they blunt the HR and limit the patient’s ability to achieve maximal HR (NO HEART MEDS); caffeine held for 24; smoke and strenuous exercise held for 3 hr before the test; obtain baseline VS and 12-lead ECG During: monitor VS and ECG during each stage of exercise and after until all VS and ECG changes have returned to normal/baseline; monitor patient’s response throughout procedure for any signs of distress (angina, SOB) Care for venous leg wounds • Compression therapy is important for healing; assess arterial status to make sure that PAD isn’t present; show patient how to correctly apply compression therapy and ‘show back’; tell pt to replace every 4-6 months • Avoid standing or sitting for long periods of time for this decreases blood return Elevate legs above the heart to reduce edema Encourage daily walking program once wound heals • • lOMoAR cPSD| 10103054 • • • • Avoid trauma to the limbs Foods high in PROTEIN Give prescribed analgesics, antibiotics, or other drugs Teach pt and caregiver about manifestations, complications, and treatment of venous insufficiency Pericarditis care (inflammation of the pericardial sac, often with fluid accumulation) • Precautions for Reynauds • • • • • Precautions: Tell patients to avoid temp extremes and wear loose, warm clothing as protection from the cold, including gloves when handling cold objects. Stop using all tobacco products and avoid caffeine and other drugs that have vasoconstrictive effects (cocaine, amphetamines, ergotamine, pseudoephedrine) Have adequate stress management strategies. Immerse hands in warm water often to decrease vasospasm. LIMIT EXACERBATIONS • • • STEMI (ST elevated MI) IS IN THE LEFT ANTERIOR VENTRICLE o MEDICAL EMERGENCY; ARTERY MUST BE OPEN WITHIN 90 MIN OF PRESENTATION TO RESTORE BLOOD AND O2 TO THE HEART MUSCLE AND LIMIT THE INFARCT SIZE TROPONIN MONA • Math ***Go over objectives before every chapter and be able to answer them Treat the underlying problem and the symptoms; bed rest; keep HOB up to 45 degrees and provide overbed table support; drug therapy (NSAIDS, Corticosteroids; avoid ETOH for risk of GI bleed; PPI can help with stomach acid); Prepare for possible Pericardiocentesis (needle is inserted in the pericardial space to remove fluid for analysis and relieve heart pressure); Explain procedure and possible causes of pain to reduce anxiety; important for the pt who previously had angina or MI BEST LAB FOR MI! MORPHINE, O2 THERAPY, NITROGLYCERIN, ASPIRIN CO = SV x HR • AMOUNT OF BLOOD PUMPED BY EACH VENTRICLE IN 1 MIN; AMOUNT OF BLOOD EJECTED FROM THE VENTRICLE WITH EACH HEARTBEAT (STROKE VOLUME x TIMES HR PER MIN) Discharge teaching after MI Time frame for thrombolytic therapy with MI • Treatment of STEMI with lOMoAR cPSD| 10103054 • thrombolytic therapy aims to limit the infarction size by dissolving the thrombus in the coronary artery to reperfuse the heart muscle. The goal is to give the thrombolytic with 30 MIN OF THE PATIENT’S ARRIVAL TO THE ED MAP calculation: SBP + 2DBP / 3 What is a good MAP? • The normal MAP range is between 70 and 100 mmHg. Mean arterial pressures that deviate from this range for prolonged periods of time can have drastic negative effects on the body. Normal EF (50%-75) and signs of poor EF • Signs: SOB; heart palpitations; edema in the legs, feet of belly; fatigue or exhaustion